Professional Documents
Culture Documents
Coi 160034
Uploaded by
David OlmosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Coi 160034
Uploaded by
David OlmosCopyright:
Available Formats
Research
JAMA Oncology | Original Investigation
Association of AR-V7 on Circulating Tumor Cells
as a Treatment-Specific Biomarker With Outcomes
and Survival in Castration-Resistant Prostate Cancer
Howard I. Scher, MD; David Lu, PhD; Nicole A. Schreiber, BA; Jessica Louw, BS; Ryon P. Graf, PhD;
Hebert A. Vargas, MD; Ann Johnson, MS; Adam Jendrisak, MBA; Richard Bambury, MB, BCh, BAO;
Daniel Danila, MD; Brigit McLaughlin, BS; Justin Wahl, BS; Stephanie B. Greene, PhD; Glenn Heller, PhD;
Dena Marrinucci, PhD; Martin Fleisher, PhD; Ryan Dittamore, MBA
Invited Commentary
IMPORTANCE A critical decision in the management of metastatic castration-resistant Supplemental content at
prostate cancer (mCRPC) is when to administer an androgen receptor signaling (ARS) jamaoncology.com
inhibitor or a taxane.
OBJECTIVE To determine if pretherapy nuclear androgen-receptor splice variant 7 (AR-V7)
protein expression and localization on circulating tumor cells (CTCs) is a treatment-specific
marker for response and outcomes between ARS inhibitors and taxanes.
DESIGN, SETTING, AND PARTICIPANTS For this cross-sectional cohort study at Memorial Sloan
Kettering Cancer Center, 265 men with progressive mCRPC undergoing a change in
treatment were considered; 86 were excluded because they were not initiating ARS or taxane
therapy; and 18 were excluded for processing time constraints, leaving 161 patients for
analysis. Between December 2012 and March 2015, blood was collected and processed from
patients with progressive mCRPC immediately prior to new line of systemic therapy. Patients
were followed up to 3 years.
MAIN OUTCOMES AND MEASURES Prostate-specific antigen (PSA) response, time receiving
therapy, radiographic progression-free survival (rPFS), and overall survival (OS).
RESULTS Overall, of 193 prospectively collected blood samples from 161 men with mCRPC, 191
were evaluable (128 pre-ARS inhibitor and 63 pretaxane). AR-V7–positive CTCs were found in
34 samples (18%), including 3% of first-line, 18% of second-line, and 31% of third- or greater
line samples. Patients whose samples had AR-V7–positive CTCs before ARS inhibition had
resistant posttherapy PSA changes (PTPC), shorter rPFS, shorter time on therapy, and shorter
OS than those without AR-V7–positive CTCs. Overall, resistant PTPC were seen in 65 of 112
samples (58%) without detectable AR-V7–positive CTCs prior to ARS inhibition. There were
statistically significant differences in OS but not in PTPC, time on therapy, or rPFS for patients
with or without pretherapy AR-V7–positive CTCs treated with a taxane. A multivariable model
adjusting for baseline factors associated with survival showed superior OS with taxanes
relative to ARS inhibitors when AR-V7–positive CTCs were detected pretherapy (hazard ratio,
0.24; 95% CI, 0.10-0.57; P = .035).
CONCLUSIONS AND RELEVANCE The results validate CTC nuclear expression of AR-V7 protein
in men with mCRPC as a treatment-specific biomarker that is associated with superior
survival on taxane therapy over ARS-directed therapy in a clinical practice setting. Continued
examination of this biomarker in prospective studies will further aid clinical utility.
Author Affiliations: Author
affiliations are listed at the end of this
article.
Corresponding Author: Howard I.
Scher, MD, Genitourinary Oncology
Service, Department of Medicine,
Sidney Kimmel Center for Prostate
and Urologic Cancers, Memorial Sloan
Kettering Cancer Center,
JAMA Oncol. doi:10.1001/jamaoncol.2016.1828 1275 York Ave, New York, NY 10065
Published online June 4, 2016. Corrected on September 29, 2016. (scherh@mskcc.org).
(Reprinted) E1
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
Research Original Investigation AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes
P
atients with progressive, metastatic castration-
resistant prostate cancer (mCRPC) are often classified Key Points
on the basis of prior chemotherapy exposure, consid-
Question Can the measurement of the nuclear androgen-
ered by many to provide modest clinical benefit relative to the receptor splice variant 7 (AR-V7) protein in circulating tumor cells
overall burden of treatment. Consequently, many patients who (CTCs) be a treatment-specific biomarker in metastatic
might benefit from chemotherapy never receive it, while oth- castration-resistant prostate cancer (mCRPC) at therapeutic
ers are only offered chemotherapy as a last resort when toler- decision points in the first-line, second-line, or third or greater line
ance and overall response rates are poor.1 Multiple approved setting?
therapeutic options with diverse mechanisms of action proven Findings In this cross-sectional cohort study, mCRPC patients
to prolong life are currently available—at issue is how best to with pre-androgen receptor signaling (ARS) inhibitor
use them to maximize benefit for individual patients, deci- AR-V7–positive CTCs had resistant prostate-specific antigen
sions that are often empirically rather than scientifically based. responses, shorter time on therapy, shorter radiographic
progression-free survival, and inferior overall survival. In a
Simply reviewing the data from registration trials can be mis-
multivariable model incorporating line of therapy and other clinical
leading because the eligibility criteria are optimized for suc- features, AR-V7 status showed significant treatment-specific
cess and by the fact that patients treated on clinical protocols interaction with taxane administration.
often experience outcomes superior to those treated in a clini-
Meaning Pretherapy CTC nuclear expression of AR-V7 protein in
cal setting.2 Further, although line of therapy and sequence
men with mCRPC is a treatment-specific biomarker predicting
of administration do matter, patterns of cross-sensitivity and superior overall survival for taxane therapy over ARS inhibitors in a
drug resistance are not predictable from patient to patient.3 clinical practice setting, warranting prospective validation.
This dilemma led the Prostate Cancer Working Group (PCWG3)
to reclassify the clinical states of mCRPC based on the order
individual treatments are administered, regardless of type.4 Epic Sciences non-EpCAM-based CTC detection platform.15,16
Validated predictive biomarkers are needed to guide thera- The context of use is the clinical decision point at which a
peutic decisions. change in systemic therapy is needed. The focus was the as-
Circulating tumor cells (CTCs) are a potential source of tu- sociation between the pretherapy detection of AR-V7–
mor for profiling that can be serially obtained with minimal positive CTCs with line of therapy and objective clinical out-
patient discomfort. Studies using a range of platforms in mul- comes following treatment with the most frequently used,
tiple tumor types have shown that prognosis is worse in pa- approved drug classes for management of mCRPC: ARS inhibi-
tients with detectable CTCs vs those without.5 Serial biologic tors and taxanes.
characterization of CTCs can provide insights into drivers of
tumor growth in patients, allowing the pharmacodynamic ef-
fects of targeted therapies to be assessed, potentially en-
abling the prediction of sensitivity to a specific treatment as
Methods
the disease evolves over time.5 The promise offered by these Patient Selection
analyses in research contrasts sharply with their use in prac- Between December 2012 and March 2015, 265 patients with
tice. Needed in both cases, however, are validated assays for histologically confirmed mCRPC undergoing a change in sys-
predictive biomarkers to inform the selection of a specific temic therapy for progressive disease were treated at Memo-
therapy for a specific patient at a specific point in time.6,7 rial Sloan Kettering Cancer Center (MSKCC). Of these, 104 were
Prostate cancer is an androgen-dependent disease. Even excluded because they were not starting therapy with abi-
tumors that are resistant to castration remain androgen re- raterone acetate, enzalutamide, ARN-509, docetaxel, cabazi-
ceptor (AR) dependent. Androgen receptor splice variants lack taxel, or paclitaxel, or owing to constraints on processing time,
the C-terminal ligand-binding domain but retain the N- leaving 191 evaluable samples from 161 unique patients for
terminal transcriptional elements that can activate AR signal- analysis (eFigure 1 in the Supplement).
