Professional Documents
Culture Documents
1455 Cumulative Dose and Length of File
Uploaded by
barrientosgerman321Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1455 Cumulative Dose and Length of File
Uploaded by
barrientosgerman321Copyright:
Available Formats
ARP Rheumatology 2023;2:148-154
ORIGINAL ARTICLES
Cumulative dose and length of methotrexate
treatment were not shown to be predictors of hepatic
fibrosis by elastography - a monocentric cohort study
Pinheiro FO1,2*, Gaspar R3*, Fernandes BM1, Peixoto A3, Macedo G2,3, Brito I2,4
ABSTRACT
Objective: Methotrexate is used in several inflammatory diseases, such as rheumatoid arthritis (RA), spondyloar-
thritis (SpA) or inflammatory bowel disease (IBD). There has been some controversy regarding methotrexate liver
toxicity, especially since the use of newer techniques. We aim to evaluate the prevalence of liver injury in methotrex-
ate-treated patients with inflammatory diseases.
Methods: We performed a cross-sectional study where consecutive patients diagnosed with RA, SpA or IBD,
treated with methotrexate, were submitted to liver elastography. The cutoff for fibrosis was ≥7.1 kPa. Comparisons
between groups were evaluated using chi-square, t test and Mann-Whitney U test. Correlations were made between
continuous variables using Spearman correlation. Logistic regression was performed to determine predictors of
fibrosis.
Results: A total of 101 patients were included, 60 (59.4%) females, aged 46.2±12.6 years. Eleven patients (10.9%)
had fibrosis, with a median score of 4.8 (4.1-5.9) kPa. Patients with fibrosis had higher rates of daily alcohol con-
sumption (63.6% vs 31.1%, p=0.045). Methotrexate exposure time (OR 1.00, 95% CI 1.00-1.00, p=0.549) and
cumulative dose (OR 1.00, 95% CI 1.00-1.00, p=0.629) were shown not to be predictors of fibrosis, unlike alcohol
(OR 3.88, 95% CI 1.05-14.32, p=0.042). In multivariable logistic regression analysis, methotrexate cumulative and
exposure times were not predictors of significant fibrosis, even when adjusted for alcohol consumption.
Conclusions: In this study, we found that fibrosis detected on hepatic elastography was not associated with meth-
otrexate, unlike alcohol. Therefore, it is of paramount importance to redefine risk factors for liver toxicity in patients
with inflammatory diseases under treatment with methotrexate.
Keywords: Spondylarthritis; Rheumatoid arthritis; Liver fibrosis; Methotrexate.
INTRODUCTION League Against Rheumatism (EULAR) and the American
College of Rheumatology (ACR) in early and established
Methotrexate (MTX) is a folate antagonist that inhibits rheumatoid arthritis, being the cornerstone of treatment1
dihydrofolate reductase and reduces intracellular stores and it may be used in patients with peripheral articular
of folic acid, affecting its role in the synthesis of purine involvement in spondyloarthritis3, 4. It has also a well-
and pyrimidine1. Due to its potent anti-inflammatory ef- known side effect profile, ranging from mild effects such
fect, it is one of the first-line treatments used for inflam- as stomatitis, fatigue, or diarrhea to more serious adverse
matory diseases, such as rheumatoid arthritis (RA), pso- effects, namely myelosuppression, pulmonary fibrosis,
riasis or inflammatory bowel disease (IBD)2. Although it risk of lymphoma or hepatotoxicity1, 5.
has limited effect in the treatment of Crohn´s disease, it is Hepatotoxicity has been one of the major drawbacks
recommended as first line therapy by both the European for the use of methotrexate. The first studies in treat-
ed psoriatic patients reported a rate of almost 50% of
1
Rheumatology Department, Centro Hospitalar Universitário de São hepatotoxicity with fibrosis being the consequence of
João, Porto, Portugal; 2Medicine Department, Faculty of Medicine, liver toxicity6,7. Some risk factors described were obe-
University of Porto, Porto, Portugal; 3Gastroenterology Department,
Centro Hospitalar Universitário de São João, Porto, Portugal; sity, high alcohol intake, diabetes, and metabolic syn-
4
Pediatric and Young Adult Rheumatology Unit, Centro Hospitalar drome8. However, most recent literature reports signifi-
Universitário de São João, Porto, Portugal
cant lower rates of liver injury. A study in patients with
* These authors contributed equally
IBD showed comparable incidence of liver toxicity with
Submitted: 25/11/2022
Accepted: 19/01/2023 MTX and thiopurines9. Two studies in patients with RA
Correspondence to: Filipe Oliveira Pinheiro
reported a very low risk of fibrosis in patients treated
E-mail: filipe.pinheiro92@gmail.com with MTX and a more recent one showed no increased
148 www.arprheumatology.com • The official Journal of the Portuguese Society of Rheumatology
Oliveira Pinheiro F et al.
risk of liver fibrosis10-12. The first guidelines addressing matology and Gastroenterology Departments of a ter-
liver toxicity of methotrexate were from Dermatology, tiary center, with a clinical diagnosis of RA, SpA (both
suggesting liver biopsy after every 1500 mg of cumu- performed by Rheumatologists) or IBD (performed by
lative dose13. More recently, Rheumatology guidelines Gastroenterologists), treated with methotrexate, were
proposed liver function tests (LFT) and albumin screen- submitted to liver elastography and LFT. Patients were
ing every 1-3 months, recommending drug discontin- included if they had a clinical diagnosis of RA, SpA
uation when levels rise more than 3 times the upper or IBD, in the absence of a previous liver disease. We
limit of normal, thereby limiting liver biopsy to cases collected demographic, clinical and laboratory data,
of persistently abnormal liver function tests after drug including alcohol intake, body mass index (BMI), dia-
discontinuation2, 14. However, it is well known that liver betes mellitus and dyslipidemia, ALT, AST, gamma-glu-
fibrosis cannot be predicted by LFT, as patients with tamyl transferase (GGT), alkaline phosphatase (ALP),
cirrhosis can have normal LFT15, so other methods of direct and indirect bilirubin (Brb), cholesterol and tri-
identifying liver toxicity are needed. glycerides, C-reactive protein (CRP) and erythrocyte
Liver biopsy is considered the gold-standard for liver sedimentation rate (ESR), hemoglobin A1c (HbA1c),
injury and liver fibrosis evaluation; however, it is an in- Homeostasis Model Assessment (HOMA), RA disease
vasive procedure with inherent risks, and it is not prac- activity measured by Disease Activity Score 28 4 vari-
tical as a monitoring tool for consecutive evaluations2. ables using C-reactive protein (DAS284V-CRP), length
Therefore, non-invasive evaluation has recently merged of treatment and methotrexate cumulative dose. We
as a very useful alternative, allowing serial evaluations additionally evaluated concurrent therapies, namely
for patients under MTX treatment for several years. non-steroidal anti-inflammatory drugs (NSAIDs), glu-
Some scores employed in clinical practice are very cocorticoids, other conventional synthetic disease-mod-
useful to calculate the risk of liver fibrosis and were ifying drugs (csDMARD) and biological DMARDs (bD-
mainly validated for hepatitis C and non-alcoholic fat- MARDs). We calculated APRI and FIB-4. The protocol
ty liver disease (NAFLD). Aspartate aminotransferase was approved by the Ethics Committee of our center.
