Professional Documents
Culture Documents
Prelim - MCN Lec
Uploaded by
laurynejoyce26Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Prelim - MCN Lec
Uploaded by
laurynejoyce26Copyright:
Available Formats
CARE OF MOTHER, CHILD AT RISK OR
WITH PROBLEMS (ACUTE AND CHRONIC)
LECTURE
PROGRAMS, TRENDS, AND ISSUES IN MATERNAL HEALTH
2015 Sustainable Development
INTRODUCTION Goals (SDGs)
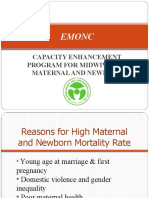
IN 1990S WHY AIM FOR MATERNAL SURVIVAL?
● Every minute, a woman dies in childbirth or from 1. MORAL IMPERATIVE
complications of pregnancy - The death of a woman during pregnancy or
● 500,000 women die each year; almost all (95%) occur childbirth is a violation of her rights to life and
in developing countries health
● For every woman who dies as many as 30 others - Governments must promote dignity and
suffer chronic illness or disability equity for women within the health-care
● Maternal mortality is the health indicator with the most system
disparity between developed and developing 2. SOCIAL IMPLICATIONS
countries - Maternal death or disability can plunge
- The cumulative lifetime risk of dying as a families into poverty and deeper despair;
result of pregnancy is 1:2800 in developed surviving children esp. those < 5 years old
versus 1:16 in developing countries are at risk of dying since no one will attend to
● Maternal mortality trends are unacceptable, but not their needs
insurmountable because the major causes are known - The loss may reverberate throughout an
and avoidable. entire community
● Nearly 2/3 of maternal deaths are due:
- Hemorrhage MATERNAL DEATH
- Obstructed labor ● The death of a woman while pregnant or within 42
- Pregnancy-induced hypertension days of termination of pregnancy, irrespective of the
- Sepsis/infection duration and site of the pregnancy, from any cause
- Complications of unsafe abortion related to or aggravated by the pregnancy or its
● Interventions can be made available even in management but not from accidental or incidental
resource-poor settings causes.
- ICD-10, 1992
METHODOLOGICAL ISSUES IN MEASURING
MATERNAL MORTALITY
1. It is a rare event and therefore its number may not be
large enough to detect statistically significant changes
over time
2. Underreporting - especially if most occur outside of
health facilities (in the absence of health personnel to
report them)
3. Misreporting because of the complicated definition
requiring also its cause and timing OR sometimes
done intentionally to avoid legal action
Different agencies around the world, either within or outside of
the United Nations, have included maternal survival as one of
their most pressing agenda PHILIPPINES COUNTRY PROFILE
1987 Safe Motherhood Initiative PHILIPPINES MATERNAL MORTALITY RATE
1990- World Summit for 1990-2015
Children
● MATERNAL MORTALITY RATIO (MMR) - number of
women who die from pregnancy-related causes while
1994 Safe Motherhood Initiative
pregnant or within 42 days of pregnancy termination
1990- World Summit for
per 100,000 live births.
Children
➔ Philippines maternal mortality rate for 2015
was 114.00, a 2.56% decline from 2014.
1995 4th World Conference on
➔ Philippines maternal mortality rate for 2014
Women 2000-Millennium
was 117.00, a 3.31% decline from 2013.
Summit/Declaration (MDGs)
➔ Philippines maternal mortality rate for 2013
was 121.00, a 3.97% decline from 2012.
NAME: LOYOLA, MA. BERNICE C. 1
KERI PA BA NATIN???
➔ Philippines maternal mortality rate for 2012 MOST MATERNAL DEATHS AND DISABILITIES
was 126.00, a 0.79% decline from 2011. WOULD BE AVERTED IF…
- All pregnancies are wanted and planned - All
pregnancies are adequately managed throughout its
course
- All births are attended by skilled health professionals
(ideally facility-based)
- All complications are managed in adequately staffed
and equipped facilities offering emergency obstetric
care
STRATEGIES TO REDUCE MATERNAL MORTALITY
1. Universal access to contraceptive services to reduce
unintended pregnancies
2. Skilled attendance at all births
Lesson learned
GENETIC ASSESSMENT AND COUNSELING
GENETIC DISORDERS RECESSIVE GENES
● Disorders that can be passed from one generation to ● Gene that is not dominant Masked and does not show
the next
● Result from some disorder in gene or chromosome HOMOZYGOUS DOMINANT
structure ● Individual with two homozygous genes for a dominant
trait
GENES
● Are basic units of heredity that determine both the HOMOZYGOUS RECESSIVE
physical and cognitive characteristic of people ● Individual with two genes for a recessive trait
● Composed of segments of DNA
● Woven into strands in the nucleus of all body cells to
form chromosomes GENETIC COUNSELING
PHENOTYPE AIMS OF GENETIC COUNSELING
● Refers to the person's outward appearance or the
● To provide accurate information
expression of the genes
● To provide reassurance
● To assist individual/couple to make informed choices
GENOTYPE ● To educate individual/couple about the effects of
● Refers to the person's actual gene composition genetic disorders
● A couple who has a child with a congenital disorder or
GENOME an inborn error of metabolism
● Complete set of genes present Normal genome -
46XX or 46XY WHO MAY BENEFIT FROM GENETIC COUNSELING?
● A couple who has a child with a congenital disorder or
an inborn error of metabolism
MENDELIAN INHERITANCE: DOMINANCE AND ● A couple whose close relatives have a child with a
RECESSIVE PATTERNS genetic disorder
● Any individual who is known balanced translocation
MENDELIAN INHERITANCE carrier
● Any individual who has an inborn error of metabolism
● Discovered and described by Gregor Mendel in
or chromosomal disorder
1800's
● A consanguineous (closely related) couple
● A person who has two like genes for a trait - two
● Any woman older than 35 years of age and any man
healthy genes for example (one from the mother and
older than 45 years of age
one from the father) --is said to be HOMOZYGOUS
● Couples of ethnic backgrounds in which specific
for a trait
illnesses are known to occur
● lf the genes differ (a healthy gene from the mother
and an unhealthy gene from the father, or vice versa),
the person is said to be HETEROZYGOUS for that ASSESSMENT FOR GENETIC DISORDERS
trait.
DOMINANT GENES ASSESSMENT
● Dominant in action when paired with other genes ● Careful assessment of the pattern of inheritance
● Visibly expressed ● History
NAME: LOYOLA, MA. BERNICE C. 2
KERI PA BA NATIN???
