Professional Documents
Culture Documents
Posterior Interosseus Palsy With An Incidental Froment-Rauber Nerve Presenting As Pseudoclaw Hand
Uploaded by
emilio9fernandez9gatOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Posterior Interosseus Palsy With An Incidental Froment-Rauber Nerve Presenting As Pseudoclaw Hand
Uploaded by
emilio9fernandez9gatCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/230784705
Posterior Interosseus Palsy with an Incidental Froment-Rauber Nerve
Presenting as a Pseudoclaw Hand
Article in Hand · September 2011
DOI: 10.1007/s11552-011-9342-8 · Source: PubMed
CITATIONS READS
4 171
3 authors, including:
Bev Guo John A I Grossman
Case Western Reserve University School of Medicine Miami Children's Hospital
4 PUBLICATIONS 155 CITATIONS 116 PUBLICATIONS 1,713 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by John A I Grossman on 20 May 2014.
The user has requested enhancement of the downloaded file.
HAND (2011) 6:344–347
DOI 10.1007/s11552-011-9342-8
CASE REPORTS
Posterior interosseus palsy with an incidental
Froment–Rauber nerve presenting as a pseudoclaw hand
Bev Y. Guo & D. R. Ayyar & John A. I. Grossman
Published online: 21 May 2011
# American Association for Hand Surgery 2011
Introduction interphalangeal joints. He was given the presumptive
diagnosis of an ulnar palsy. Prior to the onset of hand
Anatomic variations of peripheral nerves are well recog- weakness, there were previous episodes of elbow pain that
nized and reported in literature [4]. It is important to resolved without sequelae. He was referred to a hand
understand these variations because they can explain surgeon. Initial physical examination was notable for
unusual clinical deficits or findings. The Froment–Rauber clawing of the middle, ring, and small digits (Fig. 1) with
nerve is a distal continuation of the motor branch of the full passive mobility. Additionally, he had subtle weakness
posterior interosseous nerve, which innervates the first of the wrist and extrinsic digit extensors as well as of the
dorsal interosseus muscle. This report discusses a case of extensor pollicis longis and the abductor pollicis longus. He
this rare anomalous connection that initially confused the denied any sensory changes but slightly decreased protec-
diagnosis of a posterior interosseus palsy. tive sensibility was noted in the ulnar nerve distribution by
Semmes–Weinstein monofilament testing (3.61), including
the dorsal ulnar cutaneous nerve. A mildly positive Tinel’s
Case Report sign over the ulnar nerve at the elbow was detected.
Nonoperative treatments of splinting and nonsteroidal anti-
A 17-year-old left-hand dominant baseball pitcher pre- inflammatory agents had been attempted and had failed to
sented with an 8-month history of progressive pain in his improve his symptoms.
left proximal forearm and elbow. His symptoms proceeded Electrodiagnostic studies (nerve conduction and electro-
to subjective weakness of the small finger that progressed myography (EMG)) were consistent with a posterior
radially to include the ring and middle fingers with interosseous nerve (PIN) neuropathy. These findings in-
posturing in flexion at the metacarpal−phalangeal and cluded denervation in the extensor carpi ulnaris and first
dorsal interosseus with complex repetitive discharges in the
latter. The number of motor units in all muscles innervated
B. Y. Guo : J. A. I. Grossman by the posterior interosseus nerve as well as in the first
Department of Orthopaedic Surgery,
dorsal interosseus were decreased. Nerve conduction
NYU Hospital for Joint Diseases,
New York, NY, USA studies of the median and ulnar nerves were normal,
including the amplitude of the thenar and hypothenar
D. R. Ayyar compound action potentials. The amplitude of the extensor
Department of Neurology, University of Miami,
indicis proprius compound muscle action potential was
Miami, FL, USA
significantly decreased. Notable is that although no neuro-
J. A. I. Grossman (*) physiologic evidence of ulnar nerve pathology was found at
Brachial Plexus and Peripheral Nerve Program, the elbow or wrist, evidence of denervation was noted in
Miami Children’s Hospital,
his first dorsal interosseus muscle on EMG. A complete
8940 N. Kendall Drive, Suite 904E,
Miami, FL 33176, USA neurological evaluation including magnetic resonance im-
e-mail: drg@handandnervespecialist.com aging of the brain, cervical spine, elbow, and forearm were
HAND (2011) 6:344–347 345
Twenty minutes after tourniquet release, intraoperative
nerve stimulation of both the radial and ulnar nerves with
recording from the first dorsal interosseus and hypothenar
muscles was performed. Stimulation of the radial nerve
showed activity in the first dorsal interosseus (Fig. 3a),
whereas stimulation of the ulnar nerve had a response only
in the hypothenar muscle (Fig. 3b). At 2-month follow-up,
the patient had full recovery of his PIN motor and ulnar
sensory deficits (Fig. 4a, b).