(AST) to Platelet Ratio Index (APRI) can be easily ob- The study was run in accordance with the principles
tained using AST and platelet count but its ability to of the Declaration of Helsinki as amended in Fortaleza
predict liver fibrosis is only moderate16. The Fibrosis-4 (2013). Written informed consent was obtained from
(FIB-4) index is another score validated in chronic liver each study participant.
disease as hepatitis C and NAFLD that is based on age,
AST, alanine aminotransferase (ALT) and platelet count Transient elastography
that has also been used to predict liver fibrosis, with Liver stiffness measure (LSM) was performed on the
a study revealing promising results in patients under patients in the supine position, with at least 6 hours
methotrexate in RA17. of fasting, using FibroScan 502 (Echosens®) device,
Transient elastography (TE) is one of the main tools by the same certified Gastroenterologist. LSM was
for liver fibrosis staging in patients with liver disease18. performed with M or XL probes in accordance with the
It was first described and validated in Hepatitis C pa- thickness of subcutaneous fat (XL probe was used when
tients but nowadays it is widespread used in liver dis- subcutaneous thickness was > 2.5 cm). For each patient
ease. TE consists of a transducer which emits mild am- we performed 10 valid measures, and the average value
plitude and low frequency vibrations, inducing a shear was recorded. Quality criteria applied for LSM included
wave that propagates throughout the liver19. Several a success rate ≥60% and an interquartile range <30% of
studies have already evaluated TE performance in liver the median. The cut-off considered for the presence of
fibrosis assessment in RA patients under MTX, and a fibrosis was ≥7.1 kPa, found to be a reliable cut-off for
more recent one showed better results when compared fibrosis in the literature20, 21.
to APRI or FIB-4 score1.
The aim of our study was to evaluate the prevalence Statistical Analysis
and development of liver injury in methotrexate-treat- Statistical analysis was carried out by using SPSS version
ed patients with inflammatory diseases. 25. We used Shapiro-Wilk test and histogram analysis for
assessment of normality. Comparisons between groups
(fibrosis versus non- fibrosis) were evaluated using chi-
METHODS square, t test and Mann-Whitney U test. Spearman’s
correlation was used to assess associations between two
Study design or more continuous variables. Logistic regression was
We performed a cross-sectional, observational study performed to determine predictors of fibrosis. Statistical
where consecutive adult patients followed at the Rheu- analysis was performed at a significance level of 5%.
The official Journal of the Portuguese Society of Rheumatology • www.arprheumatology.com 149
Liver fibrosis in patients under methotrexate
RESULTS
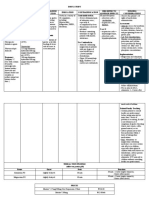
Table I. Clinical and laboratory data of the
recruited patients
A total of 101 patients were included in this study. Pa-
tient demographic and clinical data are described in Ta- Total (n=101)
ble I. Sixty patients (59.4%) were female, 49 (48.5%) Female gender – n (%) 60 (59.4)
had RA, 17 (16.8%) SpA and 35 (34.7%) IBD, with Age, years – mean (SD) 53.9 (12.1)
median disease duration of 11.5 years, median MTX Body mass index, kg/m2 – mean (SD) 25.9 (4.6)
length of treatment 204 weeks and median MTX cu- Disease – n (%)
mulative dose of 2385 mg. Thirty-five patients reported Rheumatoid arthritis 49 (48.5)
daily alcohol consumption. Of all the patients included, Inflammatory bowel disease 35 (34.7)
Spondyloarthritis 17 (16.8)
11 (10.9%) had fibrosis, with a median score of 4.8
(4.1-5.9) kPa. Patients with fibrosis were comparable Disease duration, years – median (IQR) 11.5 (5-18)
to patients without fibrosis concerning age, gender, Daily alcohol consumption – n (%) 35 (34.7)
disease and disease duration, diabetes mellitus, dys- Diabetes mellitus – n (%) 10 (9.9)
lipidemia, BMI, liver enzymes, HbA1c, HOMA, APRI, Dyslipidemia – n (%) 30 (29.7)
and FIB4 (Table II). However, patients with fibrosis re-
Current methotrexate dose, mg/week – median
vealed higher daily alcohol consumption rates (63.6% (IQR)
15 (11.3-25)
vs 31.1%, p=0.045). It should be noted that 25 patients Duration of methotrexate treatment, weeks –
(24.8%) had a daily alcohol intake lower than 30g/day, 204 (72-416)
median (IQR)
while the remainder 10 (9.9%) had an alcohol intake Cumulative methotrexate dose, mg – median
2385 (940-5200)
higher than 30g/day, with no differences in elastogra- (IQR)
phy scores. There were no statistically significant differ- NSAIDs – n (%) 36 (35.6)
ences regarding MTX length of treatment or cumulative Glucocorticoids – n (%) 33 (32.7)
dose. Other csDMARDs – n (%) 6 (5.9)
We performed a correlation analysis to assess the bDMARD – n (%) 28 (27.7)
correlation between the MTX length of treatment and
Erythrocyte sedimentation rate, mm/1st h – me-
elastography results, as well as the correlation between dian (IQR)
12 (5.3-20)
MTX cumulative dose and elastography results; we C-reactive protein, mg/L – median (IQR) 4.15 (1.95-6.53)
found no significant correlations as well (Figure 1).
