Professional Documents
Culture Documents
NIH Anticoag Jan 2022
Uploaded by
Andrea BonitoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NIH Anticoag Jan 2022
Uploaded by
Andrea BonitoCopyright:
Available Formats
The COVID-19 Treatment Guidelines Panel’s Statement on
Anticoagulation in Hospitalized Patients With COVID-19
Last Updated: January 5, 2022
Background
COVID-19 has been associated with inflammation and a prothrombotic state accompanied by increases
in fibrinogen and D-dimer.1,2 In some studies, elevations in these markers have been associated
with worse clinical outcomes.3,4 Hospitalized patients with COVID-19 are at high risk for venous
thromboembolism (VTE).5 At a minimum, hospitalized COVID-19 patients should receive prophylactic
doses of anticoagulants, such as low molecular weight heparin (LMWH) or unfractionated heparin, for
the duration of their hospitalization.
Recommendations
Based on the collective data from randomized controlled trials on the use of anticoagulation in patients
with COVID-19, the COVID-19 Treatment Guidelines Panel (the Panel) provides the following
recommendations.
For Hospitalized, Nonpregnant Adults Who Require Low-Flow Oxygen and Are Not
Receiving Intensive Care Unit Level of Care
• The Panel recommends using therapeutic-dose heparin for patients who have a D-dimer above
the upper limit of normal (ULN), require low-flow oxygen, and have no increased bleeding risk
(CIIa). LMWH is preferred over unfractionated heparin.
• Based on clinical trial exclusion criteria, contraindications for therapeutic anticoagulation
for COVID-19 due to an increased bleeding risk are as follows: platelet count <50 x 109/L,
hemoglobin <8 g/dL, need for dual antiplatelet therapy, known bleeding within the last 30 days
requiring an emergency room visit or hospitalization, known history of a bleeding disorder, or
an inherited or active acquired bleeding disorder.
• In patients without a VTE who are started on therapeutic-dose heparin, treatment should continue
for 14 days or until hospital discharge, whichever comes first.
• The Panel recommends using prophylactic-dose heparin (LMWH or unfractionated heparin) for
patients who are not administered therapeutic heparin unless a contraindication exists (AIIb).
• The Panel recommends against the use of therapeutic-dose oral anticoagulants for VTE
prophylaxis or prevention of COVID-19 progression in hospitalized patients, except in a clinical
trial (AIIa).
For Hospitalized, Nonpregnant Adults Who Are Receiving Intensive Care Unit Level of Care
(Including Patients Who Are Receiving High-Flow Oxygen)
• The Panel recommends using prophylactic-dose heparin as VTE prophylaxis unless a
contraindication exists (AI).
• The Panel recommends against the use of intermediate-dose (e.g., enoxaparin 1 mg/kg daily)
and therapeutic-dose anticoagulation for VTE prophylaxis, except in a clinical trial (BI).
• For patients who start on therapeutic-dose heparin while on low-flow oxygen due to COVID-19
and then transfer to the intensive care unit (ICU), the Panel recommends switching from
therapeutic to prophylactic-dose heparin unless a VTE is confirmed (BIII).
COVID-19 Treatment Guidelines 12
Downloaded from https://www.covid19treatmentguidelines.nih.gov/ on 1/11/2022
For Hospitalized Pregnant Adults
• The Panel recommends using prophylactic-dose anticoagulation for pregnant patients
hospitalized for manifestations of COVID-19 unless otherwise contraindicated (see below) (BIII).
