Professional Documents
Culture Documents
2005 Benzodiazepine Abuse Dependence
Uploaded by
Pinelopi KolliaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2005 Benzodiazepine Abuse Dependence
Uploaded by
Pinelopi KolliaCopyright:
Available Formats
Charles P.
O’Brien
Benzodiazepine Use, Abuse, and Dependence
Charles P. O’Brien, M.D., Ph.D.
Although benzodiazepines are invaluable in the treatment of anxiety disorders, they have some
potential for abuse and may cause dependence or addiction. It is important to distinguish between ad-
diction to and normal physical dependence on benzodiazepines. Intentional abusers of benzodiaze-
pines usually have other substance abuse problems. Benzodiazepines are usually a secondary drug of
abuse—used mainly to augment the high received from another drug or to offset the adverse effects of
other drugs. Few cases of addiction arise from legitimate use of benzodiazepines. Pharmacologic de-
pendence, a predictable and natural adaptation of a body system long accustomed to the presence of a
drug, may occur in patients taking therapeutic doses of benzodiazepines. However, this dependence,
which generally manifests itself in withdrawal symptoms upon the abrupt discontinuation of the medi-
cation, may be controlled and ended through dose tapering, medication switching, and/or medication
augmentation. Due to the chronic nature of anxiety, long-term low-dose benzodiazepine treatment
may be necessary for some patients; this continuation of treatment should not be considered abuse or
addiction. (J Clin Psychiatry 2005;66[suppl 2]:28–33)
B enzodiazepines serve an important purpose in alle-
viating the stress and anxiety of patients suffering
from anxiety disorders. Although physicians often prefer
of other substances such as cocaine and alcohol. Individ-
uals who unintentionally abuse benzodiazepines use pre-
scribed benzodiazepines inappropriately by taking them
to prescribe benzodiazepines over other drugs because in higher doses than their prescribing doctor intended
of their low toxicity, concerns about the dependence- or for a longer duration than needed after remission of
producing or addictive nature of these drugs have been ex- the anxiety disorder. Unintentional abusers may resort to
pressed for decades. Benzodiazepines may, indeed, cause other sources of benzodiazepines if their doctors stop pre-
dependence or even be abused; however, the abuse poten- scribing them, but their initial benzodiazepine use most
tial of benzodiazepines is quite low and should be weighed often starts legitimately to treat a diagnosed anxiety dis-
against their beneficial anxiolytic properties. order.
People who abuse benzodiazepines may become de-
BENZODIAZEPINE ABUSE pendent on them, although abuse and dependency are not
always mutually inclusive. An abuser of benzodiazepines
The abuse of benzodiazepines can be divided into 2 is not necessarily dependent (for example, when an indi-
abuse patterns: deliberate abuse by people who use drugs vidual irregularly takes benzodiazepines at parties to get
for their euphoriant effects and unintentional abuse by high), and a patient who is physiologically dependent on
patients who begin using benzodiazepines to treat an anxi- benzodiazepines is not necessarily abusing them. There
ety disorder and end up using them inappropriately. Delib- are 2 types of dependence that may develop: physical
erate abusers usually take benzodiazepines in an attempt or pharmacologic dependence and addiction (called “de-
to get high and often abuse other substances for the same pendence” in the Diagnostic and Statistical Manual of
purpose. Within this same constituency, benzodiazepines Mental Disorders, Fourth Edition, Text Revision [DSM-
may also be used to self-medicate the withdrawal effects IV-TR]1). It is vital that physicians differentiate between
these two types.
PHARMACOLOGIC DEPENDENCE VS. ADDICTION
From the Department of Psychiatry, University of
Pennsylvania and Philadelphia VA Medical Center.
This article is derived from the roundtable discussion
Although an individual who is addicted to benzodiaze-
“Utilizing Benzodiazepines in Clinical Practice: An Evidence- pines is usually physiologically dependent on the medi-
Based Discussion,” which was held August 16, 2004, in Boston, cation, a patient may have a physical dependence without
Mass., and supported by an unrestricted educational grant
from Pfizer Inc. being addicted. Addiction requires evidence of compul-
Corresponding author and reprints: Charles P. O’Brien, sive drug-seeking behavior and loss of control as detailed
M.D., Ph.D., Department of Psychiatry, University of
Pennsylvania, 3900 Chestnut Street/6178, Philadelphia, PA in the DSM-IV. Among legitimate users of benzodiaze-
19104 (e-mail: obrien@mail.trc.upenn.edu). pines, physical dependence can result from long-term
28 J Clin Psychiatry 2005;66 (suppl 2)
Benzodiazepine Use, Abuse, and Dependence
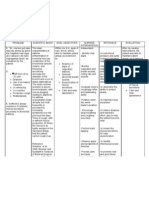
regular use according to a physician’s instructions, but this Table 1. Half-Life and Speed of Onset for Common
does not constitute addiction. Benzodiazepinesa
Pharmacologic dependence is a natural physiologic ad- Benzodiazepine Half-Life (range, h) Speed of Onset
aptation in response to the continual use of many types Alprazolam 12–15 Intermediate
of drugs that affect the nervous system. This adaptation Chlordiazepoxide 10–30 Intermediate
Clonazepam 18–50 Slow
is the biological basis for pharmacologic tolerance and Diazepam 20–80 Fast
withdrawal symptoms or rebound phenomenon upon dis- Lorazepam 10–20 Intermediate
continuation of drug use. Haefely2 describes this drug- Oxazepam 5–10 Slow
Prazepam 50–200 Slow
induced adaptive syndrome as an inevitable result of the a
Data on all drugs except clonazepam from Bailey et al.4 ; data on
repeated interaction between an organism and almost all clonazepam from Estivill et al.5
classes of drugs.