Fig. 1 Preoperative view
Discussion
normal. Subsequent clinical examinations confirmed mild
sensory changes in the ulnar nerve distribution by Semmes– Anomalous innervation of the first dorsal interosseus
Weinstein monofilament testing (3.61). Motor weakness in muscle by the radial nerve is known as the Froment–
the wrist and finger extensors also remained constant, with Rauber nerve, and this explains the finding of first dorsal
persistent clawing. He was diagnosed with a possible ulnar interosseus muscle denervation on the preoperative EMG. It
neuropathy and definite PIN compression syndrome. is probably unrelated to the digital clawing (pseudoclaw)
Operative exploration was performed. described with a PIN palsy seen in this patient [8, 9]. The
During surgery, the ulnar nerve was first exposed at the Froment–Rauber nerve is a distal continuation of the PIN
elbow. Only a limited area of subtle external compression with that innervates the first and often second and third dorsal
small fibrous bands was seen and released at the medial interosseous muscle. Froment [2] first described the distal
epicondyle. Next, the posterior interosseous nerve decompres- continuation of the PIN, and Rauber [7] also reported a
sion was performed using a standard volar forearm approach. similar finding. Spinner [8] referred to this anomalous
The radial nerve was identified proximally and traced distally connection as the Froment–Rauber nerve. Previously,
to locate the superficial radial sensory nerve and the posterior Bichat [1] also had described a distal communication of
interosseous nerve. Mild fibrosis visually compressing the the PIN with the deep branch of the ulnar nerve.
superficial radial nerve was seen and released with some nerve Compression of the PIN can occur anywhere along its
expansion noted. As the posterior interosseous nerve was anatomic course by extrinsic or intrinsic factors. Reported
mobilized at the tendinous arch at the supinator, significant extrinsic causes include ganglion cysts, lipomas, and frac-
compression was encountered. The fibrous supinator arch was tures. Intrinsic compression involves fibrous bands at the
thickened with a circumferential constriction (Fig. 2a). Release radiocapitellar joint, large blood vessels known as the leash of
of the supinator fascia and tendon with a limited myotomy Henry, a leading proximal tendinous edge of the extensor
was then performed (Fig. 2b). carpi radialis brevis, and the Arcade of Froshe [3, 9]. This
Fig. 2 Intraoperative view of
site of PIN compression: a pre-
release and b post-release
346 HAND (2011) 6:344–347
weak or absent [11]. Because of the soft clinical findings
(Tinel’s, sensory changes) of cubital tunnel syndrome in
this patient, the digital posturing was initially considered as
a result of a mild ulnar palsy. The clawing of the middle
finger, however, is not explained by an isolated ulnar palsy.
Additionally, the MP posture of all the involved digits was
relatively neutral. Intraoperative neurophysiological find-
ings confirmed, in fact, the presence of radial innervation of
the first dorsal interosseus and explained the preoperative
EMG findings of that muscle that directly are, in fact,
related to the previous diagnosis of a PIN compression.
Involvement of the second and third interosseus muscles
was not demonstrated and would not in any event explain
the hand deformity that is an example of the “pseudoclaw.”
The incidence of the Froment–Rauber nerve is unclear.
