Professional Documents
Culture Documents
Á1823ñ POSITRON EMISSION TOMOGRAPHY DRUGS-INFORMATION
Uploaded by
isabelclimaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Á1823ñ POSITRON EMISSION TOMOGRAPHY DRUGS-INFORMATION
Uploaded by
isabelclimaCopyright:
Available Formats
Accessed from 200.136.52.
120 by lear5 on Thu May 17 09:29:58 EDT 2018
8098 á1821ñ / General Information USP 41
Radiopharmaceutical (radiopharmaceutical preparation/radioactive drug): A finished dosage form that contains a radioac-
tive substance in association with one or more other ingredients and that is intended to diagnose, stage a disease, monitor
treatment, or provide therapy. A radiopharmaceutical includes any nonradioactive reagent kit or radionuclide generator that is
intended to be used in the preparation of any such substance. The terms radiopharmaceutical and radioactive drug are com-
monly used interchangeably.
Scintillation crystal counter: An instrument consisting of a crystal scintillator, such as NaI(Tl), with an attached photomulti-
plier tube and associated electronics. Scintillation light produced from the absorption of gamma and X-rays in the crystal is
converted to electrons and amplified in the photomultiplier tube. The resultant current pulse may be further analyzed with
regard to photon energy. A commonly used form of this instrument that has a hole in the crystal of sufficient size to allow
placement of a test tube or similar container is known as a well counter.
Semiconductor detector: An instrument consisting of a semiconductor material, such as silicon or germanium crystals, that
detects ionizing radiation through generation of charge carriers (passage of electrons through holes). The current pulse pro-
duced by migration of these charge carriers, under the influence of a voltage potential across the material, can be further am-
plified and analyzed to determine the quantity and energy of the incident radiation.
Solid-state detector: A crystal-based detector, in contrast to a gas-based detector; often is used as a synonym for a semicon-
ductor detector.
Specific activity: The radioactivity of a radionuclide per unit mass of the element or compound. The unit of specific activity is
radioactivity per mass expressed on a gram or mole basis [e.g., mCi/mg (MBq/mg); Ci/mmol (GBq/mmol)].
Strength: The radioactivity concentration of the radiopharmaceutical at the calibration time. The unit of strength is the
amount of radioactivity on a volume basis (e.g., mCi/mL or MBq/mL).
Total radioactivity: The radioactivity of the radionuclide, expressed per unit (e.g., vial, capsule, ampule, generator, and oth-
ers) at the calibration time.
Validation: Establishment of documented evidence that a method, process, or system meets its intended requirements.
Verification: Confirmation that an established method, process, or system meets predetermined acceptance criteria.
X-rays: A type of electromagnetic radiation emitted from the electron orbitals. Although they do not arise from the nucleus,
they are often present immediately after a decay event if there are interactions between the emitted radiation and the orbital
electrons.
REFERENCES
American Society for Testing and Materials (ASTM). Active Standard ASTM D3648. Standard practices for the measure-
ment of radioactivity. West Conshohocken, PA: ASTM International; 2011.
American Association of Physicists in Medicine (AAPM). AAPM Report No. 181. The selection, use, calibration, and quality
assurance of radionuclide calibrators used in nuclear medicine. College Park, MD: AAPM; June 2012.
á1823ñ POSITRON EMISSION TOMOGRAPHY DRUGS—INFORMATION
1. INTRODUCTION
2. TECHNIQUES FOR PRODUCTION AND QUALITY CONTROL
3. QUALITY ASSURANCE
General Chapters
3.1 Reagents and Materials
3.2 Change Control
3.3 Validation
4. PRODUCTION
4.1 Equipment for Manual Synthesis
4.2 Equipment for Automated Synthesis
5. QUALITY CONTROL
5.1 Quality Control Sampling
5.2 Reference Standards
5.3 Conditional Release
5.4 Out-of-Specification Results
6. ANALYTICAL METHODOLOGIES
6.1 Thin-Layer Chromatography
6.2 Gas Chromatography
6.3 High-Performance Liquid Chromatography
6.4 Radiation Detectors Used in Chromatographic Techniques
6.5 Multichannel Analyzer
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
USP 41 General Information / á1823ñ 8099
6.6 Ionization Chamber
7. QUALITY ATTRIBUTES
7.1 Appearance
7.2 pH
7.3 Total Radioactivity and Strength
7.4 Radionuclidic Identity
7.5 Radionuclidic Purity
7.6 Radiochemical Identity and Purity
7.7 Chemical Purity
7.8 Total Mass of the Active Pharmaceutical Ingredient and Specific Activity
7.9 Bacterial Endotoxin
7.10 Sterility
8. STERILITY ASSURANCE
8.1 Sterile Membrane Filtration
8.2 Aseptic Techniques
8.3 Presterilized Components
8.4 Environmental Controls
8.5 Media Fills
8.6 Suitability of Media
8.7 Suitability of the Sterility Test Method
8.8 Membrane Filter Integrity Test
8.9 Operator Training and Qualification
9. LABELING
GLOSSARY
1. INTRODUCTION
Positron emission tomography (PET) drugs contain radionuclides that undergo nuclear transformation, or radioactive decay,
predominantly by the emission of a positron. Positrons undergo annihilation upon interaction with electrons to produce two
photons that are emitted in nearly opposite directions to each other. Each photon possesses an energy of 511 keV, which lies
in the gamma ray portion of the electromagnetic spectrum. These radionuclides are used in a wide range of PET imaging stud-
ies, including research, investigational, and clinical applications.
The radionuclides used in PET imaging studies typically possess short physical half-lives (denoted as T1/2). Some common
examples of PET radionuclides and their associated half-lives are included in Table 1. Note that Table 1 includes radionuclides
currently in predominant use and is not intended to illustrate all positron-emitting radionuclides used in PET.
Table 1
PET Radionuclide Half-Life, T1/2
Fluorine-18 109.8 min
Carbon-11 20.4 min
Nitrogen-13 10.0 min
Oxygen-15 2.0 min
Copper-64 12.7 h
General Chapters
Gallium-68 68 min
Rubidium-82 75 s
Because certain of these radionuclides such as Carbon-11 and Nitrogen-13 when found in biological systems have the same
chemical and physical properties as their stable counterparts found in biological systems, PET offers a unique platform for in
vivo imaging studies of complex biochemical pathways. As a result, PET radionuclides have found widespread use in cardiolo-
gy, oncology, and neurology applications. PET drugs have also attracted interest as potential tools to accelerate and reduce
the cost of therapeutic drug discovery efforts.
Most PET radionuclides are produced at the point of use by a particle accelerator (e.g., a cyclotron) or a radionuclide gener-
ator. A cyclotron accelerates charged particles such as protons or deuterons to velocities sufficient to induce a nuclear transfor-
mation of the target nucleus into a different element. High-energy particles and/or radiation are emitted from the target nu-
cleus during the transformation process. An example of a transformation is the bombardment of stable Oxygen-18 nuclei with
accelerated protons to produce Fluorine-18 nuclei along with the concomitant emission of a neutron. This process may be
summarized according to the following shorthand notation:
18O(p,n)18F
The chemical form and physical state of the bombarded nuclei vary, depending on the target and the subsequent usage of
the PET radionuclide. This allows the production of PET radionuclides in gaseous, solid, and solution phases.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
8100 á1823ñ / General Information USP 41
Radionuclide generators offer an alternative method for point-of-use access to some PET radionuclides. A radionuclide gener-
ator contains an immobilized parent radionuclide that undergoes radioactive decay to a daughter radionuclide, which may be
eluted from the generator. An example of a PET radionuclide generator is the Germanium-68/Gallium-68 generator. The pa-
rent Germanium-68 (T1/2 = 271 days) is adsorbed onto the column packing material. The Germanium-68 undergoes radioac-
tive decay by electron capture into Gallium-68, which is not adsorbed onto the column packing material and may be eluted
from the generator.
