Professional Documents
Culture Documents
HIdradenite - Atraso No Diagnostico
Uploaded by
José Paulo Ribeiro JúniorOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HIdradenite - Atraso No Diagnostico
Uploaded by
José Paulo Ribeiro JúniorCopyright:
Available Formats
Research Article
Dermatology Received: February 18, 2020
Accepted: April 26, 2020
DOI: 10.1159/000508787 Published online: July 1, 2020
Delayed Diagnosis of Hidradenitis
Suppurativa and Its Effect on Patients
and Healthcare System
Georgios Kokolakis a, b Kerstin Wolk a–c Sylke Schneider-Burrus a, d
Stefanie Kalus e Sebastian Barbus f Susana Gomis-Kleindienst f Robert Sabat a, b
a Interdisciplinary
Group of Molecular Immunopathology, Dermatology/Medical Immunology,
Charité – Universitätsmedizin Berlin, Berlin, Germany; b Psoriasis Research and Treatment Centre,
Charité – Universitätsmedizin Berlin, Berlin, Germany; c Berlin-Brandenburg Centre for Regenerative Therapies,
Charité – Universitätsmedizin Berlin, Berlin, Germany; d Centre for Dermatosurgery, Havelklinik, Berlin, Germany;
e GKM Gesellschaft für Therapieforschung mbH, Munich, Germany; f AbbVie Deutschland GmbH & Co. KG,
Wiesbaden, Germany
Keywords sis delay was longer in younger and non-smoking patients.
Acne inversa · Hidradenitis suppurativa · Comorbidity · In most cases, HS was correctly diagnosed by dermatolo-
Diagnosis · Healthcare system gists. The longer the delay of diagnosis, the greater the dis-
ease severity at diagnosis. Delayed HS diagnosis was also as-
sociated with an increased number of surgically treated
Abstract sites, concomitant diseases, and days of work missed. Con-
Background: Hidradenitis suppurativa (HS) is a neglected clusion: This study demonstrates an enormous delay in the
chronic inflammatory disease with long delay in diagnosis. diagnosis of HS, which results in more severe disease. It also
Besides pain, purulent discharge, and destruction of skin ar- shows for the first time that a delay in diagnosis of a chronic
chitecture, HS patients experience metabolic, musculoskel- inflammatory disease leads to a higher number of concomi-
etal, and psychological disorders. Objectives: To determine tant systemic disorders. In addition to the impaired health
the delay in HS diagnosis and its consequences for patients status, delayed diagnosis of HS was associated with impair-
and the healthcare system. Methods: This was a prospective, ment of the professional life of affected people.
multicenter, epidemiologic, non-interventional cross-sec- © 2020 The Author(s)
tional trial carried out in Germany and based on self-report- Published by S. Karger AG, Basel
ed questionnaires and medical examinations performed by
dermatologists. In total, data of 394 adult HS patients were
evaluated. Results: The average duration from manifesta- Introduction
tion of first symptoms until HS diagnosis was 10.0 ± 9.6
(mean ± SD) years. During this time, HS patients consulted Hidradenitis suppurativa (HS; also designated as acne
on average more than 3 different physicians – most fre- inversa) is a debilitating chronic inflammatory disease that
quently general practitioners, dermatologists, surgeons, gy- affects the intertriginous skin, especially at axillary, ingui-
necologists – and faced more than 3 misdiagnoses. Diagno- nal, and perianal sites [1]. The estimated prevalence of HS
karger@karger.com © 2020 The Author(s) Robert Sabat
www.karger.com/drm Published by S. Karger AG, Basel Interdisciplinary Group of Molecular Immunopathology
This is an Open Access article licensed under the Creative Commons
Dermatology/Medical Immunology, Charité – Universitätsmedizin Berlin
Attribution-NonCommercial-4.0 International License (CC BY-NC) Charitéplatz 1, DE–10117 Berlin (Germany)
(http://www.karger.com/Services/OpenAccessLicense), applicable to robert.sabat @ charite.de
the online version of the article only. Usage and distribution for com-
mercial purposes requires written permission.
is about 1% and HS skin lesions usually appear after pu-
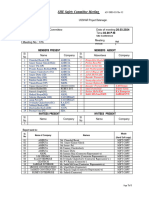
berty, thus mainly burdening the working population [2]. 492 adult patients with HS signed ICF
Approximately one third of patients are genetically predis-
posed [1]. Moreover, lifestyle factors like smoking and
obesity play a crucial role in the clinical course of HS [3–5]. 481 patients participated in FSV
HS starts with the formation of single painful inflamed
nodules or abscesses, defined as Hurley stage I. Without
adequate therapy, the abscesses may recur and build fis-
tulae that discharge malodorous purulent secretion (Hur- 394 patients answered both
the question of age at occurrence of the first symptoms
ley stage II). Finally, inflammation leads to the destruc- and the question of age at the diagnosis (total study cohort)
tion of skin architecture, visible as a diffuse involvement
of large areas with multiple abscesses, interconnected fis-
tulae, and stiff, undermined or hypertrophic scars (Hur-
ley stage III). Pain is the symptom that most strongly af- 25% of total 50% of total 25% of total
study cohort, study cohort, study cohort,
fects the everyday life of patients with HS [6]. Further- 99 patients 196 patients 99 patients
more, odorous purulent discharge and aesthetic with shortest with moderate with longest
diagnosis delay diagnosis delay diagnosis delay
alterations profoundly impair patients’ quality of life and
scarring with formation of contractures causes limitation
in mobility [1]. Therefore, untreated HS leads to embar-
Fig. 1. Flowchart of Patients and Methods demonstrating patient
rassment, social isolation, low self-esteem, and sexual life participation in this study. HS, hidradenitis suppurativa; ICF, in-
impairment [7–9]. It affects not only interpersonal rela- formed consent form; FSV, first study visit.
tionships but also education and professional activity,
producing a strongly disadvantaged population also at
the socioeconomic level [7, 10]. Importantly, a high pro-
portion of HS patients experience metabolic and endocri- rect diagnosis, as recently reported [26]. Furthermore, this
nologic disorders, including hypertriglyceridemia and data was almost exclusively gathered from HS specialized
hyperglycemia [11, 12]. As a consequence of cardiovascu- clinics suggesting that the real-world situation may appear
lar events, such as myocardial infarction or stroke, the life even worse. In this paper, we aimed to determine the length
expectancy of patients with HS is significantly reduced of delay in diagnosis and its impact on the patients’ life and
[13]. Additionally, HS patients frequently experience the healthcare system, based on data collected from a wide
spondyloarthritis [14, 15]. spectrum of dermatological settings.