DAS284V-CRP – mean (SD) 2.4 (1.2)
We assessed predictors of fibrosis by univariable
Albumin, g/L – mean (SD) 42.0 (2.4)
logistic regression analysis. Alcohol intake (OR 3.88,
Aspartate transaminase (AST), UI/L – median
95% CI 1.05-14.32, p=0.042) was the only predictor (IQR)
25 (19.3-26.8)
of fibrosis; indeed, MTX length of treatment (OR 1.00,
Alanine transaminase (ALT), UI/L – median
95% CI 1.00-1.00, p=0.549) and MTX cumulative dose (IQR)
24.5 (16.8-30.8)
(OR 1.00, 95% CI 1.00-1.00, p=0.629) were shown Glucose, mg/dL – median (IQR) 92 (86.3-96.8)
not to be predictors of fibrosis (Table III). We then
Hemoglobin A1C (HbA1c), % – mean (SD) 5.5 (0.6)
performed a multivariable logistic regression analysis
Homeostasis Model Assessment (HOMA) – me-
including these 3 multivariable, in which MTX length dian (IQR)
2.4 (2.0-3.9)
of treatment and MTX cumulative dose were not pre-
AST/ALT ratio – median (IQR) 1.0 (0.8-1.3)
dictors of significant fibrosis when adjusted for alcohol
AST to Platelet Ratio Index (APRI) – median
consumption; alcohol was found to be the only inde- (IQR)
0.3 (0.2-0.4)
pendent predictor of significant fibrosis, when adjusted Fibrosis-4 (FIB-4) Index for Liver Fibrosis – me-
for MTX length of treatment and MTX cumulative dose 1.1 (0.8-1.5)
dian (IQR)
(OR 5.49, 95% CI 1.12-26.98, p=0.036). Fibroscan score – median (IQR) 4.8 (4.1-5.9)
Regarding the limited size of the fibrosis patients’ Significant fibrosis – n (%) 11 (10.9)
group, we performed another analysis by splitting the
groups at the median, in order to obtain groups with bDMARD – biological disease-modifying drugs; csDMARD – conventional
synthetic disease-modifying drugs; DAS284V-CRP – Disease Activity Score
an equivalent number of patients – ≤4.8kPa (n=55) and 28 4 variables using C-reactive protein; IQR – Interquartile range; NSAIDS –
>4.8 kPa (n=46). Both groups were similar regarding Non-steroidal anti-inflammatory drugs; SD – Standard deviation.
age, gender, disease and disease duration, diabetes mel-
litus, dyslipidemia, BMI, liver enzymes, HbA1c, HOMA,
APRI and FIB4, while >4.8kPa patients had again high-
er rates of alcohol intake (45.7% vs 25.5%, p=0.034);
again, no differences were found regarding MTX length
150 www.arprheumatology.com • The official Journal of the Portuguese Society of Rheumatology
Oliveira Pinheiro F et al.
Table II. Comparison between patients with and without fibrosis.
No (n=90) Fibrosis (n=11) p
Female gender – n (%) 53 (58.9) 7 (63.3) 0.516
Age, years – mean (SD) 53.8 (11.6) 54.7 (16.1) 0.821
Body mass index, kg/m2 – mean (SD) 26.0 (4.6) 25.7 (5.2) 0.884
Disease – n (%)
44 (48.9)
Rheumatoid arthritis 5 (45.5)
30 (33.3) 0.507
Inflammatory bowel disease 5 (45.5)
16 (17.8)
Spondyloarthritis 1 (9.1)
Disease duration, years – median (IQR) 10 (5-16.5) 18 (10-19) 0.052
Daily alcohol consumption – n (%) 28 (31.1) 7 (63.6) 0.045
Diabetes mellitus – n (%) 8 (8.9) 2 (18.2) 0.298
Dyslipidemia – n (%) 25 (27.8) 5 (45.5) 0.295
Current methotrexate dose, mg/week – median (IQR) 15 (12.5-20) 20 (15-25) 0.755
Duration of methotrexate treatment, weeks – median (IQR) 250 (187.5-566) 200 (87.5-668) 0.922
Cumulative methotrexate dose, mg – median (IQR) 3360 (1630-6770) 2225 (1697.5-10985) 0.794
NSAIDs – n (%) 33 (36.7) 3 (27.3) 0.742
Glucocorticoids – n (%) 29 (32.2) 4 (36.4) 0.746
Other csDMARDs – n (%) 5 (5.6) 1 (9.1) 0.509
bDMARD – n (%) 25 (27.8) 3 (27.3) 0.640
Erythrocyte sedimentation rate, mm/1st h – median (IQR) 14 (8-20) 16.5 (10.5-41) 0.380
C-reactive protein, mg/L – median (IQR) 5.55 (2.1-14.0) 2.50 (2.6-5.0) 0.930
Albumin, g/L – mean (SD) 41.5 (2.9) 41.8 (3.3) 0.483
Aspartate transaminase (AST), UI/L – median (IQR) 24 (20-27) 22.5 (16.3-46) 0.540
Alanine transaminase (ALT), UI/L – median (IQR) 23 (16-29) 28 (9.5-48) 0.125
Glucose, mg/dL – median (IQR) 91 (85-98.8) 84 (75-84) 0.331
Hemoglobin A1C (HbA1c), % – mean (SD) 5.5 (0.5) 5.6 (1.3) 0.551
Homeostasis Model Assessment (HOMA) – median (IQR) 2.4 (1.7-3.3) 2.5 (2.2-2.5) 0.555
AST/ALT ratio – median (IQR) 1.1 (0.9-1.3) 1.0 (0.8-1.7) 0.675
AST to Platelet Ratio Index (APRI) – median (IQR) 0.3 (0.2-0.4) 0.3 (0.2-0.5) 0.804
Fibrosis-4 (FIB-4) Index for Liver Fibrosis – median (IQR) 1.1 (0.8-1.5) 1.1 (0.7-2.0) 0.877
bDMARD – biological disease-modifying drugs; csDMARD – conventional synthetic disease-modifying drugs; IQR – Interquartile range; NSAIDS – Non-steroidal
anti-inflammatory drugs; SD – Standard deviation.
of treatment and cumulative dose (Figure 2). activity were not found in a very significant percentage
Univariable logistic regression analysis revealed that of the other diseases studied, we performed a sub anal-
MTX length of treatment (OR 1.00, 95% CI 1.00-1.00, ysis to try to find an association between disease activi-
p=0.607) and MTX cumulative dose (OR 1.00, 95% CI ty and elastography scores. Patients with RA presented
1.00-1.00, p=0.376) were not predictors of elastogra- with a mean DAS284V-CRP disease activity of 2.4±1.2,
phy score >4.8kPa as well. and we found no differences between disease activity
Since patients with RA represent the majority of pa- assessed by DAS284V-CRP and the presence of liver fi-
tients included (n=49), and objective data on disease brosis, regardless of the cutoff used (4.8 or 7.1 kPa).
