Professional Documents
Culture Documents
Bordetella Bronchiseptica
Uploaded by
AntonisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bordetella Bronchiseptica
Uploaded by
AntonisCopyright:
Available Formats
Open Access Case
Report DOI: 10.7759/cureus.15976
A Case of Bordetella bronchiseptica Bacteremia in
a Patient With COVID-19: Brief Report
Styliani Papantoniou 1 , Antonios Tsakiris 1 , Theodoros Ladopoulos 2 , Georgios Kranidiotis 1 , Charalampos
Tamvakos 1
1. Department of Internal Medicine and Diabetes Center, Tzaneio General Hospital of Piraeus, Piraeus, GRC 2.
Department of Neurology, St. Josef Hospital, Ruhr University Bochum, Bochum, DEU
Corresponding author: Antonios Tsakiris, tsakirisanton@gmail.com
Abstract
Bordetella bronchiseptica is a gram-negative coccobacillus that colonizes the respiratory system of
mammals such as dogs, cats, rabbits and others and might cause upper respiratory tract infections. Although
it can be rarely pathogenic in humans, there are several case reports describing infections in humans. We
describe the case of a patient without prolonged immunosuppression or underlying diseases, with
bacteremia from Bordetella bronchiseptica, while being treated in a tertiary hospital for COVID-19 infection.
Categories: Emergency Medicine, Internal Medicine, Infectious Disease
Keywords: covid, bacteremia, neutrophils-lymphocytes-ratio, opportunistic, bordetella bronchiseptica,
dexamethasone
Introduction
Bordetella bronchiseptica can rarely cause infection in humans [1]. However, various case reports describe
infections such as pneumonia, bacteremia, and pancreatic abscess in patients with immunocompromising
conditions [2]. In the literature, there are reports of Bordetella bronchiseptica co-infection in patients with
COVID-19, mostly related to respiratory infections [1]. We describe the first case of bacteremia in an
immunocompetent patient with no underlying comorbidities who was hospitalized due to severe COVID-19.
Case Presentation
A 47-year-old patient presented to the emergency department of a tertiary hospital in March 2021 with fever
up to 39°C which started six days prior to admission. The patient did not report any health problems or any
home medications. A molecular test was performed by PCR for SARS-CoV-2, which was positive. Clinical
examination revealed dryness of the mucous membranes and diffuse bilateral crackles. No other
pathological findings were found during the clinical examination. Notable findings in the laboratory tests
were leukocytosis (WBC 32,190/mm 3), neutrophilia (Neu 31,200/mm 3), and severe lymphopenia (Lymph
470/mm3). The patient’s virological test was negative for HIV, hepatitis C virus (HCV), and hepatitis B virus
Review began 06/07/2021 (HBV). Treatment of the patient upon admission included antiviral therapy with remdesivir, intravenous
Review ended 06/18/2021
dexamethasone at a dose of 6 mg due to respiratory failure, prophylactic anticoagulant therapy with low
Published 06/27/2021
molecular weight heparin, and empirical antibiotic therapy with ceftriaxone and azithromycin. On the
© Copyright 2021 second day of hospitalization, his respiratory status deteriorated and his treatment was escalated in a high-
Papantoniou et al. This is an open access
flow nasal cannula. The patient’s respiratory condition de-compensated requiring endotracheal intubation
article distributed under the terms of the
Creative Commons Attribution License
and transfer to ICU. Our patient on the 10th day of his hospitalization in the Intensive Care Unit developed a
CC-BY 4.0., which permits unrestricted new fever of 39.6°C. Bordetella bronchiseptica, Candida tropicalis and Enterococcus faecium were isolated
use, distribution, and reproduction in any in blood cultures obtained from the central venous line, which was inserted before admission to ICU, while
medium, provided the original author and only Bordetella bronchiseptica was isolated peripherally (Table 1).
source are credited.
How to cite this article
Papantoniou S, Tsakiris A, Ladopoulos T, et al. (June 27, 2021) A Case of Bordetella bronchiseptica Bacteremia in a Patient With COVID-19: Brief
Report. Cureus 13(6): e15976. DOI 10.7759/cureus.15976
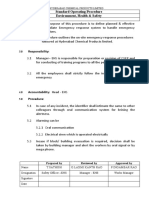
bbr
Antimicrobial MIC Result
Amikacin <=2 S
Cefotaxime 8 R
Ceftazidime 4 IE
Gentamicin <=1 S
Imipenem <=0.25 S
Meropenem <=0.25 S
Tigecycline <=0.5 S
Differential time to positivity Negative for CRB
TABLE 1: Blood Culture Results
bbr: Bordetella bronchiseptica; MIC: Minimal Inhibitory Concentration; S: Susceptible; IE: Insufficient evidence to set a clinical breakpoint; R:
Resistant; CRB: Catheter-related bacteremia.