On the other hand, addiction implies compulsive use
and drug-seeking behavior in the pursuit of getting high. Variables Affecting the Abuser’s Choice
Called substance dependence by the DSM-IV,1 addiction of Benzodiazepine
generally includes the following: tolerance to the drug Drug effect. Obviously, most drugs used recreation-
and the need for increasing amounts to achieve intoxica- ally are chosen because of their euphoriant effects and
tion or the desired effect; withdrawal symptoms upon their lack of dysphoriant effects. Among benzodiaze-
discontinuation and, often, self-administration of the sub- pines, each drug’s effects and, therefore, its appeal to
stance to relieve the withdrawal symptoms; drug-seeking abusers depend largely on the drug’s half-life, speed of
and/or drug-using behaviors that require a considerable onset, and speed of offset and on the age of the individual
amount of time or effort (e.g., going to multiple doctors taking the medication.
for prescriptions, buying substances on the street, buying Benzodiazepines vary widely in their elimination half-
illegal prescriptions, forging prescriptions); negligence of life, which is the amount of time required for half of the
important familial or occupational obligations or discon- drug taken into the body to be removed from the blood.
tinuation of previously important recreational, social, or Speed of onset of the effect is a major factor in the degree
occupational activities; and continued use despite negative of euphoria, with faster onset indicating more immediate
consequences. Although physiologic dependence (mani- and desirable euphoriant effects. Clinical experience in-
fested by tolerance and withdrawal) is typical of addiction, dicates that benzodiazepines with a slower onset tend to
physiologic dependence is not a required criterion for be abused less often, but this has not been proven with
addiction. experimental data. In some cases, the ingested drug is
really a pro-drug requiring metabolism to an active me-
DELIBERATE ABUSE OF BENZODIAZEPINES tabolite for effects to occur. Thus, drug effects are de-
layed, and the benzodiazepine is not likely to be abused.
Deliberate abuse of benzodiazepines often begins as A rapid offset, occurring in drugs with a short half-life,
deliberate prescription misuse and is usually a recreational may increase abuse potential because the user tends to
and thrill-seeking behavior. In addition to benzodiaze- repeat the dosing frequently to maintain the effect. With-
pines obtained from legitimate prescriptions, abusers ac- drawal seizures are more likely to be caused by a short
quire these drugs from various other sources. They may half-life drug such as alprazolam, which is also very po-
buy illegal prescriptions or forge prescriptions themselves. tent. Although diazepam has a long half-life because of
Benzodiazepines are also bought on the street from dealers active metabolites, it has a rapid onset; consequently, it
who obtain them through illicit channels. Although benzo- may be abused because of its immediate effects, but with-
diazepines bought on the street are possibly used appropri- drawal may be delayed and milder due to the long dura-
ately by patients who are unable or unwilling to see a doc- tion of the active metabolites. The half-lives and speed
tor for anxiety disorders, this method of drug procurement of onset of some of the most common benzodiazepines
is suspicious and usually linked to a pattern of abuse.3 are listed in Table 1.4,5 The age of the individual greatly
Abusers most often use benzodiazepines to get high.3 affects the half-life of the medication6; in older patients,
Sometimes these drugs are used in conjunction with other benzodiazepines tend to have much longer half-lives and,
substances to improve the euphoriant effects, especially therefore, a tendency to accumulate with daily dosing.
to augment methadone. Heroin addicts taking methadone This can produce dementia and may be mistaken for
may take diazepam or another benzodiazepine approxi- Alzheimer’s disease.
mately 2 hours after the methadone to augment the high Tolerance. While there is controversy about whether
they experience. Benzodiazepines are also used by abusers or not patients develop tolerance to the anxiolytic effects
to self-medicate the symptoms of opiate withdrawal or of benzodiazepines, tolerance to some of the other ef-
to treat the adverse effects of other drugs like cocaine or fects, including the sedation generally brought on by ben-
alcohol. zodiazepines, does develop.7 This may affect the abuser’s
J Clin Psychiatry 2005;66 (suppl 2) 29
Charles P. O’Brien
choice of benzodiazepine and cause him or her to require Table 2. Street Value and “Use Again” Value
higher and higher doses to get the desired euphoria. of Benzodiazepinesa
Relative high. Several studies8–11 have asked individ- Benzodiazepine Street Value “Use Again” Valueb
uals who have a history of substance abuse to subjectively Methaqualone 300 mg $3.00 12.2
rate various benzodiazepines according to the highs ex- Diazepam 20 mg $1.60 8.7
Diazepam 10 mg $0.70 6.3
perienced when taking them. Of the benzodiazepines, Lorazepam 4 mg $0.80 6.8
abusers rate diazepam as having the greatest high. Loraze- Lorazepam 2 mg $0.30 6.0
pam and alprazolam scored slightly (but not significantly) Alprazolam 2 mg $0.70 8.0
Prazepam 40 mg $0.60 7.1
lower in relative high than diazepam.8 Funderburk and Placebo $0.20 3.3
colleagues9 found diazepam and lorazepam similar in sub- a
Data from Cole.13
b
jective ratings of drug effect and drug liking by abusers. “Use again” values are rated on a 16-point scale, where 0 indicates
“would never use the drug again,” 8 indicates “maybe,” and 16
Clorazepate received significantly lower subjective rat- indicates “would definitely enjoy using drug again.”15
ings of liking from drug abusers than diazepam or loraze-
pam.10 Ratings of relative high were significantly less for
oxazepam and chlordiazepoxide compared with diazepam,
lorazepam, and alprazolam.11,12 which the medication was originally taken. Some patients
Street value. Although the relative high received from who were prescribed benzodiazepines for a certain stress-
the drug affects the popularity and desirability of the drug, ful time in their lives may experience hypnotic-induced
the street value is also affected by the reputation that the insomnia when they stop taking them. Other patients who
drug has on the street and by how much money abusers are began using benzodiazepines to treat anxiety may experi-
willing to pay for it. According to Cole’s 1988 presenta- ence a withdrawal syndrome that includes a return of anx-
tion of data from Boston substance abusers,13 methaqua- ious symptoms after discontinuation of use. These with-
lone 300 mg had the highest street value. (Methaqualone drawal syndromes are usually short in duration and should
is a sedative-euphoriant that was widely available and be differentiated from a relapse of anxiety, which will be
widely abused until it was placed on Schedule I in 1984.14) discussed later in Withdrawal vs. Relapse of Anxiety.