The official Journal of the Portuguese Society of Rheumatology • www.arprheumatology.com 151
Liver fibrosis in patients under methotrexate
A
the development of liver fibrosis. The aim of this study
20000 rho=0,033, p=0,745 was to provide a comprehensive assessment of metho-
trexate-induced hepatotoxicity in patients with chronic
Methotrexate cumulative dose (mg)
15000 inflammatory diseases. The main finding of this study
is that, apparently, there is no association between the
methotrexate dose and the presence of hepatic fibrosis
10000
in patients with inflammatory rheumatic diseases (RA
and SpA) and inflammatory bowel disease. Other stud-
5000 ies have evaluated methotrexate-related hepatotoxicity
through elevation of liver enzymes9 as well as, more
0
recently, liver elastography10-12 and even liver biopsy13.
2,5 5,0 7,5 10,0 12,5 15,0
kPa
This study used hepatic elastography and evaluated
other comorbidities, hepatic enzyme levels, and tools
that may allow the assessment of fibrosis.
B Our patients were on methotrexate at a median cu-
1200 mulative dose of 2385 mg, for a median treatment pe-
Duration of methotrexate
riod of 204 weeks. This is in line with other studies
1000 rho=0,059, p=0,555
published on this topic, with cumulative doses between
(weeks)
8000
1200 and 4900mg22,23. As previously described, despite
being a frequently reported problem, more recent stud-
600 ies have shown lower rates of hepatotoxicity in relation
with methotrexate dosing. Liver fibrosis detected by
400
transient elastography has been described in a recent
200 systematic literature review as ranging from 10.9-40%,
using the same cutoff (7.1kPa)18. Other studies have re-
0
2,5 5,0 7,5 10,0 12,5 15,0 ported higher presence of fibrosis ≥7.1kPa using sim-
kPa
ilar methods (43.9%)24. The authors reported higher
Figure 1. Correlation between elastography scores and (A) BMI and metabolic syndrome prevalence as a possible
methotrexate cumulative dose; (B) duration of methotrexate. explanation for those results25. We performed multi-
ple statistical evaluations, based on the fibrosis score,
with different cut offs, having observed a trend towards
Likewise, there was no statistically significant correla- the presence of higher fibrosis scores in patients with
tion between elastography scores, and RA disease activ- longer length of treatment and/or cumulative dose of
ity measured by DAS284V-CRP (rho 0.235, p=0.145). methotrexate, although with no statistical and clini-
Regarding the tools we used to estimate the presence cal significance. The results obtained in the regression
of liver fibrosis, we performed another correlation anal- models make it quite clear that there is no significant
ysis with elastography scores, however, we found that association between the cumulative dose and the time
there were not any significant correlations with those of exposure to methotrexate and the presence of hepat-
indices and elastography scores – APRI (rho -0.049, ic fibrosis, while we identified alcohol consumption as
p=0.626), and FIB-4 (rho 0.033, p=0.817). a determining factor in this process.
Previous studies have reported obesity, high alcohol
DISCUSSION intake, diabetes and metabolic syndrome as factors that
increase the risk of hepatotoxicity8,18,26. In this study,
Methotrexate is frequently used therapy, effective in pa- the only significant association was obtained with al-
tients with RA, SpA and IBD, but it has been linked to cohol consumption. In fact, this association is a very
Table III. Univariable logistic regression analysis for significant fibrosis.
Odds ratio
P-value
(95% confidence interval)
Alcohol intake 0.042 3.88 (1.05-14.32)
Duration of methotrexate treatment 0.549 1.00 (1.00-1.00)
Cumulative methotrexate dose 0.629 1.00 (1.00-1.00)
152 www.arprheumatology.com • The official Journal of the Portuguese Society of Rheumatology
Oliveira Pinheiro F et al.
p=0.633 used to estimate the risk of liver fibrosis, such as APRI
and FIB-416,17 which were evaluated in all patients, re-
A gardless of the diagnosis. In our study, however, it is in-
Methotrexate cumulative dose (mg)
20000
* teresting to verify that the APRI and FIB-4 values were
*
not different in the groups with and without significant
15000
*
fibrosis, and overall, there were no significant correla-
tions between those measures and elastography scores.
10000 Therefore, in our evaluation, those were not good pre-
dictors of liver fibrosis.
5000 In this study, liver biopsy, the most reliable test to
assess the presence of fibrosis, was not used. However,
0 the results seem to contradict the idea that liver biopsy
≤4,8kPA >4,8kPA
kPa
is necessary in patients under methotrexate therapy if
p=0.710
we only consider the cumulative dose of the drug, as
recommended, for example, by Dermatology13.
There are several limitations of this study. First, it is a
B
1200 retrospective study, so compliance cannot be accurately
guaranteed and there may have been some discrepancy
Duration of methotrexate
1000
related to the calculated cumulative dose of methotrex-
800 ate values; similarly, there is insufficient information
(weeks)
600
about how liver function test changed the management
of patients specifically regarding the methotrexate dose.
