Professional Documents
Culture Documents
The Effect of Gender On The Clinical Clerkship.13
Uploaded by
konkatelebeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Effect of Gender On The Clinical Clerkship.13
Uploaded by
konkatelebeCopyright:
Available Formats
Clerkships
The Effect of Gender on the Clinical Clerkship
Experiences of Female Medical Students:
Results From a Qualitative Study
Palav Babaria, Sakena Abedin, MD, MA, and Marcella Nunez-Smith, MD, MHS
Abstract
Purpose Results (5) encountered a “gender learning
To characterize how female medical Participants (1) struggled to define curve” on the wards that began to
students perceive the role of gender their role on the wards and often shape their self-view as future female
within their medical education during the defaulted to stereotypical gender roles, physicians.
transition to the clinical curriculum. (2) perceived differences in the nature
Conclusions
of their workplace relationships
Despite increased numbers of women in
Downloaded from http://journals.lww.com/academicmedicine by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdgGj2MwlZLeI= on 11/25/2021
Method compared with the nature of male
medicine, issues of gender continue to
In 2006 –2007, the authors conducted a medical students’ workplace
have a substantial impact on the medical
qualitative study consisting of in-depth relationships, (3) had gendered
education of female students. Institutions
interviews with 12 third-year female expectations of male and female
can design interventions about gender
medical students completing their first physicians that shaped their
issues in medicine that expand beyond a
clinical clerkship. Participants were interactions with clinical supervisors, (4)
focus on sexual harassment to address
purposefully selected from a single New felt able to negotiate uncomfortable the complex ways in which students are
England medical school to represent a situations with patients but felt unable affected by issues of gender.
range of ages, ethnicities, and prior life to negotiate uncomfortable situations
experiences. with supervisors and attendings, and Acad Med. 2009; 84:859–866.
Close to fifty percent of all medical members revealed an average base salary response to such experiences. When
school matriculates in the United States deficit for female physicians of $11,691 interviewed, women in academic medicine
are women, and the number of women compared with male colleagues, and the also frequently cite the lack of equitable
entering medical school continues to deficit increased with seniority. mentorship as one of the major barriers to
increase.1 Most of the existing research career advancement.
about women in medicine, largely limited In addition to such career advancement
to female physicians posttraining, has considerations, up to 70% of female Qualitative studies have also previously
demonstrated that gender often negatively faculty report gender-based discrimination described the potentially negative impact
influences their professional experiences. and sexual harassment.7–9 A study in 2000 of gender on the professional relationships of
Prior studies have shown that women in interviewed both male and female female physicians. Female physicians
academic medicine are underrepresented academic physicians regarding perceived have described tension with female
at the professorial rank and are gender discrimination and found nurses in the workplace, resulting from
compensated less than are their male statistically significant differences (P ⬍ what they perceive to be differential
colleagues even after adjusting for .001) between the experiences of male treatment of male and female physicians.11,12
academic productivity.2–5 Ash et al’s6 and female physicians.7 Forty-eight Female physicians perceived that
2004 study surveying 1,814 female faculty percent of female physicians reported they had to be “nicer” and more
having experienced sexist comments or “accommodating” to nursing staff and
behavior (compared with 1% of male also received less technical assistance
colleagues), and 30% reported experiencing caring for patients and cleaning than did
Ms. Babaria is a fourth-year medical student, Yale severe harassment, such as sexual their male colleagues.12
University School of Medicine, New Haven,
solicitation, threats, or coercive sexual
Connecticut.
advances (compared with 3% of male The consistency of the findings across the
Dr. Abedin is a graduate student, Program in the colleagues).7 These experiences are existing research literature has triggered
History of Science and Medicine, Yale University,
New Haven, Connecticut. associated with other important outcomes, the development of numerous policies
such as low career satisfaction.7,10 Carr and programs to increase the support of
Dr. Nunez-Smith is assistant director, Yale
University Robert Wood Johnson Clinical Scholars
et al’s8 in-depth 2003 qualitative study women in medicine during the past 15
Program, and assistant professor, Department of examined the effect of gender years. Many universities have established
Internal Medicine, Yale University School of discrimination on the experiences of female offices of Women in Medicine to assist
Medicine, New Haven, Connecticut. faculty. Participants who had experienced female faculty and students in addressing
Correspondence should be addressed to Ms. gender discrimination reported lower self- gender bias, instituted mandatory sexual
Babaria, Yale University School of Medicine, IE-61 harassment trainings, and increased
confidence and self-esteem, cynicism
SHM, PO Box 208088, New Haven, CT 06520-8088;
telephone: (203) 785-6454; e-mail: (Palav.babaria@ towards their academic work environment, efforts to recruit more female faculty who
yale.edu). isolation, and a lack of institutional can serve as role models for female
Academic Medicine, Vol. 84, No. 7 / July 2009 859
Clerkships
medical students in addition to national surveys have clearly documented institutional human investigation
diversifying the faculty.2,13 that female medical students report committee. We obtained signed consent
gender bias at significantly higher rates from all participants.
Although research into the professional than do their male peers, but they do not
experiences of practicing female provide any further insight into the range Data collection
physicians has been comprehensive, less of experiences attributed to gender that
From June 2006 to June 2007, in addition
is known about the experiences of female female medical students may have.
to a baseline interview conducted prior to
medical students. The majority of research
Given the increasing numbers of women starting their third year and an exit
involving female medical students has
in medicine and the substantial policy interview at the completion of their third
focused on rates of medical student abuse
changes to support gender diversity in year, we interviewed our cohort of 12
and sexual harassment.14 –17 In Nora et
medicine, understanding the influence of female medical students after the
al’s14 14-school survey from 2002, 83% of
gender on the experiences of the next completion of each 4- or 6-week clinical
female medical students reported having
generation of female physicians is clerkship. This current analysis focuses
experienced gender discrimination in a
paramount. Therefore, we conducted a only on interviews describing the
variety of clinical and nonclinical
qualitative study of female medical experiences of subjects after their first
settings. Such experiences were most
students transitioning from a preclinical month of clinical clerkships given the
prevalent in university hospitals and on
to a clinical curriculum in order to unique experiences that participants
core clerkships (notably surgery and
characterize how gender influences their reported during their initial encounters
obstetrics– gynecology). Several studies
training experience. with clinical medicine. Future analyses
have documented that both male and
will examine participant perspectives
female students report significantly
throughout the clinical year. One
higher rates of gender discrimination in
Method member of the research team (P.B.)