Although the exact pathogenetic mechanisms are not yet
understood, a relative deficiency of antibacterial proteins,
bacterial propagation, and local uncontrolled immune ac- Patients and Methods
tivation have been postulated [16]. In fact, HS lesions con-
A prospective, epidemiologic, non-interventional, cross-sec-
tain elevated levels of numerous pro-inflammatory cyto-
tional trial (PIRANHA) with HS patients was conducted in 64 Ger-
kines, such as interleukin (IL)-1β, tumor necrosis factor man sites. All patients that fulfilled the inclusion criteria (see on-
(TNF)-α, IL-17, IL-36, and interferon γ [16–20]. These pro- line suppl. material, www.karger.com/doi/10.1159/000508787)
inflammatory cytokines might induce chemokines leading and agreed on the trial were considered for participation. For data
to immune cell infiltration into the skin and purulent dis- collection, supervised paper-based self-reported questionnaires
and documented examination by dermatologists were used.
charge as well as enzymes leading to extracellular matrix
For further details, see Figure 1 and the online supplementary
degradation and fistulae formation [20–22]. Locally pro- material.
duced IL-1β, TNF-α, and IL-17 reach the bloodstream and
might play a substantial role in systemic inflammatory co-
morbidities [23–25]. Therefore, early diagnosis of HS is of
major importance for a prompt lifestyle change and the ini- Results
tiation of proper therapy limiting the inflammation and
propagation of skin destruction and systemic comorbidi- Since the correct diagnosis is the first requirement for
ties. However, worldwide more than 7 years seem to pass adequate therapy, we determined the time between oc-
between the appearance of the first HS symptoms and cor- currence of first HS symptoms and HS diagnosis. Respec-
2 Dermatology Kokolakis et al.
DOI: 10.1159/000508787
tive data were available from 394 participants (total study Table 1. Demographic and clinical characteristics of the study co-
cohort) of the PIRANHA study (Fig. 1). The analyzed hort (n = 394)
population comprised HS patients cared for by physi-
Age, years
cians in private practice, local hospitals, and university Mean ± SD 39.2±11.4
clinics, which may adequately represent the entire spec- Range 18.0–73.0
trum of patients with HS in Germany. Occurrence of first
Female, % 53.3
symptoms, as reported by the patients, was at an average Male, % 46.7
age (mean ± SD) of 24.6 ± 10.5 years (Table 1). Notably,
BMI
the mean age at diagnosis was 34.6 ± 11.2 years (Table 1), Mean ± SD 31.2±7.0
making the average duration between HS disease mani- Range 18.1–60.9
festation and diagnosis 10.0 ± 9.6 years (Fig. 2a). The
Smoker, % 60.3
mean age of the study population at inclusion was 39.2 ± Ex-smoker, % 24.4
11.4 years (Table 1), indicating an average disease dura- Never-smoker, % 15.3
tion of 14.6 ± 10.4 years.
Hurley stage
First, we examined the patient characteristics regard- Mean ± SD 2.05±0.72
ing their association with delayed diagnosis and observed Range 1–3
that the length of delay for male versus female patients
Age at first symptoms, years
was similar (Fig. 2b). The division of the total study co- Mean ± SD 24.6±10.5
hort into the 3 groups (25/50/25% of the total study co- Range 1.0–73.0
hort) according to the duration of the delay in diagnosis
Age at diagnosis, years
(short/moderate/long diagnosis delay) produced the fol- Mean ± SD 34.6±11.2
lowing thresholds: “diagnosis 2 years after first symp- Range 5.2–72.7
toms” (threshold between cohorts with short and moder- Disease duration, years
ate delay) and “diagnosis 15 years after first symptoms” Mean ± SD 14.6±10.4
(threshold between cohorts with moderate and long de- Range 0.0–46.0
lay; Fig. 1). Analyzing these groups with respect to nu-
merous parameters, we found that the age at disease onset BMI, body mass index.
influenced the time until correct diagnosis. The patients
with short delay were older at the time of first symptoms
(Fig. 2c). Accordingly, the age at disease onset negatively
correlated with the length of diagnosis delay (rS = –0.392, with HS with moderately late diagnosis and almost 90%
p < 0.0001). Interestingly, there was also an association of those with late diagnosis had been misdiagnosed com-
between smoking behavior at disease onset and diagnos- pared with 46.5% of patients with early HS diagnosis
tic delay; a significantly larger proportion of non-smokers (Fig. 3c). Moreover, patients with late diagnosis experi-
was detected in the group with the longest delay (Fig. 2d). enced, on average, almost 5 misdiagnoses (Fig. 3d). Gen-
In contrast, we did not detect any significant differences erally, the length of diagnosis delay positively correlates
between these 3 patient groups regarding the localization with the number of misdiagnoses (rS = 0.291, p < 0.0001).
and nature of first cutaneous symptoms. Abscesses, ingrown hairs, and folliculitis were the most
The in-depth analysis further revealed that the length common false diagnoses. Other misdiagnoses included
of diagnosis delay positively correlated with the number acne conglobata or even acne vulgaris (Fig. 3e). Although
of physicians that the patient consulted before HS diag- different physicians examined the patients during diag-
nosis (rS = 0.383, p < 0.0001). Accordingly, patients with nosis lag, dermatologists diagnosed the disease in the ma-
the longest delay in HS diagnosis had consulted almost 5 jority of cases (Fig. 4a).
physicians on average, significantly more than patients Our further investigation focused on the consequenc-
with short diagnostic delays (Fig. 3a). The majority of the es of HS diagnosis delay. Importantly, the length of diag-
patients had seen general practitioners, followed by der- nosis delay positively correlated with the HS severity at
matologists, surgeons, and gynecologists. Patients rarely the time of diagnosis (rS = 0.161, p = 0.005). Accordingly,
visited internists, proctologists, pediatricians, or urolo- the Hurley stage at diagnosis was significantly higher in
gists (Fig. 3b). Although the diagnostic criteria for HS patients with delayed diagnosis compared with those with
have been well established, almost 80% of the patients earlier diagnosis (Fig. 4b).
Delayed Diagnosis of Hidradenitis Dermatology 3
Suppurativa DOI: 10.1159/000508787
50 50
40
40
Delay of diagnosis, years
Delay of diagnosis, years
30
30
20
20
10
10
0
a 0 –10
b Male Female
Fig. 2. Delay of diagnosis in patients with
HS. a Distribution of time in years from oc-
80 50
currence of first HS symptoms until diag- p < 0.0001 p < 0.0001
nosis (n = 394). b Years between first symp- 70
toms and HS diagnosis in male and female 45
patients (n = 394). c Age at disease onset in 60
Patients not smoking before
Age at disease onset, years
3 patient groups with different delays in di-
40
agnosis of HS (≤2 years; > 2 to < 15 years;
disease onset, %
50
≥15 years) since first symptoms occurred
(p value of ANOVA) presented in Tukey- 40 35
type box plots, with the box extending from
the 25th to 75th percentiles of values, the 30
line in the middle of the box and “+” repre- 30
senting the median and the mean, respec- 20
tively, the maximum length of box whis- 25
kers corresponding to 1.5 times the inter- 10
quartile distance, and the values plotted
individually representing outliers (n = 0 20
394). d Percentage of patients in the 3 pa-
s
s
s
s
ar
ar
ar
ar
ar
ar
ye
ye
ye
ye
ye
ye
tient groups with different delay in diagno-
5
≤2
≤2
5
5
<1
<1
≥1
≥1
sis (n = 394), who were non-smokers before
to
to
disease onset (p value of chi-square test). c d
>2
>2
HS, hidradenitis suppurativa.
