Professional Documents
Culture Documents
Sellitto 2021
Uploaded by
JudybenavidesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sellitto 2021
Uploaded by
JudybenavidesCopyright:
Available Formats
Expert Review of Pharmacoeconomics & Outcomes
Research
ISSN: (Print) (Online) Journal homepage: https://www.tandfonline.com/loi/ierp20
Outcome measures for physical fatigue in
individuals with multiple sclerosis: a systematic
review
Giovanni Sellitto, Alessia Morelli, Susanna Bassano, Antonella Conte, Viola
Baione, Giovanni Galeoto & Anna Berardi
To cite this article: Giovanni Sellitto, Alessia Morelli, Susanna Bassano, Antonella Conte, Viola
Baione, Giovanni Galeoto & Anna Berardi (2021): Outcome measures for physical fatigue in
individuals with multiple sclerosis: a systematic review, Expert Review of Pharmacoeconomics &
Outcomes Research, DOI: 10.1080/14737167.2021.1883430
To link to this article: https://doi.org/10.1080/14737167.2021.1883430
Accepted author version posted online: 28
Jan 2021.
Submit your article to this journal
Article views: 53
View related articles
View Crossmark data
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=ierp20
Publisher: Taylor & Francis & Informa UK Limited, trading as Taylor & Francis Group
Journal: Expert Review of Pharmacoeconomics & Outcomes Research
DOI: 10.1080/14737167.2021.1883430
Outcome measures for physical fatigue in individuals with multiple sclerosis: a systematic
review
T
IP
Giovanni Sellitto1, Alessia Morelli1 , Susanna Bassano1, Antonella Conte2,3, Viola Baione2,
R
Giovanni Galeoto2 , Anna Berardi2
SC
1. Sapienza University of Rome, Piazzale Aldo Moro 5, 00185, Rome, Italy
U
2. Department of Human Neurosciences, Sapienza University of Rome, Piazzale Aldo Moro 5,
AN
00185, Rome, Italy
3. IRCCS Neuromed Pozzili, Italy
M
D
TE
*Corresponding author:
EP
Galeoto Giovanni
C
Viale dell’Università 30, Rome
AC
Email: giovanni.galeoto@uniroma1.it
Outcome measures for physical fatigue in individuals with multiple sclerosis: a systematic
review
Information Classification: General
Giovanni Sellitto1, Alessia Morelli1 , Susanna Bassano1, Antonella Conte2,3, Viola Baione2,
Giovanni Galeoto2 , Anna Berardi2
4. Sapienza University of Rome, Piazzale Aldo Moro 5, 00185, Rome, Italy
5. Department of Human Neurosciences, Sapienza University of Rome, Piazzale Aldo Moro 5,
00185, Rome, Italy
T
6. IRCCS Neuromed Pozzili, Italy
IP
R
SC
*Corresponding author:
U
AN
Galeoto Giovanni
Department of Human Neurosciences, Sapienza University of Rome, Piazzale Aldo Moro 5, 00185,
M
Rome, Italy
D
Email: giovanni.galeoto@uniroma1.it
TE
EP
C
AC
ABSTRACT
Introduction: Physical fatigue can be a common reason for early retirement or sick leave since it
appears in the earliest stages of multiple sclerosis (MS). Therefore, a prompt and accurate diagnosis
is essential. This systematic review aims to identify and describe the instruments used to assess
Information Classification: General
physical fatigue in MS patients with consideration for the languages used to validate the instruments
and their methodological qualities.
Area covered: This study has been carried out through “Medline,” “Scopus,” “Cinhal,” and “Web
of Science” databases for all the papers published before January 24, 2020. Three independent
authors have chosen the eligible studies based upon pre-set criteria of inclusion. Data collection,
T
data items, and assessment of the risk of bias: the data extraction approach was chosen based on the
IP
Cochrane Methods. For data collection, the authors followed the recommendations from the
R
COSMIN initiative. Study quality and risk of bias were assessed using the COSMIN Check List.
SC
Expert opinion: 119 publications have been reviewed. The 45 assessment scales can be divided
into specific scales for physical fatigue and specific scales for MS. The most popular tools are the
U
Fatigue Severity Scale and the Modified Fatigue Impact Scale.
AN
Keywords: Multiple Sclerosis; Outcome measures; Physical fatigue; Psychometric properties,
M
Rehabilitation; Reliability; Systematic review; Tools; Validation.
D
TE
EP
C
AC
1. INTRODUCTION
Fatigue occurs in 75-90% of people with Multiple Sclerosis (MS), with 50-60% diagnosed
reporting it as the most common symptom of the disease. Stumbling, tripping, an inability to grasp,
Information Classification: General
and dysarthria are the most significant consequences of fatigue [1] that badly impacts the social and
working lives of people with MS[2]. Moreover, fatigue is a common reason for early retirement[3].
Although physical fatigue is one of the common symptoms of MS, it is still tough to identify it as
related specific to the disease. “Fatigue trait” was defined by the MS Council for Clinical Practice
Guidelines as a “subjective lack of physical and/or mental energy that is perceived by the individual
T
or caregiver to interfere with usual and desired activities”[4]. Until now, the greatest efforts in the
IP
rehabilitation field, the peak of which was the Cochare overview of 2019[5], focused on how to
R
treat fatigue more efficiently without paying enough attention to assess the symptom itself.
SC
Nowadays, a wide range of instruments for assessing physical fatigue exist, namely the Fatigue
Severity Scale (FSS) [6], which is a specific scale to assess physical fatigue interference in any
U
patient’s daily life; also, the Modified Fatigue Impact Scale (MFIS)[7], which is a scale developed
AN
by the MS Council for Clinical Practice Guideline in 1998.
M
Knowing the scientific instruments to identify the right treatment for assessing physical fatigue is
essential to diagnosing symptoms more efficiently. Our review aims at searching and describing the
D
most common tools used to assess physical fatigue together with all its forms in people with MS.
TE
Secondly, it evaluates the languages used to validate the tools and the methodological quality of the
EP
studies. Therefore, this paper’s primary goal is to identify tools to address physical fatigue both at a
clinical and research level to build a standardized and shared assessment path to go along.
C
2. BODY
AC
A group of researchers from the University of Rome “La Sapienza” rehabilitation professionals and
the Association “Rehabilitation and Outcome measure Assessment” R.O.M.A. has carried out this
study along with several systematic reviews, and together they have validated a lot of outcome
measures in Italy over the past several years. [8], [9], [9]–[16]
Information Classification: General
2.1 Protocol and registration
The protocol has been registered in the International Register of the systematic reviews[17],
PROSPERO website, at the following link
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=176333.
The review has been carried out in compliance with the PRSMA STATEMENT 27-ITEM
T
guidelines for systematic review reporting[15][16].
IP
R
2.2 Inclusion criteria in the review: types of studies and types of participants
SC
The systematic review was confined to the studies focusing on the psychometric qualities of
outcome measures used to assess physical fatigue in people with MS.
U
The studies analyzed in the review include those focusing on the psychometric properties of
AN
physical fatigue specific scales—all the studies validating the outcome measures to assess the ADL
M
and the quality of life. The measures had one or more items assessing physical fatigue as well. The
review has taken into account questionnaires, tests, and both scale validation studies with an
D
operator’s interview and a patient’s self-report. Studies assessing the treatment efficacy but omitting
TE
assessment instrument psychometric properties were excluded. No restriction was placed upon age
EP
or other characteristics of people with MS. Neither time nor location limits were applied to the
bibliographical research.
C
2.3 Inclusion criteria
AC
• Studies of validation and cross-cultural adaptation
• Studies focusing on physical fatigue
• Studies about tests, questionnaires, self-evaluation, and performance-based outcome
measures
• Studies about a group of people with MS
2.4 Exclusion criteria
Information Classification: General
• Trials or studies evaluating the effectiveness of a treatment where the evaluation tool is used
only to make the objective concrete.
• Studies evaluating cognitive fatigue.
• Studies focusing on several neurological diseases without considering people with MS in
detail.
2.5 Research methods aiming at identifying the studies
Studies were identified for inclusion through individualized systematic searches of four electronic
T
IP
databases. All potential studies were identified by three reviewers.
R
2.6 Electronic searches
SC
The review’s primary reviewer developed the search strategy, following consultation with an expert
specialized in systematic review of rating scales and using guidance from relevant past reviews[10],
[19]. U
AN
The initial search strategy was constructed for MEDLINE (via PubMed) on 24th January 2020. A
M
combination of terms and keywords was used: ((“multiple sclerosis”) AND “fatigue”)) AND
D
((((((“scale”) OR “test”) OR “questionnaire”) OR “assessment”) OR “measure”) OR “inventory”)
TE
OR “instrument”) AND (((“validation” OR “validity”) OR “validation studies”) and adapted to
other databases. The following electronic databases were searched: MEDLINE (via Pubmed);
EP
CINHAL (via EBSCO); SCOPUS; and Web Of Science.
C
We have chosen to use the databases mentioned above as they only index journals that follow the
AC
"peer review" process in order to keep the methodological quality of the study high, this is the
reason why we have also chosen not to use literature gray.
2.7 Studies selection
Titles, keywords, and abstracts identified through the databases were screened independently by
two occupational therapists and one physical therapist.
Information Classification: General
During the first screening, the three editors have removed all the double studies. All the articles the
three editors agreed upon have been included as well as in the second screening.
During the second screening, the full-text of the included studies have been analyzed.
When the screening phase came to an end, the editors decided to include research studies not
mentioned in the database, using pre-set criteria, because general outcome measures were used. We
T
also carried out '' reference checking '' and '' citation tracking '' to identify any studies that could be
IP
included in our review. However, eligibility criteria were considered for one or more items.
R
SC
2.8 Data Collection and risk of bias assessment
Data extraction occurs in conformity with the Cochrane method[20]. Three reviewers independently
U
extracted patient demographics and descriptive information, and each study was keyworded for
AN
generic issues such as language, country, focus, population, and so on[21]. All these data have been
obtained through the information provided within the studies reports. The editors have focused for
M
every single scale of assessment the following psychometric characteristics: Cronbach Alpha for the
D
internal consistency and interrelatedness of items; the ICC for the test-retest reliability and stability
TE
after repeated measurements; and, the criterion validity represented by correlations with a gold
standard. Both the content and the methods of the studies have been assessed from a quality point of
EP
view. The quality of the study and the risk of bias has been weighed through the assessment tool for
C
the observational, cohort, and cross studies for the selection of health status Measurement
AC
(COSMIN checklist-13)[22][23].
The ten elements used to evaluate the methodological quality of the studies included in our review:
Internal consistency, defined as the interrelation between elements; Reliability, defined as stability
after repeated measurements; Measurement error, systematic and random error in a patient's score
that is not attributed to actual changes in the product to be measured; Content validity defined as the
degree to which the content of a patient-reported health-related outcome tool (HR-PRO) adequately
Information Classification: General
reflects the construct to be measured; Structural validity, is the degree to which the scores of an HR-
PRO instrument are an adequate reflection of a dimensionality of the construct to be measured;
Hypothesis testing is the degree to which the scores of an HR-PRO tool are consistent with the
hypotheses; Cross-cultural validity is the degree to which the performance of the elements on a
translated; or, culturally adapted HR-PRO is an adequate reflection of the performance of the
elements of the original version of the HR-PRO tool. The validity of the criterion defined as the
T
IP
degree to which the scores of an HR-PRO instrument adequately reflect a "gold standard";
Reactivity defined as the ability of an HR-PRO instrument to detect the change over time in the
R
structure to be measured; Interpretability is the degree to which qualitative meaning can be assigned
SC
to an instrument's quantitative scores or changes in scores[24].
U
AN
3. CONCLUSION
M
3.1 Study selection: description of the studies and results of the search
D
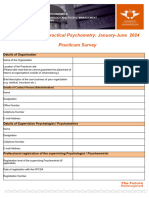
The search strategy identified 10.905 matches. After the removal of duplicates, 5.830 studies were
TE
screened for reading both title and abstract. Subsequently, 162 articles were excluded after reading
the full text. The selection and screening process is highlighted through the flow chart (Figure 1).
EP
3.2 Excluded studies
C
At the first screening of titles and abstracts, studies that did not evaluate the psychometric qualities
AC
or the validated tools did not investigate physical fatigue (e.g., quality of life scales that have no
inherent items) or the sample used did not include MS patients, were not included. Among the
studies that received a full text review, some used the assessment tool for the sole purpose of
measuring the effectiveness of an intervention, others used tools that assessed cognitive fatigue,
while others did not perform a subgroup analysis with MS patients only. Details are reported in
figure 1.
Information Classification: General
In total 5,711 were excluded for ineligibility.
3.3 Included studies
Following compliance with the inclusion criteria, 119 studies[25]–[138] were entered and reviewed,
of which 7[139] evaluated multiple tools simultaneously. Forty-five measurement tools were
identified, and 20 of these were found in multiple studies. A total of 45 tools were found that assess
T
physical fatigue in MS patients[140]. A summary of the descriptive information of the studies is
IP
presented in Table 1.
R
SC
3.4 Study characteristics: types of design and types of participants
All related studies are cross-sectional[26]. The sample size of the studies ranges from 14[103] to
U
9.324[97], [141]. Most participants are under the age of 50, with an average age range of 29,8[49]
AN
to 56,2[32]. The most conspicuous language validations are English and German, respectively, with
32 and 7 validated tools.
M
The most commonly used assessment tools are: the Fatigue Severity Scale (FSS) created in English
D
(UK)[45] and validated in German (Switzerland)[50], German (Germany)[48], Turkish[47],
TE
Italian[60], English (USA)[52], Arabic, Finnish[55], Russian[44], Greek[56], Swedish [53],
EP
Norwegian[53], Dutch[59] and Persian (Iran)[57]; the Fatigue Impact Scale (FIS), created in
English[84] and validated in Turkish[117], Swedish[106], Hungarian[38], Persian[43], Russian[44]
C
and French[128]; the Unidimentional Fatigue Impact Scale (U-FIS) created in English (UK)[51]
AC
and validated in English (USA), English (Canada), Spanish, French, French (Canada), German,
Italian and Swedish[62][73]; the Modified Fatigue Impact Scale (MFIS) validated in English
(UK)[67][61], English (USA)[52], Arabic[75][76], Persian[142], Greek[70], Italian, Spanish,
French, Slovenian[65], German[72], Portuguese (Brazil)[66] and Japanese[71].
3.5 Risk of bias within studies
Information Classification: General
The risk of bias of the studies is not uniform. The methodological quality assessment was carried
out using the COSMIN Checklist-13 tool, shown in Table 4-5. Overall, 76 of 104 studies were
performed with good methodological quality.
Items 1 (in which internal consistency is evaluated), 2 (in which reliability is evaluated), and 4
(construct validity) are the most frequently expected items in the reviewed studies. Conversely,
T
items 7 (cross-cultural validity), 9 (responsiveness), and 10 (interpretability) are those found less
IP
frequently in the studies.
R
Among the articles concerning the FIS, the studies by Armutlu et al., Flensner et al., Mathiowetz et
SC
al., and Lasonczi et al. were judged to be of good quality.
U
As for the MFIS, on the other hand, there are as many as six that possess good methodological
AN
quality: Rooney et al.[61], which also validates the FSS scale, Ghajarzadeh et al.[142], Bakalidou et
al.[70] and Kos et al.[64] Furthermore, the study validating the short-form MFIS-5 by Meca-Llana
M
et al. has an adequate methodological quality.
D
The FSS scale has also been examined in eleven studies and in the works of Otajarvi et al.[55],
TE
Bakalidou et al.[56], Armutlu et al.[47], Ottonello et al.[60], Valko et al.[50] and Rietberg et al.[59]
good methodological quality was found.
EP
3.6 Results of individual outcome measures
C
For each physical fatigue assessment tool, we have collected the validation studies and obtained the
AC
values for Cronbach's alpha and the ICC.
3.7 Fatigue Severity Scale (FSS)
FSS is a self-administered questionnaire, created in 1989 by LB Krupp[45], which evaluates the
severity of fatigue and its impact on the person's life. It is used in various clinical conditions and
neurological problems, including MS.
Information Classification: General
A literature review shows that the FSS has a good internal consistency, with a Cronbach's alpha
whose values range from 0.81 to 0.96. ICC values range from 0.43 to 0.89, indicating good scale
reliability.
The psychometric properties of the scale can be found in Table 2-3.
3.8 Fatigue Impact Scale (FIS)
T
IP
The FIS is one of the most common self-assessment scales used for MS to evaluate the impact of
fatigue in three areas of daily life: cognitive functioning, physical functioning, and psychosocial
R
SC
functioning[84]. Therefore, the FIS, on the physical component impacting fatigue, has a good
internal consistency with a Cronbach Alpha whose values range between 0.88 and 0.98. The ICC
U
values vary from 0.78 to 0.95. A single study has an ICC lower than 0.70[95]; these data reveal the
AN
scale’s reliability (Table 2).