• Because pregnant patients have not been included in most clinical trials evaluating therapeutic
anticoagulation in the setting of COVID-19, there is currently insufficient evidence to recommend
either for or against therapeutic anticoagulation for pregnant patients with COVID-19 in the
absence of a known VTE.2
Rationale
Several randomized controlled trials have evaluated the role of therapeutic doses of heparin in reducing
VTE events or mortality in patients hospitalized for COVID-19. In the ICU setting, these studies
showed that therapeutic heparin did not reduce mortality but may have a higher risk of bleeding events;
therefore, this approach is not recommended.6
Three open-label randomized controlled trials (a large multiplatform trial and the smaller RAPID and
HEP-COVID trials) compared therapeutic doses of heparin to prophylactic or intermediate doses of the
anticoagulant in selected hospitalized patients who did not require ICU care. The entry criteria for these
studies varied, but typically they included need for supplemental oxygen, elevated D-dimer level, and
no risk of major bleeding event. In the larger multiplatform trial, therapeutic heparin showed an increase
in organ support-free days but no difference in mortality or length of hospitalization compared to
prophylactic heparin.7 The RAPID trial enrolled patients with elevated D-dimer levels and hypoxemia.
The patients were randomized to receive therapeutic or prophylactic doses of heparin. There was no
statistically significant difference between the arms for the primary outcome, a composite of ICU
admission, noninvasive or invasive ventilation, or death at Day 28, but therapeutic heparin reduced
mortality at 28 days, a secondary outcome.8 The HEP-COVID trial enrolled patients who required
supplemental oxygen and had a D-dimer >4 times ULN or a sepsis-induced coagulopathy score of ≥4.
The occurrence of the primary outcome of VTE, arterial thromboembolism, or all-cause death at Day 30
was significantly lower in the therapeutic LMWH arm than in the prophylactic LMWH arm, but there
was no difference in mortality at Day 30 between the arms.9 Results from smaller randomized trials,
single-center studies, and observational studies have also been published.
Based on the available study data, the Panel recommends using therapeutic-dose heparin for patients
who have a D-dimer above the ULN, require low-flow oxygen, and have no increased bleeding risk
(CIIa). The rating reflects the fact that, although the 3 randomized controlled trials showed benefit of
therapeutic heparin in hospitalized patients, their inclusion criteria and beneficial outcomes differed.
The RAPID and HEP-COVID trials each required a specified D-dimer elevation for enrollment, but the
multiplatform trial did not. Beneficial outcomes ranged from reduction in the primary outcome of organ
support-free days without a mortality benefit in the multiplatform trial, to no change in the primary
composite outcome of ICU admission, noninvasive or invasive ventilation, or death at Day 28, but a
reduction in the secondary outcome of mortality at 28 days in the RAPID trial.8 The HEP-COVID trial
showed improvement in the composite outcome of thrombosis and death. Event rates were significantly
higher in HEP-COVID than in the other trials, highlighting the difference in their inclusion criteria. In
addition, it should be noted that <20% of screened patients enrolled into the studies; therefore, these
findings may not be generalizable to all hospitalized patients with COVID-19.
References
1. Han H, Yang L, Liu R, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection.
Clin Chem Lab Med. 2020;58(7):1116-1120. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32172226.
COVID-19 Treatment Guidelines 13
Downloaded from https://www.covid19treatmentguidelines.nih.gov/ on 1/11/2022
2. Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers,
and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352-2371. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/32201335.
3. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med.
2020;382(18):1708-1720. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32109013.
4. Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe
coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094-1099. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/32220112.
5. Nopp S, Moik F, Jilma B, Pabinger I, Ay C. Risk of venous thromboembolism in patients with COVID-19: a
systematic review and meta-analysis. Res Pract Thromb Haemost. 2020;4(7):1178-1191. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/33043231.
6. REMAP-CAP Investigators, ACTIV-4a Investigators, ATTACC Investigators, et al. Therapeutic
anticoagulation with heparin in critically ill patients with COVID-19. N Engl J Med. 2021;385(9):777-789.
Available at: https://www.ncbi.nlm.nih.gov/pubmed/34351722.
7. ATTACC Investigators, ACTIV-4a Investigators, REMAP-CAP Investigators, et al. Therapeutic
anticoagulation with heparin in noncritically ill patients with COVID-19. N Engl J Med. 2021;385(9):790-802.
Available at: https://www.ncbi.nlm.nih.gov/pubmed/34351721.