Methaqualone was followed by diazepam 20 mg, which
had about half the street value (Table 2).13 Because street LONG-TERM USE OF BENZODIAZEPINES
value is affected by drug reputation and supply and de-
mand, these values do not necessarily make rational sense. One of the biggest controversies surrounding benzo-
For instance, a 20-mg tablet of diazepam was valued diazepine use has been the efficacy and safety of long-
higher ($1.60) than 2 10-mg tablets of diazepam ($1.40). term use. In the 1980s, some psychiatrists, including many
This same street value discrepancy occurred in ratings for in the United Kingdom, stated that benzodiazepines did
2-mg and 4-mg tablets of lorazepam. more harm than good because the dependence developed
“Use again” value. Drug abusers were also asked to by some long-term users outweighed their potential anxio-
rate various benzodiazepines according to whether or not lytic benefits.16,17 This disapproval of long-term use was
they would use them again.13,15 Again, methaqualone 300 supported with the hypothesis that patients develop a
mg and diazepam 20 mg scored highest, and lorazepam 2 tolerance to the antianxiety effects of benzodiazepines,
mg and placebo scored lowest (see Table 2).13 which, if true, would mean that benzodiazepines would be
medically useful only for short-term treatment, and pa-
DEPENDENCE ON BENZODIAZEPINES tients would not need to use benzodiazepines long enough
WITHOUT INTENTIONAL ABUSE to develop a dependence. However, clinical evidence does
not support the development of this tolerance7,18; in fact,
Long-term use of benzodiazepines may cause physical anecdotal evidence from prescribing psychiatrists often
dependence; if unaccompanied by drug-seeking behavior, indicates long-term anxiolytic effectiveness of benzo-
this is neither an abuse nor an addiction. Few cases of ad- diazepines.18,19
diction or abuse arise from legitimate benzodiazepine use. Tolerance seems to develop selectively to different
Physical dependence is more relevant to clinicians than drug effects. Although chronic users of benzodiazepines
deliberate abuse because it occurs in patients who begin do develop a tolerance to the sedation and psychomotor
taking prescribed benzodiazepines for an anxiety disorder impairment caused initially by benzodiazepines, tolerance
under the direction of their doctors. Most unintentional to the acute short-term memory effects does not develop.7
abusers are unaware of their benzodiazepine dependence Thus, it is theoretically possible that antianxiety effects do
until they try to abruptly discontinue using the drugs. not show tolerance, but this has been difficult to address
Symptoms experienced after benzodiazepine discontinu- experimentally.
ation may be pharmacologic withdrawal symptoms, or The reticence of British psychiatrists to use benzo-
they may constitute a return of the anxiety disorder for diazepines for long-term treatment may also stem from the
30 J Clin Psychiatry 2005;66 (suppl 2)
Benzodiazepine Use, Abuse, and Dependence
inappropriate long-term prescribing that took place in the sometimes be difficult to determine whether a patient is
United Kingdom in the 1970s at the height of benzodiaze- experiencing benzodiazepine withdrawal or a relapse of
pine popularity. During this time, studies20–23 showed that anxiety. It is important, however, to differentiate between
U.K. patients had higher long-term and repeat use rates these situations so that patients who are experiencing a
than patients in other developed countries and that many brief withdrawal do not unnecessarily begin antianxiety
British patients were receiving repeat prescriptions without treatment again.
a physician consultation. At the same time, long-term ben- There are 2 specific differences between withdrawal
zodiazepine use in the United States was lower than in the from anxiolytic psychotropics and a relapse of anxiety.
United Kingdom.24 The first difference is the length of time between dis-
continuation of treatment and appearance of symptoms, as
WITHDRAWAL FROM BENZODIAZEPINES well as tendency of the symptoms to improve or worsen.
True withdrawal symptoms usually develop within a few
Withdrawal symptoms occur when there is a decline days of stopping the medication; they are most severe di-
in the blood or tissue concentration of any dependence- rectly after discontinuation of benzodiazepine use but con-
forming substance that an individual has been continuously tinue to lessen until, as time progresses, these symptoms
taking. Symptoms of withdrawal are time-limited, usually eventually disappear.30 However, both the length of time
occurring for only 1 or 2 weeks after the discontinuation of between benzodiazepine discontinuation and appearance
the drug, but the duration varies according to the drug and of withdrawal symptoms and the subsequent duration of
the individual person.25 These symptoms are generally the the withdrawal syndrome vary according to the half-life
opposite of the acute effects of the drug, or they may mimic of the benzodiazepine. Drugs with longer half-lives take
the symptoms for which the drug was originally taken. For longer to leave the system or reach a level low enough to
example, withdrawal from habit-forming painkillers may produce withdrawal symptoms, so withdrawal may not
include symptoms of pain, and withdrawal from sleep aids become evident for a week after discontinuation of longer
may include symptoms of insomnia. Withdrawal symp- half-life benzodiazepines like diazepam. In contrast to
toms are usually relieved by administration of the sub- withdrawal syndromes, relapses of anxiety generally man-
stance from which the patient is withdrawing.25 ifest as anxious symptoms that return more than a week
For patients who experience withdrawal from benzo- after benzodiazepine discontinuation and get progressively
diazepines, 3 factors seem to influence the intensity and/or worse until treated.