● Physical assessment
● Diagnostic testing LEGAL AND ETHICAL ASPECTS OF GENETIC
SCREENING AND COUNSELING
TRISOMY 13 SYNDROME (47XY13+ OR 47XX13)
● PATAU Syndrome
● Extra chromosome 13
● Severely cognitively challenged Midline disorders:
cleft lip and palate, heart disorders, abnormal
genitalia
● Do not survive beyond early childhood
DIAGNOSTIC TEST
KARYOTYPING
● Visual presentation of the chromosome pattern of an
individual
● Specimen: venous blood/cells from buccal membrane
● Metaphase (stage of mitosis)
● Stained, place under microscope and photographed
MATERNAL SERUM SCREENING TRISOMY 18 SYNDROME (47XY18+ OR 47XX18+)
● Alpha fetoprotein-glycoprotein produced by the fetal ● EDWARDS Syndrome
liver ● Three copies of chromosome 18 Severely cognitively
● Peaked in maternal serum between 13th and 32nd challenged
week ● Small for gestational age, low-set ears, small jaw,
● Usually done at the 15th week of pregnancy congenital heart defects, misshapen fingers and toes,
● Elevated level: spinal cord disease Decreased: rounded soles of the feet
trisomy 21 ● Do not survive beyond infancy
CHORIONIC VILLI SAMPLING CRI-DU-CHAT SYNDROME (46XX5P- OR 46XY5P-)
● Involves retrieval and analysis of chorionic villi ● Missing portion of chromosome 5
● Commonly done at 8-10 weeks, earliest at weeK 5 ● Abnormal cry (sound of a cat)
● Reveals genetic abnormalities like Retinoblastoma, ● Small head, wide-set eyes, downward slant to the
myotonic dystrophy (muscle problems), sickle cell palpebral fissure of the eye, recessed mandible
anemia, thalassemia ● Severely cognitively challenged
AMNIOCENTESIS TURNER SYNDROME (45X0)
● Withdrawal of amniotic fluid through the abdominal ● GONADAL DYSGENESIS
wall at 14th-16th wk ● One functional chromosome
● Needle is inserted, aspirate 20ml ● Short in stature
● Small & nonfunctional ovaries
PERCUTANEOUS UMBILICAL BLOOD SAMPLING ● Webbed & short neck/ wide neck folds
● Congenital anomalies- coarctation of the aorta, kidney
● Removal of blood from fetal umbilical cord at about 17
disorders
weeks using amniocentesis technique
● Severely cognitively challenged
LEGAL AND ETHICAL ASPECTS OF GENETIC
SCREENING AND COUNSELING
● Participation by couples or individuals in genetic
screening must be elective
● People desiring genetic screening must sign an
informed consent
● Results must be interpreted
● Results must not be withheld, and given only to the
people directly involved
● After genetic counseling, persons must not be
coerced to have abortion or sterilization
NAME: LOYOLA, MA. BERNICE C. 3
KERI PA BA NATIN???
KLINEFELTER SYNDROME (47XXY) CHILD WITH DOWN SYNDROME
● Males with an extra X chromosome ● Typical facial features of a child with Down syndrome
● At puberty, secondary sex characteristics do not
develop
● Testes remain small & produce ineffective sperm
● Gynecomastia (Increased breast size) High risk of
male breast cancer
FRAGILE X SYNDROME (46XY230)
● Common cause of cognitive challenge in males
● X-linked disorder- one long arm of an X
● chromosome is defective
● Hyperactivity, aggression, autism ● Simian Line, a horizontal crease seen in children with
● Deficits in speech & arithmetic Down Syndrome
● Large head, face with a high forehead, prominent
lower jaw, large protruding ears, obese
● After puberty, enlarged testicles may become evident
● Fertile & can reproduce
● Carrier females- may show physical & cognitive
characteristics
DOWN SYNDROME (TRISOME 21) (47XY21+ OR
47XX21+)
● Most common chromosomal disorder
● High risk - women more 35 yrs. old
● Nose is broad & flat
● Eyelids have extra fold of tissue at the inner canthus
(Epicanthal fold)
● Palpebral fissure (opening between the eyelids) tends
to slant laterally upward
● Iris of the eye have white specks (Brushfield spots)
● Protruding tongue (due to small oral cavity)
● Back of the head is flat
● Neck is short
● Low set ears
● Poor muscle tone - rag doll appearance
● Short & thick fingers
● Palm of the hand shows peculiar crease (Simian line)-
a single horizontal crease
● IQ less than 20
● Congenital heart disease
● Prone to Upper Respiratory Tract Infection (URTI),
Acute Lymphocytic Leukemia (ALL)
● Life span is 50-60 years
NURSING CARE OF THE HIGH RISK PREGNANT CLIENT - PART 1
HIGH RISK PREGNANCY PHYSIOLOGIC
- One in which a concurrent disorder, ● Concurrent illness
pregnancy-related complications or external factor ● Malnutrition
jeopardize the health of the woman, the fetus or both ● Physically challenged
● Frequent pregnancies
RISK FACTORS
● Physiological SOCIO DEMOGRAPHIC
● Socio demographic ● Poverty
● Psychological ● Unemployment
● Environmental ● Lack of education
NAME: LOYOLA, MA. BERNICE C. 4
KERI PA BA NATIN???
● Age ● Abnormal amniotic fluid volume
● Poor access to transportation for care ● Isoimmunization
● Lack of support people
BLEEDING DURING PREGNANCY
PSYCHOLOGICAL FACTOR ● Always deviation from the normal
● Cognitively challenge
● Single /Separated mothers
● Victims of Abuse, domestic violence, rape, incest SUMMARY OF PRIMARY CAUSES OF BLEEDING
● Mental Retardation DURING PREGNANCY
ENVIRONMENTAL FACTORS
● Exposure to Teratogens due to employment
● Environmental contaminants at home
● Poor Housing
CARING FOR A WOMAN WHO DEVELOPS A
COMPLICATION OF PREGNANCY
ASSESSMENT
● Provide enough time for thorough health history.
● Problems such as headache, blurred vision, vaginal
spotting should be discovered and investigated
thoroughly
COMMON NURSING DIAGNOSIS
● Anxiety related to guarded pregnancy outcome
● Risk for infection related to incomplete miscarriage
● Deficient knowledge related to signs and symptoms of
possible complications.
● Risk for ineffective tissue perfusion related to
pregnancy-induced hypertension.
● Ineffective role performance related to increasing level
of daily restrictions secondary to chronic illness and
pregnancy
IMPLEMENTATION
● Interventions for woman experiencing a complication
of pregnancy include measures to maintain number of
different areas:
● Continued healthy fetal growth
● A woman's and family's psychological health
● Continuation of the pregnancy as long as possible
EVALUATION
● Client's BP is maintained within acceptable
parameters
● Couple state they feel able to cope with anxiety
associated with the pregnancy complication
● Client accurately verbalizes crucial signs and
symptoms to report to the health care provider
immediately.
SUDDEN PREGNANCY COMPLICATIONS
● Bleeding during pregnancy
● Ectopic pregnancy
● Gestational trophoblastic disease
● Premature cervical dilatation
● Placenta previa Abruptio placenta
● Disseminated intravascular coagulation
● Preterm labor
● Preterm rupture of membranes
● Pregnancy induced hypertension
● HELLP Syndrome
● Multiple pregnancy
NAME: LOYOLA, MA. BERNICE C. 5
KERI PA BA NATIN???