8. Sholzberg M, Tang GH, Rahhal H, et al. Effectiveness of therapeutic heparin versus prophylactic heparin
on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with COVID-19
admitted to hospital: RAPID randomised clinical trial. BMJ. 2021;375:n2400. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/34649864.
9. Spyropoulos AC, Goldin M, Giannis D, et al. Efficacy and safety of therapeutic-dose heparin vs standard
prophylactic or intermediate-dose heparins for thromboprophylaxis in high-risk hospitalized patients with
COVID-19: the HEP-COVID randomized clinical trial. JAMA Intern Med. 2021;181(12):1612-1620.
Available at: https://www.ncbi.nlm.nih.gov/pubmed/34617959.
COVID-19 Treatment Guidelines 14
Downloaded from https://www.covid19treatmentguidelines.nih.gov/ on 1/11/2022
You might also like
- Jamainternal Wahid 2021 Ic 210027 1638550230.78177Document2 pagesJamainternal Wahid 2021 Ic 210027 1638550230.78177Zoltán BaloghNo ratings yet
- Role of Anticoagulant in Treatment Protocol of COVID 19 PatientsDocument6 pagesRole of Anticoagulant in Treatment Protocol of COVID 19 PatientsBasma ElshazlyNo ratings yet
- Antithrombotic Treatment GuidelinesDocument9 pagesAntithrombotic Treatment GuidelinesAnh NguyenNo ratings yet
- COVID-19 Treatments What's In, What's OutDocument7 pagesCOVID-19 Treatments What's In, What's OutMir Shakeel AhmedNo ratings yet
- Anticoagulant Treatment Is Associated With Decreased Mortality in Severe Coronavirus DiseaseDocument15 pagesAnticoagulant Treatment Is Associated With Decreased Mortality in Severe Coronavirus DiseaseAnonymous ps1JIBNo ratings yet
- If Ppih Covid 19 RecommendationsDocument6 pagesIf Ppih Covid 19 RecommendationsrehankhankhanNo ratings yet
- Covid y CoagulaciónDocument6 pagesCovid y CoagulaciónMaría JoséNo ratings yet
- Anticoagulant TreatmentDocument6 pagesAnticoagulant TreatmentMonica AngNo ratings yet
- Real World Experiences Pirfenidone and Nintedanib Are Effective and Well Tolerated Treatments For Idiopathic Pulmonary FibrosisDocument12 pagesReal World Experiences Pirfenidone and Nintedanib Are Effective and Well Tolerated Treatments For Idiopathic Pulmonary FibrosismaleticjNo ratings yet
- Covid + Anticoagulant (Autosaved)Document21 pagesCovid + Anticoagulant (Autosaved)Dr. Surya Abadi KristyoadiNo ratings yet
- 2020 06 22 20137273v1 Full PDFDocument24 pages2020 06 22 20137273v1 Full PDFeswarNo ratings yet
- Surviving Covid-19 With Heparin?: EditorialDocument2 pagesSurviving Covid-19 With Heparin?: EditorialTuan HaiNo ratings yet
- Therapeutic Anticoagulation With Heparin in Noncritically Ill Patients With Covid-19Document13 pagesTherapeutic Anticoagulation With Heparin in Noncritically Ill Patients With Covid-19Tuan HaiNo ratings yet
- Covid 19 TreatmentDocument2 pagesCovid 19 TreatmentGio Tamaño BalisiNo ratings yet
- Meta 8Document9 pagesMeta 8Jonathan AiresNo ratings yet
- Treatment of COVID-19 Antiviral and Pharmacotherapy 29abril2020Document5 pagesTreatment of COVID-19 Antiviral and Pharmacotherapy 29abril2020Luis LopezNo ratings yet
- 2020.05.13.20094193v1.full 2Document22 pages2020.05.13.20094193v1.full 2Rodrigo BressanNo ratings yet