ing (ARS) independent of ligand.8,9 In a recent report, detec- All patients underwent a history evaluation that in-
tion of the androgen-receptor splice variant 7 (AR-V7) cluded stage at diagnosis, initial management and all subse-
messenger RNA (mRNA) transcript in pooled epithelial cell ad- quent systemic therapies, a physical examination, and labo-
hesion molecule (EpCAM)-positive CTCs of men with progres- ratory studies including complete blood cell count, chemistry
sive mCRPC was associated with resistance to the ARS inhibi- panel (albumin, alkaline phosphatase, lactate dehydroge-
tors abiraterone and enzalutamide.10 The same group later nases, and creatinine), and serum testosterone to confirm cas-
demonstrated that the presence of AR-V7 mRNA in CTCs did tration status (<50 ng/dL [to convert to nmol/L, multiply by
not predict response to taxanes.11 This finding was validated 0.0347]). Documentation of disease progression required a
by an independent group using a similar assay that found no minimum of 2 rising prostate-specific antigen (PSA) levels 1 or
association between the presence of AR-V7 transcripts and re- more weeks apart, new lesions by bone scintigraphy, and/or
sponse to cabazitaxel.12 Taken together, the results suggest that new or enlarging soft tissue lesions by computed tomogra-
AR-V7 could represent a biomarker to guide treatment selec- phy (CT) or magnetic resonance imaging (MRI), per the Pros-
tion in mCRPC.13,14 tate Cancer Clinical Trials Working Group 2 (PCWG2)
Herein, we report on the analytical and clinical valida- guidelines.17 All patients signed consent forms based on an in-
tion of an AR-V7 protein immunofluorescent assay run on the stitutional review board–approved protocol, and blood samples
E2 JAMA Oncology Published online June 4, 2016 (Reprinted) jamaoncology.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes Original Investigation Research
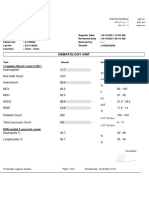
Table. Patient and Sample Demographics
Patient Characteristic All Patients
Unique patients, No. 161
Age, median (range), y 68 (45-91)
Primary treatment, No. (%)
Prostatectomy 77 (48)
Radiation 28 (18)
Brachytherapy 7 (4)
None 49 (30)
Sample Characteristic Pre-AR Therapy Pretaxane Therapy P Value All Samples
Baseline samples, No. 130 63 NA 193
Age, median (range), y 68.5 (45-87) 68 (48-91) .42 68 (45-91)
Blood age, 25 (2-78) 27 (1-51) .26 26 (1-78)
median (range), h
Treatment decision, Abbreviations: ALB, albumin; ALK,
No. (%)a alkaline phosphatase; AR, androgen
First-line 56 (43.1) 11 (17.4) 67 (34.7) receptor; AR-V7, nuclear
androgen-receptor splice variant 7;
Second-line 40 (30.8) 10 (15.9) <.001 50 (25.9) Hgb, hemoglobin; LDH, lactic
Third-line or later 34 (26.1) 42 (66.7) 76 (39.4) dehydrogenase; LN, lymph node;
Prior exposure to mCRPC, metastatic
life-prolonging therapies, castration-resistant prostate cancer;
No. (%)b PSA, prostate-specific antigen.
a
None 56 (43.1) 11 (17.5) 67 (34.7) Only includes SOC life-prolonging
ARc only 34 (26.2) 19 (30.1) 53 (27.5) therapies and experimental
<.001 therapies patient was exposed to
Taxaned and/or other 10 (7.7) 0 10 (5.2) after standard ADT and
AR and taxane 30 (23.0) 33 (52.4) 63 (32.6) development of mCRPC disease and
and/or other prior to initiation on the baseline
Chemotherapy status, therapy.
No. (%) b
Overall, 17 patients received both
Chemotherapy-naïve 90 (69) 30 (48) 120 (62) AR and taxane for 1 or more
.005
Chemotherapy-exposed 40 (31) 33 (52) 73 (38) occurrences. P values from
Wilcoxon Rank Sum test for
Metastatic disease, No. (%)
continuous parameters and Fisher
Bone only 39 (30) 19 (30) 1 [Reference] 58 (30) exact test for categorical
LN onlye 21 (16) 2 (3) .008 23 (12) parameters.
c
Bone and LN 51 (39) 18 (29) .15 69 (36) Androgen receptor therapies
include abiraterone acetate,
Bone and visceral 19 (15) 24 (38) <.001 43 (22)
and/or LNe enzalutamide, and ARN-509.
d
Laboratory measures Taxane therapies include docetaxel,
pretherapy, median (range) cabazitaxel, and paclitaxel.
PSA, ng/mLf 28.0 (0.1-2454.5) 99.5 (0.1-3728.2) <.001 37.7 (0.1-3728.2) e
Includes patients with other soft
Hgb, g/dL g
12.4 (7.0-15.0) 11.6 (8.2-14.5) .005 12.1 (7.0-15.0) tissue disease.
f
ALK, U/Lh 99 (25-2170) 181 (49-1816) <.001 111 (25-2170) To convert ng/mL to μg/L, multiply
h
by 1.0.
LDH, U/L 208 (123-1293) 251.5 (141-1004) <.001 220 (123-1293) g
To convert g/dL to g/L, multiply by
ALB, g/dLg 4.2 (3.4-4.9) 4.2 (3.1-4.9) .80 4.2 (3.1-4.9) 10.
AR-V7 test (total 1.77 (0-441.3) 4.35 (0-601.5) .004 2.38 (0-601.5) h
To convert U/L to μkat/L, multiply
CTCs/mL)
by 0.0167.
were obtained prior to initiation of either an ARS inhibitor or 50% or greater decline. Radiographic progression-free sur-
taxane-based therapy. The choice of therapy was at the dis- vival (rPFS), time receiving therapy, and overall survival (OS)
cretion of the treating physician. The treatment characteris- were also reported. Time receiving therapy was calculated from
tics are summarized in the Table. initiation of therapy until date of drug discontinuation for any
reason. Radiographic progression was determined by inde-
Posttreatment Outcomes pendent blinded review of available radionuclide bone scans,
For each treatment course, antitumor effects were assessed by CTs, or MRIs, using the PCWG2 criteria,17 and calculated from
the posttherapy PSA changes (PTPC). For ARS inhibitors, “sen- therapy initiation until radiologically confirmed progression
sitive” was defined as a 50% or greater decline from baseline or death owing to any cause within 60 days of stopping treat-
at 12 weeks, but for taxane treatment, 12 weeks or more was ment. Patients without evidence of radiologic progression at
used because the maximal decline may occur later.18 For both the time of last stable scan or end of therapy, whichever oc-
therapies, “resistant” was defined as the failure to achieve a curred later, were right censored. Overall survival was calcu-
jamaoncology.com (Reprinted) JAMA Oncology Published online June 4, 2016 E3
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
Research Original Investigation AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes
Figure 1. Immunofluorescence Staining for AR-V7 Positivity and Nuclear Localization
A AR-V7-positive single CTCs
Composite DAPI CD45 CK AR-V7
B AR-V7-positive CTC clusters
Composite DAPI CD45 CK AR-V7
Panels include DNA (blue), CD45
(leukocyte common antigen) (green),
C AR-V7-positive CK-negative CTCs pan-cytokeratin (red), and AR-V7
(white); CTCs with AR-V7 protein
signal greater than 3.2-fold
background intensity with clear
nuclear localization are scored as
AR-V7–positive and can be seen in (A)
single CTCs, (B) CTC clusters, and (C)
CK-negative CTCs. Cells without the
Composite DAPI CD45 CK AR-V7 requisite AR-V7 protein signal
intensity or localization are classified
as AR-V7–negative and are shown in
D AR-V7-negative single CTCs contrast in (D) single CTCs. Samples
with at least one AR-V7–positive CTC
per 2 slides assayed is scored as
AR-V7 positive in this study. AR-V7
indicates nuclear androgen-receptor
splice variant 7; CKs, cytokeratins;
Composite, all immunofluorescent
channels together; CTCs, circulating
Composite DAPI CD45 CK AR-V7 tumor cells; DAPI,
(4′,6-diamidino-2-phenylindole).