Central venous catheter was replaced and antibiotic treatment was escalated to piperacillin / tazobactam,
linezolid, and caspofungin. The patient remained hemodynamically stable, was successfully extubated on
the 14th day of his ICU hospitalization and he returned to the COVID-19 clinic to continue his treatment.
Three days later and while our patient was receiving the antibiotic treatment, he presented a new fever and
new blood cultures were obtained. Bordetella bronchiseptica was isolated in both the blood culture sets
taken from the central venous line and the set taken from the peripheral venous line. The strain isolated was
the same as the one isolated before. Antibiotic treatment was escalated to meropenem, while linezolid and
caspofungin were discontinued. The patient remained clinically and hemodynamically stable and received
treatment for Bordetella bronchiseptica bacteremia for a total of 14 days. He was discharged after 24 days
after his admission. At the follow-up of the patient one month after discharge, the patient did not present
any clinical complications and the laboratory parameters had recovered to normal levels.
Discussion
Bordetella bronchiseptica is a gram-negative coccobacillus that colonizes the respiratory system of
mammals, mainly dogs, cats and hares and causes infections of the respiratory system [3]. Although it can be
rarely pathogenic in humans, several case reports are describing various infections such as pneumonia,
bacteremia, pancreatic abscess in patients with immunocompromising conditions [2], while there are reports
of Bordetella bronchiseptica pneumonia in patients with COVID-19 [1]. The microorganism settles inside
the epithelial cells and escapes the host's innate immune response. This allows it to remain in the host's
respiratory system for a longer period, releasing toxic products and bacteria. In the case of patients with
immunosuppression, this procedure can be further accelerated, as the compromised mechanisms of the
innate immune system make it even more difficult to treat the microorganism [3].
According to a recent meta-analysis, the incidence of bacterial infections in patients with COVID-19 is 6.9%
and is significantly lower compared to that reported in patients with influenza [4]. Bacterial infections are
more common in patients with severe disease and occur later in viral infection.
The pathogenetic mechanism has not been clarified. In patients with COVID-19, gram-negative pathogens
are the leading cause of bacterial infections. The pathogenic microorganism responsible for bacteremia
usually originates from the microbiota of the respiratory system, especially in immunocompromised
patients. Prolonged invasive mechanical ventilation appears to play an important role in the development of
a secondary bacterial infection. The destruction of airway barriers due to ventilator-associated injury in
combination with the immune-related epithelial damage caused by SARS-CoV-2 leads to the invasion of
opportunistic bacteria which have colonized the respiratory system [4].
Our patient presented an increased neutrophils-lymphocytes-ratio (NLR), a marker that indicates a
disturbed immune response and has been associated with a worse outcome in patients with COVID-19. The
role of neutrophils in the mechanisms of innate immunity is of vital importance, while lymphocytes are
essential for the inflammatory response of the patient. NLR reflects the body's response to the infection, as
an increase shows neutrophil rising, lymphocyte apoptosis, or both. Studies have shown that NLR has a
higher prognostic value compared with other inflammatory markers for the diagnosis of bacteremia [5].
Although the NLR can be influenced by patient's comorbidities and could be a better criterion for the
rational administration of antibiotics to patients with COVID-19 [6].
2021 Papantoniou et al. Cureus 13(6): e15976. DOI 10.7759/cureus.15976 2 of 4
Despite we did not fully evaluate the immune sufficiency of our patient, we consider the patient as
immunocompetent. Our patient was HIV negative, did not report underlying diseases or medication while
his medical history did not reveal recurrent infections or opportunistic infections. Besides follow-up,
laboratory parameters, including the number of patient white blood cell populations, returned to normal
levels. In a study that aimed to develop an algorithm for the detection of immunocompromised patients with
severe sepsis, patients were classified based on chart review as having or not an immunosuppressive
condition. This algorithm detected immunocompromised patients in over 90% [7]. Our patient received
treatment with dexamethasone to prevent COVID-19 immunopathology. According to existing data, it does
not seem that dexamethasone at this dose and duration of treatment associated with immune complications
[8].