At study enrollment, 75.6% of all patients had experi- agnosis delay and concomitant diseases. At study enroll-
enced at least one surgical intervention. This was most ment, patients with delayed HS diagnosis experienced
evident in patients with the most delayed HS diagnosis, more comorbidities than patients with earlier diagnosis
approximately 90% of whom underwent surgery (Fig. 5a). (Fig. 5c). Accordingly, the length of diagnosis delay posi-
Moreover, the number of surgically treated sites per pa- tively correlated with the number of concomitant diseas-
tient in this group was higher than in patient groups with es (rS = 0.209, p < 0.0001). The largest difference between
earlier diagnosis (Fig. 5b). Accordingly, the length of di- the subgroups with the shortest and the longest diagnosis
agnosis delay positively correlated with the number of delays was observed in musculoskeletal system disorders
surgically treated sites in the total study cohort (rS = 0.212, (25.3 vs. 41.4%, respectively; p < 0.016) and mental im-
p < 0.0001). This was particularly prominent if abscess pairments (11.1 vs. 25.3%; p < 0.010). Interestingly, the
incision was used as the surgical intervention (rS = 0.204, delay of diagnosis positively correlated with the depres-
p < 0.0001). sion score of Hospital Anxiety and Depression Scale
As a high proportion of HS patients suffer from co- (HADS) collected at study enrollment (rS = 0.116, p <
morbidities, we investigated the association between di- 0.02). As expected, there was no difference in the inci-
4 Dermatology Kokolakis et al.
DOI: 10.1159/000508787
6 100 6
p < 0.0001 p < 0.0001
Misdiagnoses before HS diagnosis, n/patient
Physicians consulted before HS diagnosis,
5 5
80
Patients misdiagnosed before
4 4
HS diagnosis, %
60
n/patient
3 3
40
2 2
20
1 1
0 0 0
s
s
s
s
s
s
s
ar
ar
ar
ar
ar
ar
ar
ar
ar
ye
ye
ye
ye
ye
ye
ye
ye
ye
5
≤2
≤2
5
5
≤2
5
5
<1
≥1
<1
<1
≥1
≥1
a c d
to
to
to
>2
>2
>2
Urologist Other
Pediatrician Pilonidal cyst
Proctologist Hair follicle inflammation
Internist Sweat gland abscess
Gynecologist Ingrown hair
Surgeon Acne vulgaris/conglobata
Dermatologist Folliculitis
General physician
Abscess
0 20 40 60 80 100 0 20 40 60 80 100
Physicians consulted before e Type of misdiagnosis, %
b HS diagnosis, %
Fig. 3. Preceding misdiagnosis in patients with HS. a Number of (n = 390). d Number of misdiagnoses (mean ± SEM) experienced
consulted physicians (mean ± SEM) per patient before HS diagno- before HS diagnosis in the 3 patient groups with different delay in
sis in the 3 patient groups with different delay in diagnosis (n = diagnosis (n = 341, p value of ANOVA). e Percentage of specific
380, p value of ANOVA). b Percentage of patients visiting respec- misdiagnoses before HS was confirmed. HS, hidradenitis suppu-
tive physicians before HS diagnosis. c Percentage of misdiagnosed rativa.
patients in the 3 patient groups with different delay in diagnosis
Delayed Diagnosis of Hidradenitis Dermatology 5
Suppurativa DOI: 10.1159/000508787
2.7
Unknown or other
Pediatrician 2.5
p = 0.0488
Proctologist
Hurley stage at diagnosis
2.3
Internist
2.1
Gynecologist
Surgeon 1.9
Dermatologist
1.7
General practitioner
1.5
0 20 40 60 80 100
s
s
s
ar
ar
ar
Patients with HS diagnosed by indicated
ye
ye
ye
a
5
5
≤2
physicans, %
≥1
<1
b
to
>2
Fig. 4. Physicians involved in diagnosis and disease severity at diagnosis. a Percentage of patients whose HS was
correctly diagnosed by the indicated specialist physicians. b Disease severity reflected by Hurley stage (mean ±
SEM) in the 3 patient groups with different delay in diagnosis at time of HS diagnosis based on patients’ infor-
mation (n = 299, p value of ANOVA). HS, hidradenitis suppurativa.
100 4.0 3.0
p = 0.0045 p = 0.0008 p < 0.0001
3.5
2.5
80
Surgical intervention, % of patients
Surgically treated body sites,
3.0
Additional disease groups,
2.0
2.5
n/patient
60
n/patient
2.0 1.5
40 1.5
1.0
1.0
20
0.5
0.5
0 0 0
s
s
s
s
s
s
s
s
ar
ar
ar
ar
ar
ar
ar
ar
ar
ye
ye
ye
ye
ye
ye
ye
ye
ye
≤2
5
≤2
≤2
5
5
5
5
<1
<1
≥1
<1
≥1
≥1
a b c
to
to
to
>2
>2
>2
Fig. 5. Consequences of diagnosis delay regarding surgery history patient before study enrollment in the 3 patient groups with differ-
and current concomitant diseases. a Percentage of patients in the 3 ent delays in diagnosis (n = 391, p value of ANOVA). c Number of
patient groups with different delay in diagnosis who underwent sur- concomitant diseases (mean ± SEM) per patient at time of study
gical interventions before study enrollment (n = 394, p value of chi- enrollment in the 3 patient groups with different delays in diagnosis
square test). b Number of surgically treated sites (mean ± SEM) per (n = 394, p value of ANOVA). HS, hidradenitis suppurativa.