3.9 Unidimentional Fatigue Impact Scale (U-FIS)
M
The scale was created in English by Meads in 2009 and derived from the FIS[51]; the goal was to
D
create a one-dimensional scale of 22 elements based on the theory of quality of life-based on needs.
TE
For this instrument, the review highlights a Cronbach's alpha that varies from 0.95 to 0.98, showing
EP
excellent internal consistency, while the ICC varies from 0.86 to 0.92. The data are shown in Table
2.
C
3.10 Modified Fatigue Impact Scale (MFIS)
AC
FIS is an abbreviation of MFIS, which as modified consists of a self-made questionnaire that the
patient can answer with or without help. The MFIS has a strong internal consistency with the
Cronbach fluctuating from 0.82 to 0.97. The ICC, on the contrary, goes from 0.75 to 0.95. All the
data can be seen in Table 2.
3.11 Neurological Fatigue Index (NFI-MS)
Information Classification: General
The NFI-MS is a self-administering questionnaire created by RJ Mills in 2010, in English, and
developed based on interviews addressed to individuals with MS[80]. It is validated in Dutch[78]
and Portuguese[79]. The ICC values indicate good reliability and range from 0.75 to 0.86 (Table 2).
3.12 Fatigue Scale for Motor and Cognitive Functions (FSMC)
The FSMC is a questionnaire created in 2009 by IK Penner[82] and has been validated in
T
Danish[83] and German[72]. With this tool, it is possible to obtain a total score on physical fatigue
IP
and cognitive fatigue. Cronbach's alpha value is 0.91, while the ICC value is 0.86, thus showing
R
good internal consistency and good reliability, as reported in Table 2.
SC
3.13 Other scales
U
The review highlighted another 38 validated tools divided into two subgroups: specific scales for
AN
physical fatigue (Table 2) and scales for quality of life that present at least one item relating to
physical fatigue (Table 2).
M
Among the latter, the scales with the greatest response in our review are the Multiple Sclerosis
D
Quality of Life (MSQoL) and the Multiple Sclerosis International Quality of Life Questionnaire
TE
(MusiQoL).
EP
3.14 Multiple Sclerosis Quality of Life (MSQoL)
C
The MSQOL-54 is a multidimensional health-related quality of life measure that combines both
AC
generic and MS-specific items into a single instrument[114][143]. This 54-item instrument
generates 12 subscales, two summary scores, and two additional single-item measures. The
MSQOL-54 is a structured self-report questionnaire that a patient can generally complete with little
or no assistance. The MSQOL-54 shows good internal consistency with Cronbach's alpha ranging
from 0.75 to 0.96. Test-retest reliability for the 12 subscales is also good, with ICC ranging from
0.66 to 0.96.
Information Classification: General
3.15 Multiple Sclerosis International Quality of Life (MusiQoL)
The Multiple Sclerosis (MS) International Quality of Life (MusiQoL) questionnaire, a multi-
dimensional, self-administered questionnaire, is available in 16 languages[131][138][135], as a
disease-specific quality of life scale that can be applied internationally[131]. The MusiQoL was
validated for the first time in English by M.C. Simeoni in 2008[131]. Characterized by the presence
T
of 31 items for nine dimensions, an average score is calculated for each dimension, which is added
IP
to the other scores. Cronbach's alpha range of values, from 0.34 to 0.96 and those of the ICC from
R
0.59 to 0.99, show a certain variability
SC
3.16 Summary of the quality of the evidence
U
The impact of physical fatigue is significant in all activities, work, and more, for people with MS.
AN
In particular, physical fatigue affects manual dexterity, walking, and language, with a significant
impact from both a social and emotional point of view.[2]
M
In order to investigate physical fatigue in the most precise way possible, while also considering the
D
impact that this will have on the quality of life of people with MS, this review aims to research and
TE
describe the tools for assessing physical fatigue symptoms, while weighing psychometric
properties. Moreover, it aims to identify the cultural adaptations of evaluation tools and evaluate the
EP
studies’ methodological qualities. The data extrapolated from the major databases from January
C
2020 allowed us to identify the most important assessment tools for physical fatigue validated at the
AC
international level. The search was conducted using keywords. No search constraints were placed to
avoid excluding studies of interest for our review and report all the tools and adaptations present in
the literature.
The studies that emerged were published from 1989[6] to 2020[76]. In total, 119 studies track the
use of an evaluation scale.
Information Classification: General
Also, depending on the national contexts, a strong variety of validated tools can be seen. This can
be assumed to have a positive meaning if we consider the clinical context’s multiple needs, but it
certainly leads to the need to make the tools more suitable for several cultural contexts.
These findings suggest that clinicians have contrasting or incomplete information available to use
when making patient care decisions. Furthermore, the lack of consistency and standardization in the
T
evaluation results hindered comparative research and meta-analysis. Further investigation of
IP
outcome measures would benefit patients, researchers, and clinicians. A universal, validated
R
outcome measure is needed to allow comparisons through practice; therefore, researchers
SC
recommended using a standard set of assessments in the future.
The variety of methods used throughout the literature to measure responsiveness illustrates the
U
current problem of defining and standardizing a method or descriptor that can report responsiveness
AN
across various outcome measures accurately.
M
The COSMIN checklist was published in 2010 to assess the methodological quality of the
D
psychometric properties studies[144][145]. The COSMIN framework was developed through an
TE
international consensus process to provide specific recommendations on terminology, taxonomy,
and methodology in studies dealing with PROMs and their measurement properties[22].
EP
This review showed a disparate number of physical fatigue assessment tools, counting as many as
C
45.
AC
Within some of the most used tools, as in the FIS scale and its modified versions, MFIS and U-FIS,
there are also domains investigating social functioning and cognitive functioning, as they arise as
tools for assessing the fatigue symptom in its entirety. However, the presence of a separate domain
for physical functioning allows us to include them in our review and extrapolate psychometric
parameters as tools for assessing physical fatigue.
Information Classification: General
Overall, the review showed us that the scale with the highest number of validations at the
international level is the FSS, with 13 cultural adaptations, which also became extremely reliable.
We described the marked heterogeneity in using evaluation tools and deliberately avoided
suggestions that one evaluation is better than another. Therefore, in the absence of the "perfect"
evaluation tool, we recommend the validation and cultural adaptation of existing evaluation scales
T
in multiple languages to create a common reading index to evaluate physical fatigue in people with
IP
MS.
R
In relation to the review’s secondary objectives, we generally found a good methodological quality,
SC
with about 76 studies on 104, which fell within the COSMIN tool’s parameters.
U
The Italian context has only six culturally validated scales so it must be enriched with new studies,
AN
culturally adaptable to those considered most valid, to be among the tools that emerged from this
review.
M
3.17 Limitation of the study
D
There are obvious limitations in this review that need to be considered. Despite the systematic
TE
search of four electronic databases, it is possible that not all relevant studies have been identified.
EP
The studies may have been published in journals that were not covered by the data. Moreover, the
search string used did not detect studies that validate generic fatigue scales, which, however, having
C
specific items on physical fatigue within them, are eligible for our review.
AC
4 EXPERT OPINION
As of May 2020, the literature data made it possible to identify 45 tools for assessing physical
fatigue in people with MS. It has been acknowledged that the tools with the highest number of
validations at an international level are FSS and MFIS. The FSS has been validated in 13 languages
Information Classification: General
and uses nine items to evaluate physical fatigue, while the MFIS consists of 21 items, but among
these only nine are those investigating physical functioning. Both scales for psychometric values are
valid and reliable. However, the large number of tools identified proves the trend to create new
tools; to reach a “gold standard,” it would be more appropriate to validate and culturally adapt the
tools already available to as many languages as possible. From this point of view, the Italian context
is very sparse. In fact, only six tools have been identified to assess physical fatigue validated in
T
IP
Italian: the FSS, the MFIS, the U-FIS, the FAMS, the MusiQol, and the MSQOL-54.
R
Once we have analyzed the psychometric properties of each scale described in the literature
SC
referring to fatigue in people with MS, physics seems to us, at this point, to clearly define what
should be the context for application of more appropriate scales.
U
Regarding the specific scales for physical fatigue, FSS is the primary. This scale, from a clinical
AN
rehabilitation point of view, investigates the impact of physical fatigue on various aspects of the life
M
for the person with MS, but only in reference to the past 7 days. For possible easy administration
and the rapid data draw, we recommend FSS for subjects with MS relapsing-remitting (MS-RR),
D
perhaps immediately after an acute inflammatory phase, but we do not recommend it for research
TE
purposes.
EP
Another scale that we are interested in including in our recommendations is the FIS with its
variants, U-FIS and MFIS. The FIS was originally designed to evaluate the effects of fatigue on the
C
quality of life in patients with chronic diseases. In particular, we recommend it for use in people
AC
with MS in its secondary progressive (MS-SP) and primary progressive (MS-PP) forms. For
research purposes, we recommend MFIS, which is always able to investigate the three areas of
functioning of a person affected by MS with physical fatigue but does so with 21 targeted items and
therefore is more suited to collect data from a large number of patients.
Information Classification: General
The U-FIS, on the other hand, we recommend for research purposes because it is easy and quick to
administer, whereas in the clinical rehabilitation field, we promote its use in patients with
progressive MS, but with a significant level of EDSS disability[146], as the 22 elements that
compose U-FIS are based on a theory of quality of life is based on needs being met.
Among the scales that primarily investigate the quality of life for people with MS, we recommend
T
the FAMS, the MSQOL-54, and the MusiQoL.
IP
The FAMS is a questionnaire consisting of 59 items that evaluates six main aspects of quality of
R
life. This tool, like the FSS, investigates only the previous 7 days, so here too we recommend, for
SC
clinical rehabilitation its use, in the SM-RR form, but we do not recommend it for research use.
U
The MusiQoL, on the other hand, is a self-administering questionnaire, so before using it in a
AN
clinical rehabilitation setting, it is advisable to carefully evaluate the cognitive level of the person
with MS. It investigates nine dimensions which we consider very complete, but the heterogeneity of
M
the psychometric values that emerged from the review makes us dissent from recommending it
D
either for clinical rehabilitation or research purposes. Conversely, we suggest and promote the use
TE
of MSQOL-54 for research and for clinical rehabilitative use for SM-RR forms, yet even moreso in
chronic MS forms, as the twelve parameters it investigates can be very useful in people with many
EP
years of illness behind him. Table 1
C
Finally, we do not recommend the use of the NFIS-MS or the GNDS scales either in clinical
AC
rehabilitation or in rehabilitation research, as these, albeit with relevant psychometric values, are
purely medical scales.
In conclusion, for MS-SP and MS-PP we recommend the use of FIS, MFIS and U-FIS whereas for
MS-RR we recommend the use of FSS, FAMS, MusiQoL. Our recommendations have been
elaborated on the basis not only of items that can best represent MS, but also of the sample used for
the validation study.
Information Classification: General
We recommend that future studies enrich and integrate the Italian context of rehabilitation,
culturally adapting, among the tools that emerged from this review, those deemed most valid to
create standardized and shareable evaluation paths. In addition, we hope that specific scientific
societies of each branch of rehabilitation will promote the clinical rehabilitation use among their
professionals of these scales and that they invest resources for the validation of as many tools as
possible among those that have proved to be the most reliable.
T
IP
R
SC
Funding
This paper was not funded.
U
AN
Declaration of interest
M
The authors have no relevant affiliations or financial involvement with any organization or entity with a
financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants
D
or patents received or pending, or royalties.
TE
EP
Reviewers Disclosure
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
C
Availability of data and material
AC
The data that support the findings of this study are available from the corresponding author upon
reasonable request.
Figures and Tables
Authors confirm that all figures and tables are original.
Information Classification: General
REFERENCES
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••)
to readers.
T
[1] Occupational therapy and neurological conditions. 2016.
IP
[2] J. D. Fisk, A. Pontefract, P. G. Ritvo, C. J. Archibald, and T. J. Murray, “The Impact of
Fatigue on Patients with Multiple Sclerosis,” Can. J. Neurol. Sci. / J. Can. des Sci. Neurol.,
1994.
R
[3] I. Dyck and L. Jongbloed, “Women with multiple sclerosis and employment issues: A focus
on social and institutional environments,” Canadian Journal of Occupational Therapy. 2000.
SC
[4] S. R. Schwid, M. Covington, B. M. Segal, and A. D. Goodman, “Fatigue in multiple
sclerosis: Current understanding and future directions,” J. Rehabil. Res. Dev., 2002.
[5] B. Amatya, F. Khan, and M. Galea, “Rehabilitation for people with multiple sclerosis: An
U
overview of Cochrane Reviews,” Cochrane Database of Systematic Reviews. 2019.
**this very recent systematic review reports recommendations about rehabilitation for people
AN
with Multiple Sclerosis, with a focus on fatigue.
[6] L. B. Krupp, “The Fatigue Severity Scale,” Arch. Neurol., 1989.
[7] M. S. C. for C. P. Guidelines, “Fatigue and multiple sclerosis: evidence-based management
strategies for fatigue in multiple sclerosis,” Paralyzed Veterans Am., 1998.
M
[8] G. Galeoto et al., “General Sleep Disturbance Scale: Translation, cultural adaptation, and
psychometric properties of the Italian version,” Cranio - J. Craniomandib. Pract., 2019.
[9] A. Savona et al., “Evaluation of intra- and inter-rater reliability and concurrent validity of the
D
Italian version of the Jebsen–Taylor Hand Function Test in adults with rheumatoid arthritis,”
TE
Hand Ther., 2019.
[10] G. Galeoto et al., “The outcome measures for loss of functionality in the activities of daily
living of adults after stroke: a systematic review,” Topics in Stroke Rehabilitation. 2019.
**This study is a systematic review on outcome measures for loss of functionality in the
EP
activities of daily living of adults after stroke
[11] G. Romagnoli et al., “Occupational Therapy’s efficacy in children with Asperger’s
syndrome: a systematic review of randomized controlled trials,” Clin. Ter., 2019.
C
[12] A. Berardi, G. Galeoto, L. Lucibello, F. Panuccio, D. Valente, and M. Tofani, “Athletes with
disability’ satisfaction with sport wheelchairs: an Italian cross sectional study,” Disabil.
AC
Rehabil. Assist. Technol., 2020.
[13] F. Miniera, A. Berardi, F. Panuccio, D. Valente, M. Tofani, and G. Galeoto, “Measuring
Environmental Barriers: Validation and Cultural Adaptation of the Italian Version of the
Craig Hospital Inventory of Environmental Factors (CHIEF) Scale,” Occup. Ther. Heal.
Care, 2020.
[14] F. Panuccio et al., “General Sleep Disturbance Scale (GSDS-IT) in people with spinal cord
injury: a psychometric study,” Spinal Cord, 2020.
[15] F. Panuccio et al., “Development of the Pregnancy and Motherhood Evaluation
Questionnaire (PMEQ) for evaluating and measuring the impact of physical disability on
pregnancy and the management of motherhood: a pilot study,” Disabil. Rehabil., pp. 1–7,
Aug. 2020.
[16] A. Berardi et al., “Tools to assess the quality of life in patients with Parkinson’s disease: a
Information Classification: General
systematic review,” Expert Review of Pharmacoeconomics and Outcomes Research. 2020.
**This study is a systematic review on outcome measures for quality of life in people with
Parkinson's Disease
[17] J. Chandler, R. Churchill, T. Lasserson, D. Tovey, and J. Higgins, “Methodological standards
for the conduct of new Cochrane Intervention Reviews,” http://editorial-
unit.cochrane.org/sites/editorial-
unit.cochrane.org/files/uploads/MECIR_conduct_standards%202.3%2002122013.pdf, 2013.
[18] A. Liberati et al., “The PRISMA statement for reporting systematic reviews and meta-
analyses of studies that evaluate health care interventions: explanation and elaboration,” in
Journal of clinical epidemiology, 2009.
T
[19] M. Ruggieri et al., “Validated Fall Risk Assessment Tools for Use with Older Adults: A
IP
Systematic Review,” Phys. Occup. Ther. Geriatr., vol. 36, no. 4, pp. 331–353, Oct. 2018.
**This study is a systematic review on outcome measures for fall risk of adults.
[20] J. Noyes and S. Lewin, “Chapter 5: Extracting Qualitative Evidence,” Suppl. Guid. Incl.
R
Qual. Res. Cochrane Syst. Rev. Interv., 2011.
[21] S. Bates and E. Coren, “Systematic Map No.1: The Extent and Impact of Parental Mental
SC
Health Problems on Families and the Acceptability, Accessibility and Effectiveness of
Interventions.,” London SCIE, 2006.
[22] L. B. Mokkink et al., “The COSMIN study reached international consensus on taxonomy,
U
terminology, and definitions of measurement properties for health-related patient-reported
outcomes,” J. Clin. Epidemiol., 2010.
