Professional Documents
Culture Documents
Clostridia Lec 6
Uploaded by
markmuiruri581Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clostridia Lec 6
Uploaded by
markmuiruri581Copyright:
Available Formats
GRAM-POSITIVE BACILLI – ANAEROBIC SPORE-FORMING
1. Clostridium tetani
Disease—Tetanus. Characteristics—Anaerobic, gram-positive, spore-forming rods. Spore is at one end (“terminal spore”),
so organism looks like a tennis racket. Habitat and Transmission—Habitat is the soil. Organism enters through traumatic
breaks in the skin.
Pathogenesis—Spores germinate under anaerobic conditions in the wound. Organism produces exotoxin, which blocks
release of inhibitory neurotransmitters (glycine and γ-aminobutyric acid [GABA]) from spinal neurons. Excitatory neurons
are unopposed, and extreme muscle spasm (tetanus, spastic paralysis) results.
“Lock-jaw” and “risus sardonicus” are two examples of the muscle spasms. Tetanus toxin (tetanospasmin) is a protease
that cleaves proteins involved in the release of neurotransmitters.
Laboratory Diagnosis—Primarily a clinical diagnosis. Organism is rarely isolated. Serologic tests not useful.
Treatment—Hyperimmune human globulin to neutralize toxin. Also penicillin G and spasmolytic drugs (e.g., Valium). No
significant resistance to penicillin.
Prevention— Debride wound. Toxoid vaccine (toxoid is formaldehyde-treated toxin). Usually given to children in
combination with diphtheria toxoid and acellular pertussis vaccine (DTaP). If patient is injured and has not been
immunized, give hyperimmune globulin plus toxoid (passive–active immunization). Give tetanus toxoid booster every 10
years.
2. Clostridium botulinum
Disease—Botulism. Characteristics—Anaerobic, gram-positive, spore-forming rods.
Habitat and Transmission—Habitat is the soil. Organism and botulinum toxin transmitted in improperly preserved food.
Pathogenesis—Botulinum toxin is a protease that cleaves proteins involved in the release of acetylcholine at the
myoneural junction, causing flaccid paralysis. Failure to sterilize food during preservation allows spores to survive. Spores
germinate in anaerobic environment and produce toxin. The toxin is heat-labile; therefore, foods eaten without proper
cooking are usually implicated.
Laboratory Diagnosis—Presence of toxin in patient’s serum or stool or in food. Detection of toxin involves either
antitoxin in serologic tests or production of the disease in mice. Serologic tests for antibody in the patient are not useful.
Treatment—Antitoxin to types A, B, and E made in horses. Respiratory support may be required. Prevention—Observing
proper food preservation techniques, cooking all home-canned food, and discarding bulging cans.
3. Clostridium perfringens
Diseases—Gas gangrene (myonecrosis) and food poisoning.
Characteristics—Anaerobic, gram-positive, spore-forming rods.
Habitat and Transmission—Habitat is soil and human colon. Myonecrosis results from contamination of wound with soil
or feces. Food poisoning is transmitted by ingestion of contaminated food.
Pathogenesis—Gas gangrene in wounds is caused by germination of spores under anaerobic conditions and the
production of several cytotoxic factors, especially alpha toxin, a lecithinase that cleaves cell membranes. Gas in tissue
(CO2 and H2) is produced by organism’s anaerobic metabolism. Food poisoning is caused by production of enterotoxin
within the gut. Enterotoxin acts as a superantigen, similar to that of S. aureus.
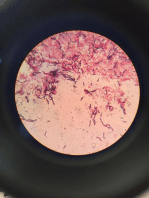
Laboratory Diagnosis—Gram-stained smear plus anaerobic culture. Spores not usually seen in clinical specimens; the
organism is growing, and nutrients are not restricted. Production of lecithinase is detected on egg yolk agar and
identified by enzyme inhibition with specific antiserum. Serologic tests not useful.
Treatment—Penicillin G plus debridement of the wound in gas gangrene (no significant resistance to penicillin). Only
symptomatic treatment needed in food poisoning.
Prevention—Extensive debridement of the wound plus administration of penicillin decreases probability of gas
gangrene. There is no vaccine.