their clinical clerkships than during the
Study design and sample conducted all interviews; the interviewer
first two years of medical school,14,18,19
was a female medical student doing
suggesting that the structure of clinical We conducted in-person, in-depth clinical clerkships at the time of the
education, as well as interactions on the interviews with 12 female third-year interviews. We purposefully chose to
wards, lend themselves to greater rates of medical students to characterize their have a single interviewer who was
gender-based discrimination compared gender-related experiences during the gender- and role-concordant with the
with classroom learning. Interestingly, first month of clinical clerkships. To interviewees, as similarities between
studies that have further examined ensure the anonymity of the limited researchers and key informants, such as
what students mean by “gender number of participants, we have chosen gender or work role, can often facilitate
discrimination” and “sexual harassment” not to identify the name of the institution rapport and therefore yield rich data.14,23,24
suggest that students actually perceive less within the text. We used a qualitative All interviews were conducted in-person,
gender discrimination and harassment as methodological approach because we with only the interviewer and a single
they progress through medical school, sought to generate hypotheses regarding participant present, and averaged 35
likely because of acculturation.20 As Nora how gender affects the experiences of minutes. Audiotaped interviews were
et al20 hypothesize in a 1993 study, female medical students that would transcribed, and transcripts were verified
“Perhaps people ‘buy into’ certain provide better understanding of previous by the interviewer. Interviews started
settings for their own psychic survival quantitative surveys.21 Only females were with the general question, “What do you
and/or to increase the likelihood of considered for participation in this study, think the impact of gender has been, if
their success. In these instances, the as it specifically examines the experiences any, on your experiences on the wards
organizational culture is accepted over of women in medicine. In addition, during the past rotation?” Follow-up
time.” Wear et al’s17 2007 qualitative students who did not intend to complete probes then examined the participants’
study looked specifically at the an entire year of clinical clerkships were views regarding interactions with
perceptions of sexual harassment among excluded from the study, as this study patients, medical staff, and other medical
contemporary female medical students. was part of a longitudinal cohort study. students. Additional questions asked
Participants reported frequent “sexual
participants about the impact of gender
innuendo, explicit sexual banter, or crude We identified and recruited a purposeful
on educational learning and about
language”; however, as Wear wrote, “not sample of female medical students, paying
participants’ views on male medical
one of the students we interviewed particular attention to characteristics such
students’ experiences (List 1).
went so far as to label any of it ‘sexual as age, self-identified racial/ethnic
harassment,’ even after our initial background, prior life experiences, non-
definition was read to them prior to each English primary language, undergraduate Data analysis
focus-group.” institution, and relationship status.22 Two Given that our objective was to generate
invited students declined to participate themes that are germane to health services
Given that many students seem to shy (one student cited time constraints, and research, we applied the principles of
away from using the terms “sexual the other expressed concerns about the inductive reasoning to guide our data
harassment” and “gender discrimination,” potentially negative impact of participating in analysis and interpretation.25 A diverse
targeted questionnaires may fail to the study on her future career), so two coding team comprising a medical
capture the full extent to which female other students were identified and student, an internist, and a pediatrician,
medical students experience such recruited to replace them. The research representing a variety of racial/ethnic and
behavior. Despite this shortcoming, protocol was approved by the religious backgrounds, developed an
860 Academic Medicine, Vol. 84, No. 7 / July 2009
Clerkships
Five common and original themes
List 1 characterized the experiences of third-
Standard Guide for Interviews Conducted With 12 Female Third-Year Students at year female medical students during their
One New England Medical School, 2006 –2007 first month of clinical clerkships. Female
medical students (1) struggled to define
● Do you think gender and issues of gender have impacted your experiences on the wards? If so, how?
their place on the wards and often
● How have these experiences impacted your learning on the wards?
defaulted to stereotypical gender roles,
● Please describe any specific incidents that you experienced or observed in which gender played a role.
(2) perceived differences in the nature of
● Do you think your experiences on the wards have differed from those of men in your class? If so, how?
their workplace relationships compared
with male medical students’ workplace
initial code structure based on a was used to assist with data management relationships, (3) had gendered expectations
preliminary reading of three randomly and retrieval. All participants reviewed a of male and female physicians that shaped
chosen transcripts. The code structure summary of the themes after data analysis their interactions with clinical
then evolved in an iterative process. The was completed, and they endorsed the supervisors, (4) felt able to negotiate
code team met regularly to revise and content of the findings.27 uncomfortable situations with patients
refine the code structure using the but felt unable to negotiate
constant comparative method of data uncomfortable situations with
analysis. Newly coded text was compared Results supervisors, and (5) encountered a
with previously coded text to identify “gender learning curve” on the wards
new themes and expand existing themes We interviewed 12 female medical
students after the first month of their that began to shape their self-view as
on the code structure.26 future female physicians.
third-year clinical clerkships, representing a
Transcripts were independently line-by- range of ages, race/ethnicities, and prior Female medical students often defaulted
line coded by code team members using life experiences (Table 1). Students to stereotypical gender roles as they
the final code structure that comprehensively participated in one of seven different struggled to define their place on the
defined all codes. The code team had clinical specialty clerkships across a wards
group meetings at regular intervals to variety of clinical settings. There were
reconcile differences between coded often several participants per clerkship, Most participants expressed confusion
transcripts by negotiated consensus.27 representing different hospitals and during the first month of clinical
Scientific software, ATLAS.ti 5.0 (Berlin), clinics. rotations about the third-year medical
student role, describing it as “a difficult
transition” and “awkward.” One
participant described her first rotation as
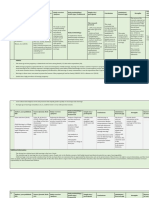
Table 1 “crazy” with the concomitant transition
Characteristics of 12 Female Third-Year Students at One New England Medical of residents. She questioned,
School Participating in a Qualitative Study of the Effect of Gender on Clinical
Clerkship Experiences, 2006 –2007 What is the role of the medical students
in that environment? Because I’m there to
Characteristic No. (%)
learn, and to work with patients . . . but
Median age (range), in years 25 (23–30) when I don’t know what I’m doing, it’s
hard for me to do that for patients. So . . .
Race
......................................................................................................................................................................................................... I think that has been sort of challenging
White 9 (75) (Emergency Medicine/Anesthesiology).
.........................................................................................................................................................................................................
Black 2 (17)
.........................................................................................................................................................................................................
Asian 1 (08) Many female medical students were
Marital status
surprised to find themselves defaulting to
......................................................................................................................................................................................................... self-described stereotypically feminine
Single 5 (42)
......................................................................................................................................................................................................... behaviors within this period of
In a relationship 5 (42) uncertainty, such as focusing on assisting
.........................................................................................................................................................................................................
Married 2 (17) nursing or support staff, nurturing
Parent 1 (8) patients, or becoming more apologetic.
Undergraduate education completed at a single-sex institution 2 (17) Whether participants viewed these
behaviors positively or negatively varied
Took time off before coming to medical school 7 (58)
......................................................................................................................................................................................................... depending on who was involved in the
Median gap in years (range) 2 (1–6) interaction. Most students who identified
Month 1 clerkship “feminine” behavior during interactions
.........................................................................................................................................................................................................
Emergency medicine and anesthesia 3 (25) with their residents and attendings
.........................................................................................................................................................................................................
Medicine 2 (17) described those situations negatively. One
......................................................................................................................................................................................................... participant, when asked how gender
Neurology 1 (8)
......................................................................................................................................................................................................... affected her interactions on the wards,
Obstetrics–gynecology 1 (8)
......................................................................................................................................................................................................... expressed surprise at how “apologetic”
Pediatrics 2 (17) she found herself in interactions with her
.........................................................................................................................................................................................................