400
The non-inclusion of a control group (patients not ex-
200 posed to methotrexate) prevented us from performing
0
another type of evaluation, namely the comparison
≤4,8kPA >4,8kPA
between taking methotrexate and not taking it, in pa-
kPa
tients with chronic inflammatory diseases. Despite be-
ing something original in this study, the sub analysis
Figure 2. Distribution of methotrexate cumulative dose (A) in patients with rheumatoid arthritis alone is limited,
and duration (B) according to the presence of elastography
since disease activity was only evaluated on the date
scores with 4.8 kPa cutoff.
of the global assessment for the study, not allowing us
to know how disease activity had been in the previous
months and/or years. Since the patients did not have
relevant conclusion of this study, since it was obtained to be escalated to other immunosuppressive therapies,
even after adjusting for the variables studied, such as we believe that we have obtained a more homogeneous
the cumulative dose and the time of exposure to meth- group in terms of global disease activity, nonetheless
otrexate. this is still a limitation. Another possible limitation in
This study is almost unique, to our knowledge, due the interpretation of these results is the fact that the
to the inclusion of patients with three different pathol- patients were on MTX for a median duration of only
ogies in terms of pathophysiology, in a collaboration 204 weeks, with a median dose of 2385mg. Although,
between Rheumatology and Gastroenterology, in which in general, the results do not differ much from what
methotrexate use is done in a different way. Others have we observed in our population, the authors believe that
reported no significant incidence of MTX-induced hep- further studies, with the inclusion of a larger sample
atotoxicity in patients with RA10, 12 and only one study and containing patients under treatment with metho-
has reported the use of elastography to evaluate hepato- trexate for a longer time, may be very important, so
toxicity in psoriasis, RA and IBD, where patients under that more robust conclusions can be reached on this
MTX treatment and patients not treated with metho- relevant topic.
trexate were included11. We analyzed patients with RA, In conclusion, the authors highlight that, in this
which was the group with higher number of patients, study, no association was identified between fibrosis
and we found that the presence of higher disease activ- detected on elastography and cumulative dose or meth-
ity was also not associated with the presence of hepatic otrexate exposure time. We found an association, how-
fibrosis. ever, with alcohol consumption. As such, it is crucial
In our study, unlike other studies, in addition to elas- to redefine risk factors for liver toxicity in patients with
tography, we additionally decided to include markers inflammatory diseases under methotrexate therapy.
The official Journal of the Portuguese Society of Rheumatology • www.arprheumatology.com 153
Liver fibrosis in patients under methotrexate
REFERENCES 14. Visser, K., et al., Multinational evidence-based recommenda-
1. Olsson-White, D.A., et al., Assessment of liver fibrosis mark- tions for the use of methotrexate in rheumatic disorders with a
ers in people with rheumatoid arthritis on methotrexate. Intern focus on rheumatoid arthritis: integrating systematic literature
Med J, 2022. 52(4): p. 566-573. research and expert opinion of a broad international panel of
2. Arena, U., et al., Liver stiffness correlates with methotrexate cu- rheumatologists in the 3E Initiative. Ann Rheum Dis, 2009.
mulative dose in patients with rheumatoid arthritis. Dig Liver 68(7): p. 1086-93.
Dis, 2012. 44(2): p. 149-53. 15. Ahmed, Z., et al., Liver function tests in identifying patients with
3. Gossec, L., et al., European League Against Rheumatism (EU- liver disease. Clin Exp Gastroenterol, 2018. 11: p. 301-307.
LAR) recommendations for the management of psoriatic arthri- 16. Loaeza-del-Castillo, A., et al., AST to platelet ratio index (APRI)
tis with pharmacological therapies: 2015 update. Ann Rheum for the noninvasive evaluation of liver fibrosis. Ann Hepatol,
Dis, 2016. 75(3): p. 499-510. 2008. 7(4): p. 350-7.
4. van der Heijde, D., et al., 2016 update of the ASAS-EULAR 17. Miyata, M., et al., Validation of the fibrosis-4 (FIB-4) index in the
management recommendations for axial spondyloarthritis. Ann diagnosis of liver disease of rheumatoid arthritis patients treated
Rheum Dis, 2017. 76(6): p. 978-991. with methotrexate. Mod Rheumatol, 2019. 29(6): p. 936-942.
5. Kalb, R.E., et al., Methotrexate and psoriasis: consensus confer- 18. Marsh, R.L., et al., Utility and Limitations of Transient Elastog-
ence. J Am Acad Dermatol, 2011. 64(6): p. 1179. raphy to Monitor Hepatic Steatosis, Hepatic Fibrosis, and Meth-
6. Nyfors, A., Liver biopsies from psoriatics related to methotrex- otrexate-Associated Hepatic Disease in Psoriasis: A Systematic
ate therapy. 3. Findings in post-methotrexate liver biopsies from Review. J Clin Aesthet Dermatol, 2021. 14(12): p. 24-28.
160 psoriatics. Acta Pathol Microbiol Scand A, 1977. 85(4): p. 19. Castera, L., et al., Prospective comparison of transient elastog-
511-8. raphy, Fibrotest, APRI, and liver biopsy for the assessment of
7. Zachariae, H., E. Grunnet, and H. Sogaard, Liver biopsy in fibrosis in chronic hepatitis C. Gastroenterology, 2005. 128(2):
methotrexate-treated psoriatics-a re-evalution. Acta Derm Ve- p. 343-50.
nereol, 1975. 55(4): p. 291-6. 20. Boursier, J., et al., Determination of reliability criteria for liver
8. Rouhi, A., et al., Prevalence and risk factors for liver fibrosis stiffness evaluation by transient elastography. Hepatology, 2013.
detected by transient elastography or shear wave elastography in 57(3): p. 1182-91.
inflammatory arthritis: a systematic review. Clin Exp Rheumatol, 21. Clinical Application of Transient Elastography in the Diagnosis
2017. 35(6): p. 1029-1036. of Liver Fibrosis: an Expert Panel Review and Opinion. J Clin
9. Khan, N., et al., Incidence of liver toxicity in inflammatory bow- Transl Hepatol, 2014. 2(2): p. 110-6.
el disease patients treated with methotrexate: a meta-analysis of 22. Bray, A.P., et al., Liver fibrosis screening for patients with psoria-
clinical trials. Inflamm Bowel Dis, 2012. 18(2): p. 359-67. sis taking methotrexate: a cross-sectional study comparing tran-
10. Park, S.H., J.Y. Choe, and S.K. Kim, Assessment of liver fibrosis sient elastography and liver biopsy. Br J Dermatol, 2012. 166(5):
by transient elastography in rheumatoid arthritis patients treated p. 1125-7.
with methotrexate. Joint Bone Spine, 2010. 77(6): p. 588-92. 23. Barbero-Villares, A., et al., Evaluation of liver fibrosis by tran-
11. Laharie, D., et al., Assessment of liver fibrosis with transient elas- sient elastography (Fibroscan®) in patients with inflammatory
tography and FibroTest in patients treated with methotrexate for bowel disease treated with methotrexate: a multicentric trial.
chronic inflammatory diseases: a case-control study. J Hepatol, Scand J Gastroenterol, 2012. 47(5): p. 575-9.