The overuse of broad-spectrum antibiotics is a potential key factor in the development of secondary
bacterial infections in patients with COVID-19, as it alters the gut and pulmonary microbiome and disrupts
the gut-lung axis. This reduces the bacterial populations that are beneficial for the host's innate immunity
and limits the action of the gut microbiome in enhancing host immunity [9]. In this way, it creates an
environment that favors the growth of resistant microorganisms to these antibiotics, which in combination
with the immune dysregulation of patients with COVID-19, can lead to bacterial superinfection [10].
Bordetella bronchiseptica has reduced susceptibility to cephalosporins, as low membrane permeability of the
pathogen prevents antibiotics from entering intact cells [11]. Although Bordetella bronchiseptica is usually
susceptible to piperacillin / tazobactam, genes such as BOR-1 have been identified as responsible for
hydrolysis of B-lactams [12]. In previous case reports, azithromycin has been used effectively to treat
respiratory infections by Bordetella bronchiseptica [1]. The failure of treatment with azithromycin in our
patient is probably due to the pharmacokinetic properties of the antibiotic, as the concentrations of
azithromycin in tissues such as the lung, are much higher than those in plasma [13].
Conclusions
We reported a case of bacteremia from Bordetella bronchiseptica in a patient being treated for COVID-19.
Although the incidence of bacterial infections is relatively low, dysregulation of the immune response and
complications caused by SARS-CoV-2 in combination with overuse of broad-spectrum antibiotics can lead to
secondary bacterial infections from opportunistic pathogens even in immunocompetent patients. Although
there is no specific laboratory sign, an increased neutrophils-lymphocytes-ratio can lead to a high index of
suspicion for coinfection among COVID-19 patients. The intrinsic resistance of Bordetella bronchiseptica to
B-lactams and the pharmacokinetics of azithromycin complicated the patient's clinical course.
Additional Information
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In
compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services
info: All authors have declared that no financial support was received from any organization for the
submitted work. Financial relationships: All authors have declared that they have no financial
relationships at present or within the previous three years with any organizations that might have an
interest in the submitted work. Other relationships: All authors have declared that there are no other
relationships or activities that could appear to have influenced the submitted work.
References
1. Nagarakanti S, Bishburg E: Coinfection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
and Bordetella bronchiseptica pneumonia in a renal transplant patient. Cureus. 2021, 13:e13113.
10.7759/cureus.13113
2. Matic NA, Bunce PE: Isolation of Bordetella bronchiseptica from blood and a pancreatic abscess . J Clin
Microbiol. 2015, 53:1778-1780. 10.1128/JCM.00175-15
3. Gueirard P, Bassinet L, Bonne I, Prevost MC, Guiso N: Ultrastructural analysis of the interactions between
Bordetella pertussis, Bordetella parapertussis and Bordetella bronchiseptica and human tracheal epithelial
cells. Microb Pathog. 2005, 38:41-46. 10.1016/j.micpath.2004.08.003
4. Langford BJ, So M, Raybardhan S, et al.: Bacterial co-infection and secondary infection in patients with
COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020, 26:1622-1629.
10.1016/j.cmi.2020.07.016
5. Yan X, Li F, Wang X, et al.: Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients
with coronavirus disease 2019: a retrospective cross-sectional study. J Med Virol. 2020, 92:2573-2581.