Psychiatry 2 (17) clinical team. She would ask, “I’m sorry,
.........................................................................................................................................................................................................
Surgery 1 (8) did I do that right? Did I do this right? Is
Academic Medicine, Vol. 84, No. 7 / July 2009 861
Clerkships
this how you want this done?” As she from her like in a half hour standing in Gendered expectations of male and
explained, “I didn’t take as much the middle of this patient’s room. I don’t female physicians shaped how female
initiative as I thought I would, and to me, know if that would have happened if I medical students interpreted their
to me it was very clear that I was doing were a guy—it probably wouldn’t have” interactions with clinical supervisors
that because I felt like . . . I didn’t fit in” (Internal Medicine). Many female students described having
(Surgery). Another participant described low expectations of encounters with male
a similar situation in which she and a Several participants felt that, though supervisors on the wards and anticipated
male medical student incorrectly they formed relationships with the that such interactions would be
performed an EKG on a patient: predominantly female nursing and uncomfortable. For instance, several
support staff, their male classmates were students reported having had anxiety
Then we had to come and do it again
forming relationships with attendings, regarding the potential of working with
and. . .. And I was the one apologizing
about how we put the leads on wrong and who were most often male. Some all-male teams and expressed surprise
really it wasn’t—we put the leads on as a participants felt they were at a disadvantage when they had good learning experiences
team, me and [the male medical student] because of the difference in quality with male physicians. One student
. . . but because I was the one apologizing between the relationships they formed thought she “would feel uncomfortable at
about it the patient remembered me as with attendings and those formed by times” when she discovered that she was
the one that messed up the EKG (Internal
Medicine).
their male counterparts. One student of working with all-male attendings and
color felt that it was “harder [to] relate to residents on her psychiatry rotation. As
In contrast, participants who exhibited older white men and have an interaction, she described, however, “Not at all . . .
self-described stereotypically feminine attachment and relationship . . . because some people, especially older men, tend
behavior during interactions with we don’t have much in common.” She to still believe that women have these
patients and support staff reflected on felt that finding similarities with defined roles, but, yeah, [the male
those such situations positively, describing attendings was a “big part of evaluations attendings and residents] basically
themselves as “helpful” and and . . . being included in procedures” showed me otherwise, throughout the
“appreciated.” One participant explained (Emergency Medicine/Anesthesiology). whole rotation, I mean everybody.”
that her “ability to be caring and
Some participants also felt that, in Participants described their encounters
nurturing has been really helpful,”
addition to forming closer relationships with male physicians in laudatory terms
especially with elderly female patients
with male students, attendings also had when their experiences surpassed their
(Emergency Medicine/Anesthesiology).
different expectations for male and relatively low expectations. One participant
Another participant on her surgery
female medical students. One participant “found the residents who were often the
clerkship described similar satisfaction
on her surgical rotation initially felt better teachers were the male residents.”
assisting support staff:
grateful that she was not being asked As she explained, “[They] were the ones
The good moments . . . mostly moments questions. However, she soon realized who sort of pushed me to do things
where I felt really helpful . . . I would do “that I just wasn’t being pushed to read more, and who were friendlier and gave
something stupid, like pick up a piece of
because I wasn’t being asked questions.” me more feedback, and encouraged me
paper off the floor and some tech would to also sort of be more comfortable”
smile at me. And those were the days that She described a “stark difference”
(Obstetrics–Gynecology). Another
I would feel good about myself. between herself and the male medical
participant expressed similar views, that
student on the rotation, explaining that
“males push you harder, they act more
Female medical students perceived her team was “asking him all the . . .
confidently, they ask you more questions,
differences in the nature of their questions so that he’d get all the right
and they expect you to know more.” She
workplace relationships compared with answers.”
concluded, “I want male attendings, I
male medical students’ workplace
want male residents. I don’t want to have
relationships Some participants thought these differential
female residents anymore because I don’t
Participants perceived substantive relationships and expectations would have
think I’d learn as much if I had females”
differences between the types of ramifications on their future careers. As (Neurology).
relationships they formed on the wards expressed by one participant,
compared with relationships formed by In contrast to their stated apprehension
their male counterparts. Many participants I think the outcome of this is going to be about working with male teams, many
that the relationships and bonds that I’ve
described forming closer bonds with participants expressed excitement about
formed in this year are going to be very
support and nursing staff than with their much, ones of—where I feel like I’m possibly working with female role models
clinical supervisors. One participant supporting female interns and nurses, and during clinical clerkships. One participant
described an encounter with a nurse that the males in my class are going to described working with almost
“who’s notoriously antagonistic with come out with a lot of powerful exclusively female residents during her
doctors.” When the student assisted the relationships with people who are going anesthesiology rotation. She spoke of her
nurse in moving a patient, the nurse to write them recommendations for “great interactions” with them and being
future powerful positions . . . it’s kind of
“flipped in a heartbeat,” confiding in the able to talk about “how they balance their
important . . . And it’s really shown me,
student about her daughter’s struggle this past month, how easy it is to get career with the rest of their life.” In
with an eating disorder. The participant ahead when you’re a man. It’s not that I some situations, students found that
attributed this interaction to her gender, didn’t know that already, it’s just made it relationships with female supervisors
stating, “And I just got this whole story more clear (Surgery). fulfilled their expectations and were very
862 Academic Medicine, Vol. 84, No. 7 / July 2009
Clerkships
rewarding. For example, one student on patients flirting, making remarks about navigating uncomfortable situations with
psychiatry described dealing with an participants’ appearance or gender, or attendings and residents who were their
inappropriate patient: “The [female calling participants “nurse.” One student supervisors. Such students often deferred
clinical supervisor] . . . and I both had described feeling “uncomfortable and to what they perceived to be the existing
this very, very, strong reaction that he frustrated and angry” when being culture, despite their discomfort. One
was this very sleazy guy. . .. I actually had referred to as “nurse.” She explained, student described her interactions with
some really good discussions with her an attending:
There is absolutely no reason why
about that.”
someone who is female would not be able It’s pretty freakin cold in the OR and I
to care for, think hard enough, or put in would get goose bumps and [the male
Some students also related specific as many hours— or whatever they think attending] would rub the back of my
expectations that they had for female would limit a woman to the point where arms with his hand, and then he got the
supervisors that were often based on “warm you wouldn’t assume she was a doctor. . .. resident doing it too, it was just a little
and fuzzy” female stereotypes. Students I feel like . . . it undermines what I’ve put strange, I have to admit, and I was like
expressed surprise and sometimes criticism in to get there (Pediatrics). “Huh. . . . How do I deal with this?” I’ve
when female supervisors did not fulfill never had anyone rub my arm for goose
Many students reported feeling bumps. . .. Would I have preferred that it
these expectations. As one student on her comfortable addressing inappropriate didn’t happen? Absolutely. It’s not exactly
pediatrics rotation described, patient behavior by the end of their first that I asked for, wanted, or solicited in
clerkship experience. One student described anyway, but did I feel comfortable saying,
I did notice though, that the women . . .