2010. 53(6): p. 1035-40. 24. Koch, K., Psoriasis, transient elastography and methotrexate:
12. Feuchtenberger, M., et al., Methotrexate does not increase the monitoring at a tertiary hospital. Australas J Dermatol, 2021.
risk of liver fibrosis in patients with rheumatoid arthritis: assess- 62(1): p. 69-70.
ment by ultrasound elastography (ARFI-MetRA study). Rheu- 25. Cashman, K.D., et al., Vitamin D deficiency in Europe: pandem-
matol Int, 2021. 41(6): p. 1079-1087. ic? Am J Clin Nutr, 2016. 103(4): p. 1033-44.
13. Berends, M.A., et al., Liver injury in long-term methotrexate 26. Darabian, S., et al., Using FibroScan to Assess for the Develop-
treatment in psoriasis is relatively infrequent. Aliment Pharma- ment of Liver Fibrosis in Patients With Arthritis on Methotrex-
col Ther, 2006. 24(5): p. 805-11. ate: A Single-center Experience. J Rheumatol, 2022. 49(6): p.
558-565.
154 www.arprheumatology.com • The official Journal of the Portuguese Society of Rheumatology
You might also like
- 10.1177 - 2050640618792819 Pubmed PDFDocument613 pages10.1177 - 2050640618792819 Pubmed PDFZakiyyah PutriNo ratings yet
- 12 CR Methotrexate Induced LiverDocument2 pages12 CR Methotrexate Induced LiverAnonymous bFByZ3FydNo ratings yet
- MSB 20188793 PDFDocument16 pagesMSB 20188793 PDFAndreea RoxanaNo ratings yet
- Model For End-Stage Liver Disease (MELD) and Allocation of Donor LiversDocument6 pagesModel For End-Stage Liver Disease (MELD) and Allocation of Donor LiversIna MartianaNo ratings yet
- AnnGastroenterol 30 217 PDFDocument8 pagesAnnGastroenterol 30 217 PDFhusni gunawanNo ratings yet
- Bmri2019 3951574Document10 pagesBmri2019 3951574Anonymous 1EQutBNo ratings yet
- Thrombocytopenia Treatment in Chronic Liver DiseaseDocument11 pagesThrombocytopenia Treatment in Chronic Liver DiseasePablo AlvarezNo ratings yet
- Clinical Liver Disease - 2020 - Francis - Use of Statins in Patients With and Without Liver DiseaseDocument6 pagesClinical Liver Disease - 2020 - Francis - Use of Statins in Patients With and Without Liver DiseaseDjabhi SpinzzNo ratings yet
- HyperthyroidDocument7 pagesHyperthyroidHaerun Nisa SiregarNo ratings yet
- Simvastatin For The Prevention of Exacerbations in Moderate-to-Severe COPDDocument10 pagesSimvastatin For The Prevention of Exacerbations in Moderate-to-Severe COPDdhamaraNo ratings yet
- Semaglutide For The Treatment of Non Alcoholic Steatohepatitis Trial Design and Comparison of Non-Invasive BiomarkersDocument9 pagesSemaglutide For The Treatment of Non Alcoholic Steatohepatitis Trial Design and Comparison of Non-Invasive BiomarkersAntonio SalemeNo ratings yet
- Non-Alcoholic Fatty Liver Disease in Patients With Type 2 - Tuong, Tran Thi Khanh Tran, Dang Khoa Phu, Pham Quang - Diagnostics, #3, 10, PagesDocument11 pagesNon-Alcoholic Fatty Liver Disease in Patients With Type 2 - Tuong, Tran Thi Khanh Tran, Dang Khoa Phu, Pham Quang - Diagnostics, #3, 10, PagesLigia AbdalaNo ratings yet
- Performance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseDocument8 pagesPerformance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseChausarPutraBenagilNo ratings yet
- Tuberculosis in Liver Cirrhosis: Rajesh Upadhyay, Aesha SinghDocument3 pagesTuberculosis in Liver Cirrhosis: Rajesh Upadhyay, Aesha SinghAnastasia Lilian SuryajayaNo ratings yet
- Gloomy LifeDocument6 pagesGloomy LifeLanna HarumiyaNo ratings yet
- Methotrexate Vs Secukinumab Safety in Psoriasis Patients With Metabolic SyndromeDocument5 pagesMethotrexate Vs Secukinumab Safety in Psoriasis Patients With Metabolic SyndromeYoga PrabawaNo ratings yet
- Niveles de Catepsina D en Plasma - Una Nueva Herramienta para Predecir Pediátrica La Inflamación HepáticaDocument9 pagesNiveles de Catepsina D en Plasma - Una Nueva Herramienta para Predecir Pediátrica La Inflamación HepáticaLuz Guadalupe Cruz HuancaNo ratings yet
- Drug Induced Hepatitis With Anti-Tubercular Chemotherapy: Challenges and Difficulties in TreatmentDocument5 pagesDrug Induced Hepatitis With Anti-Tubercular Chemotherapy: Challenges and Difficulties in Treatmentmufqifitra160491No ratings yet
- Liver Transplantation for Acute Liver Failure: Prognostic Models and OutcomesDocument7 pagesLiver Transplantation for Acute Liver Failure: Prognostic Models and OutcomesSol Del Mar SarmientoNo ratings yet
- Jurnal Bingg 1Document5 pagesJurnal Bingg 1Tasya AuliaNo ratings yet
- Evaluation of Neutrophiltolymphocyte Ratio NLR and Itscorrelation With Severity of Liver Cirrhosis Based On Childturcott PDFDocument6 pagesEvaluation of Neutrophiltolymphocyte Ratio NLR and Itscorrelation With Severity of Liver Cirrhosis Based On Childturcott PDFSilent StalkerNo ratings yet
- Ferraioli Et Al 2022 Us Attenuation For Liver Fat Quantification An Aium Rsna Qiba Pulse Echo Quantitative UltrasoundDocument12 pagesFerraioli Et Al 2022 Us Attenuation For Liver Fat Quantification An Aium Rsna Qiba Pulse Echo Quantitative UltrasoundThesisaurus IDNo ratings yet