A study looking at the anatomic variations of the course of
the PIN in the forearm was performed on both arms of 29
cadavers [5]. Only one specimen was described to have the
Froment–Rauber nerve, with the PIN terminal branch
entering the third dorsal interosseous muscle [5]. This
would set the incidence of this anomalous connection at
3.4%. Another cadaveric study, however, using immuno-
histochemical analysis of PIN motor axons found 28.5% of
specimens terminated in the muscles of the first web space
Fig. 3 a, b Intraoperative muscle recordings
[6]. This is similar to the reported incidence of the more
recognized Martin–Gruber (ulnar–median) anastomosis.
latter site refers to the proximal edge of the supinator, which Technical differences in assessing the termination of the
is the most common site of compression [10]. PIN nerve may account for the variability in the reported
Symptoms of posterior interosseous syndrome may numbers. Even so, the prevalence of the Froment–Rauber
include partial or complete paralysis of the muscles nerve may not be as rare as previously thought.
innervated by the PIN. Lack of finger extension at the The significant incidence of both median and radial
metacarpophalangeal joints and thumb extension is noted nerve anastomosis to the ulnar nerve highlights the
with complete paralysis. The wrist extends in a dorsal radial importance of understanding the muscular innervations of
direction due to unopposed extensor carpi radialis longus the ulnar nerve during a clinical exam. This redundancy in
action. When the compression is progressive and first the neural connections sometimes allows for the mainte-
involves the small finger, progressing radially, the appear- nance of some hand intrinsic function even with the loss of
ance can mimic an ulnar palsy [9, 10]. This is the ulnar nerve function.
“pseudoclaw hand,” since there is no actual hyperextension A thorough understanding of various anomalous neural
at the metacarpal phalangeal joint as seen in an ulnar palsy connections in the upper extremity allows for interpretation
[8, 9]. In fact, extensor digitorum communis function is of potentially confusing clinical presentations in patients
Fig. 4 a, b Postoperative range
of motion
HAND (2011) 6:344–347 347
and help guide surgical treatment. Thought to be a rare 5. Missankov AA, Sehgal AK, Mennen U. Variations of the
posterior interosseous nerve. J Hand Surg Br. 2000;25(3):281–2.
finding, the Froment–Rauber nerve may actually be a more
6. Okwueze MI, Cardwell NL, Wolfort SL, Nanney LB. Unexpected
common variant whose incidence is underappreciated. motor axons in the distal superficial radial and posterior
interosseous nerves: A cadaver study. Clin Anat. 2007;20:790–4.
7. Rauber A. Vater’sche Korper der Bander – und Periostnerven.
References Munich: Inauug Diss; 1865.
8. Russell SM. Examination of peripheral nerve injuries: an
anatomical approach. New York: Thieme; 2006. p. 64.
1. Bichat X, Buisson MFR, Roux PJ. Societe de Nedecube (Sarthe 9. Spinner M. Injuries to the major branches of peripheral nerves of
France). Traite d’anatomie descriptive. Paris: Brosson Gabon the forearm. 2nd ed. Philadelphia: Saunders; 1978. p. 96–100.
libraire; 1801. 10. Spinner M. Management of nerve compression lesions of the
2. Froment JBF. Traite D’Anatomie Humaine. Paris: Mequignon- upper extremity. In: Omer Jr GE, Spinner M, editors. Management
Marvis; 1846. of peripheral nerve problems. Philadelphia: Saunders; 1980. p.