duration of the withdrawal. The most significant determi- The second difference between withdrawal and relapse
nant of withdrawal is the amount of time spent in treat- is in the symptoms themselves. Symptoms of benzodiaz-
ment. The longer the treatment is, the more likely it is that epine withdrawal include anxiety, agitation, irritability, in-
the patient will experience withdrawal symptoms upon creased sensitivity to light and sound, paresthesias (strange
abrupt discontinuation of treatment. The dose of medica- sensations), muscle cramps, myoclonic jerks, fatigue, in-
tion also affects withdrawal, but it does so in combination somnia, headache, dizziness, concentration difficulties,
with duration of treatment. In a study of patients (N = 180) seizures, nausea, loss of appetite, weight loss, and depres-
taking diazepam, 15 to 40 mg/day,26 only 5% of the patients sion.25,31 Although anxiety relapses encompass some of the
who had been taking the drug for less than 8 months expe- same symptoms, such as nervousness, difficulty sleeping,
rienced withdrawal symptoms, while 43% of the patients and difficulty concentrating, several other symptoms of
taking diazepam for 8 months or more experienced with- withdrawal are not characteristic of anxiety—sensitivity
drawal. Even at low doses, long-term use results in physi- to light and sound, tinnitus, feelings of “electric shocks,”
cal dependence and withdrawal more often than short-term tremors, myoclonic jerks, perceptual changes, and even
use.25 Conversely, higher doses may cause withdrawal after seizures in cases of high-dose dependency.29,31
short-term use. In a study of patients (N = 109) taking al- Pseudowithdrawal is another phenomenon that must be
prazolam, 2 to 10 mg/day, for only 8 weeks,27 distinct tran- considered when deciding if a patient is experiencing ben-
sient withdrawal symptoms occurred in 35% of the pa- zodiazepine withdrawal. Pseudowithdrawal is a psycho-
tients, and rebound panic attacks occurred in 27%. The logical or subjective withdrawal that occurs as a result of
third factor affecting withdrawal is the half-life of the ben- a patient’s apprehension about discontinuing medication.
zodiazepine. Withdrawal symptoms tend to be more severe A review of research25 found that patients who are not
and have a quicker onset in patients taking benzodiaze- aware that they have discontinued medications because
pines with shorter half-lives.28,29 placebo was substituted for their benzodiazepine may have
fewer withdrawal symptoms; conversely, patients who
WITHDRAWAL VS. RELAPSE OF ANXIETY continue to take medication but believe that they are
receiving placebo may experience withdrawal symptoms
Because withdrawal symptoms often mimic the disorder without actual discontinuation of medication. Psycholog-
for which the medication was originally taken, it may ical withdrawal or pseudowithdrawal generally consists
J Clin Psychiatry 2005;66 (suppl 2) 31
Charles P. O’Brien
of anxious symptoms unaccompanied by the other true clonazepam,36 phenobarbital was found less effective in
withdrawal symptoms described above.25,32 successfully tapering sedative hypnotics but equally or
more effective when used to counter recurrent or rebound
CLINICAL OPTIONS FOR DISCONTINUING anxiety.
BENZODIAZEPINE TREATMENT
Treating the Symptoms of Withdrawal
There are several clinical options that help patients Other medications, including carbamazepine, clonidine,
avoid withdrawal symptoms when it is time to discontinue and propranolol, may be used to treat withdrawal symp-
benzodiazepine treatment for anxiety. Some of the clinical toms such as tremor, anxiety, and seizure experienced upon
approaches that show success include, either individually either abrupt or gradual discontinuation of benzodiaze-
or in combination, gradual tapering of the current ben- pines.37 When compared with supplemental doses of buspi-
zodiazepine, switching to a long-acting benzodiazepine, rone, imipramine, and placebo,38 supplemental doses of the
phenobarbital substitution, and treatment of withdrawal anticonvulsant carbamazepine aided the largest percentage
symptoms with other medications. of patients in successfully discontinuing their benzodi-
azepines. In a study of benzodiazepine-withdrawn rats,39
Gradual Taper carbamazepine was able to normalize the stress-response
As with all discontinuation programs, the patient system that was impaired by diazepam withdrawal. The
should be willing to stop using the drug, and the clinician beta-blocker propranolol has been used effectively to treat
should explain why a gradual taper is better than abrupt tremor and cardiovascular withdrawal symptoms,40 and pa-
discontinuation. Although the rate of reduction that will tients receiving medication augmentation with propranolol
allow the patient to avoid withdrawal symptoms varies were more likely to discontinue or decrease their benzo-
from patient to patient and depends on the original dose diazepine use.41
and duration of treatment, a quarter of the daily dose is
generally the maximum amount the medication should be Continued Treatment With Benzodiazepines
reduced each week.17 The minimum time for tapering from If discontinuation of benzodiazepine treatment is es-
full dosage to total discontinuation, therefore, should be pecially distressing to the patient, if pharmacologic de-
4 weeks. If this reduction is too drastic for the patient and pendence is extremely high, or if rebound anxiety occurs
he or she experiences withdrawal symptoms, the dose may after several attempts to discontinue the benzodiazepine,
be returned for a short period to the level just above the another option may be the most viable: continuation of
amount that brought on symptoms; tapering should then benzodiazepine treatment. Generalized anxiety disorder is
continue from this level. Nonetheless, the physician and now recognized as a chronic illness that impairs daily func-
patient must remember that the patient may still experi- tioning and causes patients to suffer for many years.42 Con-
ence some withdrawal symptoms for as long as the taper- tinual treatment with a low-dose benzodiazepine may pro-
ing continues.25 vide some patients the most functionality with the fewest
negative effects.
Substitution With a Long-Acting Benzodiazepine
or Phenobarbital CONCLUSION
Because short-acting benzodiazepines are more likely
to cause dependence and withdrawal upon discontinuation The individuals who deliberately abuse benzodiaze-
than long-acting benzodiazepines, switching to a long- pines and those who inadvertently become dependent on
acting benzodiazepine such as clonazepam may help to them differ greatly in intention, purpose, and treatment.
prevent or lessen withdrawal symptoms.33 In a study of Deliberate abuse of benzodiazepines is most often found
patients switching from alprazolam to clonazepam,34 pa- within a polydrug use pattern as an attempt to get high or
tients rated clonazepam better than alprazolam because treat the effects of other drugs used for this purpose; ben-
it lessened their mid-dose anxiety. This positive ranking zodiazepines are rarely used as the primary drug of abuse.
was attributable to the slow onset and long half-life of clo- This type of abuse is most appropriately treated in a sub-
nazepam. Slowly absorbed and slowly eliminated benzo- stance abuse setting and may be partially avoided by not
diazepines yield a more sustained and gradual antianxiety prescribing short-acting, euphoriant benzodiazepines for
effect,35 so these drugs may facilitate a smoother discon- individuals with known substance abuse issues. The num-
tinuation than benzodiazepines with a faster onset and ber of people who start taking benzodiazepines to treat
shorter half-life without negative withdrawal sequelae. anxiety and end up abusing them or becoming truly ad-
The barbiturate phenobarbital is another long-acting, dicted is very small.