AN
* This is the checklist for systematic reviews of Patient-Reported Outcome Measures
[23] L. B. Mokkink, C. B. Terwee, and D. L. Patrick, “COSMIN checklist manual,” COSMIN,
2012.
[24] J. C. Nunnally, Psychometric theory. 1979.
M
[25] H. Ford, P. Trigwell, and M. Johnson, “The nature of fatigue in multiple sclerosis,” J.
Psychosom. Res., 1998.
[26] S. Yamada et al., “Development of a short version of the motor fimTM for use in long-term
D
care settings,” J. Rehabil. Med., 2006.
TE
[27] J. Benito-León et al., “Impact of fatigue in multiple sclerosis: The fatigue Impact Scale for
Daily Use (D-FIS),” Mult. Scler., 2007.
[28] P. Michel et al., “A Multidimensional Computerized Adaptive Short-Form Quality of Life
Questionnaire Developed and Validated for Multiple Sclerosis,” Med. (United States), 2016.
EP
[29] H. Correia et al., “Spanish translation and linguistic validation of the quality of life in
neurological disorders (Neuro-QoL) measurement system,” Qual. Life Res., 2015.
[30] D. M. Miller et al., “Validating neuro-QoL short forms and targeted scales with people who
C
have multiple sclerosis,” Mult. Scler., 2015.
[31] L. D. Medina, S. Torres, E. Alvarez, B. Valdez, and K. V Nair, “Patient-reported outcomes in
AC
multiple sclerosis: Validation of the Quality of Life in Neurological Disorders (Neuro-
QoLTM) short forms,” Mult. Scler. J. - Exp. Transl. Clin., 2019.
[32] R. C. Gershon et al., “Neuro-QOL: Quality of life item banks for adults with neurological
disorders: Item development and calibrations based upon clinical and general population
testing,” Quality of Life Research. 2012.
[33] M. Ghajarzadeh et al., “Validity and reliability of the persian version of the PERception de la
scle’rose en plaques et de ses pousse’es questionnaire evaluating multiple sclerosis-related
quality of life,” Int. J. Prev. Med., 2016.
[34] A. Baroin et al., “Validation of a new quality of life scale related to multiple sclerosis and
relapses,” Qual. Life Res., 2013.
[35] R. A. Marrie and M. Goldman, “Validity of performance scales for disability assessment in
multiple sclerosis,” Mult. Scler., 2007.
Information Classification: General
[36] E. Chamot, I. Kister, and G. R. Cutter, “Item response theory-based measure of global
disability in multiple sclerosis derived from the Performance Scales and related items,” BMC
Neurol., 2014.
[37] C. E. Schwartz, T. Vollmer, and H. Lee, “Reliability and validity of two self-report measures
of impairment and disability for MS,” Neurology, 1999.
[38] E. Losonczi, K. Bencsik, C. Rajda, G. Lencsés, M. Török, and L. Vécsei, “Validation of the
Fatigue Impact Scale in Hungarian patients with multiple sclerosis,” Qual. Life Res., 2011.
[39] C. E. Schwartz, R. K. Bode, B. R. Quaranto, and T. Vollmer, “The symptom inventory
disability-specific short forms for multiple sclerosis: Construct validity, responsiveness, and
interpretation,” Arch. Phys. Med. Rehabil., 2012.
[40] C. E. Schwartz, R. K. Bode, R. Quaranto, and T. Vollmer, “The symptom inventory
T
disability-specific short forms for multiple sclerosis: Reliability and factor structure,” Arch.
IP
Phys. Med. Rehabil., 2012.
[41] R. Green, J. Kalina, R. Ford, K. Pandey, and I. Kister, “SymptoMScreen: A Tool for Rapid
Assessment of Symptom Severity in MS Across Multiple Domains,” Appl. Neuropsychol.,
R
2017.
[42] F. K.C. et al., “Validation of the SymptoMScreen with performance-based or clinician-
SC
assessed outcomes,” Mult. Scler. Relat. Disord., 2019.
[43] M. Heidari, S. M. Nabavi, M. Akbarfahim, M. Salehi, and M. Torabi-Nami, “Psychometric
properties of the Persian version of the Fatigue Impact Scale (FIS-P) in patients with
[44] U
Multiple Sclerosis,” Iran. Rehabil. J., 2015.
Y. V. Gavrilov et al., “Validation of the Russian version of the Fatigue Impact Scale and
AN
Fatigue Severity Scale in multiple sclerosis patients,” Acta Neurol. Scand., 2018.
[45] L. B. Krupp, N. G. Larocca, J. Muir Nash, and A. D. Steinberg, “The fatigue severity scale:
Application to patients with multiple sclerosis and systemic lupus erythematosus,” Arch.
Neurol., 1989.
M
[46] R. J. Mills, C. A. Young, R. S. Nicholas, J. F. Pallant, and A. Tennant, “Rasch analysis of the
Fatigue Severity Scale in multiple sclerosis,” Mult. Scler., 2009.
D
[47] K. Armutlu et al., “The validity and reliability of the Fatigue Severity Scale in Turkish
multiple sclerosis patients,” Int. J. Rehabil. Res., 2007.
TE
[48] D. Reske, R. Pukrop, K. Scheinig, W. F. Haupt, and H. F. Petereit, “Measuring fatigue in
patients with multiple sclerosis with standardized methods in German speaking areas,”
Fortschritte der Neurol. Psychiatr., 2006.
[49] H. I. Al-Sobayel et al., “Validation of an Arabic version of Fatigue Severity scale,” Saudi
EP
Med. J., 2016.
[50] P. O. Valko, C. L. Bassetti, K. E. Bloch, U. Held, and C. R. Baumann, “Validation of the
fatigue severity scale in a Swiss cohort,” Sleep, 2008.
C
[51] D. M. Meads, L. C. Doward, S. P. McKenna, J. Fisk, J. Twiss, and B. Eckert, “The
development and validation of the unidimensional fatigue impact scale (U-FIS),” Mult.
AC
Scler., 2009.
[52] Y. C. Learmonth, D. Dlugonski, L. A. Pilutti, B. M. Sandroff, R. Klaren, and R. W. Motl,
“Psychometric properties of the Fatigue Severity Scale and the Modified Fatigue Impact
Scale,” J. Neurol. Sci., 2013.
[53] A. Lerdal, S. Johansson, A. Kottorp, and L. Von Koch, “Psychometric properties of the
fatigue severity scale: Rasch analyses of responses in a Norwegian and a Swedish MS
cohort,” Mult. Scler., 2010.
[54] G. Salehpoor, S. Rezaei, and M. Hosseininezhad, “Psychometric properties of fatigue
severity scale in patients with multiple sclerosis,” J. Kerman Univ. Med. Sci., 2013.
[55] E. Rosti-Otajärvi, P. Hämäläinen, A. Wiksten, T. Hakkarainen, and J. Ruutiainen, “Validity
and reliability of the Fatigue Severity Scale in Finnish multiple sclerosis patients,” Brain
Behav., 2017.
Information Classification: General
[56] D. Bakalidou, E. K. Skordilis, S. Giannopoulos, E. Stamboulis, and K. Voumvourakis,
“Validity and reliability of the FSS in Greek MS patients,” Springerplus, 2013.
[57] N. Ghotbi, N. Nakhostin Ansari, S. Fetrosi, A. Shamili, H. Choobsaz, and H. Montazeri,
“Fatigue in Iranian patients with neurological conditions: An assessment with Persian fatigue
severity scale,” Heal. Sci. J., 2013.
[58] L. Hernandez-Ronquillo, F. Moien-Afshari, K. Knox, J. Britz, and J. F. Tellez-Zenteno,
“How to measure fatigue in epilepsy? The validation of three scales for clinical use,”
Epilepsy Res., 2011.
[59] M. B. Rietberg, E. E. H. Van Wegen, and G. Kwakkel, “Measuring fatigue in patients with
multiple sclerosis: Reproducibility, responsiveness and concurrent validity of three Dutch
self-report questionnaires,” Disabil. Rehabil., 2010.
T
[60] M. Ottonello, L. Pellicciari, A. Giordano, and C. Foti, “Rasch analysis of the fatigue severity
IP
scale in Italian subjects with multiple sclerosis,” J. Rehabil. Med., 2016.
[61] S. Rooney, D. A. McFadyen, D. L. Wood, D. F. Moffat, and P. L. Paul, “Minimally
important difference of the fatigue severity scale and modified fatigue impact scale in people
R
with multiple sclerosis,” Mult. Scler. Relat. Disord., 2019.
[62] L. C. Doward et al., “International development of the unidimensional fatigue impact scale
SC
(U-FIS),” Value Heal., 2010.
[63] S. Johansson, A. Kottorp, K. A. Lee, C. L. Gay, and A. Lerdal, “Can the Fatigue Severity
Scale 7-item version be used across different patient populations as a generic fatigue measure
U
- a comparative study using a Rasch model approach,” Health Qual. Life Outcomes, vol. 12,
no. 1, pp. 1–9, 2014.
AN
[64] D. Kos et al., “Assessing fatigue in multiple sclerosis: Dutch Modified Fatigue Impact
Scale,” Acta Neurol. Belg., 2003.
[65] D. Kos, E. Kerckhofs, I. Carrea, R. Verza, M. Ramos, and J. Jansa, “Evaluation of the
Modified Fatigue Impact Scale in four different European countries,” Mult. Scler., 2005.
M
[66] K. Pavan, K. Schmidt, B. Marangoni, M. F. Mendes, C. P. Tilbery, and S. Lianza, “Multiple
sclerosis: Cross-cultural adaptation and validation of the modified fatigue impact scale,” Arq.
D
Neuropsiquiatr., 2007.
[67] R. J. Mills, C. A. Young, J. F. Pallant, and A. Tennant, “Rasch analysis of the Modified
TE
Fatigue Impact Scale (MFIS) in multiple sclerosis,” J. Neurol. Neurosurg. Psychiatry, 2010.
[68] M. Ghajarzadeh, R. Jalilian, G. Eskandari, M. Ali Sahraian, and A. Reza Azimi, “Validity
and reliability of Persian version of Modified Fatigue Impact Scale (MFIS) questionnaire in
Iranian patients with multiple sclerosis,” Disabil. Rehabil., 2013.
EP
[69] M. H. Harirchian et al., “Evaluation of the Persian version of modified fatigue impact scale
in Iranian patients with multiple sclerosis.,” Iran. J. Neurol., 2013.
[70] D. Bakalidou, K. Voumvourakis, Z. Tsourti, E. Papageorgiou, A. Poulios, and S.
C
Giannopoulos, “Validity and reliability of the Greek version of the Modified Fatigue Impact
Scale in multiple sclerosis patients,” Int. J. Rehabil. Res., 2014.
AC
[71] H. Masuda et al., “Validation of the Japanese version of the Modified Fatigue Impact Scale
and assessment of the effect of pain on scale responses in patients with multiple sclerosis,”
Clin. Exp. Neuroimmunol., 2015.
[72] G. E. A. Pust et al., “In search of distinct MS-related fatigue subtypes: results from a multi-
cohort analysis in 1.403 MS patients,” J. Neurol., 2019.
[73] J. Twiss, L. C. Doward, S. P. McKenna, and B. Eckert, “Interpreting scores on multiple
sclerosis-specific patient reported outcome measures (the PRIMUS and U-FIS),” Health
Qual. Life Outcomes, 2010.
[74] H. Khalil et al., “Cross cultural adaptation and psychometric evaluation of an Arabic version
of the modified fatigue impact scale in people with multiple sclerosis,” Mult. Scler. Relat.
Disord., 2020.
[75] N. Farran et al., “Factors affecting MS patients’ health-related quality of life and
Information Classification: General
measurement challenges in Lebanon and the MENA region,” Mult. Scler. J. - Exp. Transl.
Clin., 2020.
[76] A. S. Alawami and F. A. Abdulla, “Psychometric properties of an Arabic translation of the
modified fatigue impact scale in patients with multiple sclerosis,” Disabil. Rehabil., 2020.
[77] V. Meca-Lallana et al., “Assessing fatigue in multiple sclerosis: Psychometric properties of
the five-item Modified Fatigue Impact Scale (MFIS-5),” Mult. Scler. J. - Exp. Transl. Clin.,
2019.
[78] A. Derksen, L. B. Mokkink, M. B. Rietberg, D. L. Knol, R. W. J. G. Ostelo, and B. M. J.
Uitdehaag, “Validation of a Dutch version of the Neurological Fatigue Index (NFI-MS) for
patients with multiple sclerosis in the Netherlands,” Qual. Life Res., 2013.
[79] J. Lopes, E. L. Lavado, and D. R. Kaimen-Maciel, “Validation of the Brazilian version of the
T
neurological fatigue index for multiple sclerosis,” Arq. Neuropsiquiatr., 2016.
IP
[80] R. J. Mills, C. A. Young, J. F. Pallant, and A. Tennant, “Development of a patient reported
outcome scale for fatigue in multiple sclerosis: The Neurological Fatigue Index (NFI-MS),”
Health Qual. Life Outcomes, 2010.
R
[81] R. J. Mills, M. Calabresi, A. Tennant, and C. A. Young, “Perceived changes and minimum
clinically important difference of the Neurological Fatigue Index for multiple sclerosis (NFI-
SC
MS),” Mult. Scler. J., 2013.
[82] I. K. Penner, C. Raselli, M. Stöcklin, K. Opwis, L. Kappos, and P. Calabrese, “The Fatigue
Scale for Motor and Cognitive Functions (FSMC): Validation of a new instrument to assess
[83] U
multiple sclerosis-related fatigue,” Mult. Scler., 2009.
M. S. Oervik, T. Sejbaek, I. K. Penner, M. Roar, and M. Blaabjerg, “Validation of the fatigue
AN
scale for motor and cognitive functions in a danish multiple sclerosis cohort,” Mult. Scler.
Relat. Disord., 2017.
[84] J. D. Fisk, P. G. Ritvo, L. Ross, D. A. Haase, T. J. Marrie, and W. F. Schlech, “Measuring
the functional impact of fatigue: Initial validation of the fatigue impact scale,” Clin. Infect.
M
Dis., 1994.
[85] F. Motaharinezhad et al., “Validation of persian version of comprehensive fatigue assessment
D
battery for multiple sclerosis (CFAB-MS),” J. Maz. Univ. Med. Sci., 2015.
[86] J. Chilcot, S. Norton, M. E. Kelly, and R. Moss-Morris, “The Chalder Fatigue Questionnaire
TE
is a valid and reliable measure of perceived fatigue severity in multiple sclerosis,” Mult.
Scler., 2016.
[87] L. A. Jason et al., “A screening instrument for chronic fatigue syndrome: Reliability and
validity,” J. Chronic Fatigue Syndr., 1997.
EP
[88] M. Worm-Smeitink et al., “The assessment of fatigue: Psychometric qualities and norms for
the Checklist individual strength,” J. Psychosom. Res., 2017.
[89] D. Kos et al., “Electronic visual analogue scales for pain, fatigue, anxiety and quality of life
C
in people with multiple sclerosis using smartphone and tablet: A reliability and feasibility
study,” Clin. Rehabil., 2017.
AC
[90] J. E. Schwartz, L. Jandorf, and L. B. Krupp, “The measurement of fatigue: A new
instrument,” J. Psychosom. Res., 1993.
[91] J. Iriarte, G. Katsamakis, and P. De Castro, “The fatigue descriptive scale (FDS): A useful
tool to evaluate fatigue in multiple sclerosis,” Mult. Scler., 1999.
[92] S. Hudgens, R. Schüler, J. Stokes, S. Eremenco, E. Hunsche, and T. P. Leist, “Development
and Validation of the FSIQ-RMS: A New Patient-Reported Questionnaire to Assess
Symptoms and Impacts of Fatigue in Relapsing Multiple Sclerosis,” Value Heal., 2019.
[93] S. Behrangrad and A. Kordi Yoosefinejad, “Validity and reliability of the multidimensional
assessment of fatigue scale in Iranian patients with relapsing-remitting subtype of multiple
sclerosis,” Disabil. Rehabil., 2018.
[94] S. Thomas, P. Kersten, and P. W. Thomas, “The Multiple Sclerosis-Fatigue Self- Efficacy
(MS-FSE) scale: Initial validation,” Clin. Rehabil., 2014.
Information Classification: General
[95] V. Mathiowetz, “Test-retest reliability and convergent validity of the fatigue impact scale for
persons with multiple sclerosis,” Am. J. Occup. Ther., 2003.
[96] K. F. Cook, A. M. Bamer, T. S. Roddey, G. H. Kraft, J. Kim, and D. Amtmann, “A PROMIS
fatigue short form for use by individuals who have multiple sclerosis,” Qual. Life Res., 2012.