ABORTION
- Medical term for any interruption of a pregnancy
before a fetus is viable
SPONTANEOUS MISCARRIAGE
- Early miscarriage if it occurs before 16th week
- Late between 16-24 weeks
CAUSES:
● Teratogenic factor
● Chromosomal aberrations/abnormal fetal
development
● Implantation abnormalities
● Failure to produce enough progesterone
● Infection
PRESENTING SYMPTOM
● Vaginal bleeding/spotting
➔ Should consult attending Obstetrician so that
instructions may be given
THREATENED MISCARRIAGE
● Vaginal bleeding, scant, bright red usually, slight
cramping
● No cervical dilatation
MANAGEMENT:
● Fetal heart assessment
● Utz
● hCG determination
● Avoid strenuous activity
● Coitus usually restricted for 2 weeks
● Spotting usually stops within 24-48 hours
IMMINENT (INEVITABLE) MISCARRIAGE
● Uterine contractions and cervical dilatation occurs
● Loss of product of conception cannot be halted
● lf no FHT and UTZ reveals empty uterus dilation and
evacuation may be performed
COMPLETE MISCARRIAGE
- Entire products of conception are expelled
spontaneously without assistance
INCOMPLETE MISCARRIAGE
- Part of the conceptus is expelled, but the membrane
or placenta is retained
MANAGEMENT:
● Dilatation and curettage or suction curettage
RECURRENT PREGNANCY LOSS
● Women who had 3 spontaneous miscarriages
● Defective spermatozoa or ova
● Endocrine factors
● Deviations of the uterus
● Uterine infections
● Autoimmune disorders
COMPLICATIONS OF MISCARRIAGE
SHOW
● Hemorrhage
- Cervix is Less than 4cm dilated and the membranes ● Infection
are still intact ● Risk for isoimmunization
NAME: LOYOLA, MA. BERNICE C. 6
KERI PA BA NATIN???
PROCESS OF SHOCK BECAUSE OF BLOOD LOSS
SIGNS AND SYMPTOMS OF HYPOVOLEMIC
SHOCK
RUPTURED ECTOPIC PREGNANCY
● Sharp stabbing pain in lower abdominal quadrant
● Vaginal spotting
● Amount of bleeding not evident
● May lead to shock
● Falling hcg level
● Utz – providers clear cut picture
ECTOPIC PREGNANCY IF THE WOMAN DOES NOT SEEK HEKP AT ONCE
● Implantation occurs outside the uterine cavity ● Cullen’s sign (umbilicus may develop a bluish tinge)
● Ovary or cervix ● Dull, vaginal abdominal pain
● Most common is fallopian tube ● Movement of cervix cause excruciating pain
● Due to fallopian scarring that slow the travel of the ● Pain in shoulder
zygote
● Woman still experience the signs of pregnancy MANAGEMENT
● Missed period ● Unruptured – methotrexate followed by leucovorin,
● Signs and symptoms of pregnancy is experienced by mifepristone (abortifacient)
the woman ● Ruptured – emergency situation
● (+) Pregnancy test ● Laparoscopy – ligate the bleeding vessels and
remove/ repair fallopian tube
NAME: LOYOLA, MA. BERNICE C. 7
KERI PA BA NATIN???
● CBC ● Symptoms of pregnancy induced hypertension may
● Administration of fluids appear before 20th week
● Ultrasound – no fetal growth and fetal heart sound
ABDOMINAL PREGNANCY ● Marked nausea and vomiting
● Woman may report sudden lower quadrant pain ● Dark brown blood, profuse flesh flow (16 weeks) with
● Fetal outline is easily palpable clear fluid filled vesicles.
● Danger is infiltration of large blood vessel, bowel
perforation, poor nutrient supply to the fetus THERAPEUTIC MANAGEMENT
● Infant must be born through laparotomy ● Suction curettage
● Post surgery:
● Pelvic examination, chest radiography, hCG level
● hCG monitoring
● Half of woman positive at 3 weeks
● ¼ positive result at 40 days
● Assess every 2 weeks until normal
● Every 4 weeks for the next 6 to 12 months
● Should use reliable contraceptive method
● Plan pregnancy at 12 months if hcg is normal.
PROPHYLAXIS
● Methotrexate
● Dactinomycin
PREMATURE CERVICAL DILATION
● Old name – Incompetent cervix
● Cervix that dilate prematurely, cannot hold a fetus
until term
● Painless
● Pink – stained vaginal discharge (1st symptom)
● Followed by rupture of membrane, discharge of
amniotic fluid
RATE OF SURVIVAL ● Uterine contractions – birth of the fetus
● 60%
ASSOCIATED WITH:
GESTATIONAL TROPHOBLASTIC DISEASE ● Increased maternal age
(HYDATIDIFORM MOLE) ● Congenital structured defect
● Abnormal proliferation and then degeneration of the ● Trauma to cervix
trophoblastic villi
● Cells become filled with fluid and appears as fluid MANAGEMENT:
filled grape sized vesicles ● Cervical cerclage – purse – string sutures are placed
● 1 in every 1500 pregnancy in the cervix by vaginal route.
● Two types:
● Complete mole – all trophoblastic villi swell and MCDONALD PROCEDURE
become cystic. ● Nylon suture are placed vertically and horizontally
● Partial mole – some of the villiform normally across the cervix and pulled tight to reduce the
cervical canal.
● Shirodkar
● Sterile tape is threaded in a purse string manner
under the submucous layer of the cervix.
ASSESSMENT
● Uterus tends to expand faster
● Strong (+) result of hCG-1 to 2 M IU compared to a
normal of 400, 000 IU)
NAME: LOYOLA, MA. BERNICE C. 8
KERI PA BA NATIN???
NURSING CARE OF THE HIGH RISK PREGNANT CLIENT - PART 2
PLACENTA PREVIA THERAPEUTIC MANAGEMENT
● Placenta is implanted abnormally in the uterus. ● Never attempt a pelvic or rectal examination with
● Most common cause of painless bleeding in the third painless bleeding late in pregnancy
trimester of pregnancy. ● Obtain baseline VS
● lVE therapy
● I and O monitoring
● External monitoring equipment
● Complete blood count
● Blood typing and crossmatching
HOW IS THE FETUS DELIVERED?
● Depends on the percentage of previa and the
condition of the pregnancy
PREMATURE SEPARATION OF THE PLACENTA /
ABRUPTIO PLACENTA
● Placenta appears to be implanted correctly
● Begins to separate and bleeding results
● Cause is unknown
OCCURS IN 4 DEGREES
PREDISPOSING FACTORS:
● Low lying - implantation in the lower rather than in the
● High parity
upper portion of the uterus
● Advanced maternal age
● Marginal - the placenta edge approaches that of the
● Short umbilical cord
cervical os
● Chronic hypertensive disease
● Partial - implantation that partially obstructs the
● Pregnancy induced hypertension
cervical os
● Direct trauma
● Total placenta previa - totally obstructs the cervical os
● Vasoconstriction
● Autoimmune antibodies
ASSESSMENT ● Chorioamnionitis
● Bleeding is abrupt, painless, bright red and sudden
● Immediate care measures: ASSESSMENT:
● Place the woman immediately on bedrest in a side
● Sharp stabbing pain high in the uterine fundus
lying position
● If labor begins, each contraction will be accompanied
by pain over and above the pain of contraction
ASSOCIATED WITH: ● Heavy bleeding - evident if separation occurs at the
● Increased parity edges
● Advanced maternal age ● Couvelaire uterus (uteroplacental apoplexy) - hard
● Past CS board like uterus with no apparent or minimally
● Past uterine curettage apparent bleedingDisseminated Intravascular
● Multiple gestation Coagulation (DIC) may occur
● Male fetus
THERAPEUTIC MANAGEMENT:
ASSESS: ● Emergency situation
● Duration of pregnancy ● Large gauge IV catheter
● Time the bleeding began ● Oxygen by mask
● Estimate amount of blood loss ● FHT and maternal VS monitoring
● Accompanying pain ● Lateral position
● Color of the blood ● No abdominal, pelvic or vaginal examination
● What has she done ● Unless separation is minimal, pregnancy must be
● Prior episodes of bleeding TERMINATED
● Prior cervical surgery
NAME: LOYOLA, MA. BERNICE C. 9
KERI PA BA NATIN???