lated from initiation of therapy to death from any cause. for background staining and cross-reactivity. AR-V7–positive
Patients still alive at time of last follow-up were right- and AR-V7–negative mCRPC patient tissue were screened and
censored. included as part of the tissue microarray panel as positive and
negative controls, respectively.
CTC Collection
Blood (7.5 mL) from each participant was collected in Streck CTC Immunofluorescent Staining and Analysis
tubes and processed at MSKCC or shipped to Epic Sciences and Slides created from healthy donor blood samples spiked with
processed within 48 hours. Red blood cells were lysed, and ap- prostate cancer cell line cells (controls), or from mCRPC pa-
proximately 3 million nucleated blood cells were dispensed tient samples, underwent automated immunofluorescent
onto 10-16 glass microscope slides (25.3 mm × 75.3 mm) and staining for DNA, cytokeratins (CK), CD45 (lymphocyte com-
placed at −80°C for long-term storage as previously mon antigen), and AR-V7 (Figure 1), as previously described.15,16
described.15,16,19 Sample processing and testing were con- A rabbit monoclonal anti-AR-V7 antibody (EPR15656; Ab-
ducted in laboratories following Clinical Laboratory Improve- cam) was used for all AR-V7 applications herein described.
ment Amendments (CLIA) regulations. Separate slides from patient samples were tested with a sec-
ond automated immunofluorescent assay, staining for DNA,
Analytical Validation: Specificity of AR-V7 Detection CK, CD45, and the AR N-terminal domain. Up to 2 slides were
As per common practice for verifying the accuracy of diagnos- evaluated per blood sample per assay. Fluorescent scanners
tic-grade antibodies, the AR-V7 antibody was comprehen- and morphology algorithms were used to identify CTCs, CTC
sively tested via tissue microarrays containing malignant, tu- clusters, apoptotic CK-positive cells, and CK-negative CTCs. A
mor-adjacent, and healthy tissue samples (eFigure 2F in the more thorough description of CTC types has been published
Supplement). An independent pathologist scored the samples previously. 16 Clinical laboratory scientists (licensed in
E4 JAMA Oncology Published online June 4, 2016 (Reprinted) jamaoncology.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes Original Investigation Research
Figure 2. Prevalence and Frequency of AR-V7 CTC Positivity by Line of Therapy
A First line (n = 67) B Second line (n = 50)
1024 1024
V7-positive/mL
V7-negative/mL
CTC/mL
CTC/mL
32 32
1 1
AR-V7-positive samples AR-V7-positive samples
Blood Sample Blood Sample
C Third or greater line (n = 74) D Incidence and subclonal contribution of AR-V7-positive CTCs by line of therapy
1024
Line of Tx in
First Second Third or greater
mCRPC setting
(n = 67) (n = 50) (n = 74)
(n samples)
Samples with
AR-V7-positive 2 (3%) 9 (18%) 23 (31%)
CTCs
CTC/mL
32 AR-V7-positive CTCs
in samples with
5.7% 38% 21%
AR-V7-positive
(0.3%-11.2%) (14.3%-100%) (0.5%-100%)
CTCs, %,
median (range)
AR-V7-positive samples
Blood Sample
The burden of intact, nonapoptotic CTCs (CTCs, CTC clusters, CK-negative of therapy in the castration-resistant metastatic setting. (D) A summary chart of
CTCs) per 2 slides is displayed volumetrically normalized to CTC/mL. The AR-V7–positive CTC incidence and subclonal contribution is shown by line of
subpopulation of AR-V7–positive CTCs detected per sample is shown in orange therapy. AR-V7 indicates androgen-receptor splice variant 7 messenger RNA;
and the AR-V7–negative CTCs are represented in blue. Samples are separated by CKs, cytokeratins; CTCs, circulating tumor cells.
those collected prior to (A) first line, (B) second line, and (C) third or greater line
California) conducted final quality control of CTC subpopula- level specificity of AR-V7–positive staining in CTCs was estab-
tion classification and subcellular biomarker localization. lished by staining up to 2 additional slides per sample with a
AR-V7 and AR N-terminal positivity were defined by pro- separate AR N-terminal immunofluorescent assay. Samples
tein expression level above a threshold intensity (eFigure 2 in with at least 1 AR-V7–positive or AR N-terminal–positive CTC
the Supplement). The expression threshold was defined by sig- were considered positive for the respective biomarker
nal quantitation above background relative to AR-V7– (Figure 2).
negative or AR N-terminal-negative control cell lines, as ap-
propriate. Nuclear localization was also required to classify Statistical Analyses
CTCs as AR-V7 positive. Apoptotic CTCs were not included or Patient demographics and clinical characteristics at the time
reported in subsequent analyses, as nuclear fragmentation pre- of blood draw were evaluated by descriptive statistics: over-
cludes protein localization analysis. all, by line of therapy, and by drug administered. Fisher exact
The specificity of AR-V7 protein detection in single pros- and Wilcoxon rank sum tests were used to compare treat-
tate cancer cell line cells spiked into whole blood was corrobo- ment groups for categorical and continuous characteristics, re-
rated by single-cell mRNA analyses (eFigure 2A-D in the Supple- spectively.
ment). The requirement for AR-V7 protein signal localization The association of AR-V7 status (positive or negative) with
in the nucleus is consistent with AR-V7–mediated ligand- resistant or sensitive PTPC was evaluated using univariable lo-
independent proliferation in preclinical models,20,21 AR-V7 lo- gistic regression. Time-to-event outcomes were evaluated
calization in human solid tumor tissue,10,22,23 and previously using the Kaplan-Meier method. Differences in time-to-
validated AR-V7 prognostic tissue scoring criteria.23 Sample- event outcomes between patient samples with AR-V7–
jamaoncology.com (Reprinted) JAMA Oncology Published online June 4, 2016 E5
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
Research Original Investigation AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes
positive and AR-V7–negative CTCs were evaluated using the AR-V7 Is Expressed in Multiple CTC Subtypes
log-rank test. The association of AR-V7 status with time-to- AR-V7 expression was found on a variety of CTC subtypes,
event outcomes was evaluated with hazard ratios (HRs) esti- including traditional CK-positive single CTCs (Figure 1A),
mated from univariable and multivariable Cox proportional CTC clusters (Figure 1B), and CK-negative CTCs (Figure 1C).
hazards regression methods. The pretherapy predictors evalu- Hereafter, all 3 subtypes will collectively be referred to as
ated for the multivariable Cox proportional hazards models in- CTCs.