Regardless of the production method, other radionuclides may be present in addition to the desired PET radionuclide. In the
case of cyclotron-produced PET radionuclides, other radionuclides may result from the bombardment of the target holder
and/or other nuclei present in the target material. For generator-produced PET radionuclides, break-through of the parent ra-
dionuclide may occur. Safeguards are readily available to avoid unnecessary contamination with radionuclidic impurities of the
final PET drug.
Once the PET radionuclide has been produced, it should be processed into a suitable form of a PET drug. The simplest form
of processing involves the purification and/or formulation of the PET radionuclide. An example is the purification of the [18F]flu-
oride ion. After production of the [18F]fluoride ion by cyclotron bombardment, ion exchange procedures may be used to re-
move impurities and yield a formulation suitable for PET imaging studies. Another example is the purification of gaseous
[15O]oxygen through various solid supports before administration of the finished PET drug by inhalation.
Simple forms of processing are rare, because PET drug products are typically synthesized from the appropriate radionuclide
through multiple synthetic processing steps. The exact process depends on the desired PET drug. The synthesis of 2-[18F]fluo-
ro-2-deoxyglucose ([18F]FDG) provides an illustration. The first step in this synthesis is the preparation of the anhydrous [18F]flu-
oride ion from cyclotron-produced Fluorine-18. The [18F]fluoride ion is activated with a phase transfer catalyst such as tetrae-
thylammonium or [2.2.2]-cryptand to enhance its reactivity toward nucleophilic substitution. The resulting complex reacts
with mannose triflate to yield a fluorinated 18F intermediate, which is deprotected and purified to yield [18F]FDG. This process is
summarized in the following set of equations:
In addition to the chemical processing and/or purification steps used to generate the desired radiochemical of interest, other
steps are typically required to formulate the PET drug product. For injectable PET drug products, formulation steps may in-
clude dilution, addition of a stabilizer, pH adjustment, and other steps. The final formulation of the PET drug product should
take place in a manner that minimizes the presence of bacterial endotoxins and bioburden. Finally, the product should be
sterilized (e.g., by passage through a membrane sterilizing filter) to provide a solution suitable for intravenous administration.
In the above example, [18F]FDG becomes the drug product Fludeoxyglucose F 18 Injection.
Before use, the finished PET drug product should be tested to ensure that the product meets suitable standards of identity,
strength, quality, and purity. Because of the short half-life of PET radionuclides, testing should be completed in a timely fash-
General Chapters
ion; however, it is not possible to complete certain quality control (QC) tests within a suitable timeframe. In some cases, it may
be necessary to adopt a “sub-batch” approach for QC testing, wherein a sub-batch of the PET drug product is prepared solely
for purposes of QC testing. Examples of PET drug products with such short half-lives include [15O]water and [13N]ammonia.
Ultimately, the short half-lives of PET radionuclides create unique constraints for the production and testing of PET drug
products and define how these products are used in research, investigational, and clinical settings. PET drugs are a unique class
of products defined by the following characteristics:
• The mass of the radioactive ingredient in a PET drug product usually ranges from nanogram to microgram quantities. This
affects pharmacological and toxicological considerations for PET drugs, usually by creating large safety margins due to
low mass of the active ingredient in the administered dose.
• An entire batch of a PET drug product may be contained in a single vial. Samples withdrawn for QC testing are represen-
tative of the entire batch. PET drug products produced in this fashion undergo 100% QC testing.
• PET drug products are produced and handled in environments with overlapping areas of regulatory authority. For exam-
ple, a site may be subject to requirements of any combination of the following authorities: Nuclear Regulatory Commis-
sion or Agreement State Agency, Food and Drug Administration, Environmental Protection Agency, occupational safety
entities, etc. These agencies may have different and conflicting requirements of the manufacturing facility, some through
regulation, some through guidelines published by the authorities, and some through license commitments made by the
facility.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
USP 41 General Information / á1823ñ 8101
• PET drug products are generally produced at or near their point of use in small-scale facilities with limited personnel and
resources. This requires:
• Allowance for multiple operations in one area with adequate controls
• Allowance for making and testing multiple PET drug products using shared equipment with appropriate cleaning be-
tween batches
• Appropriate requirements for aseptic operations
• Appropriate requirements for system suitability and other day-of-use activities
• Appropriate QC requirements for components, materials, and supplies
• Self-verification of significant steps in radionuclide production, PET drug production, compounding, and testing
• Single-person oversight of production or compounding, testing, review of batch records, and release authorization
• PET drug products do not enter a traditional distribution chain. Instead, PET drug products require just-in-time deliveries
typically performed by dedicated carriers with experience in handling radioactive materials.
• It is not possible to complete sterility testing for PET drug products before their use. Therefore, considerations are made to
provide for the assurance of sterility for injectable PET drugs intended for human use.
• Procedures should be in place to notify the responsible individuals in a timely manner if a PET drug product is found to be
in noncompliance after release for human use.
2. TECHNIQUES FOR PRODUCTION AND QUALITY CONTROL
The unique characteristics of PET drug products play a large role in the choice of instrumentation and techniques used in
production and QC testing. Production techniques and analytical methods should be efficient and rapid. The selection of tech-
niques and methods is also strongly influenced by the development stage of the PET drug. For example, early development
efforts focus on radiolabeling, purification, QC methods development, and others. These efforts are designed to support the
usage of the PET drug for in vitro studies, animal studies, and may even include first-in-human studies. At this stage, relatively
small quantities of the PET drug are required at a limited number of institutions or geographic areas. Manual production tech-
niques or semi-automated equipment may provide sufficient quantities to meet this demand. Analytical methods should also
be suitable for the usage of the PET drug at the early stages of development. Typically, method development efforts focus on
accuracy, precision, and linearity. Before the use of injectable PET drugs in human studies, provisions are made to ensure that
bacterial endotoxins are controlled at suitable levels and that the product is sterile.
In later development stages, larger quantities of the PET drug may be required in more geographic areas. At this point, the
synthesis, purification, and testing of the PET drug product should be well defined to support clinical trials. Development ef-
forts at this stage typically focus on optimization and reliability of the production process. Manual production techniques are
rarely used. Instead, semi-automated or fully automated techniques are typically required to provide sufficient quantities of the
PET drug at multiple geographic locations. This approach simultaneously assures consistent quality attributes of the PET drug
at multiple production facilities and minimizes radiation exposure of operators. Method development activities at this stage
focus on specificity, ruggedness, robustness, and other characteristics required to support QC testing of the PET drug at multi-
ple geographic locations.
Finally, at the commercial stage of production, semi-automated or fully automated techniques and equipment may be re-
quired to provide sufficient quantities of the PET drug in numerous geographic areas. Production techniques and analytical
methods for commercial PET drug products should be well defined and adequately described in the appropriate marketing
authorization.