3. Lister GD, Belsole RB, Kleiner HE. The radial tunnel syndrome. J 521.
Hand Surg Am. 1979;4:52–9. 11. Tubiana R, Gilbert A, Leclercq C, Malek R. (eds.) (2009)
4. Matloub HS, Yousif NJ. Peripheral nerve anatomy and innervation Restoration of function in upper limb paralyses and muscular
pattern. Hand Clin. 1992;8:201–14. defects. Informa, New York. pp 248–249
View publication stats
You might also like
- Electromyography in CNS Disorders: Central EMGFrom EverandElectromyography in CNS Disorders: Central EMGBhagwan T. ShahaniNo ratings yet
- Riche-Cannieu Anastomosis With Partial Transection of The Median NerveDocument3 pagesRiche-Cannieu Anastomosis With Partial Transection of The Median NerveAdam L. SchreiberNo ratings yet
- Nerve Supply of The Human Knee and ItsDocument7 pagesNerve Supply of The Human Knee and ItsErnesto VillavicencioNo ratings yet
- Anterior Interosseous Nerve Paralysis Due To Gantzer's MuscleDocument3 pagesAnterior Interosseous Nerve Paralysis Due To Gantzer's MuscleJunji Miller FukuyamaNo ratings yet
- Compression of The Posterior Interosseous Nerve Sec 2024 International JournDocument4 pagesCompression of The Posterior Interosseous Nerve Sec 2024 International JournRonald QuezadaNo ratings yet
- Epi-Perineurial Anatomy, Innervation, and Axonal Nociceptive MechanismsDocument6 pagesEpi-Perineurial Anatomy, Innervation, and Axonal Nociceptive MechanismsPedro FonsecaNo ratings yet
- Saphenous Nerve EntrapmentDocument2 pagesSaphenous Nerve Entrapmentemilio9fernandez9gatNo ratings yet
- Mus 880170310Document5 pagesMus 880170310Gabriel JoséNo ratings yet
- Lipoma Causing A Posterior Interosseous Nerve Syndrome: Case ReportDocument3 pagesLipoma Causing A Posterior Interosseous Nerve Syndrome: Case ReportShashank SNo ratings yet
- 41-Article Text-59-1-10-20190211Document3 pages41-Article Text-59-1-10-20190211Faishol Reza AdiyaksaNo ratings yet
- Pure Trigeminal Motor Neuropathy: A Case Report: Clinical NoteDocument4 pagesPure Trigeminal Motor Neuropathy: A Case Report: Clinical Noteemilio9fernandez9gatNo ratings yet
- Biomechanics-Lumbar Facet Pain Biomechanics, Neuroanatomy and NeurophysiologyDocument13 pagesBiomechanics-Lumbar Facet Pain Biomechanics, Neuroanatomy and NeurophysiologyMuhammad FahmyNo ratings yet
- Jkns 45 57Document3 pagesJkns 45 57idelviceNo ratings yet
- Patella Dislocation Association With Drop Foot: Case ReportDocument2 pagesPatella Dislocation Association With Drop Foot: Case ReportekaNo ratings yet
- Innervation The Human Shoulder Joint and Its Implications For SurgeryDocument6 pagesInnervation The Human Shoulder Joint and Its Implications For SurgerymitroisergiuNo ratings yet
- Rodilla Inervación Tran2018 PDFDocument8 pagesRodilla Inervación Tran2018 PDFLore BarreraNo ratings yet
- Spinner 2003Document2 pagesSpinner 2003Hương HuỳnhNo ratings yet
- Knee Pain and The Infrapatellar Branch of The Saphenous: NerveDocument3 pagesKnee Pain and The Infrapatellar Branch of The Saphenous: NervefostizzNo ratings yet
- Case Report PeronealDocument10 pagesCase Report Peronealfi.afifah NurNo ratings yet
- Peroneal Nerve Palsy Following Acp TreatmentDocument3 pagesPeroneal Nerve Palsy Following Acp TreatmentLydwiNa JcNo ratings yet
- Changes of Extremity and Laryngeal Muscle Electromyographic Amplitudes After Intravenous Administration of Vecuronium00005537-200812000-00014Document5 pagesChanges of Extremity and Laryngeal Muscle Electromyographic Amplitudes After Intravenous Administration of Vecuronium00005537-200812000-00014dr.hungsonNo ratings yet