- Articol RJMEDocument6 pagesArticol RJMELigia Ariana BancuNo ratings yet
- Non-Invasive Diagnosis of NASH and NAFLDDocument17 pagesNon-Invasive Diagnosis of NASH and NAFLDRaeni Dwi PutriNo ratings yet
- Liver Fibrosis Biomarkers Elf ScoreDocument4 pagesLiver Fibrosis Biomarkers Elf ScoreDani LicaroiuNo ratings yet
- 2014 Prednisolone vs. Pentoxifylline For Severe Alcoholic HepatitisDocument2 pages2014 Prednisolone vs. Pentoxifylline For Severe Alcoholic HepatitisJairo Torres SoteloNo ratings yet
- Metabolic Syndrome Associated with Prostate Inflammation and LUTS SeverityDocument6 pagesMetabolic Syndrome Associated with Prostate Inflammation and LUTS SeverityekawatierprismanNo ratings yet
- Evaluation of Liver Fibrosis and Cirrhosis On TheDocument7 pagesEvaluation of Liver Fibrosis and Cirrhosis On TheeugeniaNo ratings yet
- 1 s2.0 S0168827820304700 MainDocument11 pages1 s2.0 S0168827820304700 MainHadi KuriryNo ratings yet
- Arab Journal of Gastroenterology: Original ArticleDocument5 pagesArab Journal of Gastroenterology: Original ArticleGestne AureNo ratings yet
- Acute Alcoholic HepatitisDocument11 pagesAcute Alcoholic HepatitisDoc_NethoNo ratings yet
- Nej Mo A 1412278Document10 pagesNej Mo A 1412278amiralevishNo ratings yet
- Hp165-02b-Nash (FF 050816v) ProtegidoDocument9 pagesHp165-02b-Nash (FF 050816v) ProtegidoAnonymous 4txA8N8etNo ratings yet
- MMC 4Document26 pagesMMC 4M. PurnomoNo ratings yet
- Paper Insulin Resistance and Ferritin As Major Determinants of Nonalcoholic Fatty Liver Disease in Apparently Healthy Obese PatientsDocument7 pagesPaper Insulin Resistance and Ferritin As Major Determinants of Nonalcoholic Fatty Liver Disease in Apparently Healthy Obese PatientsNike Dwi Putri LestariNo ratings yet
- Jurnal Gastro DR Kusnanto ToumiDocument7 pagesJurnal Gastro DR Kusnanto ToumiToumi ShiddiqiNo ratings yet
- Liver Toxicity of Sitaxentan in Pulmonary Arterial HypertensionDocument2 pagesLiver Toxicity of Sitaxentan in Pulmonary Arterial Hypertensionefra maneNo ratings yet
- Obeticholic Acid For The Treatment of Non-Alcoholic Steatohepatitis: Interim Analysis From A Multicentre, Randomised, Placebo-Controlled Phase 3 TrialDocument13 pagesObeticholic Acid For The Treatment of Non-Alcoholic Steatohepatitis: Interim Analysis From A Multicentre, Randomised, Placebo-Controlled Phase 3 TrialAdo QuirozNo ratings yet
- Multinational Evidence-Based Recommendations ForDocument40 pagesMultinational Evidence-Based Recommendations FordawniejuneNo ratings yet
- Liver Transplantation - 2007 - Escorsell - Acute Liver Failure in Spain Analysis of 267 CasesDocument7 pagesLiver Transplantation - 2007 - Escorsell - Acute Liver Failure in Spain Analysis of 267 CasesJesús Guzmán DíazNo ratings yet
- Iann 53 1956686Document16 pagesIann 53 1956686M Ibnu Rahman SyahNo ratings yet
- Coffee and Herbal Tea Consumption Is Associated With Lower Liver Stiffness in The General Population: The Rotterdam StudyDocument10 pagesCoffee and Herbal Tea Consumption Is Associated With Lower Liver Stiffness in The General Population: The Rotterdam Studydebby claudiNo ratings yet
- Management of Liver CirrhosisDocument7 pagesManagement of Liver Cirrhosispet_trinNo ratings yet
- Indeks Diastase 2 PDFDocument5 pagesIndeks Diastase 2 PDFddew indahNo ratings yet
- GHFBB 7 055Document8 pagesGHFBB 7 055RezaTiansahNo ratings yet
- Comparative Effectiveness of Urate Lowering With Febuxostat Versus Allopurinol in Gout: Analyses From Large U.S. Managed Care CohortDocument7 pagesComparative Effectiveness of Urate Lowering With Febuxostat Versus Allopurinol in Gout: Analyses From Large U.S. Managed Care Cohortdemrik13No ratings yet
- Impact of Non Invasive Biomarkers On Hepatology PRDocument17 pagesImpact of Non Invasive Biomarkers On Hepatology PRCláudia SilvaNo ratings yet
- Etm 14 02 1496Document9 pagesEtm 14 02 1496Bella La Rosa HusnaNo ratings yet
- Factores Predict Ores en NASHDocument7 pagesFactores Predict Ores en NASHkukito77No ratings yet
- Epidemia HgnaDocument8 pagesEpidemia HgnaAntonio Alexis Bustos TorresNo ratings yet
- Antifibrotic Therapies-EmergingDocument3 pagesAntifibrotic Therapies-EmergingVictor Hugo Campos SierraNo ratings yet
- A New Paradigm in Gallstones Diseases and Marked Elevation of Transaminases: An Observational StudyDocument6 pagesA New Paradigm in Gallstones Diseases and Marked Elevation of Transaminases: An Observational StudyTomás Emmanuel Hernández CuevasNo ratings yet
- Thesis On Liver DiseaseDocument5 pagesThesis On Liver DiseaseCustomNotePaperCanada100% (1)
- The Misunderstood Coagulopathy of Liver Disease - WJM 2018Document9 pagesThe Misunderstood Coagulopathy of Liver Disease - WJM 2018J doeNo ratings yet
- Diagnosis Nafld 2016Document15 pagesDiagnosis Nafld 2016AfifMaulanaFirmansyahNo ratings yet