10.1002/jmv.26061
6. Fisher A, Srikusalanukul W, Fisher L, Smith P: The neutrophil to lymphocyte ratio on admission and short-
term outcomes in orthogeriatric patients. Int J Med Sci. 2016, 13:588-602. 10.7150/ijms.15445
7. Greenberg JA, Hohmann SF, Hall JB, Kress JP, David MZ: Validation of a method to identify
immunocompromised patients with severe sepsis in administrative databases. Ann Am Thorac Soc. 2016,
13:253-258. 10.1513/AnnalsATS.201507-415BC
8. Cain DW, Cidlowski JA: After 62 years of regulating immunity, dexamethasone meets COVID-19 . Nat Rev
Immunol. 2020, 20:587-588. 10.1038/s41577-020-00421-x
9. Zhang D, Li S, Wang N, Tan HY, Zhang Z, Feng Y: The cross-talk between gut microbiota and lungs in
2021 Papantoniou et al. Cureus 13(6): e15976. DOI 10.7759/cureus.15976 3 of 4
common lung diseases. Front Microbiol. 2020, 11:301. 10.3389/fmicb.2020.00301
10. Clancy CJ, Nguyen MH: Coronavirus disease 2019, superinfections, and antimicrobial development: what
can we expect?. Clin Infect Dis. 2020, 71:2736-2743. 10.1093/cid/ciaa524
11. Kadlec K, Wiegand I, Kehrenberg C, Schwarz S: Studies on the mechanisms of beta-lactam resistance in
Bordetella bronchiseptica. J Antimicrob Chemother. 2007, 59:396-402. 10.1093/jac/dkl515
12. Lartigue MF, Poirel L, Fortineau N, Nordmann P: Chromosome-borne class A BOR-1 beta-Lactamase of
Bordetella bronchiseptica and Bordetella parapertussis. Antimicrob Agents Chemother. 2005, 49:2565-2567.
10.1128/AAC.49.6.2565-2567.2005
13. Foulds G, Shepard RM, Johnson RB: The pharmacokinetics of azithromycin in human serum and tissues . J
Antimicrob Chemother. 1990, 25:73-82. 10.1093/jac/25.suppl_a.73
2021 Papantoniou et al. Cureus 13(6): e15976. DOI 10.7759/cureus.15976 4 of 4
You might also like
- 1 s2.0 S1156523321000585 MainDocument4 pages1 s2.0 S1156523321000585 MainAna PerfeitoNo ratings yet
- Bronchoscopy in Critically Ill COVID-19 Patients - Findings, Microbiological Profile, and CoinfectionDocument5 pagesBronchoscopy in Critically Ill COVID-19 Patients - Findings, Microbiological Profile, and CoinfectionJeisson Osorio TrujilloNo ratings yet
- Early Hydroxychloroquine and Azithromycin As Combined Therapy For COVID-19: A Case SeriesDocument8 pagesEarly Hydroxychloroquine and Azithromycin As Combined Therapy For COVID-19: A Case SeriesTasya OktavianiNo ratings yet
- Annals of Medicine and Surgery: Muhammad Anis Baskara, Firdian Makrufardi, Ardiana DinisariDocument4 pagesAnnals of Medicine and Surgery: Muhammad Anis Baskara, Firdian Makrufardi, Ardiana Dinisarialfan MaulanaNo ratings yet
- CR Taghizadieh2020Document3 pagesCR Taghizadieh2020Marj MendezNo ratings yet
- PDE3 Inhibitor Enoximone Prevented Mechanical Ventilation in Patients With SARS CoV 2 PneumoniaDocument13 pagesPDE3 Inhibitor Enoximone Prevented Mechanical Ventilation in Patients With SARS CoV 2 PneumoniaDoménica SánchezNo ratings yet
- TCM-08-2020 TCM and COVID-19-4Document68 pagesTCM-08-2020 TCM and COVID-19-4Brian LiNo ratings yet
- Caso Clínico 1Document9 pagesCaso Clínico 1Rodrigo Jesús Alejandro Abanto SánchezNo ratings yet
- Rapid Onset Honeycombing Fibrosis Covid 19Document3 pagesRapid Onset Honeycombing Fibrosis Covid 19JimmyNo ratings yet
- Explore: Shuo-Wen Hung, Yuan-Ching Liao, I-Chang Chi, Ting-Yen Lin, Yu-Chuan Lin, Hung-Jen Lin, Sheng-Teng HuangDocument6 pagesExplore: Shuo-Wen Hung, Yuan-Ching Liao, I-Chang Chi, Ting-Yen Lin, Yu-Chuan Lin, Hung-Jen Lin, Sheng-Teng HuangJOHNNo ratings yet
- Comprehensive Treatment COVID 19Document49 pagesComprehensive Treatment COVID 19ekoNo ratings yet
- Jurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthDocument6 pagesJurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthAimar rfNo ratings yet
- High-Dose Intravenous Immunoglobulin As A Therapeutic Option For Deteriorating Patients With Coronavirus Disease 2019Document6 pagesHigh-Dose Intravenous Immunoglobulin As A Therapeutic Option For Deteriorating Patients With Coronavirus Disease 2019my accountNo ratings yet
- Fmed 09 841506 PDFDocument8 pagesFmed 09 841506 PDFPande Agung MahariskiNo ratings yet
- The Active Lung Microbiota Landscape of COVID-19 Patients Through The Metatranscriptome Data AnalysisDocument8 pagesThe Active Lung Microbiota Landscape of COVID-19 Patients Through The Metatranscriptome Data AnalysisEdgar VázquezNo ratings yet
- Ijcp 14728Document6 pagesIjcp 14728tayibe balNo ratings yet
- SARS CoV 2 and Dengue Virus Coinfection in An Adult With Beta Thala 2021 HelDocument7 pagesSARS CoV 2 and Dengue Virus Coinfection in An Adult With Beta Thala 2021 HelMichael John AguilarNo ratings yet
- Bacterial Co-Infections and Antibiotic Resistance in Patients With COVID-19Document6 pagesBacterial Co-Infections and Antibiotic Resistance in Patients With COVID-19gwenn satunyaNo ratings yet
- 04 OFIDHighdose IVIGasatherapeuticoptionDocument7 pages04 OFIDHighdose IVIGasatherapeuticoptionmy accountNo ratings yet
- 691-Article Text-2643-3-10-20200709Document5 pages691-Article Text-2643-3-10-20200709Sharan SahotaNo ratings yet
- Prof. Bakta - VTE in Covid-19 PAPDI BALIDocument44 pagesProf. Bakta - VTE in Covid-19 PAPDI BALIClarissa HartawanNo ratings yet
- Clinical Epidemiology and Global HealthDocument9 pagesClinical Epidemiology and Global HealthHendri YantoNo ratings yet
- Covid TreatmentDocument10 pagesCovid TreatmentkanazNo ratings yet
- AACE Clinical Case Reports: Manthan Pandya, MD, Geethika Thota, MD, Xiangbing Wang, MD, Hongxiu Luo, MDDocument3 pagesAACE Clinical Case Reports: Manthan Pandya, MD, Geethika Thota, MD, Xiangbing Wang, MD, Hongxiu Luo, MDSameerNo ratings yet
- E71 FullDocument6 pagesE71 FullRenato MiguelNo ratings yet
- Fmed 08 671215Document8 pagesFmed 08 671215Jimmy PrayogiNo ratings yet
- Mesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticsDocument13 pagesMesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticswiwiNo ratings yet
- 1 s2.0 S2590041221000039 MainDocument2 pages1 s2.0 S2590041221000039 MainMa No LoNo ratings yet
- Comparison of Efficacy of Dexamethasone and Methylprednisolone in Improving Pao2/Fio2 Ratio Among Covid-19 PatientsDocument7 pagesComparison of Efficacy of Dexamethasone and Methylprednisolone in Improving Pao2/Fio2 Ratio Among Covid-19 PatientsNivedanSahayNo ratings yet
- 1 s2.0 S1930043320306208 MainDocument3 pages1 s2.0 S1930043320306208 MainRivaldy BobihuNo ratings yet
- Pneumocystis Carinii Carriage in Immunocompetent Patients WithDocument2 pagesPneumocystis Carinii Carriage in Immunocompetent Patients WithEmanuele StirpeNo ratings yet
- TCMDocument10 pagesTCM1122GNo ratings yet
- Journal of Infection and Public Health: Burcin Agridag Ucpinar, Cennet Sahin, Ugur YancDocument3 pagesJournal of Infection and Public Health: Burcin Agridag Ucpinar, Cennet Sahin, Ugur YancLISA 102012307No ratings yet
- Corona Virus Disease 2019, DHF and The Clinical SimilarityDocument3 pagesCorona Virus Disease 2019, DHF and The Clinical Similarityketut suryanaNo ratings yet
- Pathogens 12 00944Document16 pagesPathogens 12 00944Iuliana SoldanescuNo ratings yet
- Clinical Differences Between COVID-19 and A COVID-Like SyndromeDocument7 pagesClinical Differences Between COVID-19 and A COVID-Like SyndromeSharon GabrielNo ratings yet