- Journal of Orthopaedics: B.T. Pushpa, Siddharth N. Aiyer, Muhil Kannan, Anupama Maheswaran, S. RajasekaranDocument2 pagesJournal of Orthopaedics: B.T. Pushpa, Siddharth N. Aiyer, Muhil Kannan, Anupama Maheswaran, S. RajasekaranmohNo ratings yet
- Cheesborough2014 PDFDocument5 pagesCheesborough2014 PDFGregorius Thomas PrasetiyoNo ratings yet
- Ulnar Nerve Compression at The Elbow Caused by A Prominent Medial Head of The Triceps and An Anconeus Epitrochlearis MuscleDocument3 pagesUlnar Nerve Compression at The Elbow Caused by A Prominent Medial Head of The Triceps and An Anconeus Epitrochlearis MuscleNicolas AdrianoNo ratings yet
- Sonographic Diagnosis of Nontraumatic Musculotendinous Rupture of Hamstring 2008 Journal of Medical UltrasoundDocument4 pagesSonographic Diagnosis of Nontraumatic Musculotendinous Rupture of Hamstring 2008 Journal of Medical UltrasoundIman Ru-ancaNo ratings yet
- Iatrogenic Damage To The Mandibular Nerves As AssessedDocument4 pagesIatrogenic Damage To The Mandibular Nerves As AssessedAndres Rojas JerezNo ratings yet
- Common Pathological Conditions Affecting Movement System Function - HadleyDocument40 pagesCommon Pathological Conditions Affecting Movement System Function - HadleywilliamadiwinataNo ratings yet
- Shoulder Dislocation TechniquesDocument9 pagesShoulder Dislocation TechniqueskenthepaNo ratings yet
- Musculocutaneous Nerve Substituting For The Distal Part of Radial Nerve: A Case Report and Its Embryological BasisDocument3 pagesMusculocutaneous Nerve Substituting For The Distal Part of Radial Nerve: A Case Report and Its Embryological Basis19AYUSHJAINXIISCINo ratings yet
- Systematic Ultrasound Identification of The Dorsal Scapular and Long Thoracic Nerves During Interscalene BlockDocument4 pagesSystematic Ultrasound Identification of The Dorsal Scapular and Long Thoracic Nerves During Interscalene BlockWidya AriatyNo ratings yet
- 15 Peripheral Nervous InjuryDocument8 pages15 Peripheral Nervous Injury楊畯凱No ratings yet
- Proximal Radial Compression Neuropathy: Brian Rinker, MD, Charles R. Effron, MD, and Robert W. Beasley, MDDocument7 pagesProximal Radial Compression Neuropathy: Brian Rinker, MD, Charles R. Effron, MD, and Robert W. Beasley, MDRod VRNo ratings yet
- Jurnal Reading Ortho 1Document6 pagesJurnal Reading Ortho 1midellialintinNo ratings yet
- 2 PDFDocument7 pages2 PDFDeei RizalNo ratings yet
- J Neurosurg Case Lessons Article CASE23218Document4 pagesJ Neurosurg Case Lessons Article CASE23218yesozmenNo ratings yet
- Telaah 1Document3 pagesTelaah 1anri albarruNo ratings yet
- Volkmann'S Ischemic Contracture - A Case Report: Jampa, Sunith Waghray & Lakshmana Prasad GaddeDocument8 pagesVolkmann'S Ischemic Contracture - A Case Report: Jampa, Sunith Waghray & Lakshmana Prasad GaddeTJPRC PublicationsNo ratings yet
- Peripheral Nerve Trauma: Mechanisms of Injury and RecoveryDocument44 pagesPeripheral Nerve Trauma: Mechanisms of Injury and RecoveryJa NetNo ratings yet
- J Jhsa 2017 10 014Document5 pagesJ Jhsa 2017 10 014Nicolas AdrianoNo ratings yet
- PIIS2589514123001214Document2 pagesPIIS2589514123001214abrariyy ma'hadiyyNo ratings yet
- Overview of Intraoperative Neurophysiological Monitoring During Spinal Surgery - 2016 PDFDocument7 pagesOverview of Intraoperative Neurophysiological Monitoring During Spinal Surgery - 2016 PDFAndrea RoesnerNo ratings yet