[97] R. A. Marrie, G. Cutter, T. Tyry, O. Hadjimichael, D. Campagnolo, and T. Vollmer,
“Validation of the NARCOMS Registry: Fatique assessment,” Mult. Scler., 2005.
[98] S. Johansson, C. Ytterberg, B. Back, L. W. Holmqvist, and L. von Koch, “The Swedish
Occupational Fatigue Inventory in people with multiple sclerosis,” J. Rehabil. Med., 2008.
[99] D. Kos, G. Nagels, M. B. D’Hooghe, M. Duportail, and E. Kerckhofs, “A rapid screening
tool for fatigue impact in multiple sclerosis,” BMC Neurol., 2006.
[100] P. Flachenecker, G. Müller, H. König, H. Meissner, K. V Toyka, and P. Rieckmann,
T
“["Fatigue" in multiple sclerosis. Development and and validation of the ‘Würzburger
IP
Fatigue Inventory for MS’].,” Nervenarzt, 2006.
[101] P. Flachenecker, H. König, H. Meissner, G. Müller, and P. Rieckmann, “Fatigue bei multiper
sklerose: Validierung des Würzburger Erschöpfungs-Inventars bei Multipler Sklerose
R
(WEIMUS),” Neurol. und Rehabil., 2008.
[102] A. S. Chua et al., “Patient-reported outcomes in multiple sclerosis: Relationships among
SC
existing scales and the development of a brief measure,” Mult. Scler. Relat. Disord., 2015.
[103] L. S. Matza, K. D. Stewart, G. Phillips, P. Delio, and R. T. Naismith, “Development of a
brief clinician-reported outcome measure of multiple sclerosis signs and symptoms: The
U
Clinician Rating of Multiple Sclerosis (CRoMS),” Mult. Scler. Relat. Disord., 2019.
[104] D. F. Cella et al., “Validation of the functional assessment of multiple sclerosis quality of life
AN
instrument,” Neurology, 1996.
[105] C. H. Chang et al., “Quality of life in multiple sclerosis patients in Spain,” Mult. Scler., 2002.
[106] G. Flensner, E. Anna-Christina, and O. Söderhamn, “Reliability and validity of the Swedish
version of the Fatigue Impact Scale (FIS),” Scand. J. Occup. Ther., 2005.
M
[107] M. F. Mendes, S. Balsimelli, G. Stangehaus, and C. P. Tilbery, “Validation of the functional
assessment of multiple sclerosis quality of life instrument in a Portuguese language,” Arq.
D
Neuropsiquiatr., 2004.
[108] F. Patti, P. Russo, A. Pappalardo, F. Macchia, L. Civalleri, and A. Paolillo, “Predictors of
TE
quality of life among patients with multiple sclerosis: An Italian cross-sectional study,” J.
Neurol. Sci., 2007.
[109] J. Sørensen et al., “Validation of the Danish Version of Functional Assessment of Multiple
Sclerosis: A Quality of Life Instrument,” Mult. Scler. Int., 2011.
EP
[110] I. Ensari, R. W. Motl, and E. McAuley, “Structural and construct validity of the Leeds
Multiple Sclerosis Quality of Life scale,” Qual. Life Res., 2016.
[111] H. L. Ford, E. Gerry, A. Tennant, D. Whalley, R. Haigh, and M. H. Johnson, “Developing a
C
disease-specific quality of life measure for people with multiple sclerosis,” Clin. Rehabil.,
2001.
AC
[112] D. I. Akbiyik et al., “The validity and test-retest reliability of the Leeds multiple sclerosis
quality of life scale in Turkish patients,” Int. J. Rehabil. Res., 2009.
[113] J. Greenhalgh, “An assessment of the feasibility and utility of the MS Symptom and Impact
Diary (MSSID),” Qual. Life Res., 2005.
[114] B. G. Vickrey, R. D. Hays, R. Harooni, L. W. Myers, and G. W. Ellison, “A health-related
quality of life measure for multiple sclerosis,” Qual. Life Res., 1995.
[115] A. Solari et al., “Validation of Italian multiple sclerosis quality of life 54 questionnaire,” J.
Neurol. Neurosurg. Psychiatry, 1999.
[116] A. Miller and S. Dishon, “Health-related quality of life in multiple sclerosis: Psychometric
analysis of inventories,” Mult. Scler., 2005.
[117] K. Armutlu et al., “Psychometric study of Turkish version of Fatigue Impact Scale in
multiple sclerosis patients,” J. Neurol. Sci., 2007.
Information Classification: General
[118] I. E. et al., “Cross-cultural adaptation and validation of multiple sclerosis quality of life
questionnaire (MSQOL-54) in a Turkish multiple sclerosis sample,” J. Neurol. Sci., 2006.
[119] S. Heiskanen, P. Meriläinen, and A. M. Pietilä, “Health-related quality of life - Testing the
reliability of the MSQOL-54 instrument among MS patients,” Scandinavian Journal of
Caring Sciences. 2007.
[120] T. Pekmezovic, D. Kisic Tepavcevic, J. Kostic, and J. Drulovic, “Validation and cross-
cultural adaptation of the disease-specific questionnaire MSQOL-54 in Serbian multiple
sclerosis patients sample,” Qual. Life Res., 2007.
[121] J. Füvesi et al., “Cross-cultural adaptation and validation of the ‘Multiple Sclerosis Quality
of Life Instrument’ in Hungarian,” Mult. Scler., 2008.
[122] K. El Alaoui Taoussi, E. Ait Ben Haddou, A. Benomar, R. Abouqal, and M. Yahyaoui,
T
“Quality of life and multiple sclerosis: Arabic language translation and transcultural
IP
adaptation of ‘mSQOL-54,’” Rev. Neurol. (Paris)., 2012.
[123] T. Catic, J. Culig, E. Suljic, A. Masic, and R. Gojak, “Validation of the Disease-specific
Questionnaire MSQoL-54 in Bosnia and Herzegovina Multiple Sclerosis Patients Sample,”
R
Med. Arch. (Sarajevo, Bosnia Herzegovina), 2017.
[124] R. Estiasari et al., “Validation of the Indonesian version of multiple sclerosis quality of life-
SC
54 (MSQOL-54 INA) questionnaire,” Health Qual. Life Outcomes, 2019.
[125] R. Rosato et al., “Development of a short version of MSQOL-54 using factor analysis and
item response theory,” PLoS One, 2016.
U
[126] G. Baker, K. P. S. Nair, K. Baster, R. Rosato, and A. Solari, “Reliability and acceptability of
the Multiple Sclerosis Quality of Life-29 questionnaire in an English-speaking cohort,” Mult.
AN
Scler. J., 2019.
[127] B. Stern, T. Hojs Fabjan, K. Rener-Sitar, and L. Zaletel-Kragelj, “Validation of the Slovenian
version of multiple sclerosis quality of life (MSQOL-54) instrument,” Zdr. Varst., 2017.
[128] M. Debouverie, S. Pittion-Vouyovitch, S. Louis, and F. Guillemin, “Validity of a French
M
version of the fatigue impact scale in multiple sclerosis,” Mult. Scler., 2007.
[129] R. Rosato et al., “eMSQOL-29: Prospective validation of the abbreviated, electronic version
D
of MSQOL-54,” Mult. Scler. J., 2019.
[130] Y. Zhang, B. V. Taylor, S. Simpson, L. Blizzard, A. J. Palmer, and I. van der Mei,
TE
“Validation of 0–10 MS symptom scores in the Australian multiple sclerosis longitudinal
study,” Mult. Scler. Relat. Disord., 2020.
[131] M. C. Simeoni et al., “Validation of the Multiple Sclerosis International Quality of Life
questionnaire,” Mult. Scler., 2008.
EP
[132] N. Triantafyllou, A. Triantafillou, and G. Tsivgoulis, “Validity and reliability of the greek
version of the multiple sclerosis international quality-of-life questionnaire,” J. Clin. Neurol.,
2009.
C
[133] K. Baumstarck-Barrau, J. Pelletier, M. C. Simeoni, and P. Auquier, “French validation of the
Multiple Sclerosis International Quality of Life Questionnaire,” Rev. Neurol. (Paris)., 2011.
AC
[134] O. Fernández et al., “Validation of the spanish version of the multiple sclerosis international
quality of life (musiqol) questionnaire,” BMC Neurol., 2011.
[135] A. Jamroz-Wiśniewska, Z. Stelmasiak, and H. Bartosik-Psujek, “Validation analysis of the
Polish version of the Multiple Sclerosis International Quality of Life Questionnaire
(MusiQoL),” Neurol. Neurochir. Pol., 2011.
[136] J. Thumboo, A. Seah, C. T. Tan, B. S. Singhal, and B. Ong, “Asian adaptation and validation
of an English version of the multiple sclerosis international quality of life questionnaire
(MusiQoL),” Ann. Acad. Med. Singapore, 2011.
[137] A. G. Beiske, K. Baumstarck, R. M. Nilsen, and M. C. Simeoni, “Validation of the multiple
sclerosis international quality of life (MusiQoL) questionnaire in Norwegian patients,” Acta
Neurol. Scand., 2012.
[138] S. Y. Huh et al., “Validity of Korean versions of the multiple sclerosis impact scale and the
Information Classification: General
multiple sclerosis international quality of life questionnaire,” J. Clin. Neurol., 2014.
[139] P. Gompertz, P. Pound, and S. Ebrahim, “Validity of the extended activities of daily living
scale,” Clin. Rehabil., 1994.
[140] J. Lopes, E. L. Lavado, A. P. Kallaur, S. R. de Oliveira, E. M. V. Reiche, and D. R. Kaimen-
Maciel, “Assessment of fatigue in multiple sclerosis: methodological quality of adapted
original versions available in Brazil of self-report instruments,” Fisioter. e Pesqui., 2014.
[141] D. AER, P. CJ, G. JRF, and L. PA, “Development and validation of the Nottingham Leisure
Questionnaire (NLQ),” Clin. Rehabil., 2001.
[142] G. M., J. R., E. G., A. S. M., and R. A. A., “Validity and reliability of Persian version of
Modified Fatigue Impact Scale (MFIS) questionnaire in Iranian patients with multiple
sclerosis.,” Disabil. Rehabil., 2013.
T
[143] B. G. Vickrey, R. D. Hays, B. J. Genovese, L. W. Myers, and G. W. Ellison, “Comparison of
IP
a generic to disease-targeted health-related quality-of-life measures for multiple sclerosis,” J.
Clin. Epidemiol., 1997.
[144] L. B. Mokkink et al., “The COSMIN checklist for assessing the methodological quality of
R
studies on measurement properties of health status measurement instruments: An
international Delphi study,” Qual. Life Res., 2010.
SC
[145] L. B. Mokkink et al., “The COSMIN checklist for evaluating the methodological quality of
studies on measurement properties: A clarification of its content,” BMC Med. Res.
Methodol., 2010.
U
[146] J. F. Kurtzke, “Rating neurologic impairment in multiple sclerosis: An expanded disability
status scale (EDSS),” Neurology, 1983.
AN
[147] J. Iriarte and P. Castro, “Correlation between sympotom fatigue and muscular fatigue in
multiple sclerosis,” Eur. J. Neurol., vol. 5, no. 6, pp. 579–585, Nov. 1998.
[148] N. E. Carlozzi, N. R. Boileau, S. L. Murphy, T. J. Braley, and A. L. Kratz, “Validation of the
Pittsburgh Fatigability Scale in a mixed sample of adults with and without chronic
M
conditions,” J. Health Psychol., 2019.
[149] F. P., K. H., M. H., M. G., and R. P., “Fatigue in multiple sclerosis: Validation of the
D
WEIMuS scale (‘Wurzburger Erschopfungs-Inventar bei Multipler Sklerose’),” Neurologie
und Rehabilitation. 2008.
TE
[150] J. Greenhalgh, H. Ford, A. F. Long, and K. Hurst, “The MS Symptom and Impact Diary
(MSSID): Psychometric evaluation of a new instrument to measure the day to day impact of
multiple sclerosis,” J. Neurol. Neurosurg. Psychiatry, 2004.
[151] H. Ghaem, A. Haghighi, P. Jafari, and A. Nikseresht, “Validity and reliability of the Persian
EP
version of the multiple sclerosis quality of life questionnaire,” Neurol. India, 2007.
C
AC
Information Classification: General
Descriptio Reccomendation
Name Languages ADM Chacacteristics MS type Setting
Assessment tools specific for Fatigue in MS
Fatigue Severity Scale (FSS) [44]– English, Turkish, German, Arabic, Norwegian, I/SR The Fatigue Severity Scale is a 9-item scale which measures the severity of PP, RR, Research and Clinical
[49], [52]–[61] Swedish, Persian, Russian, Finnish, Greek, fatigue and its effect on a person's activities and lifestyle in patients with a SP
Dutch, Italian variety of disorders. The short version si composed by 7 items
T
Fatigue Severity Scale-7item (FSS- Swedish I PP, RR, Research and Clinical
IP
7) [63] SP
Unidimensional Fatigue Impact French-(Canada) English (Canada), French, SR The Unidimensional Fatigue Impact Scale (U-FIS) is a disease-specific PP, RR, Research and Clinical
Scale (U-FIS) [51], [62], [73] German, Italian. Spanish, Swedish, English patient-reported outcome measure which measures the impact of multiple SP
R
(USA) sclerosis related fatigue. It is a 22-item unidimensional scale which is based
on needs-based quality of life theory.
SC
Fatigue Impact Scale (FIS) [38], English, Swedish, Turkish, French, Hungarian, I/SR The FIS was developed to assess the symptom of fatigue as part of an PP, RR, Research and Clinical
[43], [44], [84], [95], [106], [117], Persian, Russian underlying chronic disease or condition. Consisting of 40 items, the SP
[128] instrument evaluates the effect of fatigue on three domains of daily life:
cognitive functioning, physical functioning, and psychoso- cial functioning.
U
Daily Fatigue. Impact Scale (D-FIS) Spanish SR The D-FIS is an eight-item version of the FIS designed for daily use in PP, RR, Clinical
[27] clinical practice. It comprises three items from the physical domain, four SP
AN
items from the cognitive domain, and one item from the psychosocial domain.
Modified Fatigue Impact Scale Dutch, Italian, Spanish, French, Slovenian, I/SR The MFIS is a modified form of the Fatigue Impact Scale (Fisk et al, 1994b) PP, RR, Research and Clinical
(MFIS) [52], [59], [61], [64]–[72], Portuguese (Brazil), Polish, English, Persian, based on items derived from interviews with MS patients concerning how SP
[74], [76] Greek, Japanese, Arabic, German fatigue impacts their lives.
M
Modified Fatigue Impact Scale – Spagnish SR PP, RR, Research and Clinical
5item (M-FIS-5)[77] SP
Neurological Fatigue Index - Dutch, Portuguese (Brazil), English, German I/SR The NFI-MS consists of 23 items in four subscales of Physical (8 items), PP, RR, Research and Clinical
Multiple Sclerosis ( NFI-MS) [78]– Cognitive (4 items), Relief by diurnal sleep or rest (6 items) and Abnormal SP
D
[81] nocturnal sleep and sleepiness (5 items)
German , Danish I/SR The FSMC is a 20-item sclae developed as a measure of cognitive and motor PP, RR, Clinical
Fatigue Scale for Motor and
Cognitive Functions (FSMC) [72],
TE fatigue for people with MS. A Likert-type 5-point scale (ranging from 'does
not apply at all' to 'applies completely')
SP
[82], [83]
Comprehensive Fatigue Assessment Persian - The CFAB-MS, in addition to assessment of the fatigue, evaluates factors PP, RR, Clinical
EP
Battery for Multiple Sclerosis related to fatigue, including sleep, pain, mobility, stress, anxiety, mood and SP
(CFAB-MS) [85] fatigue management skills.
Chalder fatigue scale (CFQ) [72], English, German SR The Chalder fatigue scale (CFQ) is a questionnaire created to measure the PP, RR, Clinical
[86] severity of tiredness in fatiguing illnesses. SP
C
Chronic Fatigue Syndrome English I The CFS SQ Symptom Inventory consisted of 19items assessing fatigue and PP, SP Clinical
Screening Questionnaire (CFS illness-related symptoms during the previousmonth.
AC
SQ) [87]
Checklist Individual Strength Dutch SR/I The CIS20R contains 20 statements, scored on a seven-point scale (1-7), PP, SP Clinical
(CIS20R) [59] reflecting four aspects of fatigue: subjective feeling of fatigue, reduction of
concentration, reduction of motivation, and reduction of physical activity.