cluded line of therapy, presence of liver and/or lung metasta-
ses, lactate dehydrogenase levels, patient age, hemoglobin Prevalence and Frequency of AR-V7 CTC Positivity Increases
levels, type of therapy, AR-V7 status, PSA levels, albumin lev- by Line of Therapy
els, and alkaline phosphatase levels. Using a best subset se- The majority of the CTCs detected were AR-V7 negative
lection method based on the global score χ2 statistic, pre- (Figure 2D). AR-V7–positive CTCs were detected in 34
therapy PSA, albumin, and alkaline phosphatase were excluded samples with AR-V7–positive CTC burden ranging from
from the final model. To address unique patients having ex- 0.74/mL to 105/mL (median 2.4/mL), exhibiting a wide
posures to more than 1 therapy, the robust sandwich esti- range of subclonal contribution to total CTCs (median
mate for the covariance matrix was implemented for all Cox [range], 22% [0.3%-100%]) (Figure 2). AR-V7–positive
proportional hazards models to correct for possible underes- CTC detection frequency increased by line of therapy
timation of variance.24 All statistical analyses were 2-sided and (Figure 2A-C), ranging from 3% (2 of 67 samples) prior to
performed at the 5% significance level using SAS version 9.4 first-line therapy, 18% (9 of 50 samples) prior to second-line
statistical software (SAS Institute Inc). therapy, and 31% (23 of 74 samples) prior to third or subse-
quent lines of therapy (Figure 2D; eTable in the Supple-
ment) (P < .001).
Results
Presence of AR-V7–Positive CTCs Predicts
Clinical Characteristics of the Patient Population Posttherapy PSA Change, rPFS, Time Receiving Therapy,
A cohort of 161 patients with mCRPC who received a total of and OS With ARS Inhibitors
193 treatments between September 2012 and March 2015 were Of the 128 samples from patients treated with ARS inhibi-
evaluated. Of these, 130 patients (80.8%) had a single therapy; tors, 47 (37%) showed sensitive and 81 (63%) had resistant
30 (18.6%), 2 therapies (60 samples); and 1 (0.6%), 3 thera- PTPC. None of the 47 with sensitive PTPC had AR-V7–
pies. Patient and treatment characteristics at the time of sample positive CTCs (0%; 95% CI, 0.0%-9.41%). In contrast, 16 of
collection are detailed in the Table. the 81 with resistant PTPC (20%; 95% CI, 12.1%-30.4%) had
AR-V7–positive CTCs prior to therapy (Figure 3A). Three of
Analytical Validation: Specificity of AR-V7 Detection these 16 samples had AR-V7 expression exclusively in
Tissue microarrays containing representative cancer, near- CK-negative CTCs. A subset analysis of the pre-ARS therapy
tumor adjacent tissue, and healthy tissues alongside posi- samples with PSA-resistant profiles (n = 81) showed dra-
tive and negative control samples were used to test assay matically worse OS with pretherapy AR-V7–positive CTCs
specificity in an immunohistochemical format akin to the relative to those without (median, 4.6 months vs not
immunofluorescent CTC assay. An independent pathologist reached; P < .001) (eFigure 4 in the Supplement).
assessed the TMA slides and found no significant off-target Pre-ARS inhibitor samples with AR-V7–positive CTCs were
staining or background signal on the tissue sections. Impor- associated with worse outcomes in all time-to-event mea-
tantly, the tissues on the array most pertinent as potential sures: rPFS (median, 2.3 vs 14.5 months; P < .001), time on
sources of CTCs, such as liver, lymph nodes, and bone, therapy (median, 2.1 vs 6.8 months; P < .001), and OS (me-
showed no appreciable specific or off-target staining, dian, 4.6 months vs not reached; P < .001) (Figure 3; eFigure
indicative of a highly AR-V7–specific antibody (eFigure 2F in 3 in the Supplement). This was not the case for pretaxane
the Supplement). samples, where time on therapy (median, 3.0 vs 3.7 months;
P = .23) and rPFS (median, 5.3 vs 6.6 months; P = .46) were not
Specificity of AR-V7 in Patient Samples significantly different by AR-V7 status. There was a signifi-
Parallel AR assays (AR N-terminal and AR-V7) run on sister cant difference in OS for pretaxane AR-V7–positive vs AR-V7–
slides revealed greater incidence of AR N-terminal-positive negative samples (median, 8.9 vs 19.8 months; P < .001). How-
CTCs relative to AR-V7–positive CTCs (eFigure 2E in the ever, this difference is best interpreted in the multivariable
Supplement), consistent with previous studies on AR-V7 setting.
prevalence in relation to total AR gene product.10,11,20,25 Of
the 193 samples tested, 191 (99%) were evaluable (2 samples Patients Harboring Pretherapy AR-V7–Positive CTCs
were inevaluable for subcellular localization): 72 samples Experience Better OS With Taxanes Than With
(38%) were AR N-terminal positive and AR-V7 negative; ARS Inhibitors After Adjusting for Clinical Measures
4 samples (2%) were AR N-terminal negative and AR-V7 Patients with AR-V7–positive CTCs had longer median sur-
positive; 30 samples (16%) were AR N-terminal positive and vival with taxanes relative to ARS inhibitors (median, 8.9 vs
AR-V7 positive; and 85 samples (44%) were AR N-terminal 4.6 months) even though taxanes tended to be adminis-
negative and AR-V7 negative. tered later (Figure 3A and B) when disease burdens were
E6 JAMA Oncology Published online June 4, 2016 (Reprinted) jamaoncology.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes Original Investigation Research
Figure 3. Presence of AR-V7–Positive CTCs and Response to AR Signaling Inhibitors
A AR signaling inhibitors
50
AR-V7 negative
12-wk PSA Change From Baseline, %
AR-V7 positive
–50
–100
First line (n = 56) Second line (n = 40) Third or greater line (n = 32)
B Taxanes
12-wk or Beyonda PSA Change From Baseline, %
50
a a
–50 a
a a a
aa AR-V7 negative
a AR-V7 positive
a
a
–100
First line (n = 11) Second line (n = 10) Third or greater line (n = 42)
C Overall survival: pre-AR signaling inhibitor samples D Overall survival: pretaxane samples
AR-V7 negative, n = 112 AR-V7 negative, n = 45
100 AR-V7 positive, n = 16 100 AR-V7 positive, n = 18
Waterfall plots, colored by presence
of AR-V7–positive CTCs, show the
75 75 percent PSA change from baseline at
(A) 12 weeks on ARS inhibitors and
(B) 12 weeks (or best decline if after
Survival, %
Survival, %
12 weeks) on taxanes. The dotted
50 50
horizontal line indicates the threshold
HR = 11.45 (95% CI: 5.67-23.82) HR = 3.74 (95% CI: 1.95-7.20)
P <.001 P =.001 for binary PSA response criteria.