- ACTION TRIAL - Therapeutic Versus Prophylactic Anticoagulation For PatientsDocument22 pagesACTION TRIAL - Therapeutic Versus Prophylactic Anticoagulation For PatientsSheerazNo ratings yet
- PIIS0007091221004359Document7 pagesPIIS0007091221004359luisfernandoamaya89No ratings yet
- HazanEtal210707 Efficacy-Ivermectin-MultidrugTherapy-Covid TRMT IVM CV19Document26 pagesHazanEtal210707 Efficacy-Ivermectin-MultidrugTherapy-Covid TRMT IVM CV19R NobleNo ratings yet
- Acut40 WarfarinDocument6 pagesAcut40 WarfarinAncaNo ratings yet
- Hematology Recommendations and Dosing Guidelines During COVID-19Document9 pagesHematology Recommendations and Dosing Guidelines During COVID-19diellzaNo ratings yet
- Modifications in Drug Adherence After Switch To Fixed Dose Combination of Perindopril Amlodipine in Clinical Practice Results of A Large ScaleDocument8 pagesModifications in Drug Adherence After Switch To Fixed Dose Combination of Perindopril Amlodipine in Clinical Practice Results of A Large ScalenembutalNo ratings yet
- Hepb y RTX PDFDocument3 pagesHepb y RTX PDFYeli VeMeNo ratings yet
- COVID 19 Drug Therapy - 2020 05 07 PDFDocument23 pagesCOVID 19 Drug Therapy - 2020 05 07 PDFDavid MorgNo ratings yet
- An EU Programme of COVID-19 Convalescent PlasmaDocument14 pagesAn EU Programme of COVID-19 Convalescent Plasmaazizk83No ratings yet
- Barnes2020 Article ThromboembolismAndAnticoagulanDocument10 pagesBarnes2020 Article ThromboembolismAndAnticoagulanRirin Efsa JutiaNo ratings yet
- COVID 19 in ChildrenDocument16 pagesCOVID 19 in ChildrenANo ratings yet
- WetcuppingDocument10 pagesWetcuppingputriaprili521No ratings yet
- 5 Recent Trials in Stress Ulcer ProphylaxisDocument6 pages5 Recent Trials in Stress Ulcer ProphylaxisCharan Teja Reddy AvulaNo ratings yet
- Effectiveness of Ivermectin As Add-On Therapy in COVID-19 ManagementDocument12 pagesEffectiveness of Ivermectin As Add-On Therapy in COVID-19 Managementprashant kumarNo ratings yet
- Tung, Ying, Chang, Nifedipin Generik Vs Nifedipin BrandDocument9 pagesTung, Ying, Chang, Nifedipin Generik Vs Nifedipin Brandhasan andrianNo ratings yet
- COVID-19 Drug Therapy: What's Been UpdatedDocument24 pagesCOVID-19 Drug Therapy: What's Been Updatedkathy colmenaresNo ratings yet
- 2009hetrase CCMDocument12 pages2009hetrase CCMgiseladelarosa2006No ratings yet
- Jurnal Anestesi 3Document8 pagesJurnal Anestesi 3Rizky Frida Monica TomasilaNo ratings yet
- Role of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy LestariDocument32 pagesRole of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy Lestaridesy lestariNo ratings yet
- Karyana - Plasma Convalescent Therapy in COVID-19 - 29 Apr 2021Document33 pagesKaryana - Plasma Convalescent Therapy in COVID-19 - 29 Apr 2021iq_dianaNo ratings yet
- Daily Interruption of Sedation in Patients Treated With Mechanical VentilationDocument4 pagesDaily Interruption of Sedation in Patients Treated With Mechanical VentilationMark_LiGx_8269No ratings yet
- Hydrocortisone, Vitamin C, and Thiamine For The Treatment of Severe Sepsis and Septic ShockDocument10 pagesHydrocortisone, Vitamin C, and Thiamine For The Treatment of Severe Sepsis and Septic Shockmmmaw mmNo ratings yet