addressing older men who had “more old- “Could you please not do that?” I mean it
they were very sharp, very professional . . .
was my first week of rotations, I didn’t
put together and they didn’t have that fashioned views of women and the roles
know what was appropriate at that time . . . so
stereotypical warm and fuzzy mode about of women”: “I make it very clear upfront I didn’t say anything (Emergency
them. . .. And that wasn’t what I was that I’m a medical student—not a nurse, Medicine/Anesthesiology).
expecting at all. . .. And that was difficult
not an assistant” (Emergency Medicine/
for me to adjust to initially. I didn’t find
them very approachable. The men that Anesthesiology). Female medical students encountered a
were that way, I would approach them the gender learning curve on the wards that
same, but for the women it was sort of Despite describing many male supervisors as
began to shape their self-view as future
startling and a bit intimidating and I was “better teachers,” a majority of students
female physicians
less willing to approach them and start also reported that most uncomfortable
building some sort of relationship but it situations they encountered on the wards Some female medical students also began
took much longer for me to feel involved male residents or attendings. to identify what sort of behavior was
comfortable around a woman with that required of female physicians based on
Such situations ranged from feeling
sort of presence (Pediatrics). their experiences. We termed this type
uncomfortable in a male-dominated
culture to unsolicited attention from of learning on the wards the “gender
Almost all students described some learning curve” to describe the process of
male residents and attendings. One
disappointment in their encounters with identifying and responding to workplace
student described the “culture of
female residents and attendings. One gender roles. Students perceived that
guyness” she experienced on the wards
student contrasted her experience with there were higher workplace expectations
that she felt was often unrecognized by
male and female physicians, explaining for female physicians and felt that the
male attendings and residents:
that the males were “more attentive” and medical environment required women
that the two female attendings “basically Just today we had this conversation about to be “more serious” and “prove”
didn’t acknowledge my presence.” some male patient who was found themselves. One student felt that male
Another student expressed surprise when masturbating by the attending. And so
physicians “joke around more” and
she, too, concluded that she “liked a lot ensued five minutes of jokes about
masturbation—I mean male “seem more accessible.” In contrast, she
of the male residents better than the felt that many female physicians “seemed
masturbation and basically all the men
female residents.” As she described, “I laughing and all the women standing just a lot colder.” She attributed such
sort of had this moment when I realized, back— even though we were all standing differences to her perception that “women
yeah, I like this resident, I like this one, I in a circle. I mean . . . that’s pretty explicit have to be more serious because they
don’t like this one so much and then I (Surgery).
have to command more respect and the
realized, wow, in general I’m liking the men get it more automatically and so
men more and that’s really weird to Another student described her
interactions with a male attending in they’re freer to joke around (Obstetrics–
me. . .. I didn’t expect that” (Obstetrics– Gynecology).” Another student expressed
Gynecology). more blunt terms:
similar views after two weeks on
Dr. [Y] stared at every girl’s chest. And pediatrics, that “male doctors had this air
Female medical students felt able to nobody ever said anything about it. He of, they had a right to be doctors . . . and
negotiate uncomfortable situations with wouldn’t look you in the face, he would females had to prove that they were going
patients but felt unable to negotiate look at your chest when he was talking to
to be, should be doctors . . . it was harder
uncomfortable situations with you. . .. And he did it to every girl, every
single female (Neurology). for women to prove that” (Neurology).
supervisors and attendings
Most female medical students experienced a Some participants explained that their Some participants described what they
range of uncomfortable situations during unfamiliarity with the medical system perceived as necessary behavior for female
the first month. Uncomfortable and medical culture during their first physicians. One participant observed how
situations with patients usually involved month of rotations prevented them from her female attending “never talked about
Academic Medicine, Vol. 84, No. 7 / July 2009 863
Clerkships
her personal life except to say that it was workplace interactions that are affected school that isolate such students.31,32
her son’s birthday.” As the participant by gender. In addition, they perceive Strategies that solely address issues of
concluded: “She was so professional, these interactions to differ substantially sexual harassment in undergraduate
always talking about intelligent things. from the workplace interactions of their medical education often fail to address
And I think that was something that I male classmates. These findings have these cultural phenomena. Adopting
realized is necessary, when you’re a important implications, because targeted more comprehensive programs that
female doctor” (Neurology). interventions to date have primarily examine the gendered culture within
focused on recruiting and supporting medicine may improve the experiences of
Several participants described feeling that female faculty and developing policies on women in medicine.
they, too, had to “prove” that they were sexual harassment.2,13 Our data reveal
competent, as compared with their male that although female medical students Our participants also described being
counterparts. One participant described mentioned sexual harassment, these unprepared to address most of the
feeling nervous about “proving that I’m experiences were neither as pervasive nor uncomfortable situations they faced on
just as good or just as smart.” As she as formative as other gender-related the wards. Previous work with female
explained, experiences that shaped their clerkship faculty has shown that women who felt
rotations and ideas about women in unequipped to deal with gender
I just want to make sure that I don’t
medicine. discrimination reported its effects on
end up looking like one of the female
residents who doesn’t know anything and their self-confidence, isolation, and
doesn’t have any confidence. I don’t want Our findings suggest that female students, in career development as well as regrets
to look like that. Seeing [female resident] addition to the clinical learning curve well about choosing to enter medicine.10,33
makes me want to not be like her associated with third-year clerkships, also Similar patterns with female medical
(Neurology). encounter a “gender learning curve.” students suggest that this process starts
The curve reflects acculturation to earlier than residency or practice. If
Some women felt that based on their stereotypical male and female workplace medical institutions want to create equal
experiences, they would not be able to roles and expectations. Similar to prior opportunities for women in medicine,
meet the demands of being a woman in studies,28 our participants described interventions will need to be targeted
medicine. As one student who is also a being especially vulnerable and struggling earlier.
mother described, to define their place on the wards during
I came in thinking you know, whatever I their first clerkship. Particularly when The findings of this study do have some
want I’ll do. And now it’s like, no. I want facing uncomfortable situations with limitations. All of the participants hailed
an easy residency, easy 10 years of practice attendings or supervisors, participants from a single medical school class at a
and then I’ll do—if I’m not satisfied, then often felt unsure of how to react and private, New England medical school.
I’ll do something different. It’s such a accepted what they perceived to be the Some of the findings may reflect the
shame. I think it’s a shame because I prevailing workplace culture as the norm. experiences of this particular class and
remember going to the Women in Medicine
talk and they’re like—someone was like,
Such impressionability during the first the policies of this school and may not
“I’m not practicing,” and I remember clinical clerkship may accentuate the be generalizeable to other parts of the
thinking this is ridiculous. And now I’m . . . gender learning curve. country or public institutions. However,
in the same position and I’m not like, we purposefully sampled a diverse group
“I’m not practicing,” but . . . my career is Our findings reveal that many aspects of of students representing a range of
determined by my kids and my family at female medical students’ experiences are specialties, hospitals, and clinics to
this point. So it’s, I think it’s really
affected by gender, including interpersonal minimize such variations in institutional
interesting that two years ago I thought
whatever the world had to offer I could relationships, career ambitions, and culture. Future work involving interviews
take it on and now I know I can’t do it behavior on the wards. A number of with male medical students would
(Psychiatry). participants reflected on the “culture of complement this study, providing a point
guyness” on the wards and felt that the of comparison between the experiences
culture of medicine valued stereotypically of male and female medical students.