Fatigue Assessment Inventory English - The 29-item scale is designed to evaluate four domains of fatigue: its severity, PP, RR, Clinical
(FAI) [90] pervasiveness, associated consequences, and response to sleep. SP
Fatigue Descriptive Scale (FDS) Spanish I FDS is a five-category interview-based scale used to assess fatigue in three PP, RR, Clinical
[147] categories: fatigue associated with asthenia; fatigue with exercise; fatigue with SP
worsening symptoms
Information Classification: General
Fatigue Symptoms and Impacts English I The FSIQ-RMS measures fatigue symptoms and impacts in relapsing multiple RR Clinical
Questionnaire - Relapsing Multiple sclerosis
Sclerosis (FSIQ-RMS) [92]
Multidimensional Assessment of Persian SR The MAF is a 16 item scale that measures fatigue according to four PP, RR, Clinical
Fatigue (MAF) [93] dimensions: degree and severity, distress that it causes, timing of fatigue (over SP
the past week, when it occurred and any changes), and its impact on various
activities of daily living (household chores, cooking, bathing, dressing,
working, socializing, sexual activity, leisure and recreation, shopping,
walking, and exercising).
T
Multiple Sclerosis-Fatigue Self– English SR The MS-FSE is composed by 6 items consists of a 10-point numeric rating PP, RR, Clinical
Efficacy (MS-FSE) [94] scale (ranging from 10-100) SP
IP
Pittsburgh Fatigability Scale (PFS) English SR The 10-item PFS physical fatigability score is a valid and reliable measure of SP Clinical
[148] perceived fatigability in older adults and can serve as an adjunct to
performance-based fatigability measures for identifying older adults at risk of
R
mobility limitation in clinical and research settings.
PROMIS-Fatigue English - The PROMIS-Fatigue PP, SP Clinical
SC
MS[96] MS is a 10-item scale designed for use across chronic
Diseases asking “How often” people experience fatigue in activities of daily
living
Swedish Occupational Fatigue Svedish I The SOFI was developed to measure subjective dimensions of work-related PP, RR, Clinical
U
Inventory SOFI[98] fatigue. The instrument consists of 20 items, in which feelings of being tired SP
are graded from 0 (not had such feelings at all) to 6 (had such feelings to a
AN
very high degree) (23).
W ürzburger Erschöpfungs- German SR The WEIMuS consists of 17 items with 5 categories each (0-4) resulting in a PP, RR, Clinical
Inventar bei Multipler Sklerose total sum score of 68, with subscores for cognitive (0-36) and physical (0-32) SP
(WEIMuS)[100], [149] fatigue.
M
Assessment tools including a Fatigue domain in the questionnaire
Brief patient-reported outcome for English I The BPRO-MS combines MS-related psychosocial and quality of life domains PP, RR, Clinical
D
MS (BPRO-MS) [102] SP
Clinician Rating of Multiple English I The CRoMS is a brief clinician-reported outcome measure of multiple PP, RR, Clinical
Sclerosis (CRoMS) [103]
Functional Assessment of Multiple
TE
English, Spanish, Portuguese, Italian, Danish I/SR
sclerosis signs and symptoms:
The FAMS allows assessment of overall physical health as reported by
SP
PP, RR, Research and Clinical
Sclerosis (FAMS) [104], [105], patients SP
[107]–[109]
EP
Leeds Multiple Sclerosis Quality of English, Turkish I/SR The LMSQOL IS an 8-item, unidimensional disease-targeted measure of PP, RR, Research and Clinical
Life (LMSQOL) [110]–[112] quality of life (QOL) SP
C
MS Symptom and Impact Diary English SR The majority of items in the MSSID focus on the physicalsymptoms of MS PP, RR, Clinical
(MSSID) [150] and their impact on daily activities, which issimilar to the item content of the SP
AC
MSIS-29.9However, like theMSIS-29, it also includes important items that
address theemotional impact of the condition. The MSSID consists ofthree
factors that measure mobility, the cognitive andemotional aspects of fatigue,
and the overall impact of MS
MSQOL-54 [114]–[116], [118]– English, Italian, Hebrew, Turkish, Finnish, SR/ The MSQOL is one of the most wide used disease specific instrument for PP, RR, Research and Clinical
[124], [127], [151] Persian, Serbian, Hungarian, Arabic, Bosnian, I measuring health related quality of life SP
Indonesian, Slovenian
MSQOL-54 Italian SR PP, RR, Research and Clinical
SF [125] SP
Information Classification: General
eMSQOL-29 SF [126], [129] Italian, English SR PP, RR, Research and Clinical
SP
Multiple Sclerosis International Spanish (Argentina), French, German, Greek, SR MusiQoL)questionnaire, a multi-dimensional, self-administered questionnaire, PP, RR, Research and Clinical
Quality of Life questionnaire Hebrew, Italian, Norwegian, Russian, Spanish, is a valid and reliable multidimensional, 31-item questionnaire for assessing SP
(MusiQoL) [75], [131], [132], [135], Turkish, English, Arabic, Spanish, English disease-specific QoL in people with MS
[137], [138] (Singapore, Malaysia, India), Polish, Korean
Multiple Sclerosis International English I PP, RR, Research and Clinical
Quality of Life questionnaire SP
T
multidimensional computerized
adaptive short-form questionnaire
IP
(MusiQoL-MCAT) [28]
Quality of Life in Neurological English, Spanish SR The NeuroQOL is a self-report of health related quality of life in 17 domains PP, RR, Research and Clinical
Disorders (Neuro-QoL) [29], [32] and sub-domains for adults, is a measurement system that evaluates and SP
R
monitors the physical, mental, and social effects experienced by adults and
Quality of Life in Neurological English SR/I children living with neurological conditions. PP, RR, Research and Clinical
SC
Disorders – short form (Neuro-QoL SP
SF) [30], [31]
Performance Scale (PS) [35], [40] English SR The PS allows patients to be classified as to their functional impairment. The PP, RR, Research and Clinical
U
lower the Karnofsky score, the worse the survival for most serious illnesses. SP
Symptom inventory (SI) [40] English SR The 99-item SI. Initial validation of the SI supported the PP, RR, Clinical
AN
reliability and validity of its 6 subscales designed to SP
reflect localization of brain lesions (visual, left and right
hemisphere, brainstem and cerebellum, spinal cord, and
nonlocalized symptoms)
M
SymptoMScreen [41], [42] English I/SR SymptoMScreen is a single-page battery of Likert scales that assesses PP, RR, Clinical
symptom impact in 12 domains commonly affected in MS SP
ADM=Administration; I=Interview; SR= Self-report; MS= Multiple Sclerosis; PP= Primary Progressive; RR= Replapsing Remittent; ; Secondary Progressive
D
Table 1 - summary and description of most important instruments for fatigue
TE
EP
C
AC
Information Classification: General
Table 2 Properties of instruments specific for Fatigue
Scales Authors (year of publication) Language Demographic information ADM Cronbach's Test-retest Construct
Sample Mean age (SD) Gender F MS Years from EDSS Alpha Validity
Size % (PP,RR,SP) diagnosis mean (SD)
(SD)
FSS Krupp et al. (1989)[6] English 25 44.8 (10) - - - - I 0.81 - -
Mills et al. (2009) [67] English 416 45.8 (10.5) 70.4 31, 246, 133 - - SR - - -
T
Armutlu et al. (2007) [47] Turkish 72 38.16 (10.03) 61.1 - 9.5 (6.43) 4 SR/I 0.89-0.94 0.81 -
IP
Reske et al. (2006) [48] German 20 39.1 70 - 3 3.2 (1.9) - 0.95 0.69 VAS
Al-Sobayel (2016) [49] Arabic 24 29.8 (6.5) 87.5 - - - SR 0.84 0.80 RAND-36
R
Valko at al. (2008) [50] German 188 44 (13) 67 - 11.07 3.61 (2.26) SR 0.94 - VAS, ESS
(9.79)
SC
Learmonth et al. (2013) [52] English 86 49.2 (9) 76.7 7, 67,12 11.8 (8.2) - SR - 0.75 PDSS
Lerdal et al. (2010) [53] Norwegian 368 49.1 (11.7) 72.3 - 11.4 (8.3) - SR - - -
Lerdal et al. (2010) [53] Swedish 228 46.6 (12.4) 69 - 14 (10.4) -
U
Salehpoor et al. (2013) Persian 162 - - SR 0.93 0.43 - 0.85 -
AN
Gavrilov et al. (2018) [44] Russian 85 37.6 (10.2) 62.4 7, 65,13 - 2.9 (1.6) SR 0.88/0.96 0.78/0.89 HADS, ESS,
Rosti-Otajarvi et al. (2017) [55] Finnish 553 53.8 (11.4) 78.7 94, 244, 160 16.4 (9.3) 4 (2.5) SR 0.95 - MSIS-29, EQ-
5D, VAS,
M
EDSS
Bakalidou et al. (2013) [56] Greek 72 43.2 (10.19) 66.7 - - 2.4 (1.56) SR 0.95 0.89 BDI-II, SF-
36v2
D
Ghotbi et al. (2013) [57] Persian 30 33.6 (5.38) 70 - - 4.68 (1.32) SR 0.92 0.78 VAS, EDSS
Hernandez-Ronquillo et al. English TE30 40.2 20/80 - - - SR - - BDI
(2011) [58]
Rietberg et al. (2010) [59] Dutch 43 48.7 (7) 69.8 7, 26, 10 14.5 (9.2) - SR/I - 0.76 EDSS
Ottonello et al. (2016) [60] Italian 156 46.03 (11.17) 39.1 21, 97, 38 8.9 (8.4) 4.5 (1.5) SR 0.95 - -
EP
Rooney et al. (2019) [61] English 365 46.2 (11.6) 81.9 34,253,68 9.6 (8.7) SR - - EQ-5D-3L,
MSIS-29
FSS-7 Johansson et al. (2014)[63] Swedish 224 46.5 (12.4) 68 - 14 (10) - I - - -
C
U-FIS Meads et al. (2009)[51] English 135 50 (11.8) 68.1 24, 46, 38 14.7 (11.7) - SR 0.96 0.86 NHP, HADS
AC
Twiss et al. (2010)[73] French-English 911 36.5 (8.4) 67.9 4.8 (5.2) - SR 0.97 - EDSS, MSFC,
(Canada) PASAT,
French - EQ-5D
German
Italian
Spanish
Swedish
English (USA)
Doward et al. (2010) [62] English (Canada) 96 44.5(9.9) 74 4,70,5 1.6(8.5) - SR 0.98 0.89 NHP
Information Classification: General
French (Canada) 102 46.1(10.5) 64.4 7,39,19 10.4(7.5) - 0.96 0.86
French 85 48.5(10.4) 66.5 17,12,23 15.3(9.4) - 0.96 0.89
German 76 42.1 (12.3) 71.1 7,40,9 8.8(8) - 0.97 0.92
Italian 100 53.1 (12.1) 65 29,17,29 17.8(10.8) - 0.96 0.91
Spanish 87 43.6 (11) 54.4 6,41,16 9(7.3) - 0.95 0.86
Swedish 167 48.7 (12.1) 61.1 14,47,25 15.4(10.1) - 0.97 0.91
T
English 104 45.7 (10.8) 81.7 4,82,10 10.1(8.9) - 0.96 0.88
IP
FIS Fisk et al. (1994)[84] English 333 52 - - - - SR 0.92 0.86 MSIS-29
MSWS-12
R
GHQ-30
Mathiowetz et al. (2003)[95] English 54 50 67 - 9.5 - SR - 0.68 FSS, SF-36
SC
Flensner et al. (2005) [106] Swedish 161 - 74 - - - SR - - -
Armutlu et al. (2007)[117] Turkish 71 38.6(9.9) 60.6 - 9.4(6.39) 3.94 SR 0.91/0.93 0.83/0.95 -
U
Debouverie et al. (2007)[128] French 237 42.5(10.) 71.3 20,147,70 9.8(7.4) 3.7(1.7) SR 0.93 0.82 -
Losonczi et al. (2011)[38] Hungarian 111 43.82(11.62) 75 - 11.12(8.29) 1.94(1.37) I 0.987 0.85 -
AN
Heidari et al. (2015)[43] Persian 140 - 81.4 - - - SR 0.89 0.86 FSS, SF-36
Gavrilov et al. (2018)[44] Russian 85 37.6 (10.2) 62.4 7, 65,13 - 2.9 (1.6) SR 0.88/0.96 0.78/0.89 HADS, ESS,
M
D-FIS Benito-Leon et al. (2007)[27] Spanish 124 - 75 - - - SR 0.91 0.81 MADRS,
FAMS
MFIS Kos et al. (2003)[64] Dutch 51 51.9(10.5) 49 - - - I
D
Kos et al. (2005)[65] Italian 50 50.1(11.9) 62 4,19,27 14.4(10.6) SR 0.92 0.91 FSS
Spanish
TE
30 47.1(11.7) 76 1,10,19 11.3(6.8) 6
French 51 52.9(10.5) 49 11,14,18 16.6(8.9) 6.5
EP
Slovenian 50 44.6(11.7) 76 3,22,23 14.1(9.3)
Pavan et al. (2007)[66] Portuguese (Brazil) 57 38.2(9.42) 66,7 - 6.84(5.64) 3.3(2.39) SR 0.82 0.93 FSS, MFIS,
EVA
C
Gruszczah et al. (2009) Polish - - - - - - - - - -
Rietberg et al. (2010)[59] Dutch 43 48.7(7) 30 7,26,10 14.3(9.2) - SR/I - 0.85 -
AC
Mills et al. (2010) [67] English (UK) 415 - 70.6 - - - SR - - -
Ghajarzadeh et al. (2012)[68] Persian 120 30.6(8.1) 84.2 0,109,11 5.3(5.1) - SR 0.86 0.91 FSS
Learmonth et al. (2013)[52] English 86 49.2 (9) 76.7 7, 67,12 11.8 (8.2) - SR - 0.75 PDSS
Harirchian et al. (2013)[69] Persian - - - - - - - - - -
Bakalidou et al. (2014)[70] Greek 99 43.2(10.2) 24.2 - - 2.4(1.56) SR 0.96 0.86 FSS
Information Classification: General
Masuda et al. (2015)[71] Japanese 30 44.9(11.8) 80 - - - SR - - MFIS, PES
Khalil et al. (2019)[74] Arabic 145 36.6810.2) 65.5 - 8.4(5.5) - SR 0,91 0.95 FSS
Pust et al. (2019)[72] German 309 43.4(10) 66.6 - - - SR - - -
Rooney et al. (2019)[61] English (UK) 365 46.2(11.6) 81.9 34,253,68 9.6(8.7) - SR - - EQ-5D-3L,
MSIS-29
Farran et al. (2020)[75] Arabic 663 37.6(12.3) 65.2 23,544,58 - 2.2(2) - 0.96 - -
T
Alawami et al. (2020)[76] Arabic 116 34.7(6.9) 78.4 - - 4.2(1.5) SR 0.97 0.92 FSS, SF-36V,
VAS-F, BDI-II
IP
M-FIS-5 Meca-LaLlana et al. (2019)[77] Spagnolo 302 42.3(10.1) 64.2 13,273,16 SR 0.90 - -
NFI-MS Derksen et al. (2013)[78] Dutch 136 46(10.4) 83 - 9.7(6.8) - - - 0.75 FSS, MFIS,
R
NRS, HADS,
MSIS–29,
SC
EDSS
Lopes et al. (2016)[79] Portuguese 240 - 76.1 6,171,16 - - I - 0.84-0.86 ESS, FSS,