- Spasticity: Pathophysiology and Neural Control: Simon M. Danner, Milan R. DimitrijevicDocument6 pagesSpasticity: Pathophysiology and Neural Control: Simon M. Danner, Milan R. DimitrijevicDimas Gatra DiantoroNo ratings yet
- Contreras 1998Document7 pagesContreras 1998Hương HuỳnhNo ratings yet
- Entrapment of The Posterior Interosseous Nerve - Ax ArticleDocument9 pagesEntrapment of The Posterior Interosseous Nerve - Ax ArticleNaz HossNo ratings yet
- Clinical Anatomy of The Radial NerveDocument2 pagesClinical Anatomy of The Radial NervemmoslemNo ratings yet
- 1 s2.0 S1388245704000975 MainDocument12 pages1 s2.0 S1388245704000975 MainpashaNo ratings yet
- Management of Peroneal Nerve Paralysis in A Rottweiler PupDocument3 pagesManagement of Peroneal Nerve Paralysis in A Rottweiler PupDrMohd IQbal SoFiNo ratings yet
- OSULLIVAN y GLASS 2017 Cip Physitis A Fracture-In-An-English-BulldogDocument4 pagesOSULLIVAN y GLASS 2017 Cip Physitis A Fracture-In-An-English-BulldogWendy Gabriela Mayén AriasNo ratings yet
- Anatomy of Ulnar NerveDocument6 pagesAnatomy of Ulnar Nervelynn blackpinkNo ratings yet
- Acu Accident LumbarDocument2 pagesAcu Accident Lumbarrswongym449No ratings yet
- Fáscias Popliteo-MeniscaisDocument7 pagesFáscias Popliteo-MeniscaisDiana TeixeiraNo ratings yet
- Muscle Tone and JoinDocument12 pagesMuscle Tone and JoinomarihuanoNo ratings yet
- Pain Book FeinDocument102 pagesPain Book FeinHansen NielsNo ratings yet
- Sindrome Miofascial de Cuadriceps CruralDocument4 pagesSindrome Miofascial de Cuadriceps CruralyzniaNo ratings yet
- Fneur 12 661441Document17 pagesFneur 12 661441ChadiIbrahimNo ratings yet
- Ohtori 2018Document7 pagesOhtori 2018geowalker7092No ratings yet
- Thopaedic Science: JournalDocument16 pagesThopaedic Science: JournalCiro Madrid FloresNo ratings yet
- Role of Fasciae in Nonspecific Low Back Pain: Gulia Casato (1), Carla Stecco (2), Riccardo BusinDocument5 pagesRole of Fasciae in Nonspecific Low Back Pain: Gulia Casato (1), Carla Stecco (2), Riccardo BusinmarcelonorisNo ratings yet
- Functional Outcome of Tardy Ulnar Nerve Palsy Manifests 2024 InternationalDocument4 pagesFunctional Outcome of Tardy Ulnar Nerve Palsy Manifests 2024 InternationalRonald QuezadaNo ratings yet
- Explanation Using: Injuries PreviouslyDocument7 pagesExplanation Using: Injuries PreviouslyjannilshansenNo ratings yet
- EEG Signals and Wireless Transfer of EEG PDFDocument3 pagesEEG Signals and Wireless Transfer of EEG PDFemilio9fernandez9gatNo ratings yet
- An EEG Study of The Neurodevelopmental H PDFDocument1 pageAn EEG Study of The Neurodevelopmental H PDFemilio9fernandez9gatNo ratings yet
- Computerized EEG Monitoring PDFDocument8 pagesComputerized EEG Monitoring PDFemilio9fernandez9gatNo ratings yet
- EEG Changes Accompanying Learned Regulat PDFDocument10 pagesEEG Changes Accompanying Learned Regulat PDFemilio9fernandez9gatNo ratings yet
- FPG 007 CriticalCareinNeurology 2012 PDFDocument119 pagesFPG 007 CriticalCareinNeurology 2012 PDFOana HereaNo ratings yet
- Stable EEG Features: V. Stefanidis, G. Anogiannakis, A. Evangelou, and M. PoulosDocument9 pagesStable EEG Features: V. Stefanidis, G. Anogiannakis, A. Evangelou, and M. Poulosemilio9fernandez9gatNo ratings yet
- Complications of Posterior Cranial Fossa PDFDocument7 pagesComplications of Posterior Cranial Fossa PDFemilio9fernandez9gatNo ratings yet
- Cerebrovascular Disease Residents 2Document29 pagesCerebrovascular Disease Residents 2emilio9fernandez9gatNo ratings yet