Discussion male characteristics more than female Comparing male and female perspectives
Although significant attention has been characteristics. Multiple studies have would have allowed us to determine
paid to supporting gender diversity in documented that female medical students whether some of our participants’ experiences
the physician workforce, we found that have higher rates of medical school were due to their role as medical students,
gender has a substantial impact on the attrition than their male classmates29 and in addition to issues of gender. If male
experiences of female medical students as report significantly more doubt about perspectives revealed differences in
they start their clinical clerkship training. whether they should have chosen to enter the way male and female students
Perhaps surprisingly, participants described the field of medicine.30 The experiences characterize gender dynamics in medical
both positive and negative gender-related that our participants report may only education, it would further support our
experiences that extended far beyond exacerbate the doubt and isolation that findings. In addition, assessing whether
issues of sexual harassment in the many female medical students feel. Prior male students are aware of the gender
workplace. Regardless of previous life work done on the experiences of both differences that their female peers
experiences, specialty rotation or female and racial/ethnic minority perceive would provide valuable insight
clerkship site, several themes emerged students has focused on the role of the for medical educators. Strengths of this
from the data that suggest female medical culture of medicine and the hidden study include gender- and role-
students share a commonality of curriculum components of medical concordant interviewing, the diversity of
864 Academic Medicine, Vol. 84, No. 7 / July 2009
Clerkships
the coding team, the use of rigorous be actively discussed and counteracted. 7 Carr PL, Ash AS, Friedman RH, et al. Faculty
qualitative methodologies such as Given that students often do not approach perceptions of gender discrimination and
sexual harassment in academic medicine.
audiotaping and transcription, and administrators to discuss such issues, Ann Intern Med. 2000;132:889 – 896.
participant verification of findings. programs might consider creating 8 Carr PL, Szalacha L, Barnett R, Caswell C,
frequent “check-ins” with students to Inui T. A “ton of feathers”: Gender
This study has numerous implications provide a structured opportunity for discrimination in academic medical careers
for medical educators and clerkship student–faculty discussion. and how to manage it. J Womens Health
(Larchmt). 2003;12:1009 –1018.
directors. As these results demonstrate, it 9 Komaromy M, Bindman AB, Haber RJ,
is necessary to expand the framework of In our study, female students also felt that Sande MA. Sexual harassment in medical
gender discrimination beyond sexual male colleagues formed consequentially training. N Engl J Med. 1993;328:322–326.
harassment to include the myriad ways in different relationships with male attendings. 10 Corbie-Smith G, Frank E, Nickens HW, Elon
which gender affects the lives of female Instituting evaluation systems that L. Prevalences and correlates of ethnic
harassment in the U.S. Women Physicians’
medical students. Programs that only provide for 360-degree evaluations, Health Study. Acad Med. 1999;74:695–701.
focus on prevention of or responses to where not only attendings, but patients, 11 Gjerberg E, Kjolsrod L. The doctor–nurse
sexual harassment do not address the nurses, and support staff provide student relationship: How easy is it to be a female
more subtle forms of gender stereotyping evaluations, would more doctor co-operating with a female nurse? Soc
experienced in the early years of medical comprehensively assess the performance Sci Med. 2001;52:189 –202.
12 Wear D, Keck-McNulty C. Attitudes of
training. of all students. female nurses and female residents toward
each other: A qualitative study in one U.S.
Interestingly, this study revealed a number of Lastly, longitudinal qualitative work is teaching hospital. Acad Med. 2004;79:291–
potential contradictions in the needed to examine the range of experiences of 301.
female medical students over time. Such 13 American Medical Association. Addressing and
perspectives of our female medical Preventing Sexual Harassment in Medicine.
student participants. Students described work would identify patterns of the Available at: (http://www.ama-assn.org/ama1/
discomfort with a “culture of guyness” impact of gender and lead to more pub/upload/mm/19/sexualharassreport.pdf).
and reported uncomfortable situations effective interventions that extend Accessed March 12, 2009.
typically involving male clinical beyond sexual harassment to address the 14 Nora LM, McLaughlin MA, Fosson SE, et al.
entirety of female medical students’ Gender discrimination and sexual harassment
supervisors, yet they credited male in medical education: Perspectives gained by
physicians with often being better experiences. a 14-school study. Acad Med. 2002;77(12 pt
teachers. Conversely, students often 1):1226 –1234.
wished to work with more female 15 Richman JA, Flaherty JA, Rospenda KM,
Disclaimer Christensen ML. Mental health consequences
supervisors, but they almost universally
The authors received funding from the Yale and correlates of reported medical student
reported disappointing experiences with abuse. JAMA. 1992;267:692– 694.
University School of Medicine Office of Student
female attendings and residents. These Research and the Yale University School of 16 Stratton TD, McLaughlin MA, Witte FM,
seemingly paradoxical viewpoints likely Medicine Office of Education. The funding Fosson SE, Nora LM. Does students’
result from the varying expectations sources played no role in the design of the study, exposure to gender discrimination and sexual
harassment in medical school affect specialty
students have of male and female the collection, analysis, and interpretation of the
data, or the decision to approve publication of choice and residency program selection? Acad
supervisors in the workplace. All of our Med. 2005;80:400 – 408.
the finished manuscript. The corresponding
participants described relatively low 17 Wear D, Aultman JM, Borges NJ.
author also had full access to all of the data in the
expectations for interactions with male study and takes responsibility for the integrity of
Retheorizing sexual harassment in medical
supervisors compared with female education: Women students’ perceptions at
the data and the accuracy of the data analysis. five U.S. medical schools. Teach Learn Med.
supervisors. Participants reflected on Winter 2007;19:20 –29.
these differential expectations, 18 Baldwin DC Jr, Daugherty SR, Eckenfels EJ.
commenting on how women in medicine References Student perceptions of mistreatment and
are expected to be “more serious” and 1 Barzansky B, Etzel SI. Medical schools in the harassment during medical school. A survey
“prove” themselves, resulting in United States, 2006 –2007. JAMA. 2007;298: of ten United States schools. West J Med.
1071–1077. 1991;155:140 –145.
female supervisors who are often 19 Richardson DA, Becker M, Frank RR, Sokol
2 Bickel J. Gender stereotypes and misconceptions:
unapproachable and off-putting to Unresolved issues in physicians’ professional RJ. Assessing medical students’ perceptions of
students. Participants also described strict development. JAMA. 1997;277:1405, 1407. mistreatment in their second and third years.
and narrow expectations they had of 3 Carr PL, Friedman RH, Moskowitz MA, Acad Med. 1997;72:728 –730.