6 Dermatology Kokolakis et al.
DOI: 10.1159/000508787
100 p = 0.0368 35 p = 0.0245
Days being work-disabled during last 6 months
30
80
Patients unable to work during
last 6 months due to HS, %
25
due to HS, n/patient
60
20
15
40
Fig. 6. Association of diagnosis delay with 10
patients’ work disability. a Percentage of
20
patients unable to work owing to HS in the
5
last 6 months in 3 patient groups with dif-
ferent delay in diagnosis (n = 388, p value
of chi-square test). b Number of days 0 0
(mean ± SEM) during which patients in the
s
s
s
s
s
ar
ar
ar
ar
ar
ar
ye
ye
ye
ye
ye
ye
3 patient groups with different delays in di-
5
5
≤2
≤2
5
≥1
<1
<1
≥1
agnosis were unable to work owing to HS a b
to
to
in the last 6 months (n = 381, p value of
>2
>2
ANOVA). HS, hidradenitis suppurativa.
dence of accidents (13.1 vs. 16.3%; p < 0.547). Even when HS units or from insurances [26, 27]. In our study cohort
adjusted for age at study enrollment and smoking status, that may represent the entire spectrum of patients with
the delay in diagnosis was significantly associated with HS, the first symptoms of disease appeared at an average
the number of comorbidities (p = 0.0370). When com- age of 24.6 ± 10.5 years. Ten years later, HS patients in
pared with the group with the shortest diagnosis delay Germany obtained the diagnosis, which implies an al-
(≤2 years), the expected number of comorbidities in the most 2-year longer delay than in neighboring France [27].
group with longest delay (≥15 years) increased by a factor The comparison to psoriasis, another TNF-α/IL-17 in-
of 1.44 (p = 0.0102). flammatory skin disease [28], where diagnosis can last up
Considering the above-mentioned associations be- to 1.6 ± 4.8 years [26], impressively showed how dramat-
tween the delay in HS diagnosis and its consequences for ic the situation in care of HS patients currently is. In our
patient health status, we aimed to explore the effect of study, patients with delayed HS diagnosis were younger.
delay on patient professional life. In doing so we found One possible explanation for this is that physicians often
that patients with longer delays in HS diagnosis reported associate HS with chronicity and, therefore, suspect the
an inability to work during the last 6 months before study disease in older people. Thus, age should not be a crite-
enrolment more frequently than those with shorter delay rion for HS diagnosis. Similarly, in non-smoking pa-
(Fig. 6a). Moreover, the number of days being work-dis- tients, HS was diagnosed later than in patients who
abled because of HS during these 6 months significantly smoked, perhaps because HS is considered as a disease of
increased with delay of diagnosis (Fig. 6b). smokers. However, about 35% of our patients were non-
smokers at disease onset, strongly suggesting that smok-
ing habits do not clearly help with diagnosing HS.
Discussion Our study points out several consequences of the delay
in HS diagnosis. First, the longer the delay, the higher the
This is the first real-world data-based, prospective number of physicians that were visited before diagnosis.
study in patients with HS that assessed the burden of late This suggests that patients with HS make an effort to find
diagnosis, not only on disease progress but also on the the correct diagnosis and the appropriate therapy. The
professional lives of patients and the healthcare system in physicians visited in that context mainly comprised gen-
Germany. In contrast, previously published data were eral physicians, dermatologists, surgeons, and gynecolo-
based on information gathered either from specialized gists. Internists, proctologists, pediatricians, or urologists
Delayed Diagnosis of Hidradenitis Dermatology 7
Suppurativa DOI: 10.1159/000508787
were visited less frequently. The diversity of the visited tients with HS, as deduced from their mean household in-
physicians reflects the complexity of the disease. How- comes and home values on a neighborhood level [33]. In a
ever, the reason for failing to diagnose HS remains un- limited cohort of patients with HS, the number of work
clear. Since well-established diagnostic criteria have sim- days lost per year has been estimated to be 33.6 ± 26.1 [10].
plified the accurate diagnosis of HS, we assume that med- In our study, the total average number of lost work days
ical care providers were not familiar with the disease. As during 6 months was 16.2 ± 36.23, matching excellently the
a consequence of visiting diverse physicians, patients ex- previous data. In this context, we have shown that the delay
perience several misdiagnoses, inevitably leading to pa- in HS diagnosis has an effect on the number of lost work
tient frustration, increased costs, or even inappropriate days. In fact, the average number of lost work days over a
therapy. On average, almost 5 incorrect diagnoses have 6-month period significantly increased from approximate-
been made for patients with a delay in HS diagnosis of ly 12 for patients with <15 years of diagnosis delay to ap-
>15 years. Furthermore, the incorrect diagnosis in com- proximately 25 for patients with ≥15 years of diagnosis
bination with the simultaneous appearance of new le- delay. Disease severity, operations, and secondary diseases
sions might result in anxiety and depression and that are all associated with delays in diagnosis and can be re-
could explain the positive correlation between length of sponsible for this restriction of the work ability.
diagnosis delay and the depression score of HADS. By including HS patients visiting a wide spectrum of
The importance of early recognition and diagnosis of medical care settings without any selection, we intended
HS is emphasized by the fact that during the time lost un- to receive representative data for the entire spectrum of
til HS diagnosis, the disease progresses from inflamma- patients with HS. However, patients not seeking medical
tory manifestations to tissue destruction. In our cohort, care, for example, because of mild disease or spontaneous
Hurley stage gradually increased with diagnosis delay. remission were not captured in this trial. Further limita-
Patients with delayed diagnosis also reported more surgi- tions of the study design include recall bias and self-re-
cally treated sites, increasing the burden for patients. Im- porting questionnaires; however, in order to improve
portantly, the number of treated sites most significantly data collection and avoid missing or ambiguous data,
correlated with diagnosis delay, when abscess incision questionnaire completion was supervised. In conclusion,
was the applied surgical intervention. Abscess incision is this study provides a detailed insight into HS diagnosis
a minimal intervention that leads to rapid and effective and the consequences of its delay. Our results highlight
pain relief [1]. However, it has no influence on the long- the need for increased awareness and early recognition of
term course of HS, as inflammatory skin alterations reoc- HS in order to ensure prompt therapy initiation for those
cur promptly [1, 29]. Furthermore, frequent surgical in- disadvantaged patients. This can be achieved by continu-
terventions increase the medical care costs. Even when ous education focused on physicians treating HS patients,
compared with patients with severe psoriasis, HS patients like general practitioners, gynecologists, or surgeons, as
showed greater utilization of high-cost medical services, well as by increasing the public awareness for HS.
such as emergency department and inpatient care [30].