cross-tolerant medication that may be effectively substi- For those patients who inadvertently become dependent
tuted for short-acting benzodiazepines upon which a pa- on therapeutic doses of benzodiazepines, several clinical
tient has developed dependence. When compared with approaches can assist those who are willing and able to dis-
32 J Clin Psychiatry 2005;66 (suppl 2)
Benzodiazepine Use, Abuse, and Dependence
continue their medication to do so in the most symptom- Issues; Sept 30–Oct 1, 1988; Boston, Mass
13. Cole JO. Estimated values of different benzodiazepines. Presented
free way possible. Nonetheless, because anxiety is a chron- at Benzodiazepines: Therapeutic, Biologic, and Psychosocial Issues;
ic disorder that may need long-term continual treatment, a Sept 30–Oct 1, 1988; Boston, Mass
need for sustained benzodiazepine treatment should not 14. Ionescu-Pioggia M, Bird M, Cole JO. Subjective effects of methaqualone.
NIDA Res Monogr 1989;95:455
necessarily be considered dependency or addiction. A pa- 15. Cole JO, Orzack MH, Beake B, et al. Assessment of the abuse liability
tient taking regular benzodiazepine treatment for chronic of buspirone in recreational sedative users. J Clin Psychiatry 1982;43
anxiety may be similar to an asthmatic who must always (12,Sec 2):69–75
16. Ashton H. Benzodiazepine withdrawal: an unfinished story. Br Med J
have medicine on hand or a patient suffering from allergies (Clin Res Ed) 1984;288:1135–1140
who must take allergy medicine daily for years. A benzo- 17. Committee on the Review of Medicines. Systematic review of the benzo-
diazepine that successfully performs its intended duty as an diazepines: guidelines for data sheets on diazepam, chlordiazepoxide,
medazepam, clorazepate, lorazepam, oxazepam, temazepam, triazolam,
anxiolytic—aiding in the daily functioning of the patient nitrazepam, and flurazepam. Br Med J 1980;280:910–912
without adding impairment—serves a legitimate medical 18. Marks J. The benzodiazepines: for good or evil. Neuropsychobiology
purpose and improves the quality of life for chronic anxi- 1983;10:115–126
19. Hollister LE, Conley FK, Britt RH, et al. Long-term use of diazepam.
ety patients. JAMA 1981;246:1568–1570
20. Murdoch JC. The epidemiology of prescribing in an urban general
Drug names: alprazolam (Xanax and others), buspirone (BuSpar practice. J R Coll Gen Pract 1980;30:593–602
and others), carbamazepine (Tegretol, Carbatrol, and others), 21. Parish PA. The prescribing of psychotropic drugs in general practice.
chlordiazepoxide (Librium and others), clonazepam (Klonopin J R Coll Gen Pract 1971;21(suppl 4):1–77
and others), clonidine (Duraclon, Catapres, and others), clorazepate 22. Parker EJ, Schrieber V. Repeat prescribing—a study in one practice.
(Gen-Xene, Tranxene, and others), diazepam (Valium and others), J R Coll Gen Pract 1980;30:603–606
imipramine (Tofranil, Surmontil, and others), lorazepam (Ativan and 23. Williams P, Murray J, Clare A. A longitudinal study of psychotropic drug
others), methadone (Methadose, Dolophine, and others), oxazepam prescription. Psychol Med 1982;12:201–206
(Serax and others), propranolol (Innopran XL, Inderal, and others). 24. Marks J. The benzodiazepines: an international perspective. J Psycho-
active Drugs 1983;15:137–149
25. Roy-Byrne PP, Hommer D. Benzodiazepine withdrawal: overview and
Disclosure of off-label usage: The author has determined that, to the implications for the treatment of anxiety. Am J Med 1988;84:1041–1052
best of his knowledge, carbamazepine, phenobarbital, propranolol, 26. Rickels K, Case WG, Downing RW, et al. Long-term diazepam therapy
and clonidine have not been approved by the U.S. Food and Drug and clinical outcome. JAMA 1983;250:767–771
Administration for the treatment of benzodiazepine withdrawal. 27. Pecknold JC. Discontinuation reactions to alprazolam in panic disorder.
J Psychiatr Res 1993;27(suppl 1):155–170
REFERENCES 28. Rickels K, Schweizer E, Case G, et al. Long-term therapeutic use
of benzodiazepines: 1, effects of abrupt discontinuation. Arch Gen
Psychiatry 1990;47:899–907
1. American Psychiatric Association. Diagnostic and Statistical Manual 29. Busto U, Sellers EM, Naranjo CA, et al. Withdrawal reaction after
of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: long-term therapeutic use of benzodiazepines. N Engl J Med 1986;
American Psychiatric Association; 2000 315:854–859
2. Haefely W. Biological basis of drug-induced tolerance, rebound, 30. Hallstrom C, Lader M. Benzodiazepine withdrawal phenomena.
and dependence: contribution of recent research on benzodiazepines. Int Pharmacopsychiatry 1981;16:235–244
Pharmacopsychiatry 1986;19:353–361 31. Owen RT, Tyrer P. Benzodiazepine dependence: a review of the evidence.