Kazis LE. Comparing the status of women 20 Nora LM, Daugherty SR, Hersh K, Schmidt J,
female physicians, such as being “warm
and men in academic medicine. Ann Intern Goodman LJ. What do medical students
and fuzzy,” that made it difficult for Med. 1993;119:908 –913. mean when they say “sexual harassment”?
female supervisors to meet these 4 Nonnemaker L. Women physicians in Acad Med. 1993;68(10 suppl):S49 –S51.
expectations. academic medicine: New insights from 21 Malterud K. The art and science of clinical
cohort studies. N Engl J Med. 2000;342:399 – knowledge: Evidence beyond measures and
405. numbers. Lancet. 2001;358:397– 400.
The number of negative encounters that 22 Patton MQ, Patton MQ. Qualitative Research
5 Peterson NB, Friedman RH, Ash AS, Franco
female students reported with female S, Carr PL. Faculty self-reported experience and Evaluation Methods. 3rd ed. Thousand
supervisors also suggests levels of with racial and ethnic discrimination in Oaks, Calif: Sage Publications; 2002.
internalized sexism resulting in students academic medicine. J Gen Intern Med. 2004; 23 Edwards R. Connecting method and
devaluing female attendings. These views 19:259 –265. epistemology: A white woman interviewing
6 Ash AS, Carr PL, Goldstein R, Friedman RH. black women. Womens Stud Int Forum.
may also complicate female mentorship Compensation and advancement of women 1990;13:477– 490.
programs and gender-concordant team in academic medicine: Is there equity? Ann 24 Wilde V. Controversial hypotheses on the
interactions. These perceptions need to Intern Med. 2004;141:205–212. relationship between researcher and
Academic Medicine, Vol. 84, No. 7 / July 2009 865
Clerkships
informant in qualitative research. J Adv Nurs. 28 Seabrook MA. Clinical students’ initial 31 Dyrbye LN, Thomas MR, Eacker A, et al.
1992;17:234 –242. reports of the educational climate in a Race, ethnicity, and medical student well-
25 Bradley EH, Curry LA, Devers KJ. Qualitative single medical school. Med Educ. 2004;38: being in the United States. Arch Intern Med.
data analysis for health services research: 659 – 669. 2007;167:2103–2109.
Developing taxonomy, themes, and theory. 29 Fitzpatrick KM, Wright MP. Gender 32 Lempp H, Seale C. Medical students’
Health Serv Res. 2007;42:1758 –1772. differences in medical school attrition rates, perceptions in relation to ethnicity and
26 Miles MB, Huberman AM. Qualitative Data 1973–1992. J Am Med Womens Assoc. 1995; gender: A qualitative study. BMC Med Educ.
Analysis: An Expanded Sourcebook. 2nd 50:204 –206. 2006;6:17.
ed. Thousand Oaks, Calif: Sage 30 Moscarello R, Margittai KJ, Rossi M. 33 Carr PL, Gareis KC, Barnett RC. Characteristics
Publications; 1994. Differences in abuse reported by female and and outcomes for women physicians who work
27 Mays N, Pope C. Rigour and qualitative male Canadian medical students. CMAJ. reduced hours. J Womens Health (Larchmt).
research. BMJ. 1995;311:109 –112. 1994;150:357–363. 2003;12:399 – 405.
Teaching and Learning Moments
Not So Routine Follow-up
That Monday morning at the clinic This was not shaping up to be a psychosocial support and provided the
started out like any other—the buzz of routine follow-up visit after all. appropriate resources along with a
nurses directing patients to examination follow-up appointment in the near
rooms, overhead pages filling the air, She was waiting accompanied by her future.
and residents milling about before the husband when we entered the room.
After our encounter, I had a chance to
start of their clinics. A few hours into my “I’m doing great. I can walk lots. I feel
reflect on what had just transpired.
morning rounds, I had developed a good healthy. I have a good appetite,” she
Between their medical illnesses and
rhythm—reviewing the patient’s chart, replied in response to our first
cognitive decline, this couple’s ability
then recording a history and performing question. We then went on to share
to cope with life was teetering on the
a physical, followed by a review with my the results of her most recent scan and
edge. They were living independently
preceptor, back to see the patient again, blood tests. Her husband, being hard
at the time, but that would soon have
dictating the follow-up letter, and of hearing, leaned in, his mind and
to change. What started out as routine
arranging for a follow-up visit. ears focused on what we were telling
and predictable drastically changed by
him. “So what does that mean?” he
the end of the visit. This particular
asked moments after we had told
Her name was towards the end of the follow-up took a little more than half
them that the cancer was back, a sign
list that day. “Routine follow-up” was an hour of my time, but it had thrown
that his cognitive state was not too far
listed as the reason for her visit. My the rest of their lives into chaos. It
behind his wife’s. Our patient had a
preceptor and I quickly perused her served as a poignant reminder of the
puzzled and worried look on her face,
chart before going in—an 82-year-old responsibility that we as physicians
her eyes darting between us and her
female with locally advanced colon have to take every encounter, however
husband. She knew something was
cancer that had been resected about routine it might appear, as one that
wrong but couldn’t quite place her
two years earlier. She had survived her could have far-reaching ramifications
finger on it. Wanting to reassure us,
surgery, and no adjuvant therapy for our patients.
she again repeated, “But I feel so
was administered. Her chart also good. I can walk. I have a great George Kurien and Christopher de
made note of “mild to moderate appetite.” We agreed these were Gara, MB, MS
Alzheimer’s.” The radiologist’s notes indeed good signs, but inside we knew
on her latest CT scan were not that her current health would not last Mr. Kurien is a fourth-year student, University of
reassuring—“lesions most consistent for too long. Together, we went over Alberta Faculty of Medicine and Dentistry,
Edmonton, Alberta, Canada; (gkurien@ualberta.ca).
with local recurrence and metastatic the options for active therapy, and one
disease.” Her blood markers (CEA) by one each was ruled out as a
Dr. de Gara is professor of surgery, University of
were trending upwards and were possibility. We introduced the couple Alberta Faculty of Medicine and Dentistry,
ominously flagged for being elevated. to the idea of palliative care and Edmonton, Alberta, Canada.