PRETERM LABOR
● Labor that occurs before the end of the 37 weeks of
gestation
● Persistent uterine contractions, cervical effacement
over 80% and dilation over 1 cm
● Unknown cause
CONDITIONS ASSOCIATED:
● Dehydration
● UTI
● Periodontal disease
● Chorioamnionitis
● Inadequate prenatal care
ASSESSMENT:
● Persistent, dull, low backache
● Vaginal spotting
● Pelvic pressure or abdominal tightening
● Menstrual like cramping
WAYS TO PREDICT WHICH PREGNANCY WILL END
EARLY:
● Analyze change in vaginal mucus
● Presence of fetal fibronectin (protein produced by
trophoblast cells) - preterm contractions are ready to
DISSEMINATED INTRAVASCULAR COAGULATION occur
(DIC) ● Absence of fetal fibronectin labor will not occur at
● Acquired disorder of blood clotting, fibrinogen (plasma least 14 days
protein produced in the liver and is converted into
fibrin during blood clot formation) level falls to below THERAPEUTIC MANAGEMENT:
effective limits ● Woman usually admitted
● Conditions associated with its development: ● Bed rest
● Premature separation of placenta ● lV fluids hydration may stop contractions
● PIH ● Tocolytic agent - halt labor (terbutaline)
● Amniotic fluid embolism (obstruction of blood vessel) ● Advise to limit strenuous activities
● Placental retention ● Fetal assessment - count to 10 test
● Septic abortion
● Retention of dead fetus ADMINISTRATION OF TERBUTALINE:
● Test tube-clemature separation of placenta
● PIH ● Mixed with Lactated Ringer's
● Amniotic fluid embolism (obstruction of blood vessel) ● Piggy back
● Placental retention ● Microdrip
● Septic abortion ● Check blood pressure and pulse rate
● Retention of dead fetus ● If contractions are halt. oral terbutaline may be given
DIC DRUG ADMINISTRATION:
- Extreme bleeding causes many platelets and fibrin ● Steroid (betamethasone) - to hasten lung maturity
from the general circulation rush to the site, not ● Effects after 24 hours and lasts 7 day
enough are left for the rest of the body
LABOR THAT CANNOT BE HALTED
TEST CLOTTING ● Membranes have ruptured
● Test tube-clot must form ● Cervix more than 50%
● Platelet assessment - less than or equal to ● effaced and 3-4 cm dilated
100,000/uL ● If fetus is very immature - CS
● Prothrombin - low
● Thrombin-elevated METHOD OF DELIVERY
● Fibrinogen - less than 150 ● If very immature - CS delivery to reduce pressure on
● mg/dL the fetal head
● Cord is clamped immediately extra amount of blood
MANAGEMENT: could overburden the circulatory system
● Halt the underlying insult
● IV administration of PRETERM RUPTURE OF THE MEMBRANES
● Heparin ● Rupture of fetal membranes with loss of amniotic fluid
● Blood or platelet transfusion during pregnancy before 37 weeks
NAME: LOYOLA, MA. BERNICE C. 10
KERI PA BA NATIN???
THREATS TO FETUS: THERAPEUTIC MANAGEMENT:
● Uterine and fetal infections - If labor does not begin, and fetus is at point of
● Increased pressure on the umbilical cord (cord viability:
prolapse) ● Woman is placed on bed rest and receives
● Potter -like syndrome - distorted facial features and corticosteroid
pulmonary hypoplasia from pressure ● Administration of broad-spectrum antibiotics
● Membranes resealed by fibrin-based commercial
ASSESSMENT: sealant
● Sudden gush of clear fluid from vagina
● Test with nitrazine paper- turns blue (alkaline)
NURSING CARE OF THE HIGH RISK PREGNANT CLIENT - PART 3
PREGNANCY INDUCED HYPERTENSION
● Vasospasm occurs during pregnancy in both small
and large arteries
● Used to be called toxemia
OCCURS MOST FREQUENTLY IN WOMEN:
● Of color
● Multiple pregnancy
● Primiparas younger than 20 years or older than
● 40 years
● Low socioeconomic backgrounds poor nutrition
● Who have had five or more pregnancies
● Hydramnios
● Underlying disease heart dse, diabetes, renal MANAGEMENT: MILD PRE ECLAMPSIA
involvement ● Promote bed rest
● Anti platelet therapy
CLASSIFICATIONS: ● Promote good nutrition
● Gestational hypertension ● Provide emotional support
● Mild eclampsia
● Severe eclampsia MANAGEMENT FOR SEVERE PRE ECLAMPSIA:
● Eclampsia ● Support bed rest
● Monitor maternal well being
ASSESSMENT ● Monitor fetal well being
● Hypertension ● Support nutritious diet
● Proteinuria ● Administer medications to prevent eclampsia
● Edema
MANAGEMENT FOR SEVERE PRE ECLAMPSIA:
● Support bed rest
● Monitor maternal well being
● Monitor fetal well being
● Support nutritious diet
● Administer medications to prevent eclampsia
MANAGEMENT OF ECLAMPSIA:
● Tonic-clonic seizures
● Maintain patent airway
● Administer oxygen
● Turn to side
● Administer Magnesium sulfate (Antidote: Calcium
Gluconate) or Diazepam (Valium)
● Assess FHT
● Check for vaginal bleeding
HELLP SYNDROME
● Variation of PIH
● H-emolysis (lysis of RBC)
● E-levated L-iver enzymes
● L-ow P-latelet count
● Increased BP. edema, proteinuria+
● Nausea, epigastric pain, general malaise, RUQ
tenderness
NAME: LOYOLA, MA. BERNICE C. 11
KERI PA BA NATIN???
MANAGEMENT: ● Reveals by ultrasound
● Improve platelet count by transfusion of fresh frozen
plasma or platelets THERAPEUTIC MANAGEMENT:
● Closer prenatal supervisions
MULTIPLE PREGNANCY
● A woman's body must adjust to the effects of more HYDRAMNIOS
than one fetus ● Normal amniotic fluid volume 500-1000mL
● Fluid index above 24 cm or more than 2000 mL
MONOZYGOTIC TWINS: ● Suggests difficulty with the fetus' ability to swallow
● Single ovum and spermatozoon, zygote N divides into ● Unusual enlargement of uterus
two IDENTICAL individuals ● Difficult to auscultate FHT
● One placenta, one chorion. 2 amnions, 2 umbilical ● Shortness of breath
cords ● Increase weight gain
● Hemorrhoid
DIZYGOTIC (FRATERNAL / NON-IDENTICAL) ● Varicosities
● Polyhydramnios - is excessive amniotic fluid
● Double ova-2 placentas, 2 chorions, 2 amnions. 2 surrounding the fetus (more)
umbilical cord
MANAGEMENT:
● Bed rest
● Assess VS and edema
● NSAID (Non-Steroidal Anti-inflammatory Drugs)
● Amniocentesis- almost daily
OLIGOHYDRAMNIOS
● Pregnancy with less than the average amount of
amniotic fluid
● Caused by bladder or renal disorder
● Fetus is cramped for space
● Uterus fails to meet expected growth rate
● Mgt: Amnio Transfusion
POST TERM PREGNANCY
● Pregnancy that exceeds 42 weeks
● Common in receiving salicylates (analgesics)
● If there is evidence of placental insufficiency
● Mgt: oxytocin to initiate labor or CS is performed
ISOIMMUNIZATION
● Occur when an Rh negative mother carries a fetus
with an Rh positive blood (D antigen)
MATERNAL ANTIBODIES MAY CROSS THE
PLACENTA CAUSING:
● Hemolytic disease of the newborn or Erythroblastosis
fetalis (RBC destruction, decreased 02 supply)
ASSESSMENT:
● Uterus increase in size at a rate faster than usual ASSESSMENT
● Alpha-fetoprotein levels elevated ● Anti D antibody titer-done at 1 st pregnancy visit
● Quickening - flurries of action at different portions of
abdomen
NAME: LOYOLA, MA. BERNICE C. 12
KERI PA BA NATIN???