Not all PET drugs are intended to advance through the various development stages from in vitro studies, to animal studies,
to clinical trials, to commercial production. For example, a PET drug product may be produced at several institutions for re-
General Chapters
search purposes without the intention of commercialization. In other instances, a PET drug product may be Food and Drug
Administration (FDA) approved but is only available in a single geographic area. These factors often result in different strategies
for production techniques, analytical methodologies, and the underlying studies and documentation to support these strat-
egies.
3. QUALITY ASSURANCE
The goal of quality assurance (QA) is to ensure that the techniques and equipment used in production and testing result in a
product that meets established standards for that specific PET drug product. The QA program should be sufficient to establish
the reliability and suitability of the techniques and equipment as appropriate to the development stage of the PET drug prod-
uct. The following topics should be considered in a QA program.
3.1 Reagents and Materials
Reagents and materials used in the synthesis and testing of a PET drug product should conform to established acceptance
criteria. Procedures for procuring, receiving, testing, storage, and use of reagents and materials should also be considered. An
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
8102 á1823ñ / General Information USP 41
audit trail may be established for the traceability of specific lots of reagents and materials to specific batches of product. These
acceptance criteria, procedures, and the audit trail should be appropriate for the development stage of the PET drug product.
3.2 Change Control
Changes in the synthesis and test methods should be evaluated for their potential for altering the product quality and be
approved in advance through established procedures. If the resultant PET drug product does not meet the criteria appropriate
to the development stage, the process change is unacceptable. Acceptable changes should be appropriately documented.
3.3 Validation
Production and analytical test methods should be validated at a level that is appropriate for the development stage of the
PET drug product. Validation of the production process should result in a process that is reliable and consistent. Analytical
method validation demonstrates that a method can quantitatively measure a PET drug product reliably and reproducibly. It is
not necessary to validate analytical methods that are described in USP compendia. The emphasis on validation typically increa-
ses as the PET drug product moves through the development stages toward commercialization. Validation of the computer
software used to control automated production equipment should also be considered as appropriate.
QUALIFICATION
Equipment used in the synthesis and testing of PET drug products should be qualified as appropriate for the development
stage of the PET drug product. This may include qualification procedures (installation, operational, and performance), as well
as procedures for periodic maintenance and equipment calibration. For commercially available equipment, the equipment
vendor may be able to support qualification requirements.
STABILITY STUDIES
Stability studies should be performed on PET drug products to establish suitable storage conditions and the expiration time
and date. Quality attributes such as radiochemical purity, appearance, pH, stabilizer, preservative effectiveness, and chemical
purity should be evaluated. The frequency and extent of these studies should be appropriate for the development stage of the
PET drug product. Significant process changes require stability studies to be repeated.
4. PRODUCTION
4.1 Equipment for Manual Synthesis
Equipment intended for the manual synthesis of PET drug products may be based on apparatus found in a typical chemistry
laboratory such as glass reaction vessels, heating blocks, tubing, and other items. These items should be suitable for their in-
tended use and selected according to the needs of the process. Items that are reused and come into contact with the reactants
and/or final drug product of the synthesis should be cleaned and depyrogenated as appropriate for the use of the final prod-
uct.
Written procedures for the manual syntheses of PET drug products should contain sufficiently detailed steps to ensure that a
General Chapters
reproducible process is followed for each batch by the operator. Observations of critical process parameters should be docu-
mented as appropriate in the batch record.
4.2 Equipment for Automated Synthesis
Preparation of Fludeoxyglucose F 18 Injection and other common PET drug products can be adapted readily to automated
synthesis. The use of programmable controllers and/or computers with switches, solenoids, and sensors allows the operator to
control the sequence of steps in an automated fashion. Thus, an automated synthesis requires minimal operator intervention,
and batch-to-batch consistency is maintained with each step executed in a reproducible manner. Software may provide feed-
back to the operator such as alarm conditions, status reports, or an end-of-synthesis report. Modules for automated synthesis
may be commercially available. These modules may use individual reagents or cassettes required for the appropriate PET drug
product synthesis. The cassettes provide preassembled collections of reagents, reaction vessels, tubing, filters, and other items
necessary to produce a batch of a PET drug product.
Laboratory robots may be appropriate in situations where complex manipulations are required for the procedure, such as
the physical movement of a reaction vessel from one station to another, or the dispensing of doses from a vial into individual
syringes. Customized equipment may also be fabricated to perform a specific function in the PET drug product synthesis.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
USP 41 General Information / á1823ñ 8103
5. QUALITY CONTROL
QC tests should be designed and executed in a manner that is appropriate for PET drugs. The short half-life of PET radionu-
clides significantly limits the timeframe for the performance of QC tests, and it may not be possible to complete all QC tests
before the use of the PET drug product.
5.1 Quality Control Sampling
In most cases, the entire batch of a PET drug is contained within a single vial. The relatively small batch volume of PET drugs
limits the amount of material available for QC testing. This is different from traditional manufacturing practices, where a batch
may consist of numerous vials and not all vials are sampled for purposes of QC testing. QC sampling of PET drug products use
a larger proportion of the drug volume, and thereby offers a greater degree of assurance that quality-related problems will be
identified in the QC testing process.
5.2 Reference Standards
Reference standards are necessary to identify the API and impurities in the PET drug product. Reference standards may be
commercially available or prepared in-house. Commercial reference standards should include documentation from the supplier
to ensure they are properly characterized. The characterization and qualification of reference standards should be appropriate
for the development stage of the PET drug product.
5.3 Conditional Release
When a required QC test for a PET drug product cannot be completed because of a malfunction of test equipment, it may
be appropriate to conditionally release the batch. It is not appropriate in the absence of critical QC tests to conditionally re-
lease batches (e.g., radiochemical identity and purity). Procedures should be developed to describe the conditional release
process, including the role of historical data, other QC test results, sample retention, and other procedures.
5.4 Out-of-Specification Results
When the results of a QC test do not meet product specifications, an investigation should be conducted to determine if the
result is due to an analytical error (false positive) or if the result is due to a product failure. Because of the short half-life of PET
radionuclides, it may not be possible to conduct investigations in the same manner as in traditional drug testing laboratories.
6. ANALYTICAL METHODOLOGIES
Various analytical methodologies and chromatographic techniques may be used for the testing of PET drug products. The
most commonly used methodologies are discussed in this section for purposes of illustration. Similar principles should apply to
other methodologies not included in this section.
6.1 Thin-Layer Chromatography
General Chapters
Thin-layer chromatography (TLC) involves separation, identification, and quantification of analytes using a stationary phase
on a support or plate and a developing solvent that may also be known as mobile phase. The stationary phase may be silica or
alumina spread in a uniform layer onto a plate of glass, metal, or plastic. A small sample of the PET drug product is applied
(spotted) onto the stationary phase, and the plate is developed in a chromatographic tank. The mobile phase moves through
the stationary phase by capillary action, and the analytes are separated based on partition, ion exchange, and/or adsorption.
The retardation factor (Rf) and radiochemical purity of the PET drug on the developed plate can be determined by either
counting the developed plate on a radio–TLC scanner, or cutting the plate into pieces and counting each piece in a radiation
detector. The Rf of an analyte, under specific TLC conditions, is considered an identifying characteristic of the analyte.
6.2 Gas Chromatography
Gas chromatography (GC) involves separation, identification, and quantification of volatile analytes using a stationary phase
and a gaseous mobile phase. A small sample of the solution is introduced into the GC instrument, which vaporizes the sample
for passage over the stationary phase that is immobilized within a GC column. As the gaseous mobile phase passes over the
stationary phase, the analytes are separated based on their partition between the gas and stationary phases. A detector located
at the exit of the column provides an electronic signal to produce the gas chromatogram.