3. Woody GE, Mintz J, O’Hare K, et al. Diazepam use by patients in a Drugs 1983;25:385–398
methadone program: how serious a problem? J Psychedelic Drugs 1975; 32. Tyrer P, Owen R, Dawling S. Gradual withdrawal of diazepam after
7:373–379 long-term therapy. Lancet 1983;1:1402–1406
4. Bailey L, Ward M, Musa MN. Clinical pharmacokinetics of benzodiaze- 33. Albeck JH. Withdrawal and detoxification from benzodiazepine
pines. J Clin Pharmacol 1994;34:804–811 dependence: a potential role for clonazepam. J Clin Psychiatry 1987;
5. Estivill E, Bov A, Garca-Borreguero D, et al. Consensus on drug 48(suppl):43–49
treatment, definition, and diagnosis for insomnia. Clin Drug Invest 34. Herman JB, Rosenbaum JF, Brotman AW. The alprazolam to clonazepam
2003;23:351–385 switch for the treatment of panic disorder. J Clin Psychopharmacol 1987;
6. Greenblatt DJ, Harmayz JS, Shader RI. Clinical pharmacokinetics of an- 7:175–178
xiolytics and hypnotics in the elderly: therapeutic considerations (part I). 35. Teboul E, Chouinard G. A guide to benzodiazepine selection, part II:
Clin Pharmacokinet 1991;21:165–177 clinical aspects. Can J Psychiatry 1991;36:62–73
7. Lucki I, Rickels K, Geller AM. Chronic use of benzodiazepines and psy- 36. Sullivan M, Toshima M, Lynn P, et al. Phenobarbital versus clonazepam
chomotor and cognitive test performance. Psychopharmacology (Berl) for sedative-hypnotic taper in chronic pain patients: a pilot study. Ann
1986;88:426–433 Clin Psychiatry 1993;5:123–128
8. Orzack MH, Friedman L, Dessain E, et al. Comparative study of the 37. Klein E, Uhde TW, Post RM. Preliminary evidence for the utility of
abuse liability of alprazolam, lorazepam, diazepam, methaqualone, and carbamazepine in alprazolam withdrawal. Am J Psychiatry 1986;143:
placebo. Int J Addict 1988;23:449–467 235–236
9. Funderburk FR, Griffiths RR, McLeod DR, et al. Relative abuse liability 38. Rickels K, Case WG, Schweizer E, et al. Benzodiazepine dependence:
of lorazepam and diazepam: an evaluation in ‘recreational’ drug users. management of discontinuation. Psychopharmacol Bull 1990;26:63–68
Drug Alcohol Depend 1988;22:215–222 39. Martijena ID, Lacerra C, Molina VA. Carbamazepine normalizes
10. Griffiths RR, Roache JD. Abuse liability of benzodiazepines: a review of the altered behavioral and neurochemical response to stress in
human studies evaluating subjective and/or reinforcing effects. In: Smith benzodiazepine-withdrawn rats. Eur J Pharmacol 1997;330:101–108
DE, ed. The Benzodiazepines: Current Standards for Medical Practice. 40. Dubovsky SL. Generalized anxiety disorder: new concepts and
Norwell, Mass: Kluwer Academic Publishers; 1985:209–225 psychopharmacologic therapies. J Clin Psychiatry 1990;51(suppl 1):
11. Iguchi MY, Griffiths RR, Bickel WK, et al. Relative abuse liability of 3–10
benzodiazepines in methadone maintained populations in three cities. 41. Hallstrom C, Crouch G, Robson M, et al. The treatment of tranquilizer
NIDA Res Monogr 1989;95:364–365 dependence by propranolol. Postgrad Med J 1988;64(suppl 2):40–44
12. Griffiths RR. Laboratory studies of benzodiazepine reinforcement. 42. Rynn MA, Brawman-Mintzer O. Generalized anxiety disorders:
Presented at Benzodiazepines: Therapeutic, Biologic, and Psychosocial acute and chronic treatment. CNS Spectr 2004;9:716–723
J Clin Psychiatry 2005;66 (suppl 2) 33
You might also like
- Drug InteractionsDocument16 pagesDrug InteractionsChrizzy ValenciaNo ratings yet
- Managing Opioid Withdrawal With BuprenorphineDocument7 pagesManaging Opioid Withdrawal With BuprenorphineAgata KurniawatyNo ratings yet
- Pharm All NotesDocument511 pagesPharm All NotesShoaib Ali100% (1)
- Schizophrenia Treatment & ManagementDocument16 pagesSchizophrenia Treatment & ManagementDimas Januar100% (2)
- Psychiatry Passmedicine & Onexamination Notes 2016 PDFDocument34 pagesPsychiatry Passmedicine & Onexamination Notes 2016 PDFJyothi ReddyNo ratings yet
- Medication Assisted Treatment 9-21-20121Document6 pagesMedication Assisted Treatment 9-21-20121GodstruthNo ratings yet
- Vesicular and Bullous Dermatosis MCQsDocument59 pagesVesicular and Bullous Dermatosis MCQsDr.Tawheed88% (8)
- Diagnostic Skills of Acupuncture: Lecture By: M.K. SastryDocument106 pagesDiagnostic Skills of Acupuncture: Lecture By: M.K. SastryLupa IngatanNo ratings yet
- Dependence, Withdrawal and Rebound of CNSDocument23 pagesDependence, Withdrawal and Rebound of CNSHassan AhmedNo ratings yet
- Motility Disorders of EsophagusDocument44 pagesMotility Disorders of EsophagusmackieccNo ratings yet
- Subutex Quick-Start-GuideDocument6 pagesSubutex Quick-Start-GuideDanNo ratings yet
- Nursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationDocument8 pagesNursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationKrahNo ratings yet
- NCP StrokeDocument7 pagesNCP StrokeMonica Gagarin Cortez100% (1)
- DRUG EDUCATION AND VICE CONTROL NewDocument34 pagesDRUG EDUCATION AND VICE CONTROL NewDark MageNo ratings yet
- Laser Therapy ProtocolsDocument89 pagesLaser Therapy ProtocolsSYED ALI HUSSAINNo ratings yet