Importantly, besides the disease severity itself, an increase
in the number of comorbidities was associated with the Key Message
delay of HS diagnosis. This might be caused by the fact
that HS patients until diagnosis did not obtain systemic There is an enormous delay in the diagnosis of hidradenitis
suppurativa, which is associated with an increased number of con-
medical treatments to control inflammation. In fact, as comitant diseases and impairment of the patients’ professional life.
already reported for psoriasis, the TNF-α/IL-17-domi-
nated inflammation increases the risk for cardiovascular
comorbidity [23, 31]. Notably, the continuous systemic Acknowledgments
anti-TNF-α or anti-IL-17 therapy seems to be capable to
reduce the risk [24]. Similarly, early detection and inflam- The authors would like to thank Susanne Weste, who is a for-
mation reducing treatment of HS might be of major im- mer AbbVie employee, for her appreciated support in organizing
portance in preventing comorbidities. and conducting this trial. Susanne Weste’s contributions were per-
formed while she was an AbbVie employee. We thank Julia Trie-
Recently published data show a higher rate of unem-
bus (Charité) for assisting with the figure preparation. The design,
ployment in patients with HS compared with control pop- study conduct, and financial support for the study were provided
ulation (25.1 vs. 5.9%) [32]. The increased unemployment by AbbVie. AbbVie participated in the interpretation of data, re-
rates may explain the lower socioeconomic status of pa- view, and approval of the publication.
8 Dermatology Kokolakis et al.
DOI: 10.1159/000508787
Statement of Ethics speaker for one or more of the following: AbbVie Inc., AbbVie
Deutschland GmbH & Co. KG, Bayer Schering Pharma AG, Bio-
The Ethics Committee of Charité – Universitätsmedizin Berlin gen IDEC GmbH, Boehringer Ingelheim Pharma GmbH & Co.
approved the study protocol. All patients provided written in- KG, Celgene GmbH, Celgene International II Sàrl, Charité Re-
formed consent. The study was conducted in accordance with the search Organisation GmbH, Dr. Willmar Schwabe GmbH & Co.
Declaration of Helsinki on Ethical Principles for Medical Research KG, Flexopharm GmbH & Co. KG, Generon Corporation ltd.,
and has been registered in the German Clinical Trials Register JanssenCilag GmbH, La Roche-Posay Laboratoire Dermatologique
(DRKS-ID: DRKS00013778). Deutschland, Novartis Pharma GmbH, Parexel International
GmbH, Pfizer Deutschland GmbH, Sanofi-Aventis Deutschland
GmbH, TFS Trial Form Support GmbH, UCB Pharma GmbH.
Conflict of Interest Statement
G.K. has received honoraria for participation in advisory Funding Sources
boards, in clinical trials, and/or as speaker from AbbVie Deutsch-
land GmbH & Co. KG, Abbott GmbH, Actelion Pharmaceuticals This study was supported by AbbVie Deutschland GmbH &
Ltd., Basilea Pharmaceutica Ltd., Bayer AG, Biogen IDEC GmbH, Co. KG.
Celgene GmbH, Janssen-Cilag GmbH, LEO Pharma GmbH, Lilly
Deutschland GmbH, MSD Sharp & Dohme GmbH, Novartis
Pharma GmbH, Parexel International GmbH, Pfizer Deutschland
GmbH, and UCB Pharma GmbH. K.W. has received research Author Contributions
grants, travel grants, consulting honoraria, and/or lecturer hono-
raria from AbbVie Inc., AbbVie Deutschland GmbH & Co. KG, S.B., R.S., and S.S.-B.: substantial contributions to the concep-
Bayer Schering Pharma AG, Celgene GmbH, Flexopharm GmbH tion and design of the PIRANHA study. R.S. and G.K.: substantial
& Co. KG, Generon Corporation Ltd., Janssen Pharmaceutica NV, contributions to the conception or design of the manuscript. S.G.-
Johnson & Johnson Pharmaceutical Services LLC, Novartis Phar- K., S.B., and R.S.: substantial contributions to the acquisition of
ma GmbH, Pfizer Deutschland GmbH, and UCB Pharma GmbH. data for the manuscript. S.K., R.S., K.W., S.G.-K., and G.K.: sub-
S.S.-B. has received honoraria for participation in advisory boards, stantial contributions to the analysis and interpretation of data for
in clinical trials and/or as speaker from AbbVie Inc., AbbVie the manuscript. G.K., K.W., and R.S.: drafting the manuscript.
Deutschland GmbH & Co. KG, Novartis Pharma GmbH, and Pfiz- S.K., S.G.-K., S.S.-B., and S.B.: revising the manuscript critically for
er Deutschland GmbH. S.K. has no conflicts of interest to declare. important intellectual content. All authors finally approved the
S.G.-K. is an employee of AbbVie Deutschland GmbH & Co. KG. version to be published and agreed to be accountable for all aspects
S.B. is a former employee of AbbVie Deutschland GmbH & Co. of the work in ensuring that questions related to the accuracy or
KG. R.S. has received research grants, scientific awards, or hono- integrity of any part of the work are appropriately investigated and
raria for participation in advisory boards, clinical trials, or as resolved.
References
1 Sabat R, Jemec GB, Matusiak Ł, Kimball AB, Rev Endocr Metab Disord. 2016 Sep; 17(3): quality of life and professional activity. J Am
Prens E, Wolk K. Hidradenitis suppurativa. 335–41. Acad Dermatol. 2010;62(4):706–8.e1.
Nat Rev Dis Primers. 2020 Mar;6(1):18. 6 Horváth B, Janse IC, Sibbald GR. Pain man- 11 Sabat R, Chanwangpong A, Schneider-Burrus
2 Ingram JR, Jenkins-Jones S, Knipe DW, Mor- agement in patients with hidradenitis suppu- S, Metternich D, Kokolakis G, Kurek A, et al.
gan CL, Cannings-John R, Piguet V. Popula- rativa. J Am Acad Dermatol. 2015 Nov; 73(5 Increased prevalence of metabolic syndrome
tion-based Clinical Practice Research Data- Suppl 1):S47–51. in patients with acne inversa. PLoS One. 2012;
link study using algorithm modelling to iden- 7 Wolkenstein P, Loundou A, Barrau K, Auqui- 7(2):e31810.
tify the true burden of hidradenitis er P, Revuz J; Quality of Life Group of the 12 Miller IM, Ellervik C, Vinding GR, Zarchi K,
suppurativa. Br J Dermatol. 2018 Apr;178(4): French Society of Dermatology. Quality of life Ibler KS, Knudsen KM, et al. Association of
917–24. impairment in hidradenitis suppurativa: a metabolic syndrome and hidradenitis suppu-
3 Kromann CB, Deckers IE, Esmann S, Boer J, study of 61 cases. J Am Acad Dermatol. 2007 rativa. JAMA Dermatol. 2014 Dec; 150(12):
Prens EP, Jemec GB. Risk factors, clinical Apr;56(4):621–3. 1273–80.