- pnpla2_rs693Document7 pagespnpla2_rs693Vishnu Sai MokshagnaNo ratings yet
- Boyd Et Al - (2012)Document2 pagesBoyd Et Al - (2012)nuiv iyvbivboiuNo ratings yet
- Fibrosis HeparDocument21 pagesFibrosis HeparelsarovolturiNo ratings yet
- The Search For Disease-Modifying Agents in Decompensated Cirrhosis: From Drug Repurposing To Drug DiscoveryDocument17 pagesThe Search For Disease-Modifying Agents in Decompensated Cirrhosis: From Drug Repurposing To Drug Discoverymuhamad deniansyahNo ratings yet
- Kidney Disease in The Setting of HIV Infection: Conclusions From A Kidney Disease: Improving Global Outcomes (KDIGO) Controversies ConferenceDocument15 pagesKidney Disease in The Setting of HIV Infection: Conclusions From A Kidney Disease: Improving Global Outcomes (KDIGO) Controversies ConferenceArini NurlelaNo ratings yet
- Aasld Practice Guidance On Risk Stratification And.612Document79 pagesAasld Practice Guidance On Risk Stratification And.612Ionut MelesteuNo ratings yet
- 2023 - Hydrocortisone in Severe CommunityDocument11 pages2023 - Hydrocortisone in Severe CommunitygiseladlrNo ratings yet
- 1 s2.0 S1473309923007569 MainDocument12 pages1 s2.0 S1473309923007569 Mainbarrientosgerman321No ratings yet
- Ophtha Quiz - INI CET High Yield TopicsDocument3 pagesOphtha Quiz - INI CET High Yield TopicsAsif MohammedNo ratings yet
- Drug CefuroximeDocument2 pagesDrug CefuroximeDhan LopezNo ratings yet
- We Should Avoid Oily Food . Be Healthy. A. Finally C. Consequently B. in Order To D. So ThatDocument1 pageWe Should Avoid Oily Food . Be Healthy. A. Finally C. Consequently B. in Order To D. So ThathendriNo ratings yet
- MCQs From All Subjects For Medical PG EntranceDocument16 pagesMCQs From All Subjects For Medical PG EntranceEMIN3MNo ratings yet
- Pathophysiology: Risk FactorsDocument4 pagesPathophysiology: Risk FactorsEdson John DemayoNo ratings yet
- Monitoring Report September, 16 2022: Ppds-1 Ipd Rs DR - Moewardi/Fk UnsDocument20 pagesMonitoring Report September, 16 2022: Ppds-1 Ipd Rs DR - Moewardi/Fk UnsZulfikar RamadhanNo ratings yet
- Krok 2 Stomatology: Test Items For Licensing ExaminationDocument30 pagesKrok 2 Stomatology: Test Items For Licensing ExaminationjimmyNo ratings yet
- MAALOX (Drug Study)Document3 pagesMAALOX (Drug Study)Kian HerreraNo ratings yet
- Diagnosis of Canine Claw Disease - A Prospective Study of 24 DogsDocument9 pagesDiagnosis of Canine Claw Disease - A Prospective Study of 24 DogsjenNo ratings yet
- OB Final Exam Study GuideDocument14 pagesOB Final Exam Study GuideMarissa SolanoNo ratings yet
- UTI (Urinary Tract Infection)Document9 pagesUTI (Urinary Tract Infection)Carson BirthNo ratings yet
- Depictions of Mental Health Topics in Malayalam CinemaDocument8 pagesDepictions of Mental Health Topics in Malayalam Cinemagion.nandNo ratings yet
- DNB Family Medicine Question BankDocument157 pagesDNB Family Medicine Question BankEpun B. Dissanayake100% (1)
- nsg-300 Care Plan 2Document21 pagesnsg-300 Care Plan 2api-521003884100% (1)
- The Gut-Kidney Connection inDocument1 pageThe Gut-Kidney Connection inAdrian CraciunNo ratings yet
- Handicapped ChildrenDocument36 pagesHandicapped ChildrenAbdur RehmanNo ratings yet
- MS 2 P1 Part 1 PDFDocument17 pagesMS 2 P1 Part 1 PDFAngel YN Patricio FlorentinoNo ratings yet
- Anemia: Causes, Symptoms and TreatmentDocument2 pagesAnemia: Causes, Symptoms and TreatmentLazeh MeNo ratings yet
- Advice For People With MSDocument10 pagesAdvice For People With MSAsma Al-MahmoudNo ratings yet
- GI System Physical Exam GuideDocument7 pagesGI System Physical Exam GuideS StPierreNo ratings yet
- Pulmonary Pharmacology & TherapeuticsDocument10 pagesPulmonary Pharmacology & TherapeuticsJoko Arif KurniawanNo ratings yet
- Common Viral Exanthemas (Measles, Chickenpox & Rubella) : DR Sarika Gupta (MD, PHD), Assistant ProfessorDocument52 pagesCommon Viral Exanthemas (Measles, Chickenpox & Rubella) : DR Sarika Gupta (MD, PHD), Assistant ProfessorashighaNo ratings yet
- Respiratory Distress SyndromeDocument41 pagesRespiratory Distress Syndromef.abrahamNo ratings yet
- Nahdi Pharma FileDocument477 pagesNahdi Pharma FileSarah JeanNo ratings yet
- Care Plan 9 Substance Use DisorderDocument18 pagesCare Plan 9 Substance Use DisorderLokeshwari KatreNo ratings yet
- Fever Proforma and Assignment - 1Document48 pagesFever Proforma and Assignment - 1SivaNo ratings yet
- Surviving Sepsis Campaign Guideline: Managing Severe Sepsis and Septic ShockDocument38 pagesSurviving Sepsis Campaign Guideline: Managing Severe Sepsis and Septic ShockSelly RizanyNo ratings yet
- Unit - 2nd-WPS Office-1Document8 pagesUnit - 2nd-WPS Office-1Suneel Kumar PrajapatiNo ratings yet
- Bhopal Tragedy - DIDULODocument19 pagesBhopal Tragedy - DIDULOMARK ARQUE LACANARIANo ratings yet
- K7 Jamur Superficial 2020Document51 pagesK7 Jamur Superficial 2020Jimmy Fran IINo ratings yet