- Central Nervous System Depressant Drug Abuse And Addiction:: Implications for CounselingFrom EverandCentral Nervous System Depressant Drug Abuse And Addiction:: Implications for CounselingNo ratings yet
- 5 Abuse Dep Benzo - Unlocked PDFDocument6 pages5 Abuse Dep Benzo - Unlocked PDFweffjoiNo ratings yet
- Management of Benzodiazepine Misuse and Dependence: Jonathan Brett Bridin MurnionDocument4 pagesManagement of Benzodiazepine Misuse and Dependence: Jonathan Brett Bridin MurnionLucius MarpleNo ratings yet
- Part I. Benzodiazepines-Side Effects, Abuse Risk and AlternativesDocument13 pagesPart I. Benzodiazepines-Side Effects, Abuse Risk and AlternativesPamella Kusuma WerdanieNo ratings yet
- BenzodiazepinesDocument7 pagesBenzodiazepinesRully B ChristinaNo ratings yet
- Benzodiazepine Safety and Tapering: A E B D T RDocument3 pagesBenzodiazepine Safety and Tapering: A E B D T RGulzaib KhokharNo ratings yet
- Are There Guidelines For The Responsible Prescription of Benzodiazepines?Document7 pagesAre There Guidelines For The Responsible Prescription of Benzodiazepines?Rian YupitaNo ratings yet
- Treatment of Benzodiazepine DependenceDocument8 pagesTreatment of Benzodiazepine DependenceJeffly Varro GilbertNo ratings yet
- Managementul BenzodiazepinelorDocument10 pagesManagementul BenzodiazepinelorSendruc OvidiuNo ratings yet
- Understanding TheDocument19 pagesUnderstanding TheHot Parsaulian SiregarNo ratings yet
- Addiction Part 1 Benzodiazepines Side Effects, About Risk and AlternativesDocument11 pagesAddiction Part 1 Benzodiazepines Side Effects, About Risk and AlternativesEga Candra FaurizaNo ratings yet
- Drug Ons: AdverseDocument5 pagesDrug Ons: AdverseMisty CheifNo ratings yet
- Benzodiazepine Dependence: Focus On Withdrawal Syndrome: Dépendance Aux Benzodiazépines: Le Syndrome de SevrageDocument6 pagesBenzodiazepine Dependence: Focus On Withdrawal Syndrome: Dépendance Aux Benzodiazépines: Le Syndrome de SevrageArias Gutierrez KatherineNo ratings yet
- Benzodiazepine Clinical Tool W TaperDocument4 pagesBenzodiazepine Clinical Tool W TaperrahmaNo ratings yet
- Antipsychotics,-WPS OfficeDocument7 pagesAntipsychotics,-WPS Officermconvidhya sri2015No ratings yet
- John Marks MA, MD, FRCP, FRCPath, MRCPsych (Auth.) - The Benzodiazepines - Use, Overuse, Misuse, Abuse-Springer Netherlands (1978)Document102 pagesJohn Marks MA, MD, FRCP, FRCPath, MRCPsych (Auth.) - The Benzodiazepines - Use, Overuse, Misuse, Abuse-Springer Netherlands (1978)Priscielly Marcelo CristovãoNo ratings yet
- CR 1 PDFDocument22 pagesCR 1 PDFtyleree3No ratings yet
- Part I. Benzodiazepines-Side Effects, Abuse Risk and AlternativesDocument2 pagesPart I. Benzodiazepines-Side Effects, Abuse Risk and AlternativesPamella Kusuma WerdanieNo ratings yet
- 1 - Introduction To PharmacologyDocument31 pages1 - Introduction To PharmacologyTanvir FahimNo ratings yet
- Substance RelatedDocument12 pagesSubstance RelatedJoyce VillalesNo ratings yet
- Uso Inapropiado de Fármacos de Prescripción: Dependencia A Benzodiazepinas en Adultos MayoresDocument7 pagesUso Inapropiado de Fármacos de Prescripción: Dependencia A Benzodiazepinas en Adultos MayorespaofrancoNo ratings yet
- A DrugDocument7 pagesA DrugAsam JawaNo ratings yet
- Prescription Sedative Misuse and Abuse: EviewDocument10 pagesPrescription Sedative Misuse and Abuse: EviewPutu OkyNo ratings yet
- Pharmacoepidemiology of Benzodiazepine and Sedative-Hypnotic Use in A Canadian General Population Cohort During 12 Years of Follow-UpDocument8 pagesPharmacoepidemiology of Benzodiazepine and Sedative-Hypnotic Use in A Canadian General Population Cohort During 12 Years of Follow-UpAnonymous TKSMzgRJoBNo ratings yet
- Antianxiety AgentsDocument4 pagesAntianxiety AgentsRoci ArceNo ratings yet
- Adverse Drug Reactions NotesDocument4 pagesAdverse Drug Reactions NoteskarthikeyanpgtNo ratings yet
- The Benzodiazepine Management: WithdrawalDocument4 pagesThe Benzodiazepine Management: WithdrawalAnne Marie ScerriNo ratings yet
- Therapeutics: A Benjamin Srivastava, John J Mariani, Frances R LevinDocument11 pagesTherapeutics: A Benjamin Srivastava, John J Mariani, Frances R LevinPsiquiatria 2021-2No ratings yet
- PT718Document15 pagesPT718Susmita GhoshNo ratings yet
- Wjem 13 01 26 PDFDocument9 pagesWjem 13 01 26 PDFMoises Vega RodriguezNo ratings yet
- P.01 Drugs of Abuse - Part 1Document3 pagesP.01 Drugs of Abuse - Part 1Yndhira Xheyenn LayloNo ratings yet
- GP Drug & Alcohol Supplement No.9: February 1998Document5 pagesGP Drug & Alcohol Supplement No.9: February 1998NiteshNo ratings yet
- Management of Drug and Alcohol Withdrawal: Review ArticleDocument10 pagesManagement of Drug and Alcohol Withdrawal: Review ArticlehernanbotinaNo ratings yet
- 3 - Lec - PahrmaDocument45 pages3 - Lec - PahrmaDr Nimra MurtazaNo ratings yet
- UCSF Residents Report Fall 2010Document20 pagesUCSF Residents Report Fall 2010souzakhNo ratings yet
- Opioid Dependence: Joseph J. Benich IIIDocument12 pagesOpioid Dependence: Joseph J. Benich IIIValentina Londoño CadavidNo ratings yet
- Kosten 2003Document10 pagesKosten 2003Ana CortezNo ratings yet
- Cdi 7 Lesson 2Document2 pagesCdi 7 Lesson 2Lili ManobanNo ratings yet