- Hypoglossal Nerve Stimulation EMG FindinDocument1 pageHypoglossal Nerve Stimulation EMG Findinemilio9fernandez9gatNo ratings yet
- Clinical: Section 3 of 7Document13 pagesClinical: Section 3 of 7emilio9fernandez9gatNo ratings yet
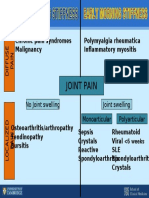
- Differential Diagnosis SlideDocument1 pageDifferential Diagnosis Slideemilio9fernandez9gatNo ratings yet
- Cerebrovascular Disease ResidentsDocument14 pagesCerebrovascular Disease Residentsemilio9fernandez9gatNo ratings yet
- Electromyography: IE 665 Dr. SenguptaDocument22 pagesElectromyography: IE 665 Dr. SenguptaIrawati HidayahNo ratings yet
- Cerebrovascular Disease Residents 1Document20 pagesCerebrovascular Disease Residents 1emilio9fernandez9gatNo ratings yet
- EEG - Basic Principles and Application in EpilepsyDocument19 pagesEEG - Basic Principles and Application in Epilepsyemilio9fernandez9gatNo ratings yet
- A Correlative Study of Quantitative EMG PDFDocument5 pagesA Correlative Study of Quantitative EMG PDFemilio9fernandez9gatNo ratings yet
- The Medial Calcaneal Nerve Anatomy and N PDFDocument7 pagesThe Medial Calcaneal Nerve Anatomy and N PDFemilio9fernandez9gatNo ratings yet
- Differnetial Diagnosis RadiculopathiesDocument58 pagesDiffernetial Diagnosis Radiculopathiesemilio9fernandez9gatNo ratings yet
- EMG Findings of Facial Muscles in ALS PDFDocument3 pagesEMG Findings of Facial Muscles in ALS PDFemilio9fernandez9gatNo ratings yet
- Comparison of Four Different Nerve Condu PDFDocument19 pagesComparison of Four Different Nerve Condu PDFemilio9fernandez9gatNo ratings yet
- Electrodiagnostic Reference Values For U PDFDocument7 pagesElectrodiagnostic Reference Values For U PDFemilio9fernandez9gatNo ratings yet
- Clinical/Scientific Notes: Schwab & England: Standardization of AdministrationDocument25 pagesClinical/Scientific Notes: Schwab & England: Standardization of Administrationemilio9fernandez9gatNo ratings yet
- Muscle Denervation and Nerve Entrapment PDFDocument9 pagesMuscle Denervation and Nerve Entrapment PDFemilio9fernandez9gatNo ratings yet
- An Unusual Case of Suprascapular NerveDocument3 pagesAn Unusual Case of Suprascapular Nerveemilio9fernandez9gatNo ratings yet
- A Systematic Review of Antibody Mediated Immunity COVID 19Document47 pagesA Systematic Review of Antibody Mediated Immunity COVID 19emilio9fernandez9gatNo ratings yet
- Utility of Elec Testing - ReaffirmedDocument7 pagesUtility of Elec Testing - Reaffirmedemilio9fernandez9gatNo ratings yet
- Saphenous Nerve EntrapmentDocument2 pagesSaphenous Nerve Entrapmentemilio9fernandez9gatNo ratings yet
- EMGLAB An Interactive EMG DecompositionDocument13 pagesEMGLAB An Interactive EMG Decompositionemilio9fernandez9gatNo ratings yet
- EMG GMed y Psoas1 PDFDocument10 pagesEMG GMed y Psoas1 PDFemilio9fernandez9gatNo ratings yet
- Saphenous Nerve Conduction in ManDocument12 pagesSaphenous Nerve Conduction in Manemilio9fernandez9gatNo ratings yet
- Tungul - Activity 1 Midterms (Pharmacology)Document6 pagesTungul - Activity 1 Midterms (Pharmacology)Ma. Rita Concepcion TungulNo ratings yet
- TetraciclinaDocument2 pagesTetraciclinaHernan GalleguillosNo ratings yet
- GST Exemptions DMFS 12Document51 pagesGST Exemptions DMFS 12Anjali Krishna SNo ratings yet
- BSNDocument5 pagesBSNNoriel GirayNo ratings yet
- Section 8. Renal Problems: 1. A. B. C. D. Ans: B PTS: 1 2. A. B. C. D. Ans: B PTS: 1 3Document8 pagesSection 8. Renal Problems: 1. A. B. C. D. Ans: B PTS: 1 2. A. B. C. D. Ans: B PTS: 1 3AliNo ratings yet