- Gopalaswamy y Subbian - 2021 - Corticosteroids For COVID-19 Therapy Potential ImDocument18 pagesGopalaswamy y Subbian - 2021 - Corticosteroids For COVID-19 Therapy Potential ImOsmar SulcaNo ratings yet
- Bulletin PDF (2) : Journal of College of Physicians and Surgeons Pakistan November 2020Document4 pagesBulletin PDF (2) : Journal of College of Physicians and Surgeons Pakistan November 2020Juan Carlos PatiñoNo ratings yet
- DR Irawaty CAP MANAGEMENT UPDATE BASED ON NEW GUIDELINESDocument35 pagesDR Irawaty CAP MANAGEMENT UPDATE BASED ON NEW GUIDELINESKornelis AribowoNo ratings yet
- The Clinical and Chest CT Features Associated With Severe and Critical COVID-19 PneumoniaDocument5 pagesThe Clinical and Chest CT Features Associated With Severe and Critical COVID-19 PneumoniaNadanNadhifahNo ratings yet
- Biomedicine & Pharmacotherapy: SciencedirectDocument10 pagesBiomedicine & Pharmacotherapy: SciencedirectCamilo Andrés CastroNo ratings yet
- Covide 19Document12 pagesCovide 19Hamza MehalliNo ratings yet
- 2021 Article 5829Document11 pages2021 Article 5829Demian HerreraNo ratings yet
- Phytochemicals A Novel Approach For The Management of Coronavirus Disease 2019Document13 pagesPhytochemicals A Novel Approach For The Management of Coronavirus Disease 2019vinayNo ratings yet
- Montelukast in COVIDDocument7 pagesMontelukast in COVIDGolam JILANI Mahbubay AlamNo ratings yet
- PEMPHIGUSDocument15 pagesPEMPHIGUSFritz DecendarioNo ratings yet
- Management Booklet Coronavirus Disease MOHP - 2019 - 28marchDocument22 pagesManagement Booklet Coronavirus Disease MOHP - 2019 - 28marchSanaa SbdelghanyNo ratings yet
- Advances and Challenges in The Prevention and Treatment of COVID-19Document8 pagesAdvances and Challenges in The Prevention and Treatment of COVID-19RoyNo ratings yet
- Bacterial and Viral Infection in Patients Hospitalized For Acute Exacerbation of Chronic Obstructive Pulmonary Disease Implication For Antimicrobial-1Document10 pagesBacterial and Viral Infection in Patients Hospitalized For Acute Exacerbation of Chronic Obstructive Pulmonary Disease Implication For Antimicrobial-1Ayu SusiyanthiNo ratings yet
- ccr3 4071Document3 pagesccr3 4071helamahjoubmounirdmoNo ratings yet
- Int J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaDocument12 pagesInt J Clinical Practice - 2021 - Acat - Comparison of Pirfenidone and Corticosteroid Treatments at The COVID 19 PneumoniaRebeca EscutiaNo ratings yet
- PGI Sarip - Covid 19Document92 pagesPGI Sarip - Covid 19Junayyah Abdullah SaripNo ratings yet
- Management Booklet Coronavirus Disease 2019 - 28marchDocument22 pagesManagement Booklet Coronavirus Disease 2019 - 28marchEzz123456789No ratings yet
- Células B e COVID-19Document7 pagesCélulas B e COVID-19MarianaLopesLeãoNo ratings yet
- An Update On Current Therapeutic Drugs Treating COVID-19Document15 pagesAn Update On Current Therapeutic Drugs Treating COVID-19Mijail Marcelo Callisaya VillacortaNo ratings yet
- Valente Acosta2020Document4 pagesValente Acosta2020Andres TameNo ratings yet
- Clinmed 2020-0351 FullDocument4 pagesClinmed 2020-0351 FullIsro AlhaqiNo ratings yet
- Does Amantadine Have A Protective Effect Against CDocument3 pagesDoes Amantadine Have A Protective Effect Against CAleksandra MarciniakNo ratings yet
- Covid 19 NsaidDocument5 pagesCovid 19 Nsaidsstefan888No ratings yet
- History of Spinal Disorders: Philipp Gruber, Thomas BoeniDocument2 pagesHistory of Spinal Disorders: Philipp Gruber, Thomas BoeniVictor CristianNo ratings yet
- Levetiracetam (Keppra®) in SarcinaDocument2 pagesLevetiracetam (Keppra®) in SarcinaI.m. DanielNo ratings yet