Median survival: 4.6 mo vs not reached Median survival: 8.9 mo vs Overall survival is shown, separated
25 25 not reached by AR-V7 status, for samples from
patients receiving (C) ARS inhibitors
or (D) taxanes. AR indicates androgen
0 0 receptor; AR-V7, nuclear
0 10 20 30 40 0 10 20 30 40 androgen-receptor splice variant 7;
Survival, mo Survival, mo CTCs, circulating tumor cells; PSA,
prostate-specific antigen.
greater. To adjust for this imbalance, a Cox proportional haz- inhibitors (HR, 0.24; 95% CI, 0.10-0.57; P = .035), while
ards model incorporating line of therapy, presence of vis- patients who were AR-V7 negative did not (HR, 0.92; 95% CI,
ceral metastases, lactate dehydrogenase, patient age, hemo- 0.44-1.95) (Figure 4B). When applied to AR N-terminal-
globin, therapy type, and AR-V7 status was developed. positive CTCs (inclusive of full-length AR and most
Results showed that AR-V7 status remained the most signifi- splice variants), the same analysis showed a trend
cant factor (P < .001) among all pretherapy clinical measures for improved survival with taxanes relative to ARS inhibitors
(Figure 4A), and that patients who were AR-V7 positive had (HR, 0.59; 95% CI, 0.32-1.08) (eFigure 5 in the Supplement).
more favorable survival times with taxanes relative to ARS However, this effect was not statistically significant (P = .11).
jamaoncology.com (Reprinted) JAMA Oncology Published online June 4, 2016 E7
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
Research Original Investigation AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes
sociation between AR-V7 positivity and PSA response to taxane-
Figure 4. Patients With Pretherapy AR-V7–Positive CTCs and Overall
Survival on Taxanes and/or AR Signaling Inhibitors.
based therapy was observed. Taken together, our results, and
those of others,10-12 suggest that patients in whom AR-V7–
Treatment-Specific Hazards of Death positive CTCs are detected would be better served with an ap-
(Overall Survival)
proved taxane over abiraterone or enzalutamide.
Favors Favors
Source Taxanes AR Therapy A unique aspect of our approach was the focus on the de-
All samples (n = 191) cision points in the management of individual patients in stan-
AR-V7–negative samples (n = 157) dard-of-care settings, where progressive disease required a
AR-V7–positive samples (n = 34) change in systemic therapy with already-approved standard
0.0625 0.125 0.25 0.5 1 2 4
of care drugs. This enabled the assessment of clinical utility:
Hazard Ratio, 95% CI patient benefit for test use vs nonuse, and separately, the harm
associated with selecting an ineffective therapy with poten-
AR-V7 Therapy Interaction: Multivariable Cox PH Model tial toxic effects. This therapy guiding approach is essential to
Comparison Hazard Ratio (95% CI)
inform when and how to use a test in practice and for proper
AR-V7 positive:
Taxane vs AR
0.24 (0.10 to 0.57) evaluation by regulators and third-party payers. Here, the in-
AR-V7 Status
and Therapy AR-V7 negative: cidence and burden of AR-V7–positive CTCs increased by line
0.92 (0.44 to 1.95)
Taxane vs AR of therapy (Figure 2), consistent with previous reports,8,27 sug-
gesting AR-V7 expression as an adapted response to systemic
Multivariable Cox Proportional Hazard Analysis of Predictors of Overall Survival therapy over time.
Effect P Value HR (95% CI)
Of note, in AR-V7–positive samples, a median (range) of
Line of therapy (3rd or later vs 1st or 2nd) .16 1.62 (0.83-3.15)
only 22% (0.3%-100%) of the CTCs were AR-V7–positive. How-
Liver and/or lung metastases pretherapy .003 2.29 (1.11-4.74)
LDH pretherapy (>250 vs ≤250 U/L) .006 2.24 (1.26-4.00) ever, even when only one AR-V7–positive CTC was detected,
Patient age (>65 vs ≤65 years) .007 0.48 (0.28-0.83) only resistant PTPC patterns and shorter rPFS, time on therapy,
Hemoglobin (>12 vs ≤12 g/dL) .007 0.40 (0.19-0.82) and OS were observed on ARS inhibitors. Here, even among
Therapy (taxane vs AR) .84 0.86 (0.49-1.50)
the subset of patients with resistant PTPC, pretherapy AR-V7
AR-V7 status (positive vs negative) <.001 4.15 (1.76-9.77)
AR-V7 (positive) taxane interaction .035 0.24 (0.10-0.57)
positivity further stratified patients with the worst prognosis
when treated with ARS inhibitors (eFigure 4 in the Supple-
Individual covariates were tested for additive predictive power to predict ment). The clinical implication is that, within each line of
outcome using a Cox proportional hazards model. The P values are the result of therapy, once AR-V7–positive cells are detected, the pre-
compensating for the other factors listed. The interaction of therapy and AR-V7 ferred choice of therapy is a taxane rather than an ARS inhibi-
status was further investigated using a multivariable Cox proportional hazards
model. The forest plot shows the hazard ratios and 95% confidence intervals.
tor.
AR indicates androgen receptor; AR-V7, nuclear androgen-receptor splice
variant 7; CTCs, circulating tumor cells.
Conclusions
Discussion The treatment-specific effect for taxane therapy in the set-
ting of AR-V7 positivity was shown when baseline factors as-
The goal of a treatment-specific predictive biomarker is to de- sociated with survival were accounted for in a multivariable
termine patients likely to have a poor outcome to a particular Cox proportional hazards model: patients who had AR-V7–
drug or drug class and simultaneously identify a potentially positive CTCs treated with taxanes had a much lower risk of
effective, already approved alternative therapy. Focusing on death than those on ARS inhibitors (HR, 0.24; 95% CI, 0.10-
the context of use of predicting response to either ARS inhibi- 0.57; P = .035). This level of evidence has not been achieved
tors or taxanes, we used an immunofluorescent AR-V7 pro- with other AR-V7 testing modalities.10,11 Given the magni-
tein assay on CTCs isolated from the blood of men with pro- tude of substratification and outcome specificity of the nuclear-
gressive mCRPC starting a new systemic therapy to evaluate specific AR-V7 protein test in CTCs, a diagnostic-grade test that
the association between detection of nuclear AR-V7–positive informs the selection of ARS inhibitors or taxanes has the po-
CTCs and resistance to ARS inhibitors. Every patient harbor- tential to significantly improve outcomes, by enabling pa-
ing AR-V7–positive CTCs was resistant to treatment with ARS tients to receive treatments to which they are most likely to
inhibitors, including 3 patients with AR-V7 positivity only on respond while avoiding the toxic effects and costs associated
CK-negative CTCs, cells not detectable with EpCAM-based CTC with an ineffective treatment. Prospective trials to validate
capture methods,26 including the previously reported AR-V7 these findings and further elucidate clinical utility are cur-
mRNA transcript detection approaches.10-12 In contrast, no as- rently in development.
ARTICLE INFORMATION affiliations and to add missing table headers to Open Access: This article is published under JAMA
Accepted for Publication: April 21, 2016. eTable 1 in the Supplement. Oncology’s open access model and is free to read on
Published Online: June 4, 2016. the day of publication.
Correction: This article was corrected online
September 29, 2016, for incorrect author doi:10.1001/jamaoncol.2016.1828. Author Affiliations: Genitourinary Oncology
Service, Department of Medicine, Memorial Sloan
E8 JAMA Oncology Published online June 4, 2016 (Reprinted) jamaoncology.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
AR-V7 Expression in Circulating Tumor Cells and Castration-Resistant Prostate Cancer Outcomes Original Investigation Research
Kettering Cancer Center, New York, New York study, and the clinical and laboratory staff at MSKCC 13. Antonarakis ES. Predicting treatment response
(Scher, Schreiber, Bambury, Danila, McLaughlin); and Epic Sciences. We would additionally like to in castration-resistant prostate cancer: could
Department of Medicine, Weill Cornell Medical thank Kyle Botsch, BS, and Connie Landaverde, androgen receptor variant-7 hold the key? Expert
College, New York, New York (Scher, Danila); Epic PhD, from Epic Sciences for technical laboratory Rev Anticancer Ther. 2015;15(2):143-145.