- Psychotropic Polypharmacy in Australia, 2006 To 2015: A Descriptive Cohort StudyDocument8 pagesPsychotropic Polypharmacy in Australia, 2006 To 2015: A Descriptive Cohort StudyAna Paula Soares GondimNo ratings yet
- Remington W-1912-1925ooDocument14 pagesRemington W-1912-1925ooMikan De LeonNo ratings yet
- Prescription Drug Misuse: Street DrugsDocument7 pagesPrescription Drug Misuse: Street Drugsrainbow godessNo ratings yet
- Benzodiazepine and Hypnotic Guidelines (V1.0 July 2010)Document18 pagesBenzodiazepine and Hypnotic Guidelines (V1.0 July 2010)Deza IngridNo ratings yet
- Substance-Related and Addictive DisordersDocument28 pagesSubstance-Related and Addictive DisordersPersius NavalNo ratings yet
- Siti Badriah Unit 16Document2 pagesSiti Badriah Unit 16BadriahNo ratings yet
- NC 6042 Week 12 - Potential Abuse and Etiology of Psychotropic Substance Abuse - Version B 2020Document35 pagesNC 6042 Week 12 - Potential Abuse and Etiology of Psychotropic Substance Abuse - Version B 2020TIFFANY CHAN WEN YINGNo ratings yet
- BSN Compiled Notes - PharmacologyDocument6 pagesBSN Compiled Notes - PharmacologyAbigail RegaladoNo ratings yet
- Pharmacological Factors Influencing Drug Compliance Among Patients Taking Psychotropic Drugs - A Cross-Sectional StudyDocument4 pagesPharmacological Factors Influencing Drug Compliance Among Patients Taking Psychotropic Drugs - A Cross-Sectional Studyrmconvidhya sri2015No ratings yet
- Pharma Module 1Document26 pagesPharma Module 1RIZALYN AMANTIADNo ratings yet
- Lilley: Pharmacology and The Nursing Process, 7th EditionDocument8 pagesLilley: Pharmacology and The Nursing Process, 7th EditionthubtendrolmaNo ratings yet
- Prescribing BenzoDocument10 pagesPrescribing BenzoAndreea CraioveanuNo ratings yet
- Cdi8 Assignment1Document7 pagesCdi8 Assignment1ashanagrey68No ratings yet
- Cannabinoid Abuse And Misuse:: Its Connected Impact On Health And Well-BeingFrom EverandCannabinoid Abuse And Misuse:: Its Connected Impact On Health And Well-BeingNo ratings yet
- Chapter 15Document27 pagesChapter 15Jessica nonyeNo ratings yet
- What Is ParaplegiaDocument3 pagesWhat Is Paraplegiaalok_kumar_guptaNo ratings yet
- Acute Limb Ischemic: Titien Buniyati Ali Aspar MappahyaDocument40 pagesAcute Limb Ischemic: Titien Buniyati Ali Aspar MappahyaNurhasanah WahabNo ratings yet
- Mansonella StreptocercaDocument14 pagesMansonella StreptocercaALLISON PAMITTANNo ratings yet
- CDC Welcome LetterDocument5 pagesCDC Welcome Letterapi-242666861No ratings yet
- Blumenfeld Neuroanatomy Ch. 5 SummaryDocument5 pagesBlumenfeld Neuroanatomy Ch. 5 SummaryMeeraNo ratings yet
- Module 1: Foundations of Health Assessment: Lesson 1: Physical Examination and History Taking: OverviewDocument10 pagesModule 1: Foundations of Health Assessment: Lesson 1: Physical Examination and History Taking: OverviewEmily BernatNo ratings yet
- Determination of DeathDocument8 pagesDetermination of DeathZam PamateNo ratings yet
- Normal ObDocument31 pagesNormal ObShai EstrellerNo ratings yet
- Ulkus VarricosumDocument26 pagesUlkus VarricosumNurul FadilahNo ratings yet
- Duodenal GistDocument5 pagesDuodenal Gistmudasir61No ratings yet
- Ineffective Airway ClearanceDocument1 pageIneffective Airway ClearancejomerdalonaNo ratings yet
- Urnal Vox Sanguinis - 2023 - Pons - Prevalence of Red Blood Cell Alloantibodies Among Blood Donors in The French Military BloodDocument5 pagesUrnal Vox Sanguinis - 2023 - Pons - Prevalence of Red Blood Cell Alloantibodies Among Blood Donors in The French Military BloodFauzan.ANo ratings yet
- Vernal Keratoconjunctivitis (VKC)Document19 pagesVernal Keratoconjunctivitis (VKC)api-3742497No ratings yet
- Extreme Preterm Premature Rupture of Membranes: KSM Obstetri Dan Ginekologi Rumah Sakit Umum Pusat PersahabatanDocument27 pagesExtreme Preterm Premature Rupture of Membranes: KSM Obstetri Dan Ginekologi Rumah Sakit Umum Pusat Persahabatanrilla saeliputriNo ratings yet
- Human Health and DiseaseDocument20 pagesHuman Health and DiseaseA BeheraNo ratings yet
- Information Sheet 4.1-4: 1. Occupational Health and Safety IndicatorsDocument3 pagesInformation Sheet 4.1-4: 1. Occupational Health and Safety Indicatorsmark ian joverNo ratings yet
- Geriatric Index of Comorbidity: Validation and Comparison With Other Measures of ComorbidityDocument9 pagesGeriatric Index of Comorbidity: Validation and Comparison With Other Measures of ComorbidityDesya EspriliaNo ratings yet
- Atelektasis Jurnal RadiologiDocument19 pagesAtelektasis Jurnal RadiologiRachmi MerrinaNo ratings yet
- Knowledge and Attitude Towards Malaria Knowlesi: A Case Study at Senaning Village, Ketungau Hulu Sub-District Sintang DistrictDocument15 pagesKnowledge and Attitude Towards Malaria Knowlesi: A Case Study at Senaning Village, Ketungau Hulu Sub-District Sintang DistrictAbdul RamalangiNo ratings yet
- Soft Tissue Disorders and Fibromyalgia: Jaya Ravindran Consultant RheumatologistDocument54 pagesSoft Tissue Disorders and Fibromyalgia: Jaya Ravindran Consultant RheumatologistarunupadhayaNo ratings yet
- Sepsis Bundle by DR - ZakiDocument3 pagesSepsis Bundle by DR - Zakizaki ansariNo ratings yet
- Ems NC Iii - SagDocument10 pagesEms NC Iii - SagJaypz DelNo ratings yet