● If normal (0) or minimal (below 1:8) test repeated in
the 28th week
● If normal no therapy
● If elevated (1:16) - fetal condition monitored every 2
weeks
THERAPEUTIC MANAGEMENT:
● Passive Rh (D) antibodies against the Rh factor is
administered to women who are Rh-negative at 28
weeks
● Given in the 1 st 72 hours after birth
● Cord blood is tested if Rh positive (Coombs' negative)
large amount of antibodies are not present in the
mother, mother will receive RhIG injection
● If Rh negative injection not necessary
INTRAUTERINE TRANSFUSION
● Injection of RBC directly into the vessel of the fetal
cord or depositing them in the fetal abdomen
FETAL DEATH
● If labor does not begin, it will be induced by a
combination of prostaglandin gel such as misoprostol
(Cytotec) and oxytocin
● Cytotec should not be given to pregnant women
because it can trigger abortion; it is meant for ulcer
NAME: LOYOLA, MA. BERNICE C. 13
KERI PA BA NATIN???
NURSING CARE OF A FAMILY EXPERIENCING PREGNANCY COMPLICATIONS FROM PREEXISTING OR NEWLY
ACQUIRED ILLNESS - PART 1
● Hypertensive vascular disease
CARDIOVASCULAR DISORDERS AND ● Thromboembolic disease
PREGNANCY ● Rheumatic heart disease
CONCERNS: CLASSIFICATION OF HEART DISEASE
● Can a woman get pregnant? ● CLASS 1 - No limitation of physical activities, regular
● If the couple decides to get pregnant, how will it affect activity do not produce symptoms
the health condition of the woman and the growing ● CLASS 2 - Slightly compromised, slight limitation,
fetus? asymptomatic at rest but regular activities produce
● How does it affect the decision making of the couple? palpitations, fatigue, dyspnea and anginal pains
● CLASS 3 - Marked limitations, ordinary / regular
activities cause symptoms
CARDIAC DISEASE
● CLASS 4 - Marked limitation, symptomatic
- Variety of health conditions both congenital and
acquired that complicate pregnancy LEFT SIDED HEART FAILURE
● Mitral valve cannot effectively push blood forward
CARDIAC OUTPUT
● Back pressure on the pulmonary circulation
● Rises significantly ● If pressure w/in the pulmonary vein reaches 25 mm
● Plateau is 28-32 weeks hg, fluids pass from capillary membranes to interstitial
space surrounding the alveoli
FACTORS INCREASING CARDIAC OUTPUT ● Pulmonary edema
● Blood volume ● Dyspnea, blood specked sputum, change in vital
● Hormonal influences signs, orthopnea, paroxysmal nocturnal dyspnea
● Autonomic nervous system
RIGHT SIDED HEART FAILURE
BLOOD VOLUME ● Output of right ventricle<blood volume received by
● Increases by plasma volume expansion and RBC right atrium from the vena cava
multiplication ● Back pressure=congestion of the systemic venous
● Heart rate increases and dilated systemic vasculature circulation and less cardiac output to the lungs
is maintained ● Jugular venous distention, increased portal
circulation, Extreme dyspnea, Pain, Ascites,
HORMONAL INFLUENCES Peripheral edema
● Increased estrogen
● Systemic vasodilation PERIPARTAL CARDIOMYOPATHY
● Lowered peripheral resistance - Weakness and enlargement of the heart muscle that
● Increased cardiac output usually occurs from around the final month of
pregnancy through about five months after pregnancy
AUTONOMIC NERVOUS SYSTEM ● No previous history of heart disease
● Cardiovascular system is hyperfilled from increased ● Shortness of breath
blood volume and hyperdynamic ● Chest pain
● Edema
PT WILL LIKELY REPORT SIGNS AND SYMPTOMS
THAT MIMIC CARDIAC DISEASE RHEUMATIC HEART DISEASE
● Compilation of rheumatic fever in which the heart
● Dyspnea
valves are damaged
● Orthopnea
● Affects the valves of the heart secondary to previous
● Edema
exposure to beta hemolytic streptococcus such as
● Syncope
streptococcal pharyngitis
● Palpitations
RISK FACTORS ASSESSMENT
● History of pre pregnancy cardiac status
● Rheumatic fever 90%
● Level of exercise performance
● Congenital defects
● Physical assessment
● Arteriosclerosis
● Diagnostic tests
● Myocardial infections
● Fetal assessment
● Pulmonary diseases
● Renal diseases
● Heart surgery CRITERIA FOR ESTABLISHING A DIAGNOSIS OF
CARDIAC DISEASE IN PREGNANCY
EXAMPLES OF CARDIAC DISEASE ● Persistent murmur
● Left sided heart failure ● Permanent cardiomegaly- enlargement of the heart
● Right sided heart failure ● Severe dysrhythmias
● Cardiomyopathy
NAME: LOYOLA, MA. BERNICE C. 14
KERI PA BA NATIN???