Sciences, La Jolla, California (Lu, Louw, Graf, support for the analyses used in the Supplemental 14. Maughan BL, Antonarakis ES. Clinical relevance
Johnson, Jendrisak, Wahl, Greene, Marrinucci, Data, and Margaret McPartland, BA, an of androgen receptor splice variants in
Dittamore); Body Imaging Service, Department of independently supported editor at MSKCC, for castration-resistant prostate cancer. Curr Treat
Radiology, Memorial Sloan Kettering Cancer Center, editorial assistance. Compensation was not Options Oncol. 2015;16(12):57.
New York, New York (Vargas); Department of received for their contributions and written
Radiology, Weill Cornell Medical College, New York, permission was obtained for their inclusion in the 15. Marrinucci D, Bethel K, Kolatkar A, et al. Fluid
New York (Vargas); Cancer Services, Department of Acknowledgments. biopsy in patients with metastatic prostate,
Medical Oncology, Cork University Hospital, Wilton, pancreatic and breast cancers. Phys Biol. 2012;9(1):
Cork, Ireland (Bambury); Biostatistics Service, REFERENCES 016003.
Author Contributions: Dr Scher had full access to 1. Lissbrant IF, Garmo H, Widmark A, Stattin P. 16. Werner SL, Graf RP, Landers ML, et al.
all of the data in the study and takes responsibility Population-based study on use of chemotherapy in Analytical validation and capabilities of the Epic CTC
for the integrity of the data and the accuracy of the men with castration resistant prostate cancer. Acta platform: Enrichment-free circulating tumour cell
data analysis. Oncol. 2013;52(8):1593-1601. detection and characterization. J Circulating
Study concept and design: Scher, Bambury, Danila, Biomarkers. 2015;4(3). doi:10.5772/60725.
Marrinucci, Fleisher, Dittamore. 2. Templeton AJ, Vera-Badillo FE, Wang L, et al.
Translating clinical trials to clinical practice: 17. Scher HI, Halabi S, Tannock I, et al; Prostate
Acquisition, analysis, or interpretation of data: Cancer Clinical Trials Working Group. Design and
Scher, Lu, Schreiber, Louw, Graf, Vargas, Johnson, outcomes of men with metastatic castration
resistant prostate cancer treated with docetaxel end points of clinical trials for patients with
Jendrisak, Bambury, Danila, McLaughlin, Wahl, progressive prostate cancer and castrate levels of
Greene, Heller, Dittamore. and prednisone in and out of clinical trials. Ann Oncol.
2013;24(12):2972-2977. testosterone: recommendations of the Prostate
Drafting of the manuscript: Scher, Lu, Schreiber, Cancer Clinical Trials Working Group. J Clin Oncol.
Graf, Johnson, Jendrisak, Danila, Dittamore. 3. Schrader AJ, Boegemann M, Ohlmann CH, et al. 2008;26(7):1148-1159.
Critical revision of the manuscript for important Enzalutamide in castration-resistant prostate
intellectual content: Scher, Lu, Schreiber, Louw, cancer patients progressing after docetaxel and 18. Pond GR, Armstrong AJ, Wood BA, et al.
Graf, Vargas, Jendrisak, Bambury, Danila, abiraterone. Eur Urol. 2014;65(1):30-36. Evaluating the value of number of cycles of
McLaughlin, Wahl, Greene, Heller, Marrinucci, docetaxel and prednisone in men with metastatic
4. Scher HI, Morris MJ, Stadler WM, et al. Trial castration-resistant prostate cancer. Eur Urol. 2012;
Fleisher, Dittamore. design and objectives for castration-resistant
Statistical analysis: Louw, Graf, Johnson, Jendrisak, 61(2):363-369.
prostate cancer: updated recommendations from
Heller. the Prostate Cancer Clinical Trials Working Group 3 19. Punnoose EA, Ferraldeschi R, Szafer-Glusman
Obtained funding: Scher. [published online February 22, 2016]. J Clin Oncol. E, et al. PTEN loss in circulating tumour cells
Administrative, technical, or material support: Scher, doi:10.1200/jco.2015.64.2702. correlates with PTEN loss in fresh tumour tissue
Lu, Schreiber, Louw, Graf, Vargas, Bambury, Danila, from castration-resistant prostate cancer patients.
McLaughlin, Marrinucci, Fleisher, Dittamore. 5. Krebs MG, Metcalf RL, Carter L, Brady G, Br J Cancer. 2015;113(8):1225-1233.
Study supervision: Scher, Graf, Vargas, Marrinucci, Blackhall FH, Dive C. Molecular analysis of
circulating tumour cells-biology and biomarkers. 20. Watson PA, Chen YF, Balbas MD, et al.
Fleisher, Dittamore. Constitutively active androgen receptor splice
Assay development: Lu. Nat Rev Clin Oncol. 2014;11(3):129-144.
variants expressed in castration-resistant prostate
Patient sample testing: Lu. 6. Scher HI, Morris MJ, Larson S, Heller G. cancer require full-length androgen receptor. Proc
Conflict of Interest Disclosures: Dr Scher reports Validation and clinical utility of prostate cancer Natl Acad Sci U S A. 2010;107(39):16759-16765.
nonfinancial support from Janssen and Medivation, biomarkers. Nat Rev Clin Oncol. 2013;10(4):225-234.
personal fees from Astellas and Sanofi Aventis, and 21. Sun F, Chen HG, Li W, et al. Androgen receptor
7. Joosse SA, Gorges TM, Pantel K. Biology, splice variant AR3 promotes prostate cancer via
research funding from Janssen Diagnostics, detection, and clinical implications of circulating
Janssen Pharmaceuticals, and Medivation. Dr modulating expression of autocrine/paracrine
tumor cells. EMBO Mol Med. 2014;7(1):1-11. factors. J Biol Chem. 2014;289(3):1529-1539.
Danila reports financial support from Janssen and
Medivation-Astellas. Drs Lu, Graf, Greene, 8. Li Y, Chan SC, Brand LJ, Hwang TH, Silverstein 22. Efstathiou E, Titus M, Wen S, et al. Molecular
Marrinucci; Ms Louw, Ms Johnson; and Mr KA, Dehm SM. Androgen receptor splice variants characterization of enzalutamide-treated bone
Jendrisak, Mr Wahl, and Mr Dittamore are mediate enzalutamide resistance in metastatic castration-resistant prostate cancer. Eur
employees of Epic Sciences. No other disclosures castration-resistant prostate cancer cell lines. Urol. 2015;67(1):53-60.
are reported. Cancer Res. 2013;73(2):483-489.
23. Qu Y, Dai B, Ye D, et al. Constitutively active
Funding/Support: This study was supported by 9. Ware KE, Garcia-Blanco MA, Armstrong AJ, AR-V7 plays an essential role in the development
equal distributions of funds from the National Dehm SM. Biologic and clinical significance of and progression of castration-resistant prostate
Institutes of Health (grant no. NIH/NCI P50- androgen receptor variants in castration resistant cancer. Sci Rep. 2015;5:7654.
CA92629 SPORE in Prostate Cancer; and NIH/NCI prostate cancer. Endocr Relat Cancer. 2014;21(4):
Cancer Center Support Grant P30 CA008748); the T87-T103. 24. Lin DY, Wei LJ. The robust inference for the Cox
Department of Defense Prostate Cancer Research proportional hazards model. J Am Stat Assoc. 1989;
10. Antonarakis ES, Lu C, Wang H, et al. AR-V7 and 84(408):1074-1078.
Program (grants PC071610 and PC121111), the resistance to enzalutamide and abiraterone in
Prostate Cancer Foundation Challenge Award, and prostate cancer. N Engl J Med. 2014;371(11):1028- 25. Nakazawa M, Lu C, Chen Y, et al. Serial
the David H. Koch Fund for Prostate Cancer 1038. blood-based analysis of AR-V7 in men with
Research. advanced prostate cancer. Ann Oncol. 2015;26(9):
Role of the Funder/Sponsor: The funders/ 11. Antonarakis ES, Lu C, Luber B, et al. Androgen 1859-1865.
sponsors had no role in the design and conduct of receptor splice variant 7 and efficacy of taxane
chemotherapy in patients with metastatic 26. Yap TA, Lorente D, Omlin A, Olmos D, de Bono
the study; collection, management, analysis, and JS. Circulating tumor cells: a multifunctional
interpretation of the data; preparation, review, or castration-resistant prostate cancer. JAMA Oncol.