866 Academic Medicine, Vol. 84, No. 7 / July 2009
You might also like
- The Effects of Acute Stress On Performance .8Document9 pagesThe Effects of Acute Stress On Performance .8marcobravodNo ratings yet
- A New Era in Graduate Medical Education A Novel.33Document3 pagesA New Era in Graduate Medical Education A Novel.33drhusseinfaour3126No ratings yet
- Coaching With Compassion Showcase Poster Final ShotDocument1 pageCoaching With Compassion Showcase Poster Final ShotMarli SantosNo ratings yet
- Research 1 - RRLDocument3 pagesResearch 1 - RRLJunkoNo ratings yet
- MD 0000000000022430Document10 pagesMD 0000000000022430some oneNo ratings yet
- Navarro, General Trias City, Cavite: Senior High School DepartmentDocument5 pagesNavarro, General Trias City, Cavite: Senior High School DepartmentVan TracilynNo ratings yet
- PT 1 Performance Group 1Document10 pagesPT 1 Performance Group 1RONCIEL JOHN MAROTONo ratings yet
- Human Anatomy.9Document2 pagesHuman Anatomy.9ssabilasaNo ratings yet
- Summary of Research Articles - 2 Juni 2021Document9 pagesSummary of Research Articles - 2 Juni 2021Fenny Mei LinaNo ratings yet
- JournalsDocument4 pagesJournalsMarie Joy Luzon SabueroNo ratings yet
- Knowledge and Attitudes Associated With MenopauseDocument10 pagesKnowledge and Attitudes Associated With MenopauseMr. Md. Imdadul HaqueNo ratings yet
- A - Review - of - Literature - On - Medical - Students - and SCH - 220926 - 082955Document12 pagesA - Review - of - Literature - On - Medical - Students - and SCH - 220926 - 082955Muriel GonzálezNo ratings yet
- Paradigms ResearchDocument1 pageParadigms ResearchAsmamaw K.No ratings yet
- PRBM 274337 Perceptions Knowledge and Attitude Toward Mental Health DiDocument10 pagesPRBM 274337 Perceptions Knowledge and Attitude Toward Mental Health DiLisa SariNo ratings yet
- How Can Students Diagnostic Competence Benefit.32Document7 pagesHow Can Students Diagnostic Competence Benefit.32Carlos Roberto Pires de Oliveira LimaNo ratings yet
- Tmpe373 TMPDocument9 pagesTmpe373 TMPFrontiersNo ratings yet
- Does Mindfulness Training Enhance The Professional Development of Residents? A Qualitative StudyDocument6 pagesDoes Mindfulness Training Enhance The Professional Development of Residents? A Qualitative StudySeda Şahin ÖnerNo ratings yet
- Identifying Naturalistic Coaching Behavior Among.26Document6 pagesIdentifying Naturalistic Coaching Behavior Among.26drhusseinfaour3126No ratings yet
- Belinda, C - 2017 ThesisDocument146 pagesBelinda, C - 2017 ThesisCassiopeia WhiteNo ratings yet
- Fuente 1Document8 pagesFuente 1Jaque RANo ratings yet
- Medicine: Burnout in Emergency Medicine PhysiciansDocument7 pagesMedicine: Burnout in Emergency Medicine PhysiciansJaíza DiasNo ratings yet
- Spector, Hebditch, Stoner & Gibbor 2016Document10 pagesSpector, Hebditch, Stoner & Gibbor 2016CLNo ratings yet
- Box 3.15 Focus On Student Research: Developing A Thematic Analysis GridDocument2 pagesBox 3.15 Focus On Student Research: Developing A Thematic Analysis GridMuhammad MoazNo ratings yet
- Self-Reports: How The Questions Shape The AnswersDocument13 pagesSelf-Reports: How The Questions Shape The AnswersCiro ALVAREZ-NAVARRONo ratings yet
- Medicine: Effects of Social Stories Intervention For Children and Adolescents With Autism Spectrum DisordersDocument4 pagesMedicine: Effects of Social Stories Intervention For Children and Adolescents With Autism Spectrum DisordersJarmzzzzNo ratings yet
- Responsabilidades de EnfermeriaDocument11 pagesResponsabilidades de EnfermeriabryanNo ratings yet
- Manapat 2023 - EFADocument19 pagesManapat 2023 - EFAJessiane AraujoNo ratings yet
- Structured Interviewer Training For The Implementation of Standardized Behavioral Questions in Medical School AdmissionsDocument5 pagesStructured Interviewer Training For The Implementation of Standardized Behavioral Questions in Medical School AdmissionsAdam LevineNo ratings yet
- TeachingDocument6 pagesTeachingmelanieNo ratings yet
- Dominance of The Leptoprosopic Face and Mesorrhine.40-1Document3 pagesDominance of The Leptoprosopic Face and Mesorrhine.40-1Godwin SundayNo ratings yet
- Quantitative Study On Human Cerebellar Cortex From Anatomy Cadaver PreparationsDocument5 pagesQuantitative Study On Human Cerebellar Cortex From Anatomy Cadaver PreparationsIlincaNo ratings yet
- Gezer 2010Document5 pagesGezer 2010Tuan Muhammad DanilNo ratings yet
- Neurologic Complications of Cancer Drug Therapies.11Document11 pagesNeurologic Complications of Cancer Drug Therapies.11Mayra AlejandraNo ratings yet
- E056655 FullDocument7 pagesE056655 Fulljackson wongNo ratings yet
- Slack Wassenaar 1999Document8 pagesSlack Wassenaar 1999Nanda Dwi ChartinNo ratings yet
- In Search of Better Practice in Executive Functions Assessment: Methodological Issues and Potential SolutionsDocument30 pagesIn Search of Better Practice in Executive Functions Assessment: Methodological Issues and Potential SolutionsguoNo ratings yet
- Survey Research.32Document9 pagesSurvey Research.32Una LeymanNo ratings yet
- Nonlinear Partial Differential Equations Their Solutions and Pr-By Shubham PadhiDocument74 pagesNonlinear Partial Differential Equations Their Solutions and Pr-By Shubham PadhiShubham PadhiNo ratings yet
- Trainee Attachment To Supervisor and Perceptions of Novice Psychotherapist Counseling Self-Efficacy: The Moderating Role of Level of ExperienceDocument6 pagesTrainee Attachment To Supervisor and Perceptions of Novice Psychotherapist Counseling Self-Efficacy: The Moderating Role of Level of ExperienceJulio César Cristancho GarcíaNo ratings yet
- Relacion Entre El Burnout y Estudiantes de Medicina HumanaDocument4 pagesRelacion Entre El Burnout y Estudiantes de Medicina HumanaJair Benavente AsinNo ratings yet
- Waring Kelly 2019 Sitar EditedDocument1 pageWaring Kelly 2019 Sitar Editedapi-258201243No ratings yet
- Deep Semantic Segmentation of Natural and Medical ImagesDocument47 pagesDeep Semantic Segmentation of Natural and Medical ImagesMario Galindo QueraltNo ratings yet
- Coaching Versus Therapy: A PerspectiveDocument9 pagesCoaching Versus Therapy: A PerspectivePuljić DragoNo ratings yet