A GC instrument consists of a gas source, injection port, column, detector, and a data collection device. The injection port,
column, and detector are temperature controlled and may be varied as part of the analysis. The gas source depends on the
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
8104 á1823ñ / General Information USP 41
column and detector in use. The type of detector depends on the nature of the compounds analyzed. Typical detectors in-
clude flame ionization and thermal conductivity. In addition, radiation detectors may be used in GC analysis. Detector output
is recorded over time, and the instrument response, measured as peak area or peak height, is a function of the amount
present. The retention time of an analyte under specific GC conditions is considered an identifying characteristic. GC analysis is
most typically used to quantify residual solvents in PET drug products but may also be used to determine radiochemical and
chemical purity of the PET drug product formulation.
6.3 High-Performance Liquid Chromatography
High-performance liquid chromatography (HPLC) is an analytical technique used to separate, identify, and quantify the
components of a solution. HPLC separations are based on the interaction of the analytes between the stationary and mobile
phases, which in turn leads to the retention of the analytes. The mechanism of interaction between the analytes and stationary
phase may be partition, size exclusion, adsorption, and/or ion exchange chromatography. The retention time of an analyte
under specific HPLC conditions is considered an identifying characteristic.
HPLC instruments consist of a reservoir containing the mobile phase, a pump to force the mobile phase through the system
at high pressure, an injector to introduce the sample into the mobile phase, a chromatographic column, a detector, and a data
collection device. The type of detector used depends on the nature of the compounds analyzed. In addition to mass detectors
such as refractive index, ultraviolet, and conductivity, radiation detectors are also used in HPLC analysis. An HPLC system with
a radiation and mass detector allows the simultaneous determination of radiochemical and chemical purity, retention time,
and the subsequent identity of the PET drug product. This configuration also allows the determination of specific activity. Elu-
tion methods include gradient or isocratic methods with aqueous and/or organic buffers.
The calibration of a GC or HPLC instrument may be achieved by different means. One approach involves the creation of a
calibration curve from a range of standards with known concentrations. The calibration curve may be used over a specified
period of time for product testing. A second approach for calibration involves the creation of a single-point calibration at the
beginning of each testing cycle. The results may be averaged and used to provide a calibration factor for product testing. Re-
gardless of the approach for calibration, the tailing factor and chromatographic resolution (or column efficiency as appropri-
ate) should be determined routinely as a part of system suitability. Routine system suitability testing should include checks for
these parameters.
6.4 Radiation Detectors Used in Chromatographic Techniques
Radiation detectors used in TLC, GC, and HPLC for quantitative measurements should be calibrated when possible with suit-
able NMI-traceable radionuclide standards at appropriate frequency. Routine system suitability testing should be performed on
the radiation detection system to ensure proper operation. Because of the nature of TLC, system suitability for a radio–TLC
scanner should address uniformity, positional accuracy, detector linearity, and resolution. The calibration of radiation detectors
should be repeated as appropriate.
6.5 Multichannel Analyzer
A multichannel analyzer (MCA) is an instrument used to obtain a spectrum of gamma rays emitted by a PET radionuclide.
The key component of a MCA is an energy-sensitive detector. On the basis of the gamma spectrum of a sample, radionuclides
present in the sample may be identified and quantified. Calibration of the system is typically performed with certified stand-
ards and may involve one or more radionuclides with gamma energies and quantities that span the range of typical analyses at
General Chapters
appropriate frequency.
6.6 Ionization Chamber
An ionization chamber, often referred to as a dose calibrator, is an instrument used to measure the quantity of radioactivity
in a PET drug product. The key component of an ionization chamber is an argon-filled chamber with an applied electrical po-
tential that allows the detection of ions produced by the passage of gamma rays through the chamber. Calibration of the sys-
tem is typically performed with certified standards at appropriate frequencies and may involve one or more radionuclides with
gamma energies and quantities that span the range of typical analyses.
7. QUALITY ATTRIBUTES
Quality attributes should be defined and assessed for each PET drug. These attributes should be suitable for the intended use
of the PET drug and should also reflect the dosage form. Because most PET drug products are administered by intravenous
injection, this section focuses on quality attributes associated with injectable PET drug products. Different attributes may be
appropriate for other dosage forms. In addition, the definition and assessment of quality attributes may vary with the develop-
ment phase of the PET drug product in comparison to the final drug phase.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
USP 41 General Information / á1823ñ 8105
7.1 Appearance
Injectable PET drug products should be free of visible particulate matter. Because of the radioactive nature of PET drug prod-
ucts, the test for appearance should be a visual inspection that meets radiation safety requirements. The use of a visual stand-
ard should be considered to ensure the accuracy of appearance determinations.
7.2 pH
Injectable PET drug products should be in the pH range suitable for intravenous administration. Because of the limited vol-
ume of a PET drug product, pH measurement is typically performed using narrow-range paper strips. The use of pH standards
should be considered to ensure the accuracy of pH determinations.
7.3 Total Radioactivity and Strength
The total radioactivity of a PET drug product may be determined by an ionization chamber and should be stated at a given
date and time. From the total radioactivity and the volume of the PET drug product, the strength may be determined. The
strength of the PET drug product should be stated, along with the date and time of the determination of total radioactivity.
7.4 Radionuclidic Identity
Half-life (also referred to as approximate half-life) is a characteristic of the radionuclide that may be used for its identification.
To adequately confirm the identity of a PET radionuclide, the half-life should be measured in a suitable counting device over a
period of time appropriate to the half-life of the radionuclide.
7.5 Radionuclidic Purity
By definition, all positron-emitting radionuclides emit 511 keV gamma rays but may also emit gamma rays with different
energies. Therefore, it is generally not possible to determine the radionuclidic purity of PET drug products with a MCA. One
suitable solution to this problem is the use of validation studies to ensure the removal and/or decay of accelerator-produced
radionuclidic impurities during the production process. Other approaches may be appropriate depending on the characteris-
tics and source of the radionuclidic impurities. In addition, periodic analysis of decayed samples in routine production with a
MCA may be used to quantify radionuclidic impurities developed.
7.6 Radiochemical Identity and Purity
Depending on the physical and chemical properties of the PET drug product, the radiochemical identity and purity may be
determined by TLC, HPLC, or GC. The identity of the active pharmaceutical ingredient (API), and possibly other analytes,
should be based on the known retention time of the analyte. The simultaneous use of reference standards during sample anal-
ysis should be considered for purposes of radiochemical identification. The radiochemical purity of the PET drug product
should be determined based on the sum of all chemical forms of the radionuclide of interest. As appropriate, it should be es-
tablished during validation that all radiochemical analytes are eluting from the chromatographic system and that the radioac-
tive detector is operating within its linear range.
General Chapters
7.7 Chemical Purity
The chemical purity of the PET drug product should be assessed for the presence of volatile impurities, residual reagents
and/or precursors, and by-products. For example, residual solvents, such as acetonitrile and ethyl alcohol, may assessed by GC.
[2.2.2]-Cryptand, a common reagent used in the preparation of PET drug products, may be assessed by colorimetric techni-
ques.