2015;1(5):582-591. biomarker. Clin Cancer Res. 2014;20(10):2553-2568.
approval of the manuscript; and decision to submit
the manuscript for publication. 12. Onstenk W, Sieuwerts AM, Kraan J, et al. 27. Guo Z, Yang X, Sun F, et al. A novel androgen
Previous Presentation: This study was presented Efficacy of cabazitaxel in castration-resistant receptor splice variant is up-regulated during
at the 2016 American Society of Clinical Oncology prostate cancer is independent of the presence of prostate cancer progression and promotes
(ASCO) meeting; June 4, 2016; Chicago, Illinois. AR-V7 in circulating tumor cells. Eur Urol. 2015;68 androgen depletion-resistant growth. Cancer Res.
Additional Contributions: We would like to thank (6):939-945. 2009;69(6):2305-2313.
the patients and their families taking part in this
jamaoncology.com (Reprinted) JAMA Oncology Published online June 4, 2016 E9
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 10/08/2016
You might also like
- Asima-Bisha 2012Document8 pagesAsima-Bisha 2012Bisha UzirNo ratings yet
- First-Line Treatment of Metastatic Renal Cell Carcinoma: A Systematic Review and Network Meta-AnalysisDocument8 pagesFirst-Line Treatment of Metastatic Renal Cell Carcinoma: A Systematic Review and Network Meta-AnalysisDr. Alexandre SatoNo ratings yet
- First-Line Crizotinib Versus Chemotherapy in ALK-Positive Lung CancerDocument11 pagesFirst-Line Crizotinib Versus Chemotherapy in ALK-Positive Lung CancerRitam JoarderNo ratings yet
- Systemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal CancerDocument8 pagesSystemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal Canceralberto cabelloNo ratings yet
- Nejmoa 1606220Document10 pagesNejmoa 1606220Jay TiwariNo ratings yet
- JurnalDocument6 pagesJurnalNur AnindyaNo ratings yet
- ANZ Journal of Surgery - 2021 - Yang - Outcomes of Patients With Metastatic Cutaneous Squamous Cell Carcinoma To The Axilla PDFDocument8 pagesANZ Journal of Surgery - 2021 - Yang - Outcomes of Patients With Metastatic Cutaneous Squamous Cell Carcinoma To The Axilla PDFRong LiuNo ratings yet
- Clinical Features and Outcomes of Patients With Colorectal Cancers Harboring NRAS MutationsDocument8 pagesClinical Features and Outcomes of Patients With Colorectal Cancers Harboring NRAS MutationsAde Tan RezaNo ratings yet
- KRAS Status As A Predictor of Chemotherapy Activity in Patients With MCRCDocument7 pagesKRAS Status As A Predictor of Chemotherapy Activity in Patients With MCRCIvoBarrosNo ratings yet
- Who Are The Best Candidates For DecompressiveDocument8 pagesWho Are The Best Candidates For DecompressiverecolenciNo ratings yet
- D'Amico Risk ClassificationDocument6 pagesD'Amico Risk ClassificationStirNo ratings yet
- J Juro 2017 04 086Document19 pagesJ Juro 2017 04 086nimaelhajjiNo ratings yet
- Mrna Vaccine cv9103 and cv9104 For The Treatment of Prostate CancerDocument8 pagesMrna Vaccine cv9103 and cv9104 For The Treatment of Prostate Cancerapi-675909478No ratings yet
- MDV 161Document12 pagesMDV 161rasika bhatNo ratings yet
- Yoon 2018Document9 pagesYoon 2018Muhammad Yusuf HanifNo ratings yet
- Diagnosisofrenalcell Carcinoma: A Clinician'S PerspectiveDocument6 pagesDiagnosisofrenalcell Carcinoma: A Clinician'S PerspectiveGangsar DamaiNo ratings yet
- A Genomic StrategyDocument11 pagesA Genomic StrategyAmirahShalehaNo ratings yet
- Swog 8794Document7 pagesSwog 8794yingming zhuNo ratings yet
- 10 1093@icvts@ivz140Document8 pages10 1093@icvts@ivz140PEDRO JESuS GUERRA CANCHARINo ratings yet
- Detection of Mutations in EGFR in Circulating Lung-Cancer Cells.Document12 pagesDetection of Mutations in EGFR in Circulating Lung-Cancer Cells.Joonseok ParkNo ratings yet
- Tumor Markers in Clinical Practice: General Principles and GuidelinesDocument8 pagesTumor Markers in Clinical Practice: General Principles and GuidelinesNurmalia SariNo ratings yet
- 2014 Kemeny Kras Influence Recurrence PatternDocument15 pages2014 Kemeny Kras Influence Recurrence Patternnasifahsankhan4No ratings yet
- Baek 2017Document10 pagesBaek 2017witaNo ratings yet
- 1 s2.0 S1051044322011903 MainDocument30 pages1 s2.0 S1051044322011903 MainEsmaeel Jafargholi RangrazNo ratings yet
- Tca 12 2161Document9 pagesTca 12 2161hafidisara05No ratings yet
- An Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesDocument9 pagesAn Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesBobNo ratings yet
- Outcomes After Stereotactic Body Radiotherapy or Radiofrequency Ablation For Hepatocellular CarcinomaDocument10 pagesOutcomes After Stereotactic Body Radiotherapy or Radiofrequency Ablation For Hepatocellular CarcinomaRaul Matute MartinNo ratings yet
- Lutetium 177-PSMA 617 For MetastaticDocument13 pagesLutetium 177-PSMA 617 For MetastaticpaulobriosNo ratings yet
- Circulating Tumor DNA As A Therapy Response Marker in Metastatic Colorectal CancerDocument2 pagesCirculating Tumor DNA As A Therapy Response Marker in Metastatic Colorectal CancerStephanie YaungNo ratings yet
- Rocha 2014Document5 pagesRocha 2014pakemainmainNo ratings yet
- Efficacy of Trans-Arterial Radio Embolization With Yattrium-90 For Hepatic MalignanciesDocument8 pagesEfficacy of Trans-Arterial Radio Embolization With Yattrium-90 For Hepatic MalignanciesIJAR JOURNALNo ratings yet
- Articulo Sesion 2 DMII 2023 Karapetis2008Document9 pagesArticulo Sesion 2 DMII 2023 Karapetis2008abcd 1234No ratings yet
- Enzalutamide in Metastatic Prostate Cancer Before ChemotherapyDocument10 pagesEnzalutamide in Metastatic Prostate Cancer Before ChemotherapyRanda HalfianNo ratings yet
- Cytogenetic Profile Predicts Prognosis of Patients With Clear Cell Renal Cell CarcinomaDocument8 pagesCytogenetic Profile Predicts Prognosis of Patients With Clear Cell Renal Cell CarcinomaRivan 21No ratings yet
- Clinical Nutrition: ESPEN GuidelineDocument38 pagesClinical Nutrition: ESPEN GuidelineDana MuresanNo ratings yet
- Reply To E.A. Rakha Et Al: Lajos PusztaiDocument2 pagesReply To E.A. Rakha Et Al: Lajos PusztaiNeil GriggNo ratings yet