course and long-term prognosis in hidradeni- 8 Kurek A, Peters EM, Chanwangpong A, Sabat 13 Egeberg A, Gislason GH, Hansen PR. Risk of
tis suppurativa: a cross-sectional study. Br J R, Sterry W, Schneider-Burrus S. Profound major adverse cardiovascular events and all-
Dermatol. 2014 Oct;171(4):819–24. disturbances of sexual health in patients with cause mortality in patients with hidradenitis
4 Garg A, Papagermanos V, Midura M, Strunk acne inversa. J Am Acad Dermatol. 2012; suppurativa. JAMA Dermatol. 2016 Apr;
A. Incidence of hidradenitis suppurativa 67(3):422–8.e1. 152(4):429–34.
among tobacco smokers: a population-based 9 Schneider-Burrus S, Jost A, Peters EM, Witte- 14 Richette P, Molto A, Viguier M, Dawidowicz
retrospective analysis in the U.S.A. Br J Der- Haendel E, Sterry W, Sabat R. Association of K, Hayem G, Nassif A, et al. Hidradenitis sup-
matol. 2018 Mar;178(3):709–14. hidradenitis suppurativa with body image. purativa associated with spondyloarthritis –
5 Karagiannidis I, Nikolakis G, Sabat R, JAMA Dermatol. 2018 Apr;154(4):447–51. results from a multicenter national prospec-
Zouboulis CC. Hidradenitis suppurativa/ 10 Matusiak L, Bieniek A, Szepietowski JC. Hi- tive study. J Rheumatol. 2014 Mar;41(3):490–
Acne inversa: an endocrine skin disorder? dradenitis suppurativa markedly decreases 4.
Delayed Diagnosis of Hidradenitis Dermatology 9
Suppurativa DOI: 10.1159/000508787
15 Schneider-Burrus S, Witte-Haendel E, Chris- 21 Wolk K, Wenzel J, Tsaousi A, Witte-Händel 27 Loget J, Saint-Martin C, Guillem P, Kanaga-
tou D, Rigoni B, Sabat R, Diederichs G. High E, Babel N, Zelenak C, et al. Lipocalin-2 is ex- ratnam L, Becherel PA, Nassif A, et al.; sous
prevalence of back pain and axial spondyloar- pressed by activated granulocytes and kerati- l’égide de « ResoVerneil ». [Misdiagnosis of
thropathy in patients with hidradenitis sup- nocytes in affected skin and reflects disease hidradenitis suppurativa continues to be a
purativa. Dermatology. 2016;232(5):606–12. activity in acne inversa/hidradenitis suppura- major issue. The R-ENS Verneuil study]. Ann
16 Wolk K, Warszawska K, Hoeflich C, Witte E, tiva. Br J Dermatol. 2017 Nov; 177(5): 1385– Dermatol Venereol. 2018 May;145(5):331–8.
Schneider-Burrus S, Witte K, et al. Deficiency 93. 28 Sabat R, Wolk K, Loyal L, Döcke WD, Ghore-
of IL-22 contributes to a chronic inflamma- 22 Tsaousi A, Witte E, Witte K, Röwert-Huber schi K. T cell pathology in skin inflammation.
tory disease: pathogenetic mechanisms in HJ, Volk HD, Sterry W, et al. MMP8 is in- Semin Immunopathol. 2019 May; 41(3): 359–
acne inversa. J Immunol. 2011 Jan; 186(2): creased in lesions and blood of acne inversa 77.
1228–39. patients: a potential link to skin destruction 29 Ritz JP, Runkel N, Haier J, Buhr HJ. Extent of
17 van der Zee HH, de Ruiter L, van den Broecke and metabolic alterations. Mediators In- surgery and recurrence rate of hidradenitis
DG, Dik WA, Laman JD, Prens EP. Elevated flamm. 2016;2016:4097574. suppurativa. Int J Colorectal Dis. 1998; 13(4):
levels of tumour necrosis factor (TNF)-α, in- 23 Boehncke WH. Systemic inflammation and 164–8.
terleukin (IL)-1β and IL-10 in hidradenitis cardiovascular comorbidity in psoriasis pa- 30 Khalsa A, Liu G, Kirby JS. Increased utiliza-
suppurativa skin: a rationale for targeting tients: causes and consequences. Front Im- tion of emergency department and inpatient
TNF-α and IL-1β. Br J Dermatol. 2011 Jun; munol. 2018 Apr;9:579. care by patients with hidradenitis suppurati-
164(6):1292–8. 24 Elnabawi YA, Dey AK, Goyal A, Groenendyk va. J Am Acad Dermatol. 2015 Oct;73(4):609–
18 Hessam S, Sand M, Gambichler T, Skrygan M, JW, Chung JH, Belur AD, et al. Coronary ar- 14.
Rüddel I, Bechara FG. Interleukin-36 in hi- tery plaque characteristics and treatment with 31 Piaserico S, Osto E, Famoso G, Zanetti I, Gre-
dradenitis suppurativa: evidence for a distinc- biologic therapy in severe psoriasis: results gori D, Poretto A, et al. Treatment with tumor
tive proinflammatory role and a key factor in from a prospective observational study. Car- necrosis factor inhibitors restores coronary
the development of an inflammatory loop. Br diovasc Res. 2019 Mar;115(4):721–8. microvascular function in young patients
J Dermatol. 2018 Mar;178(3):761–7. 25 Taams LS, Steel KJ, Srenathan U, Burns LA, with severe psoriasis. Atherosclerosis. 2016
19 Lima AL, Karl I, Giner T, Poppe H, Schmidt Kirkham BW. IL-17 in the immunopathogen- Aug;251:25–30.
M, Presser D, et al. Keratinocytes and neutro- esis of spondyloarthritis. Nat Rev Rheumatol. 32 Theut Riis P, Thorlacius L, Knudsen List E,
phils are important sources of proinflamma- 2018 Aug;14(8):453–66. Jemec GB. A pilot study of unemployment in
tory molecules in hidradenitis suppurativa. Br 26 Saunte DM, Boer J, Stratigos A, Szepietowski patients with hidradenitis suppurativa in
J Dermatol. 2016 Mar;174(3):514–21. JC, Hamzavi I, Kim KH, et al. Diagnostic de- Denmark. Br J Dermatol. 2017 Apr; 176(4):
20 Witte-Händel E, Wolk K, Tsaousi A, Irmer lay in hidradenitis suppurativa is a global 1083–5.
ML, Mößner R, Shomroni O, et al. The IL-1 problem. Br J Dermatol. 2015 Dec; 173(6): 33 Deckers IE, Janse IC, van der Zee HH, Nijsten
pathway is hyperactive in hidradenitis suppu- 1546–9. T, Boer J, Horvath B, et al. Hidradenitis sup-
rativa and contributes to skin infiltration and purativa (HS) is associated with low socioeco-
destruction. J Invest Dermatol. 2019 Jun; nomic status (SES): a cross-sectional refer-
139(6):1294–305. ence study. J Am Acad Dermatol. 2016;75(4):
755–9.e1.