- Activity Intolerance NCPDocument7 pagesActivity Intolerance NCPamitNo ratings yet
- Chapter 27 Chest Injuries Final TermDocument4 pagesChapter 27 Chest Injuries Final Termluwi vitonNo ratings yet
- Hydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionDocument15 pagesHydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionElisha WorworNo ratings yet
- Respiratory Distress SyndromeDocument54 pagesRespiratory Distress SyndromeKristine CaringalNo ratings yet
- Vns 01092021Document28 pagesVns 01092021fanmingjinNo ratings yet
- Chapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusDocument10 pagesChapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusAgnieszka WisniewskaNo ratings yet
- Digestive Symptoms in COVID-19 Patients With Mild Disease SeverityDocument13 pagesDigestive Symptoms in COVID-19 Patients With Mild Disease SeveritytyariNo ratings yet
- Natural Medicines Comprehensive Database 2010Document26 pagesNatural Medicines Comprehensive Database 2010PsineticNo ratings yet
- Normal Neonate and General Exam of The Newborn MCH BukDocument94 pagesNormal Neonate and General Exam of The Newborn MCH BukAbdullahi Suleiman MakaNo ratings yet
- Konasana PoseDocument2 pagesKonasana PoseMIBNo ratings yet
- San Jiao Chap 12Document3 pagesSan Jiao Chap 12Bolt VoNo ratings yet
- 1n2 OrganicSD-drshakyaDocument26 pages1n2 OrganicSD-drshakyaUMESH KANDELNo ratings yet
- Acute Generalized Exanthematous Pustulosis: Sima HalevyDocument18 pagesAcute Generalized Exanthematous Pustulosis: Sima HalevyDody PrasetyaNo ratings yet
- Genetics Notes - Other Patterns of Inheritance & PedigreesDocument4 pagesGenetics Notes - Other Patterns of Inheritance & PedigreesJoseph Dav6657No ratings yet
- ECG InterpretationDocument6 pagesECG InterpretationANDREW DEL ROSARIONo ratings yet
- Meditations On Reserve Life, Biosociality, and The Taste of Non-SovereigntyDocument16 pagesMeditations On Reserve Life, Biosociality, and The Taste of Non-SovereigntyJacob SmithNo ratings yet
- Congenital Heart Disease: Education and Practice GapsDocument18 pagesCongenital Heart Disease: Education and Practice GapsAlvaro Ignacio Lagos SuilNo ratings yet
- Pulmonary Interventions-Page 1504: 1. Give at Least 3 Pulmonary Interventions For Cystic Fibrosis?Document3 pagesPulmonary Interventions-Page 1504: 1. Give at Least 3 Pulmonary Interventions For Cystic Fibrosis?ADOLF FRUELAN HIDALGONo ratings yet
- The History of Tuberculosis: From The First Historical Records To The Isolation of Koch's BacillusDocument4 pagesThe History of Tuberculosis: From The First Historical Records To The Isolation of Koch's BacillusGrace Meigawati IwantoNo ratings yet
- Angina Pectoris Pharmacological and Acupuncture TherapyDocument5 pagesAngina Pectoris Pharmacological and Acupuncture TherapyEditor IJTSRDNo ratings yet
- Pulses: Shu Chi HuanDocument1 pagePulses: Shu Chi HuanRicardo TeixeiraNo ratings yet
- PathoDocument2 pagesPathohrry stylesNo ratings yet
- RS ARI-Common Cold - PPT 93Document57 pagesRS ARI-Common Cold - PPT 93Dr.P.NatarajanNo ratings yet
- Co-Occurrence of Dissociative Identity Disorder and Borderline Personality DisorderDocument13 pagesCo-Occurrence of Dissociative Identity Disorder and Borderline Personality DisorderCarla MesquitaNo ratings yet
- The Language of AnatomyDocument7 pagesThe Language of AnatomyLinziJaeOnelNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)