4. Clostridium difficile
Disease—Pseudomembranous colitis. Characteristics—Anaerobic, gram-positive, spore-forming rods. Habitat and
Transmission—Habitat is the human colon. Transmission is fecal–oral.
Pathogenesis—Antibiotics suppress normal flora of colon, allowing C. difficile to overgrow and produce large amounts of
exotoxins. Exotoxins A and B inhibit GTPases, causing inhibition of signal transduction and depolymerization of actin
filaments. This leads to apoptosis and death of enterocytes. The pseudomembranes seen in the colon are the visual
result of the death of enterocytes.
Laboratory Diagnosis—Exotoxin in the stool is typically detected by using known antibody to the toxin in an ELISA test or
by polymerase chain reaction (PCR) assay. Exotoxin in stool can also be detected by cytopathic effect on cultured cells.
Identified by neutralization of cytopathic effect with known antibody.
Treatment—Metronidazole. Vancomycin, although effective, should not be used because it may select for vancomycin-
resistant enterococci. Prevention—No vaccine or drug is available.
You might also like
- Micro Chapter 17Document8 pagesMicro Chapter 17Ana AbuladzeNo ratings yet
- Gram Positive BacteriaDocument3 pagesGram Positive BacteriaZety ATNo ratings yet
- Clostrdia: G Positive Spore Forming Anaerobic Toxin Producing RodsDocument36 pagesClostrdia: G Positive Spore Forming Anaerobic Toxin Producing Rodsjamal nasirNo ratings yet
- ClostridumDocument30 pagesClostridumFrancesca VargasNo ratings yet
- 5B - Spore Forming Gram Positive Bacteria - CLOSTRIDIUMDocument5 pages5B - Spore Forming Gram Positive Bacteria - CLOSTRIDIUMRaunaq Singh RatraNo ratings yet
- Faculty of Medicine Hashemite University DR Mohammad Al-Tamimi, MD, Master Biomed, PHDDocument46 pagesFaculty of Medicine Hashemite University DR Mohammad Al-Tamimi, MD, Master Biomed, PHDDaniel AtiehNo ratings yet
- Morphology & Identification: Clostridium SpeciesDocument14 pagesMorphology & Identification: Clostridium Specieshussain AltaherNo ratings yet
- Causative Agents of Anaerobe Infections. (NXPowerLite)Document70 pagesCausative Agents of Anaerobe Infections. (NXPowerLite)ashishanandaakNo ratings yet
- UII Gram Pos Spore-FormfefefeDocument30 pagesUII Gram Pos Spore-FormfefefeDito TrunogatiNo ratings yet
- The Clostridium Specis.Document38 pagesThe Clostridium Specis.علي عبد الكريم عاصيNo ratings yet
- (Powerpoint) CHAPTER 16 AND 22 - BACILLUS, CLOSTRIDIUM, ANAEROBIC BACTERIOLOGYDocument59 pages(Powerpoint) CHAPTER 16 AND 22 - BACILLUS, CLOSTRIDIUM, ANAEROBIC BACTERIOLOGYNel TinduganiNo ratings yet
- MSK StaphDocument3 pagesMSK Staphعبدالرحمن عابدNo ratings yet
- Clostridium BotulinumDocument37 pagesClostridium Botulinummaria dulceNo ratings yet
- Lec4 Clostridium 2Document6 pagesLec4 Clostridium 2hindaoda90No ratings yet
- Gram Negative Rods of Enteric TractDocument2 pagesGram Negative Rods of Enteric TractJohn TerryNo ratings yet
- Intestinal Cestodes: DR Mohiedden M Abdul-FattahDocument27 pagesIntestinal Cestodes: DR Mohiedden M Abdul-FattahMicroscopeGeekNo ratings yet
- Lec. 8 Bacillus Clostridium1193786926542Document18 pagesLec. 8 Bacillus Clostridium1193786926542تجربة أولىNo ratings yet