10 Dermatology Kokolakis et al.
DOI: 10.1159/000508787
You might also like
- Epidemiology Haemophilus DucreyiDocument8 pagesEpidemiology Haemophilus DucreyiIngeniería Alpa TelecomunicacionesNo ratings yet
- Disease Severity, Quality of Life and Health Care in Plaque-Type Psoriasis: A Multicenter Cross-Sectional Study in GermanyDocument7 pagesDisease Severity, Quality of Life and Health Care in Plaque-Type Psoriasis: A Multicenter Cross-Sectional Study in Germanymahmoud korieshNo ratings yet
- Features Associated With Quality of Life Impairment in Hidradenitis Suppurativa PatientsDocument9 pagesFeatures Associated With Quality of Life Impairment in Hidradenitis Suppurativa PatientsFRESYA CHALISSANo ratings yet
- JCM 10 00797Document11 pagesJCM 10 00797alazarNo ratings yet
- Chemo Induced HFSDocument7 pagesChemo Induced HFSjames njengaNo ratings yet
- JR Alergi 4Document7 pagesJR Alergi 4ellafinarsihNo ratings yet
- PIIS1201971220305543Document6 pagesPIIS1201971220305543favorendaNo ratings yet
- Hidradenitis 3Document11 pagesHidradenitis 3Yudia MahardikaNo ratings yet
- Fitzgerald 2019Document10 pagesFitzgerald 2019senkonenNo ratings yet
- Uncertainty and COVID-19Document6 pagesUncertainty and COVID-19Arthur FernandesNo ratings yet
- DescargaDocument2 pagesDescargaAdriana Santander OliveraNo ratings yet
- Knowledge, Attitudes, and Practices (KAP) of Healthcare Workers On Viral Hepatitis B and Its Vaccination in 12 Health Establishments in The Centre Region of CameroonDocument8 pagesKnowledge, Attitudes, and Practices (KAP) of Healthcare Workers On Viral Hepatitis B and Its Vaccination in 12 Health Establishments in The Centre Region of CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 7 (2) - Aboul Naga-2022-Behçet Uveitis - Current PracticeDocument16 pages7 (2) - Aboul Naga-2022-Behçet Uveitis - Current Practicekueiying.suNo ratings yet
- Ol 20 1 441 PDFDocument7 pagesOl 20 1 441 PDFeka satyani belinaNo ratings yet
- Psoriasis A Comprehensive Review On The AetiopathoDocument29 pagesPsoriasis A Comprehensive Review On The AetiopathoGregorius HocevarNo ratings yet
- Ajbsr MS Id 001564Document3 pagesAjbsr MS Id 001564Rodrigo AlpizarNo ratings yet
- Risk Factors For Herpes Zoster Infection: A Meta-Analysis: Review ArticleDocument8 pagesRisk Factors For Herpes Zoster Infection: A Meta-Analysis: Review Articleyenny handayani sihiteNo ratings yet
- Article 6Document8 pagesArticle 6Yasmine SlhNo ratings yet
- Tuberculosis Thesis IntroductionDocument8 pagesTuberculosis Thesis Introductionifywpqvcf100% (2)
- Guidline NTM 2020Document36 pagesGuidline NTM 2020irfanNo ratings yet
- Value of Epi Research in Clinical PracticeDocument6 pagesValue of Epi Research in Clinical PracticeFouzia ShariqNo ratings yet
- BEDsoresDocument9 pagesBEDsoresGeoffrey KimaniNo ratings yet
- COVID-19: Guidance On Palliative Care From A European Respiratory Society International Task ForceDocument13 pagesCOVID-19: Guidance On Palliative Care From A European Respiratory Society International Task ForceRahmanu ReztaputraNo ratings yet
- EpuizareDocument4 pagesEpuizareMaria-Emanuela SultanaNo ratings yet
- Geriatric Syndromes: How To Treat: ReviewDocument9 pagesGeriatric Syndromes: How To Treat: ReviewAdrian TambunNo ratings yet
- Exploring The Risk of SevereDocument3 pagesExploring The Risk of Severexc_corinaNo ratings yet
- Jurnal Ing MK 4Document10 pagesJurnal Ing MK 4Iffah AlhikmahNo ratings yet
- Rodrigues 2017Document13 pagesRodrigues 2017Luisa LopezNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Usesfulness of Monocyte Distributions Width MDWDocument5 pagesUsesfulness of Monocyte Distributions Width MDWWilliam AlvaradoNo ratings yet
- Ciz 1197Document8 pagesCiz 1197Lindia PrabhaswariNo ratings yet
- The Evidence Supporting The Revised EORTC-MSGERC Definitions For Invasive Fungal InfectionsDocument2 pagesThe Evidence Supporting The Revised EORTC-MSGERC Definitions For Invasive Fungal Infectionsgwyneth.green.512No ratings yet
- Ofa 0020 0001Document14 pagesOfa 0020 0001Atenea Laboratorios Microbiología ClínicaNo ratings yet
- 2018 Article 276Document8 pages2018 Article 276Lulu NurainiNo ratings yet
- PIIS1198743X16000094Document10 pagesPIIS1198743X16000094ضحى الغزيNo ratings yet
- The Potential Role of Artificial Intelligence in The Clinical Management of Hansen's Disease (Leprosy)Document7 pagesThe Potential Role of Artificial Intelligence in The Clinical Management of Hansen's Disease (Leprosy)mloureiro17No ratings yet
- Rare Diseases Epidemiology PDFDocument565 pagesRare Diseases Epidemiology PDFRoland KristoNo ratings yet
- Ofad 488Document8 pagesOfad 488fahaxa7201No ratings yet
- The Impact of The COVID-19 Pandemic On The MentalDocument5 pagesThe Impact of The COVID-19 Pandemic On The MentalDAGOBERTO COPETE MOSQUERANo ratings yet
- Changes in Appendicitis Treatment During The COVID-19 PandemicDocument13 pagesChanges in Appendicitis Treatment During The COVID-19 PandemicCarla GarcíaNo ratings yet
- Microbiology of Diabetic Foot InfectionsDocument13 pagesMicrobiology of Diabetic Foot InfectionsFida MuhammadNo ratings yet
- Clinically Relevant Mycoses: A Practical ApproachFrom EverandClinically Relevant Mycoses: A Practical ApproachElisabeth PresterlNo ratings yet
- Modern Approaches To The Treatment of Viral Stomatitis in ChildrenDocument5 pagesModern Approaches To The Treatment of Viral Stomatitis in ChildrenCentral Asian StudiesNo ratings yet
- Jof 06 00216 v2Document18 pagesJof 06 00216 v2Grace Yuni Soesanti MhNo ratings yet
- Global Report: On The Epidemiology and Burden of SepsisDocument56 pagesGlobal Report: On The Epidemiology and Burden of Sepsisb6q77cjwwcNo ratings yet