- 1 s2.0 S0007091217542075 MainDocument11 pages1 s2.0 S0007091217542075 Maineny_sumaini65No ratings yet
- COVID-19.QUICK SUMMARY OF Drug Treatment For COVIDDocument3 pagesCOVID-19.QUICK SUMMARY OF Drug Treatment For COVIDmuhammed barznjiNo ratings yet
- Antibiotics 11 01664Document15 pagesAntibiotics 11 01664Ottofianus Hewick KalangiNo ratings yet
- Meta 1Document21 pagesMeta 1Jonathan AiresNo ratings yet
- Ayerbe2020 Article TheAssociationBetweenTreatmentDocument4 pagesAyerbe2020 Article TheAssociationBetweenTreatmentNando RezaNo ratings yet
- G-4 Presentation DoneDocument24 pagesG-4 Presentation DoneAbdulrhman 123No ratings yet
- Transfusión en Pacientes PediatricosDocument14 pagesTransfusión en Pacientes PediatricosAndrea Abigail ChacónNo ratings yet
- EBN - Typhoid Fever FinalDocument5 pagesEBN - Typhoid Fever FinalHeart CarambasNo ratings yet
- Outcome of Conservative Therapy in COVID-19 in Pts Presenting With GI BleedingDocument7 pagesOutcome of Conservative Therapy in COVID-19 in Pts Presenting With GI BleedingTAUSEEFA JANNo ratings yet
- Guidelines On The Use of Intravenous Immune Globulin For Hematologic ConditionsDocument48 pagesGuidelines On The Use of Intravenous Immune Globulin For Hematologic ConditionssarahulfaaNo ratings yet
- COVID-19 Drug Therapy: What's Been UpdatedDocument25 pagesCOVID-19 Drug Therapy: What's Been Updatedtordo22No ratings yet
- Marik 2016Document10 pagesMarik 2016PedroNo ratings yet
- Vitamina C, Tiamina, Corticoides and Shock SepticoDocument10 pagesVitamina C, Tiamina, Corticoides and Shock SepticoNorvingNo ratings yet
- 2021 Remap-Cap - Activ-4a - Attacc Covid Severes Heparinoptherapie NejmDocument13 pages2021 Remap-Cap - Activ-4a - Attacc Covid Severes Heparinoptherapie Nejmcarb0ne14rNo ratings yet
- JHMI Clinical Guidance For Available Pharmacologic Therapies For COVID-19Document13 pagesJHMI Clinical Guidance For Available Pharmacologic Therapies For COVID-19bemnetNo ratings yet
- s12887 018 1215 7Document14 pagess12887 018 1215 7Zwinglie SandagNo ratings yet
- PIIS2666634020300064Document47 pagesPIIS2666634020300064Erick RomeroNo ratings yet
- Jama Connors 2021 Oi 210109 1633723843.57239-1Document10 pagesJama Connors 2021 Oi 210109 1633723843.57239-1silviaNo ratings yet
- COVID-19 Antiviral and Pharmacotherapy Information: PreferentialDocument6 pagesCOVID-19 Antiviral and Pharmacotherapy Information: Preferentialmrosyidn0% (1)
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Anglo American - Belt Conveyor Design CriteriaDocument19 pagesAnglo American - Belt Conveyor Design CriteriaIgor San Martín Peñaloza0% (1)
- Emergency War Surgery Nato HandbookDocument384 pagesEmergency War Surgery Nato Handbookboubiyou100% (1)
- Theoretical Background: Theories Relevance To The Study SourcesDocument3 pagesTheoretical Background: Theories Relevance To The Study SourcesAdelfa Mae BerdonNo ratings yet
- Practice Test: Ielts UsaDocument11 pagesPractice Test: Ielts UsajoseNo ratings yet
- Responsibility Accounting Practice ProblemDocument4 pagesResponsibility Accounting Practice ProblemBeomiNo ratings yet
- MPSI OverviewDocument15 pagesMPSI OverviewZaqee AlvaNo ratings yet
- Allison Burke Adime 4Document8 pagesAllison Burke Adime 4api-317577095No ratings yet