- Relationship Between Gender and Employment Contexts of Bicol University Graduates PDFDocument9 pagesRelationship Between Gender and Employment Contexts of Bicol University Graduates PDFimanolkioNo ratings yet
- Center For Poverty Research Discussion Paper Series, DP2008-07. Retrieved (Date) From lications/DP2008-07 PDFDocument2 pagesCenter For Poverty Research Discussion Paper Series, DP2008-07. Retrieved (Date) From lications/DP2008-07 PDFGwy TamsNo ratings yet
- NURS 4369 Preceptor Packet Core 2013Document11 pagesNURS 4369 Preceptor Packet Core 2013Aruna Chezhian100% (1)
- Scoping Reviw TableDocument2 pagesScoping Reviw TableAngela BortaNo ratings yet
- Lei 2019Document7 pagesLei 2019LaRNo ratings yet
- 2017 - Research - Symposium - Abstracts - PostersDocument32 pages2017 - Research - Symposium - Abstracts - PostersAndreia SilvaNo ratings yet
- Trait Knowledge Forms A Common Structure Across Social CognitionDocument14 pagesTrait Knowledge Forms A Common Structure Across Social CognitionYnes LadhariNo ratings yet
- The Perspective of Healthcare Providers and Patients On Health Literacy - A Systematic Review of The Quantitative and Qualitative StudiesDocument11 pagesThe Perspective of Healthcare Providers and Patients On Health Literacy - A Systematic Review of The Quantitative and Qualitative StudiesKusrini Kadar SyamsalamNo ratings yet
- Wu 2016 (Severity)Document11 pagesWu 2016 (Severity)Laura HdaNo ratings yet
- MenaDocument23 pagesMenaangelNo ratings yet
- التصورات الاجتماعية عند الطلبات الجامعيات (المخطوبات) لسمات شريك الحياة المثاليDocument22 pagesالتصورات الاجتماعية عند الطلبات الجامعيات (المخطوبات) لسمات شريك الحياة المثاليAnfel RamdaniNo ratings yet
- Provided by K-State Research ExchangeDocument145 pagesProvided by K-State Research ExchangeEugénio JaquetaNo ratings yet
- Short Communication: Why Don't Boys Apply To Vet School? A Pilot StudyDocument3 pagesShort Communication: Why Don't Boys Apply To Vet School? A Pilot StudyElenaNo ratings yet
- Brief A Job Analysis To Define The Role of The Pharmacy PreceptorDocument12 pagesBrief A Job Analysis To Define The Role of The Pharmacy Preceptorbesta citraNo ratings yet
- Ex Part 1 Blueprinting Grid NewDocument1 pageEx Part 1 Blueprinting Grid NewKaushika KalaiNo ratings yet
- ARTIGO CLASSIFICAÇÃO NIVEL DE TREINAMENTO - Santos-Junior Et Al., 2021 Classification - and - Determination - Model - (FINAL)Document10 pagesARTIGO CLASSIFICAÇÃO NIVEL DE TREINAMENTO - Santos-Junior Et Al., 2021 Classification - and - Determination - Model - (FINAL)Gordo FakeNo ratings yet
- ThiruvananthapuramDocument31 pagesThiruvananthapuramsuryadev s24No ratings yet
- Abnormal CBC - PresentationDocument23 pagesAbnormal CBC - PresentationMateen ShukriNo ratings yet
- BFHI Revised Section2.6 HandoutsDocument35 pagesBFHI Revised Section2.6 HandoutsMrinal SivadasanNo ratings yet
- Counseling Parents About Cochlear ImplantsDocument6 pagesCounseling Parents About Cochlear ImplantsJordan HansonNo ratings yet
- Antimcrobial Therapy NELSON 2016 288 PagDocument288 pagesAntimcrobial Therapy NELSON 2016 288 PagNorvy CuberosNo ratings yet
- Summer Internships Project On Base On Employees Exit at Health-Care Sector With Literature ReviewDocument91 pagesSummer Internships Project On Base On Employees Exit at Health-Care Sector With Literature ReviewParshwa Shah100% (1)
- Sodium Chloride (0.9) Pi PDFDocument8 pagesSodium Chloride (0.9) Pi PDFdian kurniaNo ratings yet
- Vijayalakshmi S Kotrashetti, Alka D Kale, Mamata Hebbal, Seema R HallikeremathDocument12 pagesVijayalakshmi S Kotrashetti, Alka D Kale, Mamata Hebbal, Seema R HallikeremathwelcometohellNo ratings yet
- Seminars in Orthodontics: VOL 26, NO 2 JUNE 2020Document1 pageSeminars in Orthodontics: VOL 26, NO 2 JUNE 2020Jawad TariqNo ratings yet
- Magnesium CitrateDocument3 pagesMagnesium CitrateMorticia AdamsNo ratings yet
- Brain Atlas of Human Anatomy With MRIDocument1 pageBrain Atlas of Human Anatomy With MRIBerk HalilbeyoğluNo ratings yet
- Supraventricular Tachycardia in ChildrenDocument4 pagesSupraventricular Tachycardia in ChildrentshahriyarNo ratings yet
- Somatom Session 28Document76 pagesSomatom Session 282vjNo ratings yet
- Wang.2008.Central Serous ChorioretinopathyDocument20 pagesWang.2008.Central Serous ChorioretinopathyRohit GuptaNo ratings yet
- Mom Review 6 Aiims at Aiims BBRDocument44 pagesMom Review 6 Aiims at Aiims BBRgaurav chauhanNo ratings yet
- PALS (Pediatric Advanced Life Support)Document67 pagesPALS (Pediatric Advanced Life Support)Ayyesha Yuanita100% (1)
- An Atlas of Head and Neck Images Part I 2002 Atlas of The Oral and Maxillofacial Surgery ClinicsDocument2 pagesAn Atlas of Head and Neck Images Part I 2002 Atlas of The Oral and Maxillofacial Surgery ClinicsMohammed Qasim Al-WataryNo ratings yet
- Patofisiologi Nyeri DasarDocument87 pagesPatofisiologi Nyeri DasarHidayat Bazeher0% (1)
- Writing Your Personal StatementDocument6 pagesWriting Your Personal StatementBilal MohammadNo ratings yet
- Child Cerebral Pasly Guideline For CliniciansDocument2 pagesChild Cerebral Pasly Guideline For CliniciansAnonymous qbQIQaPlNo ratings yet
- Paediatric Orthopaedics (Leh)Document97 pagesPaediatric Orthopaedics (Leh)Fera MulidarNo ratings yet
- Dilip Shanghvi ReportDocument12 pagesDilip Shanghvi ReportMangalya ShahNo ratings yet
- FC Orth (SA) Intermediate Past Papers - 2012 Mar 28-3-2015Document2 pagesFC Orth (SA) Intermediate Past Papers - 2012 Mar 28-3-2015Uhuebor DavidNo ratings yet
- Mci Drill PresentationDocument10 pagesMci Drill Presentationapi-243894974No ratings yet
- Instructional Design On Proper Latch On During Breast FeedingDocument4 pagesInstructional Design On Proper Latch On During Breast FeedingJanschel Zara DimaapiNo ratings yet
- AbstractsDocument5 pagesAbstractsElham ZareNo ratings yet
- Separation Anxiety DisorderDocument4 pagesSeparation Anxiety Disordernot your medz duranNo ratings yet
- Cochrane, Nathan - Iatrogenic Damage To Enamel During Fixed Orthodontic TreatmentDocument1 pageCochrane, Nathan - Iatrogenic Damage To Enamel During Fixed Orthodontic TreatmentmalifaragNo ratings yet
- R e S U M 2Document2 pagesR e S U M 2Sandeep Shah100% (1)
- Milroy Disease Pak TomoDocument3 pagesMilroy Disease Pak TomoMeta SariNo ratings yet