● Severe dyspnea prior to stage of pressure on the DECREASE WORKLOAD OF THE HEART
diaphragm ● Adequate rest and sleep
● Treat early anemia
SIGNS OF CARDIAC DECOMPENSATION ● Prevent exhaustion, fatigue, stress
● Moist cough
● Pedal edema AVOID ACTIVITIES THAT DECREASE OXYGENATION
● Dyspnea ● Smoking
● Tachycardia ● Overcrowded place
● Tachypnea
● Chest pain on exertion AVOID CONSTIPATION
● Cyanosis
● Persistent heart murmur ● Daily fruits
● Vegetables
MATERNAL EFFECTS ● Regular bowel movement
● Regular exercise
● Patients with valvular problems causing atrial
fibrillation-susceptible to embolic episodes PROPER NUTRITION
● Cyanotic heart disease-increase the maternal
mortality by 50% ● Well balanced diet
● Adequate protein
FETAL AND NEONATAL EFFECTS ● Low sodium, fats and carbohydrates
● No junk foods and stimulants
● Compromised maternal circulation- uterine blood flow
will be reduced INTRAPARTUM PERIOD GOALS
● Spontaneous abortion- Growth retardation and Mental
retardation ● Minimize changes in pulse and blood pressure:
● Fetal Distress- Preterm delivery and fetal ● Lateral position
morbidity/fetal death ● Adequate pain relief
● Avoidance of hemorrhage
USUAL MEDICAL MANAGEMENT AND PROTOCOLS ● Avoidance of infection
● Oxygen per mask
FOR NURSE PRACTITIONERS ● Forceps or vacuum extraction
● GENERAL MANAGEMENT ● Elective CS
○ Team approach
○ Adjust cardiac medications PRIMARY GOAL:
○ Bed rest/restricted activity
● Reduce risks for complications
○ Prophylactic antibiotic
○ Careful titration of fluid volume
○ Advance planning for route of delivery ACHIEVED BY:
● DRUG THERAPY ● Education
○ Heparin – anticoagulant ● Routine assessment
○ Warfarin - pulmonary embolism/prosthetic ● Proper referral
valves ● Facilitation of patient participation in decision
○ Furosemide - diuretic ● Being an advocate and coordinator for the
○ Digitalis - crosses placental barrier multidisciplinary team approach
○ Tocolytics
○ Beta blockers - treat hypertension
NURSING IMPLEMENTATIONS
● Encourage early, frequent and regular prenatal visits
● Encourage compliance with therapeutic regimen
NURSING CARE OF A FAMILY EXPERIENCING PREGNANCY COMPLICATIONS FROM PREEXISTING OR NEWLY
ACQUIRED ILLNESS - PART 2
IRON DEFICIENCY ANEMIA
HEMATOLOGIC DISORDERS AND PREGNANCY
● Most common
● Diet low in iron
ANEMIA ● Heavy menstrual period
- Decrease in oxygen carrying capacity of the blood ● Unwise weight reduction program
due to decrease hemoglobin (protein in the red blood ● Woman experiences fatigue and poor exercise
cells that carries oxygen) in the blood tolerance
RISK FACTORS: RBC’S ARE:
● Decrease nutritional intake ● Microcytic - exceptionally small RBC
● Heredity ● Hypochromic - decreased hemoglobin in the RBC
● Increased demands as in pregnancy and adolescence
● Poor absorption
NAME: LOYOLA, MA. BERNICE C. 15
KERI PA BA NATIN???
ASSESSMENT FINDINGS SICKLE CELL ANEMIA
● Pale skin and mucous linings ● Caused by abnormal amino acid in the beta chain of
● Pearl white sclera hemoglobin
● Brittle flattened nails ● Recessively inherited
● Low Hgb - less than 10 g/dl ● Majority of RBCs are irregular or sickle shaped and
● Low Hematocrit (measures how much space in the cannot carry much hemoglobin
blood is occupied by red blood cells) - less than 33% ● If amino acid valine is replaced - sickle hemoglobin
● Serum Iron (< 65 ug/100 ml blood) (Hbs)
● If amino acid lysine is replaced - non sickling
MAY LEAD TO
● Low birth weight
● Preterm birth
● Increased incidence of abortion and premature labor
PREVENTION / MANAGEMENT
● Prenatal vitamins containing iron supplement of 60
mg elemental iron
● Diet high in iron such as green leafy vegetables,
meat, legumes (beans) and fruits
● If with deficiency : 120-200 mg/day
● Severe anemia- IV iron dextran (substitute for blood MAY RESULT TO:
plasma or transfusion) ● Blockage to placental circulation
● Low birth weight
NURSING IMPLEMENTATIONS ● Fetal death
● Promote a balance of activity and rest with avoidance
of fatigue THERAPEUTIC MANAGEMENT
● Provide dietary instructions ● Exchange transfusion
● Encourage regular intake of ordered hematinics ● Administering oxygen
(ferrous sulfate) ● Controlling pain
● Increasing fluid volume
FOLIC ACID DEFICIENCY ● The chances of passing it to the offspring depends on
genetic composition of the parents
● Folic acid-B vitamin necessary for the normal
formation of red blood cells
● Leads to megaloblastic anemia (abnormally large, RENAL AND URINARY DISORDERS
immature and dysfunctional red blood cell) ● Urinary tract Infection (UTI)
● Becomes apparent in the 2nd trimester of pregnancy ● Chronic Renal Failure
● More common in multiple pregnancy
INCIDENCE
CAUSES ● Infection - 1-5% of pregnancies
● Alcohol abuse (alcohol prevents absorption of several ● Chronic kidney disease - 6 to 12 cases per 10,000
nutrients especially the B vitamins) pregnancies
● Poor diets (common in alcoholics, the elderly, those
living alone or in poverty, and infants especially those KIDNEYS
with infections or diarrhea) ● Excrete water, electrolytes and nitrogenous waste
● Impaired absorption because of intestinal dysfunction product
● Bacteria competing for available folic acid ● Acid-base balance
● Overcooking of food, destroying valuable ● Secretes erythropoietin - kidney hormone that
water-soluble nutrients, including a high percentage of increases the number of RBC in cases of anemia
folic acid ● Renin - angiotensin - aldosterone system Renin -
● Limited storage capacity in infants hormone released in the kidney in response to either
● Prolonged drug therapy, especially from decrease BP or plasma sodium concentration
anticonvulsants and estrogens ● Accounts 20-25 % of the cardiac output
● Not addressing increased folic acid needs of certain
age groups URINARY TRACT INFECTION
● Ureters dilate from the effect of progesterone - urine
MAY CONTRIBUTE stasis/stagnation
● Early miscarriage ● Minimal glucosuria - growth of microorganisms
● Early separation of placenta
ASCENDING INFECTION
PREVENTION / MANAGEMENT - Caused by Escherichia coli
● 400 ug of folic acid daily before getting pregnant
● Folacin rich food: green leafy vegetables, oranges, DESCENDING INFECTION
dried beans - Streptococcus B
● During pregnancy: 600 ug/day
NAME: LOYOLA, MA. BERNICE C. 16
KERI PA BA NATIN???