MFIS, MSIS-
29, NFI-
U
MS/BR, PSQI
Mills et al. (2015) English 208 48.3 24.5/75.5 SR - - -
AN
Mills et al. (2010)[80] English 318 46.4(10.6) 68.2 29,168,89 14.2(9.4) - I - 0.85 FSS - MFIS
FSMC Pust et al. (2019)[72] German (Germany) 1094 - - - - - SR - - MFIS
Penner et al. (2009)[82] German 309 43.4(9.9) 66.7 - - - I 0.91 0.86 MFIS, FSS
M
(Switzerland)
Oervik et al. (2017)[83] Danish 84 51.1(9.4) 69 - - 3.43(1.8) SR 0.91 - MFIS
D
German 309 43.4(9.9) 67 - - 3.68(1.2)
CFABMS Motaharinezhad et al. (2015)[85] Persian -
TE - - - - - - - - -
CFQ Chilcot et al. (2016)[86] English 444 - - - - - - - - WSAS, MFIS,
HADS
Pust et al. (2019)[72] German (Germany) 605 - - - - - SR - - FSMC, MFIS
EP
CFS Jason et al. (1997)[87] English 15 - 73.3 - - - I - - -
SQ
CIS20R Rietberg et al. (2010)[59] Dutch 43 48.7(7) 30 7,26,10 14.3(9.2) - SR/I - 0.85 -
C
FAI Schwartz et al. (1993)[90] English 40 - - - 0.70-0.92 0.50-0.70 -
AC
FAI/FSI Hernandez-Ronquillo et al. English 30 40.2 20/80 - - - SR - - BDI
(2011) [58]
FDS Iriarte et al. (1998)[147] Spanish 50 32.4(9.8) 52 - - 2.2(1.9) I - - FSS
FSIQ- Hudgens et al. (2019)[92] English - - - - - - I 0.94 0,928 RAND-35 -
RMS MFIS
MAFS Behrangrad et al. (2017)[93] Persian 130 35.6(4.18) 66.9 - 7.55(3.2) 2.17(1.43) SR 0.98 0.97-0.99 FIS
MS-FSE Thomas et al. (2014)[94] English 164 49.0(9.7) 73 - - - SR 0.89 - MSSE, SF-36
Information Classification: General
PFS Carlozzi et al. (2019)[148] English 65 52.2 (13.0) 84.6 - 13.8 (9.6) - SR 0.85/0.91 0.86 FSS, ESS
PROMIS- Cook et al. (2012)[96] English 231 53.6(10.8) 82.7 - 16.3(9.5) - - - - -
Fatigue
MS
PSF Marrie et al. (2005)[97] English 9324 52.39(10.8) 71.9 - - - SR - - MFIS, FSS
SOFI Johansson et al. (2008)[98] Svedish 219 47(12) 68.1 9,127,83 14 (10) - I 0.87–0.91 - FSS
Vas Kos et al. (2006)[99] Dutch 62 52(10.5) 53.2 14,16,20 6.5 SR - 0.69; FSS, MFIS
T
WEIMuS Flachenecker et al. (2006)[100] German 158 39.2(9.2) 77 7,96,53 9.9(6.7) 3.9(1.7) SR 0.922 - FSS - MFIS -
IP
VAS
Flachenecker et al. (2008)[149] German - - - - - - - - - -
R
SD= Standard Deviations; F= Female; ADM=Administration; I=Interview; SR= Self-report; EDSS= Expanded Disability Status Scale; VAS= Visual Analogic Scale; FSS= Fatigue Severity Scale; FIS= Fatigue Impact
Scale; U-FIS= Unidimensional Fatigue Impact Scale; D-FIS= Fatigue Impact Scale for Daily Use; MFIS= Modified Fatigue Impact Scale; NFI-MS= Neurological Fatigue Index – Multiple Sclerosis; CFABMS=
SC
Comprehensive Fatigue Assessment Battery for Multiple Sclerosis; CFQ= Chalder Fatigue Scale; CIS20R= Checklist Individual Strength 20 item; FAI= Fatigue Assessment Index; FAI/FSI= Fatigue/Assessment
Instrument/ Fatigue Severity Inventory; FDS= Fatigue Descriptive Scale; FSIQ-RMS= Fatigue Symptoms and Impact Questionnaire – Relapsing Multiple Sclerosis; MAFS= Multiple Assessment of Fatigue; MS-FSE=
Multiple Sclerosis-Fatigue Self-Efficacy; PFS= Piper Fatigue Scale; PSF= Post-Stroke Fatigue; SOFI= Swedish Occupational Fatigue Inventory; WEIMuS= Würzburg Fatigue Inventory for Multiple Sclerosis; ESS=
Epworth Sleepiness Scale; PDSS= Panic Disorder Severity Scale; HADS= Hospital Anxiety and Depression Scale; MSIS= Multiple Sclerosis Impact Scale; EQ= Health-Related Quality of Life Questionnaire; BDI= Beck
Depression Inventory; SF-36= 36-Item Short Form Survey; MSFC= Multiple Sclerosis Functional Composite; PASAT= Paced Auditory Serial Addition Test; NHP= Nottingham Health Profile; MSWS-12= 12-item
U
Multiple Sclerosis Walking Scale; GHQ= General Health Questionnaire; MADRS= Montgomery Asberg Depression rating scale; FAMS= Functional Assessment of Multiple Sclerosis; MSWS-12= 12-item Multiple
Sclerosis Walking Scale; EVA= Pain Comparison Whit Visual Analog Scale; PSQI= Pittsburgh Sleep Quality Index; MADRS= Montgomery Asberg Depression rating scale; WSAS= Work and Social Adjustment Scale;
AN
MOS= Medical Outcomes Study; EORTC QLQ-C30= European Organization for Research and Treatment of Cancer quality of life questionnaire
M
D
TE
EP
C
AC
Information Classification: General
Table 3 Properties of Instrument including a Fatigue domain in the questionnaire
Scales Authors (year of Language Demographic information ADM Cronbach's Test- Construct Validity
publication) Alpha retest
Sample Mean age Gender MS Years from EDSS mean
Size (SD) F% (PP,RR,SP) diagnosis (SD) (SD)
BPRO-MS Chua et al. (2015)[102] English 537 46.4(11.23) 73.2 - - - I 0.82 -
CRoMS Matza et al. (2019) English 14 51.1 78.6 1,6,6 - - I - - -
eVas Kos et al. (2017) Dutch 52 49.1(8.9) 65.4 - - - SR - 0.91 -
T
FAMS Cella et al. (1996)[104] English 377; 56 44.9 70 - - 4.6(2.2) SR 0.91/0.89 0.85 SF-36, HADS, MDI,
IP
PSR, MCSDS,
EDSS, NRS
Chang et al. (2002)[105] Spanish 625 37.25(9.9) 66 25,462,122 8.8(6.6) 3(2) SR 0.92 - MSQOL-54 - MSQLI
R
Mendes et al. (2004)[107] Portuguese 143 34.8(8.1) 78.1 - - 2.19(1.65) I 0.81 - EDSS
SC
Patti et al. (2007)[108] Italian 344 36.9(9.9) 64.8 13,261,45 6(5.4) 2.5(1.7) I 0.93 0.96 -
Sørensen et al. (2011)[109] Danish 190 - 59 34,56,98 - - SR 0.91 EDSS
U
LMSQOL Ensari et al. (2015)[110] English 292 48(10.3) 80.9 12,246,34 10.3(7.9) - SR - - HADS, MSIS-29,
SWLS, MSSE, SF-
12, FSS, MPQ,
AN
LLFDI, PDDS,
EXSE, GLTEQ
Akbiyik et al. (2009)[112] Turkish 69 38.4(9.7) 59.4 - - - I 0.74-0.78 - -
M
Ford et al. (2001)[111] English 180 47.1 76 36,46,44 - - SR 0.79 0.85 GWBI, SF-36 PF
MSSID Greenhalgh et al. English 63 46(10) 81 - 11(8) - SR 0.78–0.88 0.79- MSQol-54,
(2003)[150] 0.96 LMSQoL, RNLI,
D
LHS
MSQOL-54 Vickrey et al. (1995)[114] English 179 TE 45 72 - 9 - SR/ 0.84 0.85 -
I
Solari et al. (1999)[115] Italian 204 42.6(11.2) 52 - 12.8(8.9) 4.5(2.1) SR/ >0.70 - EDSS, BDI, MMSE
I
EP
Miller et al. (2005)[116] Hebrew 215 43.3(11.05) 76 - 3.2(0.84) - I 0.94 - EDSS
Idiman et al. (2005)[118] Turkish 183 39.2(10.6) 75.4 6,145,32 - - SR - - EDSS
Heiskanen et al. (2006) Finnish 81 43 72.8 - - - SR 0.88 - -
C
[119]
Ghaem et al. (2007)[151] Persian 146 32.6(9.6) 75.2 4,105,28 3.8(7.2) 2.3(2.1) SR 0.77 - -
AC
Pekmezovic et al. Serbian 200 37.7(8.2) 67 21,124,55 10.1(6.2) 3.8(1.8) SR 0.82 - EDSS
(2007)[120]
Füvesi et al. (2008)[121] Hungarian 438 43.3(11.1) 74 9,332,35 10.1(7.8) 2.6(1.8) SR 0.84 - -
Taoussi et al. (2012)[122] Arabic 78 39(10) 70.5 10,41,27 9(6) - SR 0.76 - -
Catic et al. (2017)[123] Bosnian 62 39.8(10.9) 61.3 - - 2.9(1.9) SR 0.83 - EDSS
Estiasari et al. (2019)[124] Indonesian 43 30 79.1 - - 3 SR/I 0.72 - EDSS
Information Classification: General
Stern et al. (2017)[127] Slovenian 134 43.2(11.1) 68.7 6,105,23 - - SR 0.84 - -
MSQOL-54 Rosato et al. (2016)[129] Italian 473 40.8(11.3) 64 - - - SR 0.88 0.89 FAMS, EQ-5D-3L,
SF HADS, EDSS
eMSQOL-29 Rosato et al. (2019)[125] Italian 623 44.3(11.5) 68.1 29,498,79 - - SR - - -
SF
Baker et al. (2018)[126] English 100 42.8(9.1) - 2,87,2 5.5(7) - SR 0.87 0.91; -
0.97
MSSymptom Zhang et al. (2020)[130] English 1985 55.3(11.3) 78.1 - - - SR - 0.68 FSS
T
Scores
MusiQol Simeoni et al. (2008)[131] Spanish 1992 42.2(12.6) 60.5 138,1365,4 3.2(2.1) SR 0.92 0.87 -
IP
(Argentina) 07
French
German
R
Greek
Hebrew
SC
Italian
Norwegian
Russian
Spanish
Turkish
U
English (UK)
English
AN
(USA)
Arabic
Triantafyllon et al. Greek 92 40.2(13.9) 35 2,74,16 - - SR 0.95 0.99 -
(2009)[132]
M
Fernández et al. (2011)[134] Spanish 224 39(10) 70.4 6,176,40 10.6(7.2) 2.9(2) SR 0.70-0.92 0.60- SF-36,14-symptom
0.91 scales
Baumstarck-Barrau et al. French 179 44.1(11.5) 67.5 37,69,47 - 4.5 SR 0.91 - SF36,14-symptom
D
(2011)[133] scales
Thumboo et al. (2011)[136] English 66 42.7 78 2,42,16 - - SR 0.94; 0.92 - SF-36
(Singapore,
Malaysia,
TE
India)
Jamroz-Wiœniewska et al. Polish 150 41(10) 73 17,60,73 11.7(7.2) - SR 0.90 - EDSS, FAMS,
EP
(2011)[135] MSIS-29
Beiske et al. (2012)[137] Norwegian 104 50(9) 65.4 25,34,45 - 5(2) SR 0.34-0.79 0.86 SF-36
Huah et al. (2014)[138] Korean 56 36.5(8.6) 57.1 2,36,2 5.7(4.7) 2(1.9) SR 0.77-0.96 0.59- EDSS
C
0.92
Farran et al. (2020)[75] Arabic 663 37.6(12.3) 65.2 23,544,58 - 2.2(2) - 0.96 - -
AC
MusiQoL- Michel et al. (2016)[28] English 1992 42,2(11.9) 70.5 - - - I - 0.60 - SF-36
MCAT 0.78
Neuro-QoL Gershon et al. (2011)[32] English 581 55.21(14.3) 54 - - - SR 0.99 - -
Spanish
Correia et al. (2014)[29] Spanish - - - - - - - - - -
Neuro-QoL Miller et al. (2016)[30] English 161 49.8(10.5) 86 - - - SR/I 0.81-0-95 0.76- MSFC, PASAT,
SF 0.91 FAMS, MSPS, EQ-
5D, KPS, SDMT,
GHS, GHQ, GRC
Information Classification: General
Medina et al. (2019)[31] English 902 46.8(12.2) 76.1 44,705,82 9.1(8.1) - SR 0.96 - -
PERSEPP Ghajarzadeh et al. Persian 211 32.2(8.4) 79.1 - 6.5(2.5) - SR 0.81 0.88 MSQOL-54 , SF-36
(2016)[33]
Baroin et al. (2013)[34] French 305 41(9.8) 77.1 - 7.4(6.1) 2.2(1.7) SR 0.74 0.86 SF-12, EHD,
MusiQoL
PS Schwartz et al. (1999)[37] English 274 46(12) 71 12,44,39 8.8(8.1) - SR 0.78 0.89 EDSS, DD, DS, AI,
HSQS, Quality of
Well-Being Index
T
Marrie et al. (2007)[35] English 44 42.2(8.1) 79.6 1,30,10 8.3(6.7) - SR - - MSQLI, MSFC
IP
PSS Chamot et al. (2014) English 7851 46(11) 79.4 - 15(11.3) - SR - - PDDS
Symptom Schwartz et al. (1999)[37] English 274 46(12) 71 12,44,39 8.8(8.1) - SR 0.78 0.89 EDSS, DD, DS, AI,
R
inventory HSQS, Quality of
Well-Being Index
SC
Symptom Schwartz et al. (2012)[39] English 1142 54.4(9.2) 75.1 - - - SR 0.77-0.95 - PDDS, PS, SF-12
inventory
disability- Schwartz et al. (2012)[40] English 1532 54.21(9.41) 75 - - - SR 0.88 - -
specific short
U
forms
SymptoMScr Green et al. (2016)[41] English 410 46.6(12.9) 74 - 12.2(8.6) - I - 0.71- PDDS, PS, SF-12
AN
een 0.94
Fitzgerald et al. (2019)[42] English 162 47.6(12.3) 73,9 - - - SR 0.93 ≥0.70 PS-F
SD= Standard Deviations; F= Female; I=Interview; SR= Self-report; EDSS= Expanded Disability Status Scale; BPRO-MS: Brief Patient-reported outcomes in multiple sclerosis; CRoMS: Clinician Rating of Multiple
Sclerosis; eVAS: Electronic visual analogue scales; FAMS= Functional Assessment of Multiple Sclerosis; LMSQOL= Leeds Multiple Sclerosis-QoL; MSSID= The MS Symptom and Impact Diary; MSQOL-54= Multiple
M
Sclerosis Quality of Life-54; MSQOL-29 SF= Multiple Sclerosis Quality of Life-29 short form; eMSQOL-54= electronic version Multiple Sclerosis Quality of Life-54; MDI, PSR= Performance Status Rating, MCSDS=
Marlowe-Crowne Social Desirability Scale; NRS= fatigue numeric rating scale; SWLS= Satisfaction With Life Scale, SF-12= 12-Item Short Form Survey; SF-36= 36-Item Short Form Survey; MPQ= McGill Pain
Questionnaire; LLFDI= Late-Life Function and Disability Instrument; PDDS= Patient-Determined Disease Steps; EXSE= exercise self-efficacy; GLTEQ= Godin Leisure-Time Exercise Questionnaire; GWBI=
D
Psychological General Well-Being Index; RNLI= Reintegration to Normal Living Index; LHS= London Handicap Scale; MMSE= Mini Mental State Examination; HADS= Hospital Anxiety and Depression Scale; EQ=
Health-Related Quality of Life Questionnaire; PS=Performance Scale; PSS=Performance Scale Sum.
TE
EP
C
AC
Information Classification: General
Table 4 Quality assessment of included studies evaluating instruments specific for Fatigue
Scales Authors (year of publication) Language Item
1 2 3 4 5 6 7 8 9 10
FSS Krupp et al. (1989)[6] English
+ + - + - - - + - -
Mills et al. (2009) [67] English
+ - - + + + + + - +
Armutlu et al. (2007) [47] Turkish
+ + - + + - - + - -
T
Reske et al. (2006) [48] German
+ + - + + + + - - -
IP
Al-Sobayel (2016) [49] Arabic
+ + - + - - - - - -
Valko at al. (2008) [50] German
R
+ + - + + - - + - -
Learmonth et al. (2013) [52] English
- + - + - - - + - -
SC
Lerdal et al. (2010) [53] Norwegian + - - + + - - + - +
Lerdal et al. (2010) [53] Swedish + - - + + - - + - +
Persian + + ? + ? ? ? ? ? ?
U
Salehpoor et al. (2013)
Gavrilov et al. (2018) [44] Russian + + - + - + + + - -
AN
Rosti-Otajarvi et al. (2017) [55] Finnish + + - + + + - + + +
Bakalidou et al. (2013) [56] Greek + + + + + + + + - +
M
Ghotbi et al. (2013) [57] Persian + + - + + + + - - -
Hernandez-Ronquillo et al. (2011) [58] English - - + ? ? ? ? ? ? ?