- Anaerobic Spore-Forming Bacteria: S.Y.MaselleDocument41 pagesAnaerobic Spore-Forming Bacteria: S.Y.MaselleMasali MacdonaNo ratings yet
- Bacillus SPP: There Are Two Medically ImportantDocument20 pagesBacillus SPP: There Are Two Medically ImportantEng CirroNo ratings yet
- BotulismDocument29 pagesBotulismRohan TejaNo ratings yet
- Anaerobes and AnthraxDocument65 pagesAnaerobes and AnthraxGalih Maygananda PutraNo ratings yet
- Enterotoxemia, Anaerobic Dysentery, Bradsot, Botulism and NecrobacteriosisDocument17 pagesEnterotoxemia, Anaerobic Dysentery, Bradsot, Botulism and NecrobacteriosisNajafova SuadaNo ratings yet
- 760 Staphylococcus PPT UG LectureDocument47 pages760 Staphylococcus PPT UG Lectureridwan.biotekNo ratings yet
- Gram Positive CocciDocument55 pagesGram Positive CocciAyat MostafaNo ratings yet
- Staphylococci: Streptococcus PyogenesDocument20 pagesStaphylococci: Streptococcus PyogenesPharmacy2015100% (2)
- 3.2.1. Gram Positive Rods - ClostridiaDocument58 pages3.2.1. Gram Positive Rods - Clostridiaahmed mohammed100% (1)
- 3 Streptococcus: 3.2.1 The Direct Bacteriological Diagnosis in Streptococcal PharyngitisDocument5 pages3 Streptococcus: 3.2.1 The Direct Bacteriological Diagnosis in Streptococcal PharyngitisMahmoud IdlbiNo ratings yet
- Penunjang Kuliah Botulisme DRDocument7 pagesPenunjang Kuliah Botulisme DRAnonymous DA8iQzNo ratings yet
- Dm-Lecture 4-11-23Document28 pagesDm-Lecture 4-11-23s.zainabtanweerNo ratings yet
- Bacterial ToxinsDocument23 pagesBacterial ToxinsSummayya Kanwal AhmadNo ratings yet
- S. AureusDocument39 pagesS. AureusRajkishor YadavNo ratings yet
- 1.4 - ClostridiumDocument45 pages1.4 - Clostridiumsajad abasNo ratings yet
- Gram +ve BacteriaDocument58 pagesGram +ve BacteriaGx NavinNo ratings yet
- Piogenic Cocci: Ania Kurniawati PD, Dr. MkesDocument58 pagesPiogenic Cocci: Ania Kurniawati PD, Dr. MkesSilmi Zhillan Nur RahmanNo ratings yet
- PSEUDOMONAS Bacilli ListreiaDocument12 pagesPSEUDOMONAS Bacilli ListreiaSheikh FaishalNo ratings yet
- Diarrhea in Kittens and Young Cats - WSAVA2011 - VINDocument4 pagesDiarrhea in Kittens and Young Cats - WSAVA2011 - VINkukuhamru19No ratings yet
- Foodborne Intoxication and ToxicoinfectionsDocument73 pagesFoodborne Intoxication and ToxicoinfectionsAyuIrhoniRosadiNo ratings yet
- Gram Positive CocciDocument140 pagesGram Positive CocciBles Cy LagrimasNo ratings yet
- Nervous System InfectionDocument50 pagesNervous System InfectionputiNo ratings yet
- Clostridium and MycobacteriumDocument40 pagesClostridium and MycobacteriumSAYMABANUNo ratings yet
- staplylococci محاضرة الاولىDocument20 pagesstaplylococci محاضرة الاولىArwa HussienNo ratings yet
- Finasls 1 Staph Strep PDFDocument50 pagesFinasls 1 Staph Strep PDFFrancis ValdezNo ratings yet
- Clostridium Botulinum: Ria MemoriaDocument17 pagesClostridium Botulinum: Ria MemoriaJanvi PatelNo ratings yet
- Chapter 2 Pathogenic Gram Positive CocciDocument76 pagesChapter 2 Pathogenic Gram Positive CocciMubaarįk ÝãřeNo ratings yet
- Part-2-ParasitologyDocument33 pagesPart-2-ParasitologyAli AhmedNo ratings yet
- Clostridium PerfingensDocument7 pagesClostridium PerfingensEma KurgasNo ratings yet
- BRUCELLADocument38 pagesBRUCELLAunknown WorldNo ratings yet
- Food PoisoningDocument20 pagesFood PoisoningNgọcNo ratings yet