ASSESSMENT ● Empty bladder at least every 2 hours ● Perineal
● Frequency and pain on urination hygiene from front to back
● Pain in the lumbar region
● Nausea and vomiting
● Malaise
● Temperature elevation
MATERNAL EFFECTS
● May lead to preterm labor
● Bacteremia causing septic shock
THERAPEUTIC MGT
● Urine C & S
● Administration of antibiotics
● Amoxicillin and ampicillin are safe to administer
TRIMETHOPRIM
● Antibiotic used mainly in the prevention and treatment
of urinary tract infections
● Folic acid antagonist (neutralizes the effect of another
drug)
● Must not be given on the first trimester
PREVENTION OF UTI
● Void frequently
● Wiping perineal area from front to back
● Wearing cotton underwear
● Voiding immediately after sexual intercourse
NURSING IMPLEMENTATIONS
● Advise 3-4L of water/day
● Knee chest position - to promote urine drainage
● Compliance to medications
CHRONIC RENAL DISEASE
● Results in accumulation of waste products in the
blood, electrolyte abnormalities and anemia
● CBC may indicate anemia
● May develop severe anemia
● Increased glomerular filtration rate / creatinine level
MEDICAL MANAGEMENT
● ACE inhibitor-preserves kidney function but fetotoxic
● Low dose aspirin
● Urine output monitoring
● Ultrasound every 2 weeks from 24 wks of gestation
● Non stress test
CARE OF THE WOMAN WITH CHRONIC RENAL
DISEASE
● If undergoing dialysis, peritoneal (removal of fluid
from the abdominal cavity) is more preferred - monitor
for preterm labor
● Nutrition consultation
● Emotional support
NURSING INTERVENTIONS
● Monitor I and O
● Evaluate degree of edema
● Make referral to a dietician
● Teach home blood pressure monitoring
● Teach pt signs and symptoms of preterm labor
● Educate on the importance of drinking variety of fluids
NAME: LOYOLA, MA. BERNICE C. 17
You might also like
- MCN Lec PMFDocument108 pagesMCN Lec PMFClaireNo ratings yet
- Programs, Trends, and Issues in Maternal HealthDocument20 pagesPrograms, Trends, and Issues in Maternal Healthanon_720827871No ratings yet
- MCN Lec - Prelims Reviewer 1Document15 pagesMCN Lec - Prelims Reviewer 1ClaireNo ratings yet
- M.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)Document3 pagesM.01 MNCHN (Part 1) (Dr. Hora) (03-04-21)VanessaNo ratings yet
- MCHN Midterm NotesDocument27 pagesMCHN Midterm NotesSeungwoo ParkNo ratings yet
- MCN Lec - 2ND SemDocument29 pagesMCN Lec - 2ND SemALYSSA NICOLE GINESNo ratings yet
- Philippines: At-A-Glance: PhilippinesDocument8 pagesPhilippines: At-A-Glance: PhilippinesGari LazaroNo ratings yet
- Acta Obstet Gynecol Scand - 2018 - Nyfl T - Strategies To Reduce Global Maternal MortalityDocument2 pagesActa Obstet Gynecol Scand - 2018 - Nyfl T - Strategies To Reduce Global Maternal Mortalityadelbertha aprianaNo ratings yet
- f.2 Policy Brief MMR GidaDocument4 pagesf.2 Policy Brief MMR GidaLeigh Chanelle OngNo ratings yet
- 109 Midterms TransesDocument28 pages109 Midterms TransestumabotaboarianeNo ratings yet
- Maternal Health in NigeriaDocument8 pagesMaternal Health in NigeriaprofangieNo ratings yet
- NCM 109 Lec PrelimsDocument12 pagesNCM 109 Lec PrelimsAngel Kim MalabananNo ratings yet
- WHO RHR 19.20 Eng PDFDocument4 pagesWHO RHR 19.20 Eng PDFElsa SembiringNo ratings yet
- MCN Reviewer 1STDocument10 pagesMCN Reviewer 1STAnthony Joseph ReyesNo ratings yet
- Part 2 MCHDocument30 pagesPart 2 MCHademabdella38No ratings yet
- MNCH-FINAL. 2023pptxDocument28 pagesMNCH-FINAL. 2023pptxpritaneionNo ratings yet
- Improve Maternal and Newborn Health and Nutrition: Facts, Solutions, Case Studies, and Calls To ActionDocument11 pagesImprove Maternal and Newborn Health and Nutrition: Facts, Solutions, Case Studies, and Calls To ActionMonika TanushevskaNo ratings yet
- Improve Maternal NutritionDocument14 pagesImprove Maternal NutritionRAHMI AYUDANo ratings yet
- Maternal Mortality - 0Document9 pagesMaternal Mortality - 0antidius johnNo ratings yet
- En SRH Fact Sheet LifeandDeathDocument5 pagesEn SRH Fact Sheet LifeandDeathbirolidiaNo ratings yet
- Healthy Mothers, Healthy Babies:: Taking Stock of Maternal HealthDocument12 pagesHealthy Mothers, Healthy Babies:: Taking Stock of Maternal HealthYurika Elizabeth SusantiNo ratings yet
- Unsafe Abortion: Unnecessary Maternal Mortality: W ' H D WDocument5 pagesUnsafe Abortion: Unnecessary Maternal Mortality: W ' H D WBhageshwar ChaudharyNo ratings yet
- SDG Briefing Note 4 - Maternal Mortality and Skilled Birth AttendanceDocument5 pagesSDG Briefing Note 4 - Maternal Mortality and Skilled Birth Attendanceambsheriff.nycdsierraleoneNo ratings yet
- Maternal Note 1Document34 pagesMaternal Note 1JAN REY LANADONo ratings yet
- Maternal (Well-Client) : Framework of Maternal and Child CareDocument3 pagesMaternal (Well-Client) : Framework of Maternal and Child CarealallaallalaNo ratings yet
- P.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Document3 pagesP.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Dasha VeeNo ratings yet
- Iles S. Normal Pregnancy and Antenatal Care. Essential Obstetrics and Gynaecology. 6th Ed2020. P. 82-92.Document11 pagesIles S. Normal Pregnancy and Antenatal Care. Essential Obstetrics and Gynaecology. 6th Ed2020. P. 82-92.Alhafiz KarimNo ratings yet
- Prenatal CareDocument8 pagesPrenatal CareChristine Evan HoNo ratings yet
- Indicators of Mother and Child Health Care. Maternal Mortality Rate, Mortality in Infancy and ChildhoodDocument37 pagesIndicators of Mother and Child Health Care. Maternal Mortality Rate, Mortality in Infancy and ChildhoodMonika shankar100% (1)
- MCHN PrelimDocument17 pagesMCHN PrelimantoynetteaNo ratings yet
- MCHN - Reproductive SystemDocument5 pagesMCHN - Reproductive SystemDOMINIQUE UYNo ratings yet
- Care of Mother and Child at RiskDocument2 pagesCare of Mother and Child at RiskJane CuencaNo ratings yet
- MCN Lec Group 1 Written ReportDocument51 pagesMCN Lec Group 1 Written ReportTrishNo ratings yet
- NOTES - Group 1 DOH PROGRAMSDocument18 pagesNOTES - Group 1 DOH PROGRAMSPatrisha Bianca Paige BadillesNo ratings yet
- LGT-9 Introduction To Child Health CareDocument26 pagesLGT-9 Introduction To Child Health CareMazinNo ratings yet
- Improving Perinatal and Neonatal Mortality in Sri Lanka: Is It Cost Effective?Document5 pagesImproving Perinatal and Neonatal Mortality in Sri Lanka: Is It Cost Effective?Vijayakanth VijayakumarNo ratings yet
- Obstetrics and Gynecology: in PH in Relation To Health CareDocument22 pagesObstetrics and Gynecology: in PH in Relation To Health Carejean de los santosNo ratings yet
- Evidence Based Approaches For Reduction of Maternal MortalityDocument44 pagesEvidence Based Approaches For Reduction of Maternal MortalityJalajarani Aridass100% (1)