7.8 Total Mass of the Active Pharmaceutical Ingredient and Specific Activity
Potential toxicity issues and pharmacological effects may be associated with the API in a PET drug product (e.g., the mass-
dependent localization of neurotransmitters or other more generalized forms of toxicity). In these instances, the total mass of
the API should be determined before use of the PET drug product. The total mass of the API contained in a patient dose should
be defined for PET drug products where mass-related localization or toxicity concerns require such assessment, which may be
determined by HPLC or GC. On the basis of the mass of the API, the specific activity may be calculated. To determine the
appropriate quality of the injected drug product in the patient dose, any two of three measured parameters (total mass, total
activity, or specific activity) are sufficient. Specific activity should be stated along with the date and time of determination.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
8106 á1823ñ / General Information USP 41
7.9 Bacterial Endotoxin
The quantity of bacterial endotoxin in an injectable PET drug product should comply with USP standards (<175 USP Endo-
toxin Units/patient dose). The test for bacterial endotoxin uses a solution of limulus amebocyte lysate (LAL). Various methods
exist for this test, including gel-clot, chromogenic, and others. Test samples should be obtained and handled in a manner that
minimizes contamination before testing. In addition, control measures should be used to ensure accurate test results without
interferences from the test solution, such as certain formulations that enhance or inhibit the interaction of LAL with bacterial
endotoxin. This effect may be corrected by dilution of the PET drug product before testing. The necessity of dilution in this test
is determined in the validation of the specific formulation of the PET drug product.
7.10 Sterility
Injectable PET drug products should be sterile. For reasons described in 1. Introduction, it is not possible to complete the
sterility test before the use of PET drug products. The test for sterility should consist of inoculating a test sample into media
capable of supporting the growth of aerobic and anaerobic microbes, which may be established with an appropriate certificate
of analysis. The test samples should be obtained and handled in a manner that minimizes contamination before testing. To
reduce radiation exposure to operators, the test samples may be allowed to decay before inoculation. The inoculation should
use techniques that minimize the potential for false positives during the sterility test. In addition, control measures should be
used to ensure accurate test results without interferences from the test solution. After inoculation, the sterility test samples
should be incubated for the appropriate period of time at the prescribed temperature. If visible growth is detected during the
incubation period, the investigator or physician should be informed in a timely manner, and an investigation should be initi-
ated to determine whether the growth was due to accidental contamination during the sample handling process or to a true
product failure. The investigation should include identification of the microbe(s) in the sterility test sample to determine the
source of the contamination. This aspect of the investigation may be limited if production and sterility test sampling occur in
the same laboratory.
8. STERILITY ASSURANCE
A suitable sterility assurance program should be established for PET drug products that are intended for intravenous injec-
tion. This section describes appropriate measures that assure the routine production of a sterile product suitable for injection.
8.1 Sterile Membrane Filtration
Injectable PET drug products are typically sterilized by passage of the solution through a sterile membrane filter into a pre-
sterilized vial. To provide the greatest assurance of sterility, the PET drug product should pass through an appropriate steriliz-
ing filter into a presterilized vial that has been assembled using aseptic techniques.
8.2 Aseptic Techniques
Critical steps that affect the sterility of the PET drug product should be identified and, where appropriate, aseptic techniques
should be used to complete these steps. Aseptic techniques should include the use of a suitable gowning, proper handling of
components, environmental controls, and others. Aseptic techniques should be described in written procedures.
General Chapters
8.3 Presterilized Components
PET drug production typically employs various components and containers that are presterilized and pyrogen free. Appropri-
ate sterile components are generally assembled aseptically in a controlled environment before use in production. Presterilized
vials and sterile diluents such as sterile water for injection or sodium chloride solution are typically used. Other sterile compo-
nents are sometimes utilized in nonsterile applications in production where a commercially available product may be useful.
An example is use of a sterile transfer line for fluid transfer prior to a sterilizing filter, where the diameter or length of a com-
mercially available sterile line is appropriate to the application.
8.4 Environmental Controls
The environment where aseptic techniques are executed should be controlled to ensure appropriate aseptic conditions.
These controls may include temperature and humidity, ventilation and air filtration, cleaning and disinfection, equipment
maintenance, proper garb, and microbiological monitoring. Air filtration standards should conform to local and/or national
standards relevant to environmental standards, for example, International Organization for Standardization (ISO) standards.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
USP 41 General Information / á1823ñ 8107
8.5 Media Fills
A media fill, also known as a “process simulation”, is the performance of an aseptic procedure using a sterile microbiological
growth medium in place of the PET drug product. The goal of a media fill is to test whether the aseptic procedure is adequate
to prevent microbiological contamination during the actual process. Media fills may be used to evaluate aseptic techniques
used in the assembly of presterilized components and to qualify operators for aseptic techniques. A media fill should be de-
signed to ensure that the simulation is representative of the aseptic manipulations performed during the actual process, includ-
ing personnel, components, gowning, locations, batch size, number of replicates, and other factors. After completing the me-
dia fill, components filled with media should be incubated appropriately to permit the growth of microbes. The use of nega-
tive controls should be considered during the media fill procedure.
8.6 Suitability of Media
Sterility test media should be tested before use to ensure that the media adequately support the growth of microbes. These
tests are typically referred to as growth-promotion tests and may be conducted in-house, by the supplier, or by a contract
laboratory. Media should be used within the manufacturer’s expiration date.
8.7 Suitability of the Sterility Test Method
The sterility test should be tested to ensure that the PET drug product is not bacteriostatic or fungistatic. The suitability of
the sterility test may be conducted in-house or by a contract laboratory.
8.8 Membrane Filter Integrity Test
To ensure the proper sterilization of the PET drug product by passage through a membrane sterilization filter, the bubble
point of the filter should be determined after completing the filtration process. The bubble point of the filter, measured in
pounds per square inch (psi), is the pressure required to force air through the pores of the wetted membrane in the device.
Other suitably validated procedures may be used.
8.9 Operator Training and Qualification
Operators involved in aseptic techniques should be trained in proper gowning, environmental controls, handling sterile
components, and other techniques. Operators should be qualified through successful completion of media fills. Media fills
should be periodically repeated to ensure ongoing competency of the technique.
9. LABELING
The labeling associated with PET drug products may evolve as the drug progresses through the various development stages.
For example, the labeling for PET drug products used for in vitro and animal studies may be very simple and designed to avoid
mix-ups in the routine use of the PET drug product. In later development stages, the labeling may include information re-
quired for the investigational use of the PET drug product in humans. Finally, at the commercial stage of production, the label-
ing should include ingredients, warnings, approved indications, and other elements required by the appropriate regulatory
General Chapters
agencies (e.g., FDA, Nuclear Regulatory Commission, and others).
GLOSSARY
The following definitions apply to words and phrases as they are used in this chapter:
Accuracy: The closeness of test results obtained by that method to the true value established across the range of the meth-
od.
Active pharmaceutical ingredient (API): A radioactive substance that exhibits spontaneous disintegration of unstable nuclei
by the emission of positrons and is incorporated into a PET drug product to furnish a direct effect in the diagnosis or monitor-
ing of a disease or a manifestation of a disease in humans, or monitoring treatment of disease or therapeutic procedures (e.g.,
tumor therapy). Both radioactive and nonradioactive forms of the PET drug are included in the API.
Batch: A quantity of PET drug product that is intended to have uniform character and quality, within specified limits, and
that is made in a single, defined operational cycle.