- 1 s2.0 S1470204522007835 Main PDFDocument11 pages1 s2.0 S1470204522007835 Main PDFOncología CdsNo ratings yet
- Analysis of The Risk Factors of Untransplantable Recurrence After Primary Curative Resection For Patients With Hepatocellular CarcinomaDocument8 pagesAnalysis of The Risk Factors of Untransplantable Recurrence After Primary Curative Resection For Patients With Hepatocellular CarcinomaJoão Gabriel Ferreira ArgondizziNo ratings yet
- Autologous Stem Cell TransplantDocument7 pagesAutologous Stem Cell TransplantgauravsinghalNo ratings yet
- Psa Persistentemente Elevado Post P RadicalDocument20 pagesPsa Persistentemente Elevado Post P RadicalBenjamin HuamanchauNo ratings yet
- Contemporary Management of Metastatic Colorectal Cancer: A Precision Medicine ApproachFrom EverandContemporary Management of Metastatic Colorectal Cancer: A Precision Medicine ApproachAslam EjazNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 17: OncologyFrom EverandComplementary and Alternative Medical Lab Testing Part 17: OncologyNo ratings yet
- Acs 06 02 167Document8 pagesAcs 06 02 167MixalisKaplanisNo ratings yet
- Paper 1Document11 pagesPaper 1บอส เลิศเกียรติรัชตะNo ratings yet
- CrizotinibDocument10 pagesCrizotinibLuca StamerraNo ratings yet
- Sabcs 2014 AllabstractsDocument1,508 pagesSabcs 2014 Allabstractsrajesh4189No ratings yet
- Radicals RTDocument9 pagesRadicals RTyingming zhuNo ratings yet
- Rectal Cancer: International Perspectives on Multimodality ManagementFrom EverandRectal Cancer: International Perspectives on Multimodality ManagementBrian G. CzitoNo ratings yet
- MainDocument8 pagesMainIoana CucuNo ratings yet
- Provenge 2Document12 pagesProvenge 2api-675909478No ratings yet
- Cancer Stem Cells: Targeting the Roots of Cancer, Seeds of Metastasis, and Sources of Therapy ResistanceFrom EverandCancer Stem Cells: Targeting the Roots of Cancer, Seeds of Metastasis, and Sources of Therapy ResistanceHuiping LiuNo ratings yet
- NRG Consensus Contouring Guidelines For Postop emCA + CervixDocument12 pagesNRG Consensus Contouring Guidelines For Postop emCA + Cervixgermanfutbol7No ratings yet
- Original ArticleDocument6 pagesOriginal ArticleClaudinete SouzaNo ratings yet
- Treatment of The Elderly When Cure Is The GoalDocument8 pagesTreatment of The Elderly When Cure Is The GoalCatia AraujoNo ratings yet
- Dalton-Clin Cancer Res-2017 (Wilgus-Group Paper)Document14 pagesDalton-Clin Cancer Res-2017 (Wilgus-Group Paper)MounikaGoruganthuNo ratings yet
- Management of Urologic Cancer: Focal Therapy and Tissue PreservationFrom EverandManagement of Urologic Cancer: Focal Therapy and Tissue PreservationNo ratings yet
- Homeopathic ImmunizationDocument53 pagesHomeopathic Immunizationalex100% (2)
- 9650-0301-01 Rev. MDocument48 pages9650-0301-01 Rev. MCarlos AndresNo ratings yet
- Case Study UrtiDocument9 pagesCase Study UrtiRonica GonzagaNo ratings yet
- Abilify Dosing GuideDocument2 pagesAbilify Dosing GuidemtassyNo ratings yet
- 09 ITLS PretestDocument6 pages09 ITLS PretestArlanosaurus100% (2)
- UNIT-I: General Pharmacology As Per Syllabus Unit-1, Chapter A (Half)Document18 pagesUNIT-I: General Pharmacology As Per Syllabus Unit-1, Chapter A (Half)Atthapu ThirupathaiahNo ratings yet
- Clinical EnzymologyDocument23 pagesClinical EnzymologyKishore KaranNo ratings yet
- Preterm Neonate VS AssessmentDocument10 pagesPreterm Neonate VS AssessmentggggangNo ratings yet
- ANC ModuleDocument103 pagesANC ModulePreeti ChouhanNo ratings yet
- Makalah Leigh Disease by Boys KDocument6 pagesMakalah Leigh Disease by Boys KAzizul HakimNo ratings yet
- Standard Operating Procedure (Biochemistry - Diasys RESPONS - 910)Document17 pagesStandard Operating Procedure (Biochemistry - Diasys RESPONS - 910)Aniruddha ChatterjeeNo ratings yet
- Philippine College of Science and Technology College of NursingDocument21 pagesPhilippine College of Science and Technology College of NursingAijem RyanNo ratings yet
- Pulsion Work Booklet: Bucarest Hemodynamic Monitoring WorkshopDocument43 pagesPulsion Work Booklet: Bucarest Hemodynamic Monitoring WorkshopghuoiNo ratings yet
- Nama: Khoirus Viestaria NIM: 135130101111035 Kelas: 2013/CDocument2 pagesNama: Khoirus Viestaria NIM: 135130101111035 Kelas: 2013/CDina SahmirandaNo ratings yet
- Hematology Unit: Complete Blood Count (CBC)Document2 pagesHematology Unit: Complete Blood Count (CBC)Rasha ElbannaNo ratings yet
- Shared Psychotic Disorder - NCBIDocument8 pagesShared Psychotic Disorder - NCBI5KevNo ratings yet
- 32 Oet Reading Summary 2.0-697-717Document21 pages32 Oet Reading Summary 2.0-697-717Santhus100% (7)
- NCP Ko BabyDocument3 pagesNCP Ko BabyDaniel ApostolNo ratings yet
- Dulcolax Stool Softener Supp (Docusate Sodium)Document2 pagesDulcolax Stool Softener Supp (Docusate Sodium)ENo ratings yet
- Gastric GavageDocument3 pagesGastric GavageRico Delgado of WorldbexNo ratings yet
- Narrative Report ContentsDocument15 pagesNarrative Report ContentsGladie Ann Dela RosaNo ratings yet
- HEPATOMEGALY CaseDocument5 pagesHEPATOMEGALY CaseKanwaljeet SinghNo ratings yet
- Pedia ADCONDocument24 pagesPedia ADCONRaul MangrobangNo ratings yet
- 7.down SyndromeDocument15 pages7.down SyndromeGadarNo ratings yet
- Anesthesia ALL PDFDocument195 pagesAnesthesia ALL PDFYasir RasoolNo ratings yet
- Needle CricothyroidotomyDocument9 pagesNeedle Cricothyroidotomyhatem alsrour100% (2)
- Antenatal Care Services: by DR - Chinedu Ibeh Thursday, 16 APRIL 2015Document81 pagesAntenatal Care Services: by DR - Chinedu Ibeh Thursday, 16 APRIL 2015SehaRizaNo ratings yet
- Pmls Finals ReviewerDocument72 pagesPmls Finals ReviewerIsiwjsbnwhshz Hshshzhbshs100% (1)
- Case Presentation: - Vuppu BhavaniDocument53 pagesCase Presentation: - Vuppu BhavaniLohith Kumar MenchuNo ratings yet
- A Leading Surgical Gastroenterologist in Hyderabad Dr. Dinesh ReddyDocument4 pagesA Leading Surgical Gastroenterologist in Hyderabad Dr. Dinesh Reddydrdineshreddy02No ratings yet