- Clostridium BotulinumDocument11 pagesClostridium BotulinumStefy BarranoNo ratings yet
- Gram Positive Bacilli: A. Bacillus SpeciesDocument9 pagesGram Positive Bacilli: A. Bacillus SpeciesOddly SatisfyingNo ratings yet
- G-Positive Non Spore Forminmg Rods-Listeria and Coynebacterium-FinalDocument36 pagesG-Positive Non Spore Forminmg Rods-Listeria and Coynebacterium-FinalDaniel AtiehNo ratings yet
- Gas GangreneDocument21 pagesGas GangreneSyaIra SamatNo ratings yet
- Pyogenic Cocci Pyogenic Means " Pus Forming" Cocci Means "Spherical Bacteria"Document14 pagesPyogenic Cocci Pyogenic Means " Pus Forming" Cocci Means "Spherical Bacteria"Ab AbNo ratings yet
- UTS 3.zonosis 1Document68 pagesUTS 3.zonosis 1Andi Zul AzhriNo ratings yet
- Rod Bacillus: SporogeneDocument10 pagesRod Bacillus: SporogeneNina NovakovićNo ratings yet
- 3.1 Staphylococci PDFDocument36 pages3.1 Staphylococci PDFWong ShuanNo ratings yet
- Bacterial Food PoisoningDocument40 pagesBacterial Food Poisoningdigracia manatigaNo ratings yet
- Screenshot 2021-06-04 at 23.19.29Document72 pagesScreenshot 2021-06-04 at 23.19.29Amina Mohamed AbdikeirNo ratings yet
- Adrenocorticotropic Hormone - Video & Anatomy - OsmosisDocument8 pagesAdrenocorticotropic Hormone - Video & Anatomy - Osmosismarkmuiruri581No ratings yet
- Enteric Nervous System - Video, Anatomy & Definition - OsmosisDocument7 pagesEnteric Nervous System - Video, Anatomy & Definition - Osmosismarkmuiruri581No ratings yet
- Carbohydrates and Sugars - Video, Anatomy & Definition - OsmosisDocument7 pagesCarbohydrates and Sugars - Video, Anatomy & Definition - Osmosismarkmuiruri581No ratings yet
- Endocrine System-1Document90 pagesEndocrine System-1markmuiruri581No ratings yet
- Spermatogenesis Group 3 PresentationDocument10 pagesSpermatogenesis Group 3 Presentationmarkmuiruri581No ratings yet
- Examination Questions and Answers in Basic Anatomy and Physiology. 2000 Multiple Choice Questions - Martin CaonDocument508 pagesExamination Questions and Answers in Basic Anatomy and Physiology. 2000 Multiple Choice Questions - Martin CaonMiguel Angel Mendoza Zabalaga67% (6)
- HNS 2111. Psychology Docx New CurriculumDocument3 pagesHNS 2111. Psychology Docx New Curriculummarkmuiruri581No ratings yet
- Mycology1 Lec 8Document6 pagesMycology1 Lec 8markmuiruri581No ratings yet
- Coronary CirculationDocument5 pagesCoronary Circulationmarkmuiruri581No ratings yet
- 1 Year B.SC Nursing Psychology (QP - Code-1758) Question Bank Unit - I: IntroductionDocument9 pages1 Year B.SC Nursing Psychology (QP - Code-1758) Question Bank Unit - I: IntroductionBasit RamzanNo ratings yet
- Ideal (General) Gas LawDocument8 pagesIdeal (General) Gas Lawmarkmuiruri581No ratings yet
- Theories and ModelsDocument30 pagesTheories and Modelscykemoraa16No ratings yet
- Anatomy of The Oculomotor (CN III), Trochlear (CN IV) and Abducens (CN VI) Nerves - OsmosisDocument4 pagesAnatomy of The Oculomotor (CN III), Trochlear (CN IV) and Abducens (CN VI) Nerves - Osmosismarkmuiruri581No ratings yet
- Dmso TinnitusDocument7 pagesDmso TinnitusJoão FrancoNo ratings yet
- Pembahasan Semester 4-5 Maret 2022Document21 pagesPembahasan Semester 4-5 Maret 2022Angger SatriaNo ratings yet