Chemical purity: The purity of a PET drug product based on the nonradioactive components of the formulation, for exam-
ple, residual solvents and/or volatile impurities, reagents, and or precursors used in the synthesis and purification, stabilizers,
excipients, or by-products produced in the synthesis.
Compounding: The process of synthesis or formulation of a PET drug for use under the practice of pharmacy and medicine.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
8108 á1823ñ / General Information USP 41
Conditional final release: A final release for patient administration before completion of a required test because of a break-
down of analytical equipment.
Limit of detection: The lowest amount of analyte in a sample that can be detected but not necessarily quantified under the
stated method conditions.
Linearity: The ability to elicit test results that are, directly or by a well-defined mathematical transformation, proportional to
the concentration of analyte in samples within a given range.
Lot: A quantity of materials (e.g., reagents, solvents, gases, purification columns, and other auxiliary materials) that have
uniform character and quality within specified limits and are used to make a PET drug product.
Lower limit of quantification: The lowest amount of an analyte in a sample that can be determined with acceptable preci-
sion and accuracy under the stated method conditions.
National Metrology Institute (NMI): A measurement standards body that is a laboratory of metrology that establishes
standards for a country or organization. The National Institute of Standards and Technology (NIST) is the NMI for the United
States.
PET drug: A radioactive substance (active pharmaceutical ingredient) that exhibits spontaneous disintegration of unstable
nuclei by the emission of positrons and is incorporated into a PET drug product to furnish direct effect in the diagnosis or
monitoring of a disease or a manifestation of a disease in humans, or monitoring treatment of disease or therapeutic proce-
dures (e.g., tumor therapy).
PET drug product: A finished dosage form that contains a PET drug, whether or not in association with one or more other
ingredients.
Precision (as repeatability): The degree of agreement among individual test results when the method is applied repeatedly
to multiple samplings of a homogenous sample within a lab over a short period of time using the same analyst with the same
equipment.
Quality assurance (QA): A planned and systematic program to ensure that a PET drug product possesses the quality re-
quired for its intended purpose.
Quality control (QC): A system for testing the quality of components, materials, supplies, and PET drug products by proce-
dures, tests, analytical methods, and acceptance criteria.
Radiochemical identity: The molecular structure of the intended active radiopharmaceutical ingredient that is present in
the radiopharmaceutical preparation.
Radiochemical purity: The ratio, expressed as a percentage, of the radioactivity of the intended active radiopharmaceutical
ingredient to the total radioactivity of all radioactive ingredients present in the radiopharmaceutical preparation.
Radionuclidic identity: The intended radionuclide in the radiopharmaceutical preparation.
Radionuclidic purity: The ratio, expressed as a percentage, of the radioactivity of the intended radionuclide to the total ra-
dioactivity of all radionuclides in the radiopharmaceutical preparation.
Range: The interval between the upper and lower levels of a quality attribute that can be determined with a suitable level of
precision and accuracy.
Reagents and materials: A reagent is a chemical used in the synthesis and/or testing of a PET drug, whereas a material is an
ancillary object, such as tubing, glassware, vials, and others.
Retardation factor (TLC): The ratio of the distance the analyte moved from the origin line divided by the distance the sol-
vent moved from the origin line denoted by the variable Rf.
Retention time (HPLC or GC): The time required, after the injection, for the analyte to move through the column and reach
the detector.
Robustness: The measure of the capacity of an analytical method to remain unaffected by small variations in method pa-
rameters.
General Chapters
Ruggedness (as reproducibility): The degree of reproducibility of test results obtained by the analysis of the same samples
under a variety of conditions, such as different labs, different analysts, different instruments, different lots of reagents, different
assays, and different days.
Specific activity: The radioactivity of a radionuclide per unit mass of the element or compound. The unit of specific activity
is the amount of radioactivity on a mass basis [e.g., mCi/mg (MBq/mg) or Ci/mmol (GBq/mmol)].
Specificity: The ability to assess unequivocally the analyte in the presence of components that may be expected to be
present such as impurities, degradation products, and matrix components.
Strength: The radioactivity concentration of the active pharmaceutical ingredient in a PET drug product at a given date and
time. The unit of strength is the amount of radioactivity on a volume basis [e.g., mCi/mL (MBq/mL)].
Sub-batch: A quantity of PET drug product having uniform character and quality, within specified limits, that is produced
during one succession of multiple irradiations using a given synthesis or purification operation. A group of sub-batches collec-
tively forms a batch that is intended to have uniform character and quality, within specified limits. Sub-batches may be re-
quired for PET drug products with very short-lived radionuclides (e.g., 13N and 15O), because QC tests cannot be completed
before use.
System suitability: Requirements used to verify that the system performs according to established criteria.
Tailing factor (symmetry factor): A measure indicating the non-ideality of a chromatographic peak resulting from the distri-
bution and the migration of the analyte through the chromatographic column.
Validation: Establishment of documented evidence that a method, process, or system meets its intended requirements.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
Accessed from 200.136.52.120 by lear5 on Thu May 17 09:29:58 EDT 2018
USP 41 General Information / á1852ñ 8109
Verification: Confirmation that an established method, process, or system meets predetermined acceptance criteria.
á1852ñ ATOMIC ABSORPTION SPECTROSCOPY—THEORY AND
PRACTICE
THEORY
The instrumental technique of atomic absorption spectrometry (AAS; see Appendix for a list of acronyms in this chapter) uses
the Beer–Lambert Law (Beer's Law), which relates the concentration of an analyte in a sample to the sample's absorption of
electromagnetic radiation. Beer's Law states that the optical absorbance of a chromophore in a transparent solvent is linearly
proportional to the chromophore's concentration and also to the sample cell path length. Beer's Law is applicable only if the
spectral bandwidth of the light is narrow compared to the spectral line widths in the spectrum and is expressed as follows:
A = ebc
A = absorbance
e = molar absorptivity [L/(mol · cm)]
b = path length of the sample cell (cm)
c = concentration (mol/L)
In addition:
A = log10(P0/P) = log10(1/T) = log10(100/%T) = 2 − log10%T
P0 = intensity of light passing through a sample
P = intensity of light leaving the sample
T = transmittance
%T = 100 × T
AAS methods fall into two categories: flame (FAAS) and flameless. Flameless methods include graphite furnace AAS (GFAAS),
also known as electrothermal vaporization AAS (ETVAAS), for ultra-trace analyses. Other flameless methods are cold vapor AAS
(CVAAS), intended specifically for the analysis of mercury, and hydride generation AAS (HGAAS), intended specifically for the
analysis of arsenic, bismuth, germanium, lead, antimony, selenium, tin, and tellurium.
A basic AAS consists of a radiation source, a sample introduction device, a means to atomize the sample, a monochromator
or a polychromator, a detector, and some means of acquiring data (usually a computer). Most instruments also have some sort
of background correction system, which will be discussed later in this chapter.
In the case of FAAS, the flame through which the sample passes is considered to be the sample cell. In the case of electro-
thermal vaporization (ETV), the graphite tube into which the sample is deposited is considered to be the sample cell. In the
case of CVAAS, a quartz absorption cell is mounted on top of the burner head, and the space above the burner in the optical
path is considered to be the sample cell. In the case of hydride generation, hydrides are swept into a heated cell.
INSTRUMENTATION
General Chapters
Figure 1. Basic components of an atomic absorption spectrophotometer.
All atomic absorption spectrophotometers share fundamental components (Figure 1). A wide variety of AAS is available com-
mercially and is based on one of two designs: a single-beam or a double-beam light path.