D
Rietberg et al. (2010) [59] Dutch - + - + - + - - + +
Ottonello et al. (2016) [60] Italian TE + + - + + + + - - -
Rooney et al. (2019) [61] English + - - + + + + - + +
FSS-7 Johansson et al. (2014)[63] Swedish + - - + + - - + + -
EP
U-FIS Meads et al. (2009)[51] English + + + + + + + + + +
Twiss et al. (2010)[73] French- + - - + + + + + + +
English
C
(Canada)
French
AC
German
Italian
Spanish
Swedish
English
(USA)
Doward et al. (2010) [62] English + + - + + + + + + +
(Canada)
French + + - + + + + + + +
(Canada)
Information Classification: General
French + + - + + + + + + +
German + + - + + + + + + +
Italian + + - + + + + + + +
Spanish + + - + + + + + + +
Swedish + + - + + + + + + +
English + + - + + + + + + +
T
FIS Fisk et al. (1994)[84] English + - - + - + - + - -
IP
Mathiowetz et al. (2003)[95] English - + - + + + - + + +
R
Flensner et al. (2005) [106] Swedish + + - + + + + + + +
Armutlu et al. (2007)[117] Turkish + + - + + + - - - +
SC
Debouverie et al. (2007)[128] French + + - - - + + - + -
Losonczi et al. (2011)[38] Hungarian + + - + + + - + - -
U
Heidari et al. (2015)[43] Persian + + - + + + - + - -
AN
Gavrilov et al. (2018)[44] Russian + + - + + - + + + +
D-FIS Benito-Leon et al. (2007)[27] Spanish + + - + + + - + - +
MFIS Kos et al. (2003)[64] Dutch - - - + - + - + + -
M
Kos et al. (2005)[65] Italian + + - + + + - - - -
Spanish + + - + + + - - - -
D
French + + - + + + - - - -
Slovenian
TE + + - + + + - - - -
Pavan et al. (2007)[66] Portuguese - + - + - + + - - -
(Brazil)
EP
Gruszczah et al. (2009) Polish - + - + - + + - - -
Rietberg et al. (2010)[59] Dutch - + - + - + - - + +
Mills et al. (2010) [67] English (UK) + - - + + - - + - -
C
Ghajarzadeh et al. (2012)[68] Persian + + - + - + - + - -
AC
Learmonth et al. (2013)[52] English
- + - + - - - + - -
Harirchian et al. (2013)[69] Persian - + - + + - - - - -
Bakalidou et al. (2014)[70] Greek + + - + + - - + - -
Masuda et al. (2015)[71] Japanese - + - + + - - + - -
Khalil et al. (2019)[74] Arabic + + + + + + + + + +
Information Classification: General
Pust et al. (2019)[72] German + - + + + + + - + +
Rooney et al. (2019)[61] English (UK) + - - + + + + - + +
Farran et al. (2020)[75] Arabic + + - + + - - - - -
Alawami et al. (2020)[76] Arabic + + + + + - + + + -
M-FIS-5 Meca-LaLlana et al. (2019)[77] Spagnolo + + - + + - + - - -
Derksen et al. (2013)[78] Dutch - + + + + + + + + -
T
NFI-MS
Lopes et al. (2016)[79] Portuguese - + + + + + + + - -
IP
Mills et al. (2015) English - - - + - + - + + +
R
Mills et al. (2010)[80] English - + - + + + + - + +
Pust et al. (2019)[72] German + - + + + + + - + +
SC
FSMC
(Germany)
Penner et al. (2009)[82] German + + + + + + + + + +
(Switzerland)
Oervik et al. (2017)[83] Danish + + - + + + + + + -
U
German + + - + + + + + + -
AN
CFABMS Motaharinezhad et al. (2015)[85] Persian ? ? ? ? ? ? ? ? ? ?
CFQ Chilcot et al. (2016)[86] English - + - + + + - + - +
M
Pust et al. (2019)[72] German + - + + + + + - + +
(Germany)
CFS Jason et al. (1997)[87] English - - - + + - - - + -
D
SQ
CIS20R Rietberg et al. (2010)[59] Dutch - + - + - + - - + +
FAI
FAI/FSI
Schwartz et al. (1993)[90]
Hernandez-Ronquillo et al. (2011) [58]
English
English
TE
+
-
+
-
-
+
+
? ?
+
?
-
?
-
?
-
?
-
?
-
Iriarte et al. (1998)[147] Spanish + + - + + + - + - -
EP
FDS
FSIQ- Hudgens et al. (2019)[92] English + + + + - + + - + +
RMS
MAFS Behrangrad et al. (2017)[93] Persian + + - + + + - + + +
C
MS-FSE Thomas et al. (2014)[94] English + - - + + + - + + -
AC
PFS Carlozzi et al. (2019)[148] English + + + + + + + + - +
PROMIS- Cook et al. (2012)[96] English - - - + + + - + + -
Fatigue
MS
PSF Marrie et al. (2005)[97] English - - - + + - - + - -
SOFI Johansson et al. (2008)[98] Svedish + + - + + + - + + -
Vas Kos et al. (2006)[99] Dutch - + - + + - - + - -
Information Classification: General
WEIMuS Flachenecker et al. (2006)[100] German + - + + + ? + + + +
Flachenecker et al. (2008)[149] German ? ? ? ? ? ? ? ? ? ?
Item 1= Internal validity; Item 2= Reliability; Item 3=Measurement error; Item 4= Content validity; Item 5= Structural validity; Item 6= Hypotheses testing; Item 7= Cross-cultural validity; Item 8= Criterion validity; Item
9= Responsiveness; Item 10= Interpretability.+= sufficient; -=insufficient; ?= indeterminate; CFAB-MS= Comprehensive Fatigue Assessment Battery for MS; CFQ= Chronic Fatigue Questionnaire; FSMC= Fatigue Scale
for Motor and Cognitive Functions; MFIS= Modified Fatigue Impact Scale; CFS screening questionnaire= Chronic Fatigue Syndrome screening questionnaire; CIS= Checklist Individual Strength; D-FIS= Daily Fatigue
Impact Scale; eVAS= Electronic Visual Analogue Scale; FAI= Fatigue Assessment Instrument; FAMS= Functional Assessment of Multiple Sclerosis; FDS= Fatigue Descriptive Scale; FIS= Fatigue Impact Scale; FSS=
Fatigue Severity Scale; FSI= Fatigue Symptom Inventory; FSIQ-RMS= Fatigue Symptoms and Impacts Ques;tionnaire - Relapsing Multiple Sclerosis; FSMC= Fatigue Scale for Motor and Cognitive Functions; FSS-7=
Fatigue Severity Scale-7; LMSQoL= Leeds Multiple Sclerosis Quality of Life; MAFS= Multidimensional Assessment of Fatigue Scale; MFIS-5= Modified Fatigue Impact Scale-5; MS-FSE= Multiple Sclerosis-Fatigue
T
Self– Efficacy; MSQoL-54= Multiple Sclerosis Quality of Life-54; MSQoL-29= Multiple Sclerosis Quality of Life-29; eMSQoL-29= Electronic Format Multiple Sclerosis Quality of Life-29; MSSID= MS Symptom and
IP
Impact Diary; MSSymS= MS Symptom Score; MusiQoL= Multiple Sclerosis International Quality of Life questionnaire; MCAT= Multidimensional Computerized Adaptive Test; Neuro-QoL= Neurology Quality of Life;
Neuro-QoL SF= Neurology Quality of Life Short Forms; NFI-MS= Neurological Fatigue Index MS; PERSEPP= “PERception de la Scle'rose En Plaques et de ses Pousse'es; PFS= Physical Functioning Scale; PROMIS-
Fatigue MS= Patient Reported Outcomes Measurement Information System-Fatigue MS; PS= Performance Scales; PSF= Performance Scales Fatigue; PSS= Perceived Stress Scale; SMSS= SymptoMScreen questionnaire ;
R
SOFI= Swedish Occupational Fatigue In×entory; U-FIS= Unidimensional-Fatigue Impact Scale; VAS= Visual Analogue Scale; WEIMuS= Würzburg Fatigue Inventory in MS.
SC
U
AN
M
D
TE
EP
C
AC
Information Classification: General
Table 5 Quality assessment of included studies evaluating instruments including a fatigue domain in the questionnaire
Scales Authors (year of publication) Language Item
1 2 3 4 5 6 7 8 9 10
BPRO-MS Chua et al. (2015)[102] English + - - + + - - + - +
CRoMS Matza et al. (2019) English + - - + + - - + - +
eVas Kos et al. (2017) Dutch - + + + + - - + - -
T
FAMS Cella et al. (1996)[104] English + + - + + + - + - -
IP
Chang et al. (2002)[105] Spanish + - - + + - - + - +
Mendes et al. (2004)[107] Portuguese + - - + + - - + - +
R
Patti et al. (2007)[108] Italian + - - + + - - + - +
SC
Sørensen et al. (2011)[109] Danish + - - + + - - + - +
LMSQOL Ensari et al. (2015)[110] English + ? ? + + + - + - +
Akbiyik et al. (2009)[112] Turkish + + - + - + - - - -
U
Ford et al. (2001)[111] English + - - + + - - + - +
AN
MSSID Greenhalgh et al. (2003)[150] English + + - + + + - - + -
MSQOL-54 Vickrey et al. (1995)[114] English + + - + + + + - - -
M
Solari et al. (1999)[115] Italian + - - + + + + - - -
Miller et al. (2005)[116] Hebrew + - - + + - - + - +
D
Idiman et al. (2005)[118] Turkish - - - - - + + + - -
Heiskanen et al. (2006) [119] Finnish
TE + + - - + - + + - -
Ghaem et al. (2007)[151] Persian + - - + + - - + - +
Pekmezovic et al. (2007)[120] Serbian + + - - - + + + - -
EP
Füvesi et al. (2008)[121] Hungarian + + - - + - + + - -
Taoussi et al. (2012)[122] Arabic + - - + - + + - - -
C
Catic et al. (2017)[123] Bosnian + + - - - + - + - -
Estiasari et al. (2019)[124] Indonesian + + - + + - + + - -
AC
Stern et al. (2017)[127] Slovenian + + - + + - + + - -
MSQOL-54 Rosato et al. (2016)[129] Italian - + - + - + - + - -
SF
eMSQOL- Rosato et al. (2019)[125] Italian + + + + + + - + + -
29 SF
Baker et al. (2018)[126] English + + - - + + - + - -
MSSympto Zhang et al. (2020)[130] English - + - + + - - + + -
mScores
Information Classification: General
MusiQol Simeoni et al. (2008)[131] Spanish (Argentina) + + - + + + - + + -
French, German
Greek
Hebrew
Italian
Norwegian
Russian
Spanish
Turkish
T
English (UK)
English (USA)
IP
Arabic
Triantafyllon et al. (2009)[132] Greek + + - + + + - + - -
R
Fernández et al. (2011)[134] Spanish + + - + + + - + + +
SC
Baumstarck-Barrau et al. (2011)[133] French - - - + + ? ? + + -
Thumboo et al. (2011)[136] English (Singapore, + - - + + + + + - -
Malaysia, India)
Jamroz-Wiœniewska et al. (2011)[135] Polish + + - - - + + + - -
U
Beiske et al. (2012)[137] Norwegian + + - + + + - + - -
AN
Huah et al. (2014)[138] Korean + - - + + - - + - +
Farran et al. (2020)[75] Arabic + + - + + - - - - -
M
MusiQoL- Michel et al. (2016)[28] English - + + + + + - + - +
MCAT
Neuro-QoL Gershon et al. (2011)[32] English + - + + + + + + + +
Spanish
D
Correia et al. (2014)[29] Spanish ? ? ? + ? ? + + ? ?
Neuro-QoL
SF
Miller et al. (2016)[30]
Medina et al. (2019)[31]
TE
English
English
+
+
+
+
-
-
+
+
+
-
+
+
-
-
+
+
+
+
+
-
Ghajarzadeh et al. (2016)[33] Persian + + - + + - - - - -
EP
PERSEPP
Baroin et al. (2013)[34] French + + + + + + - + - -
PS Schwartz et al. (1999)[37] English + + - + + + - - - +
C
Marrie et al. (2007)[35] English - - - + + + - + - -
AC
PSS Chamot et al. (2014) English - - + + + + + + + +
Symptom Schwartz et al. (1999)[37] English + + - + + + - - - +
inventory
Symptom Schwartz et al. (2012)[39] English + - - + + - - + + +
inventory
disability- Schwartz et al. (2012)[40] English + - - + + - - - - -
specific
short forms
Information Classification: General
SymptoMSc Green et al. (2016)[41] English - + + + + + - + - -
reen
Fitzgerald et al. (2019)[42] English + + + + + + + + + +
Item 1= Internal validity; Item 2= Reliability; Item 3=Measurement error; Item 4= Content validity; Item 5= Structural validity; Item 6= Hypotheses testing; Item 7= Cross-cultural validity; Item 8= Criterion validity; Item
9= Responsiveness; Item 10= Interpretability.+= sufficient; -=insufficient; ?= indeterminate; CFAB-MS= Comprehensive Fatigue Assessment Battery for MS; CFQ= Chronic Fatigue Questionnaire; FSMC= Fatigue Scale
for Motor and Cognitive Functions; MFIS= Modified Fatigue Impact Scale; CFS screening questionnaire= Chronic Fatigue Syndrome screening questionnaire; CIS= Checklist Individual Strength; D-FIS= Daily Fatigue
Impact Scale; eVAS= Electronic Visual Analogue Scale; FAI= Fatigue Assessment Instrument; FAMS= Functional Assessment of Multiple Sclerosis; FDS= Fatigue Descriptive Scale; FIS= Fatigue Impact Scale; FSS=
Fatigue Severity Scale; FSI= Fatigue Symptom Inventory; FSIQ-RMS= Fatigue Symptoms and Impacts Ques;tionnaire - Relapsing Multiple Sclerosis; FSMC= Fatigue Scale for Motor and Cognitive Functions; FSS-7=
Fatigue Severity Scale-7; LMSQoL= Leeds Multiple Sclerosis Quality of Life; MAFS= Multidimensional Assessment of Fatigue Scale; MFIS-5= Modified Fatigue Impact Scale-5; MS-FSE= Multiple Sclerosis-Fatigue
T
Self– Efficacy; MSQoL-54= Multiple Sclerosis Quality of Life-54; MSQoL-29= Multiple Sclerosis Quality of Life-29; eMSQoL-29= Electronic Format Multiple Sclerosis Quality of Life-29; MSSID= MS Symptom and
IP
Impact Diary; MSSymS= MS Symptom Score; MusiQoL= Multiple Sclerosis International Quality of Life questionnaire; MCAT= Multidimensional Computerized Adaptive Test; Neuro-QoL= Neurology Quality of Life;
Neuro-QoL SF= Neurology Quality of Life Short Forms; NFI-MS= Neurological Fatigue Index MS; PERSEPP= “PERception de la Scle'rose En Plaques et de ses Pousse'es; PFS= Physical Functioning Scale; PROMIS-
Fatigue MS= Patient Reported Outcomes Measurement Information System-Fatigue MS; PS= Performance Scales; PSF= Performance Scales Fatigue; PSS= Perceived Stress Scale; SMSS= SymptoMScreen questionnaire ;
R
SOFI= Swedish Occupational Fatigue In×entory; U-FIS= Unidimensional-Fatigue Impact Scale; VAS= Visual Analogue Scale; WEIMuS= Würzburg Fatigue Inventory in MS.
SC
U
AN
M
D
TE
EP
C
AC
Information Classification: General
T
IP
R
SC
U
AN
M
D
TE
EP
C
AC
Figure 1 - Flowchart of search and screening process.
Information Classification: General
1Section/topic # Checklist item
TITLE
Title 1 Identify the report as a systematic review, meta-analysis, or both.
T
ABSTRACT
IP
Structured summary 2 Provide a structured summary including, as applicable: background; objectives; data
participants, and interventions; study appraisal and synthesis methods; results; limita
implications of key findings; systematic review registration number.
R
INTRODUCTION
SC
Rationale 3 Describe the rationale for the review in the context of what is already known.
Objectives 4 Provide an explicit statement of questions being addressed with reference to particip
outcomes, and study design (PICOS).
METHODS
Protocol and registration 5 U
Indicate if a review protocol exists, if and where it can be accessed (e.g., Web addre
AN
registration information including registration number.
Eligibility criteria 6 Specify study characteristics (e.g., PICOS, length of follow-up) and report characteris
language, publication status) used as criteria for eligibility, giving rationale.
M
Information sources 7 Describe all information sources (e.g., databases with dates of coverage, contact wit
additional studies) in the search and date last searched.
Search 8 Present full electronic search strategy for at least one database, including any limits
D
repeated.
TE
Study selection 9 State the process for selecting studies (i.e., screening, eligibility, included in systema
included in the meta-analysis).
Data collection process 10 Describe method of data extraction from reports (e.g., piloted forms, independently, i
for obtaining and confirming data from investigators.
EP
Data items 11 List and define all variables for which data were sought (e.g., PICOS, funding source
simplifications made.
Risk of bias in individual 12 Describe methods used for assessing risk of bias of individual studies (including spe
C
studies done at the study or outcome level), and how this information is to be used in any da
Summary measures 13 State the principal summary measures (e.g., risk ratio, difference in means).
AC
Synthesis of results 14 Describe the methods of handling data and combining results of studies, if done, incl
(e.g., I2) for each meta-analysis.
Page 1 of 2
Section/topic # Checklist item
Risk of bias across studies 15 Specify any assessment of risk of bias that may affect the cumulative evidence (e.g.
reporting within studies).
Additional analyses 16 Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, met
which were pre-specified.
RESULTS
Information Classification: General
Study selection 17 Give numbers of studies screened, assessed for eligibility, and included in the review
each stage, ideally with a flow diagram.