- Mortality and The Use of Antithrombotic Therapies Among Nursing Home Residents With COVID-19Document6 pagesMortality and The Use of Antithrombotic Therapies Among Nursing Home Residents With COVID-19Shone DayNo ratings yet
- Tele 2Document10 pagesTele 2Sajin AlexanderNo ratings yet
- Adherence To Pharmacological Treatment of Systemic Arterial Hypertension in Primary CareDocument6 pagesAdherence To Pharmacological Treatment of Systemic Arterial Hypertension in Primary CarePriyanka KilaniyaNo ratings yet
- Etiology of Cellulitis and Clinical Prediction of Streptococcal Disease: A Prospective StudyDocument9 pagesEtiology of Cellulitis and Clinical Prediction of Streptococcal Disease: A Prospective StudyNurul Dwi LestariNo ratings yet
- Design and Implementation of Online Covid-19 Testing: KeywordsDocument6 pagesDesign and Implementation of Online Covid-19 Testing: KeywordslekanNo ratings yet
- DR - GulsivDocument5 pagesDR - GulsivPravin SurendranNo ratings yet
- Emergency Department Management of Cellulitis and Other Skin andDocument24 pagesEmergency Department Management of Cellulitis and Other Skin andJesus CedeñoNo ratings yet
- LancetDocument11 pagesLancetvieira.beatrizNo ratings yet
- MainDocument16 pagesMainrosarioaliaga2609No ratings yet
- Sepsis Abdominal ScoreDocument8 pagesSepsis Abdominal ScoreMaria Ocotlan Gonzalez herreraNo ratings yet
- International Journal of SurgeryDocument12 pagesInternational Journal of SurgeryNadya PutriNo ratings yet
- Morbidity and Aging in HIV-Infected Persons: The Swiss HIV Cohort StudyDocument10 pagesMorbidity and Aging in HIV-Infected Persons: The Swiss HIV Cohort StudyStefania CristinaNo ratings yet
- Study of Haematological Biochemical Profile and CLDocument8 pagesStudy of Haematological Biochemical Profile and CLNandani NarineNo ratings yet
- Sépsis em Pacientes Neurovascular Focus On Infection and Sepsis in Intensive Care PatientsDocument3 pagesSépsis em Pacientes Neurovascular Focus On Infection and Sepsis in Intensive Care PatientsEdson MarquesNo ratings yet
- WSES/GAIS/SIS-E/WSIS/AAST Global Clinical Pathways For Patients With Intra-Abdominal InfectionsDocument48 pagesWSES/GAIS/SIS-E/WSIS/AAST Global Clinical Pathways For Patients With Intra-Abdominal InfectionsMarisol López HernándezNo ratings yet
- Emergency ManagementDocument78 pagesEmergency ManagementHuey Calabines50% (2)
- Madeleine Leininger and The Transcultural Theory of NursingDocument8 pagesMadeleine Leininger and The Transcultural Theory of NursingTommy PangandahengNo ratings yet
- Blood and Marrow Transplant:: Resident Education Lecture SeriesDocument30 pagesBlood and Marrow Transplant:: Resident Education Lecture SeriesAparna KinginiNo ratings yet
- Cataract PDFDocument8 pagesCataract PDFeashelNo ratings yet
- Ngoa, Jose Troy - Sas3Document7 pagesNgoa, Jose Troy - Sas3Ella AroNo ratings yet
- Student Nurse Cover Letter SampleDocument3 pagesStudent Nurse Cover Letter SampleZeleen Ann Saberon100% (1)
- Semper Fit Advance Fitness CourseDocument255 pagesSemper Fit Advance Fitness CourseUnited States Militia73% (11)
- Hajj A Bio Mechanical JourneyDocument7 pagesHajj A Bio Mechanical Journeyrizla67No ratings yet
- Powerpoint Presentation On Eating DisordersDocument52 pagesPowerpoint Presentation On Eating DisordersNirdesh MagarNo ratings yet
- Case Digests in Legal MedicineDocument19 pagesCase Digests in Legal MedicineLenette LupacNo ratings yet
- Artikel Latihan Fisik Untuk Low Back PainDocument8 pagesArtikel Latihan Fisik Untuk Low Back Painvanny fabiantiNo ratings yet
- Pathophysiology DKADocument2 pagesPathophysiology DKALovely CacapitNo ratings yet
- Synthesis Paper David Lee PDocument17 pagesSynthesis Paper David Lee Papi-610188683No ratings yet
- B. Natural History of Disease WorksheetDocument3 pagesB. Natural History of Disease WorksheetYahya MoralesNo ratings yet
- College of Human Kinetics: Cagayan State UniversityDocument4 pagesCollege of Human Kinetics: Cagayan State UniversityJulieanne Garcia MaldaNo ratings yet
- TABLE 160-9: Treatment of DermatophytesDocument11 pagesTABLE 160-9: Treatment of DermatophytesIrsa SevenfoldismNo ratings yet
- Donnelly Ann Weebly ResumeDocument5 pagesDonnelly Ann Weebly Resumeapi-456585994No ratings yet
- Homeopathy For Memory and ConcentrationDocument5 pagesHomeopathy For Memory and Concentrationshashi_gadadNo ratings yet
- Cerebral Palsy Care Giving GuideDocument511 pagesCerebral Palsy Care Giving GuideJoel OntiverosNo ratings yet
- Hospital Annual Work Plan Format FinalDocument28 pagesHospital Annual Work Plan Format FinalSila Ontita100% (9)
- Mom-20 03 2024Document7 pagesMom-20 03 2024smn.ussharNo ratings yet
- Inv PedDocument55 pagesInv PedrapayrapayNo ratings yet
- Noetic ScienceDocument3 pagesNoetic ScienceMiguel DomingoNo ratings yet
- Approved Harmonized National RD Agenda 2017-2022 PDFDocument90 pagesApproved Harmonized National RD Agenda 2017-2022 PDFJoemel Bautista100% (1)
- BSC English Notes NewDocument54 pagesBSC English Notes NewFahad HabibNo ratings yet
- Hospital Designing and PlanningDocument55 pagesHospital Designing and PlanningSiddharthh Nutan Gokani81% (27)
- Admission and DischargeDocument14 pagesAdmission and DischargeDaryl Adrian Recaido100% (1)
- Communication Studies I.ADocument11 pagesCommunication Studies I.ABrandon J. Basdeo70% (30)
- The Features and Benefits of Broiler Starter Feeds That Include Alphasoy™Document31 pagesThe Features and Benefits of Broiler Starter Feeds That Include Alphasoy™Matute SalmonNo ratings yet
- Practical Exercise 3 Pareto Diagram: DR Yousef Amer - School of Engineering University of South Australia Page 1 of 3Document6 pagesPractical Exercise 3 Pareto Diagram: DR Yousef Amer - School of Engineering University of South Australia Page 1 of 3HarisNo ratings yet