- Physical Restraint Reduction For Older AdultsDocument11 pagesPhysical Restraint Reduction For Older Adultsantariksa tedyNo ratings yet
- Semester 3 PBL Student Casebook 2022 23Document26 pagesSemester 3 PBL Student Casebook 2022 23zalsoud2002No ratings yet
- Hpex 357 Midterm ReviewDocument11 pagesHpex 357 Midterm ReviewJoanna RiveraNo ratings yet
- Hypertensive Crisis PathoDocument4 pagesHypertensive Crisis PathoJanelle Dela CruzNo ratings yet
- Seidman 2014Document17 pagesSeidman 2014Anonymous G6zDTD2yNo ratings yet
- Postpartum ComplicationsDocument13 pagesPostpartum ComplicationsAlexa PasionNo ratings yet
- CANINE-Cricopharyngeal Achalasia in DogsDocument6 pagesCANINE-Cricopharyngeal Achalasia in Dogstaner_soysurenNo ratings yet
- UntitledDocument340 pagesUntitledAlistair KohNo ratings yet
- 1st Year MBBS Question Papers RGUHS 2021Document10 pages1st Year MBBS Question Papers RGUHS 2021Gaurav parashar100% (1)
- Booklet On Implementation of Antibiotic Stewardship ProgrammeDocument42 pagesBooklet On Implementation of Antibiotic Stewardship Programmedakmok100% (1)
- Readings (The Sexual Self)Document10 pagesReadings (The Sexual Self)NOOBON100% (1)
- 3 MicroDocument4 pages3 MicroDumitraNo ratings yet
- Charles Bonnet SyndromeDocument3 pagesCharles Bonnet SyndromeStuart SmithNo ratings yet
- Feline Infectious PeritonitisDocument14 pagesFeline Infectious PeritonitisdmantsioNo ratings yet
- Ostomies: LessonDocument21 pagesOstomies: Lessonlovelykiss100% (1)
- The Pathophysiology of Sepsis - 2021 Update - Part 2, Organ Dysfunction and AssessmentDocument13 pagesThe Pathophysiology of Sepsis - 2021 Update - Part 2, Organ Dysfunction and AssessmentValerie ZimmermannNo ratings yet
- Roger Case Study and Nursing Process 2Document9 pagesRoger Case Study and Nursing Process 2E.R.ONo ratings yet
- MD Radio Diagnosis - Plan of Thesis (Year 2015)Document2 pagesMD Radio Diagnosis - Plan of Thesis (Year 2015)Muhammad UmarNo ratings yet
- FECALYSISDocument14 pagesFECALYSISMarl EstradaNo ratings yet
- NLE2Document10 pagesNLE2giansulakisosuNo ratings yet
- Nuvastatic Practitioner Only Information 12.5.20Document8 pagesNuvastatic Practitioner Only Information 12.5.20Jamall EllisNo ratings yet
- Effect of Covid 19 On Trade and BusinessDocument87 pagesEffect of Covid 19 On Trade and BusinessTasmay EnterprisesNo ratings yet
- CV By, Yvette02Document4 pagesCV By, Yvette02Yvette PamatmatNo ratings yet
- Feature Writing About Covid-19 - MortelDocument2 pagesFeature Writing About Covid-19 - MortelAna Carmela MortelNo ratings yet
- Wilms' Tumour (Nephroblastoma) : EpidemiologyDocument3 pagesWilms' Tumour (Nephroblastoma) : EpidemiologyPauleen Trisha SamparaniNo ratings yet
- Newborn Disorders - : Small For Gestational Age (Sga) NewbornDocument11 pagesNewborn Disorders - : Small For Gestational Age (Sga) Newborncayla mae carlosNo ratings yet
- Covid-19 and Mathematics: AN ANALYSIS WITH THE HELP OF SYSTEM OF LINEAR EQUATIONSDocument9 pagesCovid-19 and Mathematics: AN ANALYSIS WITH THE HELP OF SYSTEM OF LINEAR EQUATIONSGogyNo ratings yet
- Animal Health Product Listing BrochureDocument16 pagesAnimal Health Product Listing BrochureHuamaní Rodríguez JhordyNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)