Figure 2 illustrates the light path for a single-beam spectrophotometer. The dotted line represents the modulated light signal
from the external light source (line source), and the solid line represents the direct current signal from the atomizer, represen-
ted by a flame. The ovals represent lenses.
In this example, the beam from the line source is electrically modulated, and an amplifier placed after the detector is tuned
to this modulation frequency. The beam from the line source becomes coded in this manner. The result is that the noise from
the radiation emitted at all frequencies, except for the resonance frequency, is rejected, and the signal-to-noise ratio is im-
proved.
Single-beam spectrophotometers rely on a very stable line source to maintain accuracy. It is also necessary to run a separate
blank solution in order to provide a correct 100% T adjustment.
Official from May 1, 2018
Copyright (c) 2018 The United States Pharmacopeial Convention. All rights reserved.
You might also like
- Cyclotron Training BookletDocument51 pagesCyclotron Training BookletNawaf BamasoudNo ratings yet
- Principles and Applications of Liquid Scintillation CountingDocument15 pagesPrinciples and Applications of Liquid Scintillation CountingDavid BrownNo ratings yet
- Nuclear Data Relevant To The Production and Application of Diagnostic RadionuclidesDocument10 pagesNuclear Data Relevant To The Production and Application of Diagnostic RadionuclidesPaulo SérgioNo ratings yet
- Copper-64 Radiopharmaceuticals: Production, Quality Control and Clinical ApplicationsFrom EverandCopper-64 Radiopharmaceuticals: Production, Quality Control and Clinical ApplicationsNo ratings yet
- Applications of Zeeman Graphite Furnace Atomic Absorption Spectrometry in the Chemical Laboratory and in ToxicologyFrom EverandApplications of Zeeman Graphite Furnace Atomic Absorption Spectrometry in the Chemical Laboratory and in ToxicologyC. MinoiaNo ratings yet
- Ai CP 02Document5 pagesAi CP 02Random gmailNo ratings yet
- QC of RadiopharmaceuticalsDocument9 pagesQC of Radiopharmaceuticalscarchakam0% (1)
- Radioactive GHJNVN PDFDocument37 pagesRadioactive GHJNVN PDFReality of lifeNo ratings yet
- 2016 Zeitschrift Fur Anorganische Und Aligemeine ChemieDocument6 pages2016 Zeitschrift Fur Anorganische Und Aligemeine ChemieildaNo ratings yet
- PrinciplesDocument100 pagesPrinciplesKouka MahfoudiNo ratings yet
- ECL Presentation Radionuclide-RuleDocument39 pagesECL Presentation Radionuclide-RuleEdmilson MonteiroNo ratings yet
- Ai CP 02Document5 pagesAi CP 02Random gmailNo ratings yet
- JETIR2305743Document13 pagesJETIR2305743Ilhan KhanNo ratings yet
- Implementation of The International Code of Practice On Dosimetry in Radiotherapy (TRS 398) : Review of Testing ResultsDocument111 pagesImplementation of The International Code of Practice On Dosimetry in Radiotherapy (TRS 398) : Review of Testing ResultsCristian GondacNo ratings yet
- ContributionDocument2 pagesContributionJohnson CNo ratings yet
- Huclier-Markai - DOTA Labeling of Sc-44 - 2014Document8 pagesHuclier-Markai - DOTA Labeling of Sc-44 - 2014PAULINA MUNGUIANo ratings yet
- Plutonium by Iron (II) /chromium (VI) Amperometric Titration: Standard Test Method ForDocument4 pagesPlutonium by Iron (II) /chromium (VI) Amperometric Titration: Standard Test Method ForPrakash MakadiaNo ratings yet
- ASTM D 7085 - 04 (2010) E1Document10 pagesASTM D 7085 - 04 (2010) E1quochunguicNo ratings yet
- Nuclear Analytical TechniquesDocument18 pagesNuclear Analytical TechniquesAsad Noman100% (1)
- Radiopharmaceuticals Guide to Half-Lives & Medical UsesDocument31 pagesRadiopharmaceuticals Guide to Half-Lives & Medical UsesGail AidNo ratings yet
- Namratha FinalDocument56 pagesNamratha FinalAkhil KattamuriNo ratings yet
- Radiopharmaceutical preparationsDocument7 pagesRadiopharmaceutical preparationsDayana BecerraNo ratings yet
- 1 s2.0 S1507136714000339 MainDocument10 pages1 s2.0 S1507136714000339 MainViviana Carrascal ArenasNo ratings yet
- Module 2Document15 pagesModule 2WillykateKairuNo ratings yet
- Radioactive TracerDocument7 pagesRadioactive TracerJonathanNo ratings yet
- Radiation Resistance of Amino AcidsDocument10 pagesRadiation Resistance of Amino Acidsaniket singhNo ratings yet
- UCL CHEM2601 Imaging L3-4 (Nuclear Imaging & Radiochemistry)Document61 pagesUCL CHEM2601 Imaging L3-4 (Nuclear Imaging & Radiochemistry)AlexTsuiNo ratings yet
- Validation Plan FormatDocument8 pagesValidation Plan FormatNora BuanNo ratings yet
- PotassiumDocument5 pagesPotassiumAhmed IsmailNo ratings yet
- Highly Sensitive Immunoassay Based On Immunogold - Silver Amplification and Inductively Coupled Plasma Mass Spectrometric DetectionDocument7 pagesHighly Sensitive Immunoassay Based On Immunogold - Silver Amplification and Inductively Coupled Plasma Mass Spectrometric DetectionLylia MalakNo ratings yet
- Analytical Procedures I. SpectrophotometryDocument16 pagesAnalytical Procedures I. SpectrophotometryAnh VõNo ratings yet
- 3908 ST6 1e PDFDocument12 pages3908 ST6 1e PDFMed Ali SmaouiNo ratings yet
- Classical least-squares method for assay of antihypertensives and photoproductsDocument8 pagesClassical least-squares method for assay of antihypertensives and photoproductsiabureid7460No ratings yet
- 68Ga-PET: A Powerful Generator-Based Alternative To Cyclotron-Based PET RadiopharmaceuticalsDocument11 pages68Ga-PET: A Powerful Generator-Based Alternative To Cyclotron-Based PET Radiopharmaceuticalsarifudin_achmadNo ratings yet
- Analysis Guideline for the RoHS Directive Revision Working GroupDocument49 pagesAnalysis Guideline for the RoHS Directive Revision Working GroupMai PhuNo ratings yet
- A Project Report O1Document65 pagesA Project Report O1Pratik PacharneNo ratings yet
- Anachem Group 3 SpectrosDocument15 pagesAnachem Group 3 SpectrosApufwplggl JomlbjhfNo ratings yet
- 2016-Determination of Phenolic Compounds Using Spectral and Color Transitions of Rhodium NanoparticlesDocument8 pages2016-Determination of Phenolic Compounds Using Spectral and Color Transitions of Rhodium NanoparticlesIsmael Antonio Gonzalez RamirezNo ratings yet