- Potters Ballotini Glass Beads SDSDocument4 pagesPotters Ballotini Glass Beads SDSTibor AngeloNo ratings yet
- Persuasive Essay PDFDocument5 pagesPersuasive Essay PDFapi-603689898No ratings yet
- Building A Resilient Workforce. Opportunities For The Department of Homeland Security Workshop Summary PDFDocument249 pagesBuilding A Resilient Workforce. Opportunities For The Department of Homeland Security Workshop Summary PDFKrloz Zaid SetnarodNo ratings yet
- Mental Health Recovery Summit: FacultyDocument2 pagesMental Health Recovery Summit: Facultyapi-281479373No ratings yet
- Bi Support Groups1Document6 pagesBi Support Groups1api-301357752No ratings yet
- HANDOUT 5 - HEALTH PROMOTION, HEALTH MAINTENANCE and HEALTH CONSIDERATIONSDocument2 pagesHANDOUT 5 - HEALTH PROMOTION, HEALTH MAINTENANCE and HEALTH CONSIDERATIONSkaycelyn jimenez100% (1)
- Kuhs Thesis 2014Document5 pagesKuhs Thesis 2014juliejensenrochester100% (2)
- Construction Style QuestionsDocument4 pagesConstruction Style QuestionsNikki DarlingNo ratings yet
- Homeless Pocket Resource Guide 06.29.2022 UpdatedDocument2 pagesHomeless Pocket Resource Guide 06.29.2022 UpdatedReferee JohannesNo ratings yet
- Running Head: Mass Incarceration and Politics 1Document16 pagesRunning Head: Mass Incarceration and Politics 1kimoda freelancerNo ratings yet
- Title: Mock Drill: Hyderabad Chemical Products LimitedDocument4 pagesTitle: Mock Drill: Hyderabad Chemical Products Limitedakshay arya100% (1)
- Novel Drug Delivery SystemsDocument3 pagesNovel Drug Delivery SystemsSanketraje JadhavNo ratings yet
- Kuesioner Ndi PDFDocument4 pagesKuesioner Ndi PDFeloooyiyNo ratings yet
- 5 Elements of Abdominal DiagnosisDocument14 pages5 Elements of Abdominal Diagnosiscelliastt100% (4)
- Dissertation Topics MidwiferyDocument4 pagesDissertation Topics MidwiferyCustomizedWritingPaperNewark100% (1)
- Employee Benefits Whitepaper BambooHRDocument17 pagesEmployee Benefits Whitepaper BambooHRMuhammad SaadNo ratings yet
- Adult Obesity ResearchDocument19 pagesAdult Obesity Researchchoraz100% (1)
- Lawsuit Against DeWine, Ohio Over Coronavirus RestrictionsDocument56 pagesLawsuit Against DeWine, Ohio Over Coronavirus RestrictionsJo InglesNo ratings yet
- R Reeggaarrddiinngg Tthhee Eexxaam Miinnaattiioonn: GDD ? H@Qka A9Fk KMJ? GFK H9Cakl9FDocument2 pagesR Reeggaarrddiinngg Tthhee Eexxaam Miinnaattiioonn: GDD ? H@Qka A9Fk KMJ? GFK H9Cakl9FAbdullah BangwarNo ratings yet
- Preeclampsia - Management and Prognosis - UpToDateDocument22 pagesPreeclampsia - Management and Prognosis - UpToDateNunung firda IstiqomahNo ratings yet
- топик a visit to a dentistDocument2 pagesтопик a visit to a dentistEyeless DanteJackNo ratings yet
- Geriatric Index of Comorbidity: Validation and Comparison With Other Measures of ComorbidityDocument9 pagesGeriatric Index of Comorbidity: Validation and Comparison With Other Measures of ComorbidityDesya EspriliaNo ratings yet
- HEPATOLITIASISDocument49 pagesHEPATOLITIASISFitriardi SejatiNo ratings yet
- 20190813033948amassgn. 12 Physical Edu.Document4 pages20190813033948amassgn. 12 Physical Edu.Sonica GuptaNo ratings yet
- Corn Coffee FinalDocument85 pagesCorn Coffee FinalNhelia Santos Bañaga100% (1)
- Food Related Dissertation TopicsDocument6 pagesFood Related Dissertation TopicsPaperWritingServicesLegitimateCanada100% (1)
- Risk Assessment Template - HouseDocument3 pagesRisk Assessment Template - HouseSean SpencerNo ratings yet
- Year Planner TemplateDocument2 pagesYear Planner TemplateSimon DzokotoNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (31)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (60)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)