Study characteristics 18 For each study, present characteristics for which data were extracted (e.g., study siz
provide the citations.
Risk of bias within studies 19 Present data on risk of bias of each study and, if available, any outcome level assess
Results of individual studies 20 For all outcomes considered (benefits or harms), present, for each study: (a) simple
intervention group (b) effect estimates and confidence intervals, ideally with a forest
Synthesis of results 21 Present results of each meta-analysis done, including confidence intervals and meas
Risk of bias across studies 22 Present results of any assessment of risk of bias across studies (see Item 15).
T
Additional analysis 23 Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, m
IP
DISCUSSION
Summary of evidence 24 Summarize the main findings including the strength of evidence for each main outco
R
key groups (e.g., healthcare providers, users, and policy makers).
Limitations 25 Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level
SC
identified research, reporting bias).
Conclusions 26 Provide a general interpretation of the results in the context of other evidence, and im
FUNDING
Funding 27
U
Describe sources of funding for the systematic review and other support (e.g., supply
systematic review.
AN
Appendix 1 - OUTCOME MEASURES FOR PHYSICAL FATIGUE IN INDIVIDUALS WITH MULTIPLE SCLEROSIS: A SYSTEMATIC
REVIEW
M
D
TE
EP
C
AC
Information Classification: General
You might also like
- Successful vs. Effective Real Managers by Fred LuthansDocument7 pagesSuccessful vs. Effective Real Managers by Fred LuthansDeepika GulatiNo ratings yet
- Psychometric ReportDocument53 pagesPsychometric ReportSyeda Fatima Hasnain100% (2)
- Chapter 9 - Assessment of IntelligenceDocument13 pagesChapter 9 - Assessment of Intelligencemarjorie bantilanNo ratings yet
- Time Management and Personal Effectiveness at WorkDocument188 pagesTime Management and Personal Effectiveness at Workeng.abed100% (1)
- Test Grafomotor de Pascual para NiñosDocument14 pagesTest Grafomotor de Pascual para NiñosLeonardo HerreraNo ratings yet
- 2019 Article 196Document8 pages2019 Article 196Karylle Ezra GulifardoNo ratings yet
- 2019 - Branco - Aging With Multiple Sclerosis - Prevalence and Profile of Cognitive ImpairmentDocument7 pages2019 - Branco - Aging With Multiple Sclerosis - Prevalence and Profile of Cognitive ImpairmentjesicaNo ratings yet
- Jurnal Demensia 5Document9 pagesJurnal Demensia 5Mutiara Anak NegeriNo ratings yet
- Journal Neurologi 2Document10 pagesJournal Neurologi 2fatya azaraNo ratings yet
- Curcioetal InpressDocument10 pagesCurcioetal InpressWesy GustinaNo ratings yet
- 10Document7 pages10akmal shahzadNo ratings yet
- Impact of Physical Activity On Disability Risk inDocument7 pagesImpact of Physical Activity On Disability Risk inLyrian LohNo ratings yet
- 32676052: Neurological and Musculoskeletal Features of COVID-19 A Systematic Review and Meta-Analysis PDFDocument14 pages32676052: Neurological and Musculoskeletal Features of COVID-19 A Systematic Review and Meta-Analysis PDFLeonardo MedinaNo ratings yet
- 490-Article Text-1324-1-10-20180508Document9 pages490-Article Text-1324-1-10-20180508FahmiNo ratings yet
- Effectiveness of Rehabilitation Interventions in Adults With Multi-Organ Dysfunction Syndrome: A Rapid ReviewDocument8 pagesEffectiveness of Rehabilitation Interventions in Adults With Multi-Organ Dysfunction Syndrome: A Rapid Reviewsari murnaniNo ratings yet
- Escalas de Disfuncion OrganicaDocument8 pagesEscalas de Disfuncion OrganicavalfreNo ratings yet
- Adults With Idiopathic Scoliosis Improve Disability After Motor and Cognitive Rehabilitation: Results of A Randomised Controlled TrialDocument10 pagesAdults With Idiopathic Scoliosis Improve Disability After Motor and Cognitive Rehabilitation: Results of A Randomised Controlled TrialCarolina Drummond Rocha MoraisNo ratings yet
- Jurnal InternasionalDocument7 pagesJurnal Internasional34. Putu Mariska Abdi CahyaniNo ratings yet
- The Assessment of FatigueDocument14 pagesThe Assessment of FatigueMarianinha AlonsoNo ratings yet
- Understanding The Relationship Between Cognitive Performance and Function in Daily Life After Traumatic Brain InjuryDocument11 pagesUnderstanding The Relationship Between Cognitive Performance and Function in Daily Life After Traumatic Brain InjuryKatia DjerroudNo ratings yet
- SalivaDocument21 pagesSalivaGegiu GabrielaNo ratings yet
- Quality of Life in Glaucoma: A Review of The LiteratureDocument23 pagesQuality of Life in Glaucoma: A Review of The LiteratureMakhda Nurfatmala LNo ratings yet
- Bio Marcadores en Sarcopenia Calvani2017Document6 pagesBio Marcadores en Sarcopenia Calvani2017JAVIER VELASQUEZ100% (1)
- Neglect Syndrome in Post-Stroke Conditions: Assessment and Treatment (Scoping Review)Document13 pagesNeglect Syndrome in Post-Stroke Conditions: Assessment and Treatment (Scoping Review)Gabriella ALeNo ratings yet
- EFNS Guideline 2010 Diagnosis and Management of ADDocument13 pagesEFNS Guideline 2010 Diagnosis and Management of ADDeni Andre AtmadinataNo ratings yet
- Journal of Ayurveda and Integrative MedicineDocument4 pagesJournal of Ayurveda and Integrative MedicineMiftakhul ViviNo ratings yet
- SIMFER Rehabilitation Treatment Guidelines in Postmenopausal and Senile OsteoporosisDocument23 pagesSIMFER Rehabilitation Treatment Guidelines in Postmenopausal and Senile OsteoporosisOanaBFTNo ratings yet
- Accepted Manuscript: Journal of Bodywork & Movement TherapiesDocument53 pagesAccepted Manuscript: Journal of Bodywork & Movement TherapiesEduardo Santana SuárezNo ratings yet
- 2016 - Cumming T.B. Et Al - Prevalence of Fatigue After StrokeDocument10 pages2016 - Cumming T.B. Et Al - Prevalence of Fatigue After Strokerichard LemieuxNo ratings yet
- ECT Side EffectDocument7 pagesECT Side EffectsherinjeanicatresyaNo ratings yet
- Artical No 1 PDFDocument15 pagesArtical No 1 PDFShankranand TiwariNo ratings yet
- The Effects of Magnesium Melatonin Vit B Complex Supplementation in Treatment of InsomniaDocument5 pagesThe Effects of Magnesium Melatonin Vit B Complex Supplementation in Treatment of InsomniaDiego NevesNo ratings yet
- Fpsyt 11 608896Document20 pagesFpsyt 11 608896shumailaNo ratings yet
- Machine Learning Solutions Applied To Amyotrophic Lateral Sclerosis Prognosis: A ReviewDocument12 pagesMachine Learning Solutions Applied To Amyotrophic Lateral Sclerosis Prognosis: A ReviewJoel ArraisNo ratings yet
- Jurnal Neuropaty dm2Document2 pagesJurnal Neuropaty dm2ferryNo ratings yet
- Symptomatic Therapy and Neurorehabilitation in Multiple SclerosisDocument10 pagesSymptomatic Therapy and Neurorehabilitation in Multiple Sclerosissarawu9911No ratings yet
- Novel Technological Solutions ForDocument23 pagesNovel Technological Solutions ForANTONIO REYES MEDINANo ratings yet
- 10 1002@msc 1498Document13 pages10 1002@msc 1498Ricardo PietrobonNo ratings yet
- Franke 2016Document40 pagesFranke 2016M MisbahunnurNo ratings yet
- Measurement Tools of StrokeDocument42 pagesMeasurement Tools of StrokeDharam PandeyNo ratings yet
- Rodakowski 2015 Non Pharmacological InterventiDocument16 pagesRodakowski 2015 Non Pharmacological InterventiSu AjaNo ratings yet
- Jurnal Pendukung 1 - A Systematic Review and Meta-Analysis of Exercise Interventions in Schizophrenia PatientsDocument19 pagesJurnal Pendukung 1 - A Systematic Review and Meta-Analysis of Exercise Interventions in Schizophrenia PatientsM SNo ratings yet
- 1 s2.0 S1532046419300577 MainDocument22 pages1 s2.0 S1532046419300577 MainAmith PrasanthNo ratings yet
- VejezDocument7 pagesVejezPamelaNo ratings yet
- Variation in Guideline Implementation and Adherence Regarding Severe Traumatic Brain Injury Treatment: A CENTER-TBI Survey Study in EuropeDocument6 pagesVariation in Guideline Implementation and Adherence Regarding Severe Traumatic Brain Injury Treatment: A CENTER-TBI Survey Study in EuropefinaNo ratings yet
- The Swedish Occupational Fatigue Inventory in People With Multiple SclerosisDocument7 pagesThe Swedish Occupational Fatigue Inventory in People With Multiple SclerosisikrambahariNo ratings yet
- Verano TraidorDocument8 pagesVerano TraidorMaria AgredaNo ratings yet
- Basics of NeuropsychologyDocument7 pagesBasics of NeuropsychologyJasroop MahalNo ratings yet
- Healthcare 09 00513 v2Document10 pagesHealthcare 09 00513 v2Clorox BleachNo ratings yet
- Ev Estado de ConcienciaDocument18 pagesEv Estado de ConcienciaFabiolaNo ratings yet
- Fpsyg 13 859478Document18 pagesFpsyg 13 859478Hannah PengNo ratings yet
- EBM Final AssignmentDocument3 pagesEBM Final Assignmentleehi.pridanNo ratings yet
- Instrumental Assessment of Balance Functional Performance A Numerical Score To Discriminate Defective Subjects A Retrospective StudyDocument12 pagesInstrumental Assessment of Balance Functional Performance A Numerical Score To Discriminate Defective Subjects A Retrospective Studyrusu andreeaNo ratings yet
- Alzheimers Disease Diagnosis Using Misfolding ProDocument18 pagesAlzheimers Disease Diagnosis Using Misfolding ProRoberta Lessa RibeiroNo ratings yet
- Optimizing The Combination of Oxytocin M 7872188dDocument6 pagesOptimizing The Combination of Oxytocin M 7872188dAnggi WidyaNo ratings yet
- Icf Core Sets For StrokeDocument7 pagesIcf Core Sets For StrokeMuhammadMusa47No ratings yet
- Pone 0204774Document52 pagesPone 0204774Karina OktaviyadiNo ratings yet
- Career Satisfaction and Burnout Among U.S. Neurosurgeons: A Feasibility and Pilot StudyDocument10 pagesCareer Satisfaction and Burnout Among U.S. Neurosurgeons: A Feasibility and Pilot Studyakmal shahzadNo ratings yet
- Vilarino2021 Article Effects of Resistance Training On TDocument10 pagesVilarino2021 Article Effects of Resistance Training On TJoaquim Lorenzetti BrancoNo ratings yet
- Ethical Questions in The Treatment of Subjects With Dementia-1Document16 pagesEthical Questions in The Treatment of Subjects With Dementia-1mathexa.infoNo ratings yet
- Summary of An Evidence-Based Guideline On Soft Tissue Shoulder Injuries and Related Disorders - Part 1: AssessmentDocument6 pagesSummary of An Evidence-Based Guideline On Soft Tissue Shoulder Injuries and Related Disorders - Part 1: AssessmentrdkelsallNo ratings yet
- Distinctiveness of Psychological Obstacles To Recovery in Low Back Pain Patients in Primary CareDocument9 pagesDistinctiveness of Psychological Obstacles To Recovery in Low Back Pain Patients in Primary CareMauro GarciaNo ratings yet
- Santangelo2014 Article ApathyInUntreatedDeNovoPatientDocument10 pagesSantangelo2014 Article ApathyInUntreatedDeNovoPatientketevanNo ratings yet
- Core Outomes Set ESJ2015Document16 pagesCore Outomes Set ESJ2015Ju ChangNo ratings yet
- Early Childhood AssessmentDocument501 pagesEarly Childhood Assessmentshahzad jalbani100% (1)
- Guidelines For Developing, Translating, and Validating A Questionnaire in Perioperative and Pain MedicineDocument14 pagesGuidelines For Developing, Translating, and Validating A Questionnaire in Perioperative and Pain MedicineCatharinaWidiartiniNo ratings yet
- Enhancing The Quality of Life of People With Intellectual Disabilities - From Theory To PracticeDocument455 pagesEnhancing The Quality of Life of People With Intellectual Disabilities - From Theory To PracticeletstopfightingNo ratings yet
- Deviant Behavior Variety Scale: Development and Validation With A Sample of Portuguese AdolescentsDocument9 pagesDeviant Behavior Variety Scale: Development and Validation With A Sample of Portuguese AdolescentsSajjadNo ratings yet
- Nichols 1994Document30 pagesNichols 1994Paul NicholsNo ratings yet
- Educational Measurement - 2012 - Williamson - A Framework For Evaluation and Use of Automated ScoringDocument12 pagesEducational Measurement - 2012 - Williamson - A Framework For Evaluation and Use of Automated ScoringNapat JitpaisarnwattanaNo ratings yet
- Health Economics&PharmacoeconomicsDocument89 pagesHealth Economics&PharmacoeconomicsRasvini RajendranNo ratings yet
- Bias in Terms of Culture and A Method For ReducingDocument21 pagesBias in Terms of Culture and A Method For ReducingMaryam KhanzaiNo ratings yet
- 647403a38907a86af5731e54 WPPSI-3Document2 pages647403a38907a86af5731e54 WPPSI-3s.casison.allykkaNo ratings yet
- State Trait Anxiety ManualDocument7 pagesState Trait Anxiety ManualAnanya SharmaNo ratings yet
- Brief History of Psychological TestingDocument2 pagesBrief History of Psychological TestingZenNo ratings yet
- Issues in Test Construction and Assessment Ethical Principles of Psychological Testing 1. Their Knowledge and Skills inDocument17 pagesIssues in Test Construction and Assessment Ethical Principles of Psychological Testing 1. Their Knowledge and Skills inOinokwesiga PinkleenNo ratings yet
- Mcalog 2017Document12 pagesMcalog 2017Κωνσταντίνος ΓκάργκαςNo ratings yet
- Reliability and Validity of Instruments Measuring Job Satisfaction-A Systematic ReviewDocument10 pagesReliability and Validity of Instruments Measuring Job Satisfaction-A Systematic ReviewFira Charming VerinaNo ratings yet
- MCQ in Advanced Engineering Math Part 1 Answers PDFDocument5 pagesMCQ in Advanced Engineering Math Part 1 Answers PDFxXx uuNo ratings yet
- Classical Test Theory Vs Item Response TheoryDocument42 pagesClassical Test Theory Vs Item Response TheoryFirmanNo ratings yet
- Lucy Barnard-Brack - Revising Social Communication Questionnaire Scoring Procedures For Autism Spectrum Disorder and Potential Social Communication DisorderDocument1 pageLucy Barnard-Brack - Revising Social Communication Questionnaire Scoring Procedures For Autism Spectrum Disorder and Potential Social Communication DisorderAUCDNo ratings yet
- PSYCHOMETRIC PROPERTIES of CRIDocument5 pagesPSYCHOMETRIC PROPERTIES of CRIEman Siddiqi100% (1)
- Adaptation of The Mental Health Inventory MHI-38 For Adolescents - Indonesian VersionDocument12 pagesAdaptation of The Mental Health Inventory MHI-38 For Adolescents - Indonesian VersionREFIDA MUTIANo ratings yet
- Core Principles of Assessment in Competency Based Medical EducationDocument9 pagesCore Principles of Assessment in Competency Based Medical EducationJasmik SinghNo ratings yet
- Quiz in Reliability 1Document6 pagesQuiz in Reliability 1BELARMINO LOUIE A.No ratings yet
- Psychometric Review of Language Test For Preschool ChildrenDocument29 pagesPsychometric Review of Language Test For Preschool ChildrenemmpeethreeNo ratings yet
- RISBDocument78 pagesRISBRoxi Resurreccion57% (14)
- N % Cases Valid 20 100.0 Excluded 0 .0 Total 20 100.0 A. Listwise Deletion Based On All Variables in The ProcedureDocument8 pagesN % Cases Valid 20 100.0 Excluded 0 .0 Total 20 100.0 A. Listwise Deletion Based On All Variables in The Procedurenzi_eX6943No ratings yet
- CEP - 4 of 5 Practicum Survey January-June 2024Document3 pagesCEP - 4 of 5 Practicum Survey January-June 2024peacefulsitholeNo ratings yet