- Drug Analysis by Capillary ElectrophoresDocument14 pagesDrug Analysis by Capillary ElectrophoresSORIN AVRAMESCUNo ratings yet
- NMR in Forensic Science-MainDocument83 pagesNMR in Forensic Science-MainIva ManasiNo ratings yet
- Radio PharmacyDocument44 pagesRadio PharmacyIndah PrihandiniNo ratings yet
- E6 104 ThemeContentsDocument13 pagesE6 104 ThemeContentssunildhamaleeNo ratings yet
- Spectrometer Analysis V2 PDFDocument49 pagesSpectrometer Analysis V2 PDFOscar SotomayorNo ratings yet
- Null 2Document24 pagesNull 2Muhammad FaizanNo ratings yet
- 1 s2.0 S0026265X21006330 MainDocument5 pages1 s2.0 S0026265X21006330 MainSab RineNo ratings yet
- Liquid Scintillation Counting: Technique For Detecting RadioactiveDocument12 pagesLiquid Scintillation Counting: Technique For Detecting RadioactiveZeNiNo ratings yet
- 1 s2.0 S1001074209602515 MainDocument9 pages1 s2.0 S1001074209602515 Mainoluwaseunajala404No ratings yet
- Radiochemical Stability of Radiopharmaceutical Preparations: IsbnDocument6 pagesRadiochemical Stability of Radiopharmaceutical Preparations: IsbnIin Tirta SunartaNo ratings yet
- 7483 Et EtDocument11 pages7483 Et Etrudalgupt88No ratings yet
- 58 Spectrometer Analysis v6Document53 pages58 Spectrometer Analysis v6Suriyachai Niamsorn75% (4)
- Real-Time PCR Applications - Presentation by Nasr SinjilawiDocument69 pagesReal-Time PCR Applications - Presentation by Nasr SinjilawiMolecular_Diagnostics_KKUHNo ratings yet
- Review Kajal GawdeDocument12 pagesReview Kajal GawdeNutan Desai RaoNo ratings yet
- Zhou2018 Article TungstenDisulfideWS2NanosheetDocument8 pagesZhou2018 Article TungstenDisulfideWS2NanosheetTrường Nguyễn VănNo ratings yet
- Analytical InstrumentationDocument44 pagesAnalytical InstrumentationIjazNo ratings yet
- PET-CT in Medical PhysicsDocument29 pagesPET-CT in Medical Physicsಸಂಪತ್ ಕುಮಾರ್No ratings yet
- A Practical Approach to Quantitative Metal Analysis of Organic MatricesFrom EverandA Practical Approach to Quantitative Metal Analysis of Organic MatricesNo ratings yet
- W 2HotlineContacts2019 - 0 2 PDFDocument3 pagesW 2HotlineContacts2019 - 0 2 PDFNathan Townsend Levy100% (1)
- Pizza Hut Training Manual FinishedDocument34 pagesPizza Hut Training Manual FinishedEdilson MaziveNo ratings yet
- Centered Nursing Process Approach (9th Ed.) - St. Louis, MO: ElsevierDocument1 pageCentered Nursing Process Approach (9th Ed.) - St. Louis, MO: ElsevierfaizaNo ratings yet
- DCM300E Clamp Meter Measures Earth Leakage CurrentDocument2 pagesDCM300E Clamp Meter Measures Earth Leakage CurrentKatamba RogersNo ratings yet
- 20170322190836toms CaseDocument9 pages20170322190836toms CaseJay SadNo ratings yet
- Circuit Breaker Analyzer & Timer CAT126D: DescriptionDocument7 pagesCircuit Breaker Analyzer & Timer CAT126D: Descriptionkenlavie2No ratings yet
- Tracing Chronic Fatigue Syndrome Tsfunction Is Key To ME - CFS - B Day PDFDocument91 pagesTracing Chronic Fatigue Syndrome Tsfunction Is Key To ME - CFS - B Day PDFsanthigiNo ratings yet
- MEL - Math 10C Item Writing - MC & NR ReviewDocument71 pagesMEL - Math 10C Item Writing - MC & NR ReviewMya TseNo ratings yet
- Iranian Food Enquiries ReportDocument22 pagesIranian Food Enquiries Reportswapnilrane03100% (1)
- The Teacher and Student Relationship of Haydn and BeethovenDocument10 pagesThe Teacher and Student Relationship of Haydn and BeethovenVinny MuscarellaNo ratings yet
- Currency DerivativesDocument16 pagesCurrency DerivativesAdityaNandaNo ratings yet
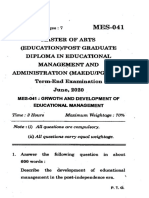
- Master of Arts (Education) /post Graduate Diploma in Educational Management and Administration (Maedu/Pgdema) Term-End Examination June, 2020Document7 pagesMaster of Arts (Education) /post Graduate Diploma in Educational Management and Administration (Maedu/Pgdema) Term-End Examination June, 2020Shreyashi Santra MitraNo ratings yet
- Hdpe Guide PDFDocument81 pagesHdpe Guide PDFbalotNo ratings yet
- THE END - MagDocument164 pagesTHE END - MagRozze AngelNo ratings yet
- Cilegon-Order Material Pt. Quantum Radja Perkasa-280823Document1 pageCilegon-Order Material Pt. Quantum Radja Perkasa-280823Ria Maretta DewiNo ratings yet
- Laptops and Desktop-MAY PRICE 2011Document8 pagesLaptops and Desktop-MAY PRICE 2011Innocent StrangerNo ratings yet
- Introduction To SQL Programming TechniquesDocument24 pagesIntroduction To SQL Programming Techniquesakashdeepime100% (2)
- Ultra-compact Terrier drilling rig fits through standard doorwaysDocument8 pagesUltra-compact Terrier drilling rig fits through standard doorwaysjpantazis1975No ratings yet
- Listening and Speaking 3 Q: Skills For Success Unit 4 Student Book Answer KeyDocument4 pagesListening and Speaking 3 Q: Skills For Success Unit 4 Student Book Answer KeyAhmed MohammedNo ratings yet
- (Eng) Advanced Concept Training - 2d Concrete Members en 1992 - 2017Document69 pages(Eng) Advanced Concept Training - 2d Concrete Members en 1992 - 2017Muscadin MakensonNo ratings yet
- Abbott Piramal AgreementDocument88 pagesAbbott Piramal AgreementHemanth NandigalaNo ratings yet
- Sbi KukkatpallyDocument2 pagesSbi KukkatpallyRavi Babu KonkatiNo ratings yet
- Sodium Lignosulfonate MSDS: Section 1: Chemical Product and Company IdentificationDocument5 pagesSodium Lignosulfonate MSDS: Section 1: Chemical Product and Company IdentificationYasdiOKNo ratings yet
- Electronics, Furniture, Clothing and Home Stores in KalkaDocument4 pagesElectronics, Furniture, Clothing and Home Stores in KalkaMANSA MARKETINGNo ratings yet
- Coalgebraic Modelling of Timed ProcessesDocument298 pagesCoalgebraic Modelling of Timed ProcessesFaris Abou-SalehNo ratings yet
- Industrial Radiography Image Forming Techniques English 4Document114 pagesIndustrial Radiography Image Forming Techniques English 4Narasimha Murthy InampudiNo ratings yet
- UntitledDocument39 pagesUntitledKaren CobachaNo ratings yet
- Bamuoingaythienquan NguyenduynhienDocument9 pagesBamuoingaythienquan NguyenduynhienFLed NguyenNo ratings yet
- Psv5 FHD 215naDocument1 pagePsv5 FHD 215naVijay BhureNo ratings yet
- Studies on the vertically barred Haplochromis electra from Lake MalawiDocument5 pagesStudies on the vertically barred Haplochromis electra from Lake MalawiCenk Sururi KarabulutNo ratings yet