- LivingScience CBSE CompanionDocument56 pagesLivingScience CBSE Companionnjlenovo95% (19)
- Canfield FairDocument3 pagesCanfield Fairapi-546463844No ratings yet
- The Mystique of The Dominant WomanDocument8 pagesThe Mystique of The Dominant WomanDorothy HaydenNo ratings yet
- HandbookDocument6 pagesHandbookAryan SinghNo ratings yet
- Government of Tamilnadu Directorate of Legal Studies: Inter-Collegeiate State Level Moot Court Competition-2022Document30 pagesGovernment of Tamilnadu Directorate of Legal Studies: Inter-Collegeiate State Level Moot Court Competition-2022Divya SrinimmiNo ratings yet
- Contact Point ContoursDocument69 pagesContact Point ContourstarekrabiNo ratings yet
- Kernberg, O. (1991) - A Contemporary Reading of On Narcissism in Freud's On Narcissism An IntroductionDocument10 pagesKernberg, O. (1991) - A Contemporary Reading of On Narcissism in Freud's On Narcissism An IntroductionAngelina Anastasova100% (2)
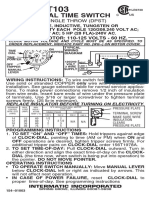
- T103 InstructionsDocument1 pageT103 Instructionsjtcool74No ratings yet
- Purpose in Life Is A Robust Protective Factor of Reported Cognitive Decline Among Late Middle-Aged Adults: The Emory Healthy Aging StudyDocument8 pagesPurpose in Life Is A Robust Protective Factor of Reported Cognitive Decline Among Late Middle-Aged Adults: The Emory Healthy Aging StudyRaúl AñariNo ratings yet
- Evaluation of Whole-Body Vibration (WBV) On Ready Mixed Concrete Truck DriversDocument8 pagesEvaluation of Whole-Body Vibration (WBV) On Ready Mixed Concrete Truck DriversmariaNo ratings yet
- Sulzer Centrifugal Pumps - Basic OperationDocument26 pagesSulzer Centrifugal Pumps - Basic OperationMarcelo PerettiNo ratings yet
- Culturally Safe Classroom Context PDFDocument2 pagesCulturally Safe Classroom Context PDFdcleveland1706No ratings yet
- 9 - 1 H Wood Cabinet Spec Options NelDocument8 pages9 - 1 H Wood Cabinet Spec Options NelinformalitybyusNo ratings yet
- Giardiasis PDFDocument14 pagesGiardiasis PDFSaad Motawéa0% (1)
- Eric CHE326 JournalpptDocument33 pagesEric CHE326 JournalpptRugi Vicente RubiNo ratings yet
- Windows Perfectpath: Promise Multipath DriverDocument3 pagesWindows Perfectpath: Promise Multipath Driverpd904526No ratings yet
- Rifle Threat Performance Matrix: SeriesDocument1 pageRifle Threat Performance Matrix: SeriesKuhnNo ratings yet
- Respiratory Examination - Protected 1Document4 pagesRespiratory Examination - Protected 1anirudh811100% (1)
- Fitness Program: Save On Health Club Memberships, Exercise Equipment and More!Document1 pageFitness Program: Save On Health Club Memberships, Exercise Equipment and More!KALAI TIFYNo ratings yet
- MLT IMLT Content Guideline 6-14Document4 pagesMLT IMLT Content Guideline 6-14Arif ShaikhNo ratings yet
- Mediclinic Weekly Progress Report No 29Document27 pagesMediclinic Weekly Progress Report No 29Julius Ceasar SanorjoNo ratings yet
- Digital Habits Across Generations: Before ReadingDocument3 pagesDigital Habits Across Generations: Before ReadingSharina RamallahNo ratings yet
- Chemsheets AS 006 (Electron Arrangement)Document27 pagesChemsheets AS 006 (Electron Arrangement)moiz427No ratings yet