- Skilled Birth Attendance-Lessons LearntDocument9 pagesSkilled Birth Attendance-Lessons LearntTriksha GeorgeNo ratings yet
- LESSON PLAN On Maternal Mortality and Morbidity FinalDocument17 pagesLESSON PLAN On Maternal Mortality and Morbidity FinalYerra SukumalaNo ratings yet
- d1-s2 Icrc Sok Imam - Nutrition StatusDocument25 pagesd1-s2 Icrc Sok Imam - Nutrition Statuscabdinuux32No ratings yet
- Philippine Government Policies On Maternal, Newborn and Child Health and NutritionDocument20 pagesPhilippine Government Policies On Maternal, Newborn and Child Health and Nutritioncarlos-tulali-1309100% (33)
- Maternal Health, ICPDDocument24 pagesMaternal Health, ICPDHadley AuliaNo ratings yet
- Framework of Maternal, Child Health Nursing Care: ObstareDocument40 pagesFramework of Maternal, Child Health Nursing Care: ObstareJohn CarloNo ratings yet
- Maternal Mortality and The Safe Motherhood Programme in Nigeria: Implication For Reproductive HealthDocument12 pagesMaternal Mortality and The Safe Motherhood Programme in Nigeria: Implication For Reproductive HealthArie Risdiana Asmita'No ratings yet
- Week 11 Framework For Maternal and Child Health Nursing Focusing On at Risk High Risk and Sick ClientsDocument15 pagesWeek 11 Framework For Maternal and Child Health Nursing Focusing On at Risk High Risk and Sick Clientss.tabaquin.edwardjrNo ratings yet
- EMONCDocument17 pagesEMONCJessie OranoNo ratings yet
- Chapter 3 Levels and Causes of MaternalDocument38 pagesChapter 3 Levels and Causes of MaternalFakhira Adzkiya SalsabilaNo ratings yet
- The Current Maternal and Child Health and Health NutritionDocument12 pagesThe Current Maternal and Child Health and Health NutritionGiselle EstoquiaNo ratings yet
- 5 - Maternal and Child Health MCV EditedDocument18 pages5 - Maternal and Child Health MCV Editedcantonecchi8142No ratings yet
- Final Proposal ExampleDocument7 pagesFinal Proposal ExampleRichel SuarezNo ratings yet
- The Safe Motherhood Initiative and Beyond: Monir IslamDocument1 pageThe Safe Motherhood Initiative and Beyond: Monir IslamCliveland RumondorNo ratings yet
- 11.21 - Maternal Health Status in The PhilippinesDocument7 pages11.21 - Maternal Health Status in The PhilippinesJøshua CruzNo ratings yet
- FeDocument7 pagesFeWilfredo PesanteNo ratings yet
- Lesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthDocument2 pagesLesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthA CNo ratings yet
- NCM 109 TransDocument26 pagesNCM 109 TransTherese Melchie SantuyoNo ratings yet
- CHN CH 4 Maternal and Child Care Including Bemonc and CemoncDocument5 pagesCHN CH 4 Maternal and Child Care Including Bemonc and CemoncElaiza RiegoNo ratings yet
- Maternal Health Programs: Monitoring and EvaluationDocument48 pagesMaternal Health Programs: Monitoring and Evaluationvikas takNo ratings yet
- The Therapy BookDocument398 pagesThe Therapy BookAbdelrahman Mamdouh90% (10)
- SSRI - MenyusuiDocument14 pagesSSRI - MenyusuirezkyagustineNo ratings yet
- Frequently Asked Questions: Weekly Iron Folic Acid Supplementation (WIFAS) For AdolescentsDocument16 pagesFrequently Asked Questions: Weekly Iron Folic Acid Supplementation (WIFAS) For Adolescentsdiana.alyNo ratings yet
- Gulf Care Members GuideDocument31 pagesGulf Care Members Guidesuheil samaraNo ratings yet
- Acute Care PT For Covid 19 PatientsDocument17 pagesAcute Care PT For Covid 19 PatientsSelvi SoundararajanNo ratings yet
- The Clear Skin Diet by Nina Nelson PDFDocument370 pagesThe Clear Skin Diet by Nina Nelson PDFmia agustina60% (10)
- Icf Pri P2 414 PDFDocument17 pagesIcf Pri P2 414 PDFMichael Forest-dNo ratings yet
- Review: How Old Is This Fracture? Radiologic Dating of Fractures in Children: A Systematic ReviewDocument5 pagesReview: How Old Is This Fracture? Radiologic Dating of Fractures in Children: A Systematic Reviewsigne_paoNo ratings yet
- Matas RationalizationDocument12 pagesMatas RationalizationCerezo, Cherrieus Ann C.No ratings yet
- Active Hexose Correlated Compound - Wikipedia, The Free EncyclopediaDocument7 pagesActive Hexose Correlated Compound - Wikipedia, The Free EncyclopedianurpeekNo ratings yet
- 2023 Music Therapy & NICUDocument36 pages2023 Music Therapy & NICUMohammad Izaan TahirNo ratings yet
- Hyperthermia (Thurs)Document1 pageHyperthermia (Thurs)Christine Esguerra OrozcoNo ratings yet
- Efficacy of Ethanol Against Viruses in Hand DisinfectionDocument9 pagesEfficacy of Ethanol Against Viruses in Hand DisinfectionImaec LimitedNo ratings yet
- Rheumatic FeverDocument61 pagesRheumatic FeverCostea CosteaNo ratings yet
- Most Common Ophthalmic Diagnoses in Eye Emergency Departments: A Multicenter StudyDocument8 pagesMost Common Ophthalmic Diagnoses in Eye Emergency Departments: A Multicenter StudyAlba García MarcoNo ratings yet
- F 16 CLINNeurologicalObservationChartDocument2 pagesF 16 CLINNeurologicalObservationChartRani100% (1)
- 3rd Mid CaseDocument32 pages3rd Mid CaseHarshini MakkenaNo ratings yet
- Bhandari MagneticDocument12 pagesBhandari MagneticrajanrathodNo ratings yet
- Test Bank For Basic Pharmacology For Nursing 17th EditionDocument10 pagesTest Bank For Basic Pharmacology For Nursing 17th EditionUsman HaiderNo ratings yet
- 322-Article Text-1656-1-10-20230630Document11 pages322-Article Text-1656-1-10-20230630Bunga nurmala septiaNo ratings yet
- Medsave - Claim Form For MediclaimDocument1 pageMedsave - Claim Form For Mediclaimpawan1501No ratings yet
- FASENRA - PFS To Pen Communication Downloadable PDFDocument2 pagesFASENRA - PFS To Pen Communication Downloadable PDFBrîndușa PetruțescuNo ratings yet
- Traumatic Tension Pneumothorax in Pediatric PatientDocument4 pagesTraumatic Tension Pneumothorax in Pediatric Patientadrif dzNo ratings yet
- Gabriel D. Vasilescu 68 Dorchester Road Ronkonkoma, Ny 11779Document3 pagesGabriel D. Vasilescu 68 Dorchester Road Ronkonkoma, Ny 11779Meg Ali AgapiNo ratings yet
- TTB Dtest SP-NT Deteclev 0409e2 PDFDocument3 pagesTTB Dtest SP-NT Deteclev 0409e2 PDFTairine AranhaNo ratings yet
- RG 241 Hospital Practice Correct 2018 2019Document10 pagesRG 241 Hospital Practice Correct 2018 2019Jude ChinecheremNo ratings yet
- Inspection Report - Texoma Medical Center TMC Behavioral Health CenterDocument2 pagesInspection Report - Texoma Medical Center TMC Behavioral Health CentermilesmoffeitNo ratings yet
- Jurnal AntibiotikDocument5 pagesJurnal AntibiotikSela PutrianaNo ratings yet
- Tanzania STG 052013-Copy 1544379670122Document220 pagesTanzania STG 052013-Copy 1544379670122Waqar WikiNo ratings yet
- Perinatal Care Manual 3rd Edition 2013Document251 pagesPerinatal Care Manual 3rd Edition 2013Anonymous 9dVZCnTXS100% (3)