Professional Documents
Culture Documents
Chapter-3 10 7-Salmonellosis
Uploaded by
Saulo EvangelistaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter-3 10 7-Salmonellosis
Uploaded by
Saulo EvangelistaCopyright:
Available Formats
1 CHAPTER 3.10.7.
2 SALMONELLOSIS*1
3 SUMMARY
4 Description of the disease: Salmonellosis is an infectious disease of humans and animals caused
5 by bacteria of the genus Salmonella. Salmonellae are aetiological agents of diarrhoeal and
6 systemic infections. They often cause subclinical infections and may be shed in large numbers
7 within the faeces of clinical cases and carrier animals resulting in contamination of the environment.
8 Infection in food animals often leads to contamination of meat, eggs, milk and cheese milk
9 products. Salmonellosis is one of the most common and economically important food-borne
10 zoonotic diseases in humans. The disease has been recognised in all countries and non-typhoidal
11 Salmonella appears to be most prevalent in areas of intensive animal husbandry, especially in pigs,
12 intensively reared calves and poultry.
13 The disease can affect all species of domestic animals; young animals and pregnant and lactating
14 animals are the most susceptible to clinical infections. Enteric disease is the commonest clinical
15 manifestation, but a wide range of clinical signs, which include acute septicaemia, abortion, arthritis
16 and respiratory disease, may be seen. Many animals, especially pigs and poultry, may be infected
17 but show no clinical illness. Such animals may be important animal species have a central role in
18 relation to the spread of infection between flocks and herds and as sources of food contamination
19 and human infection.
20 Fowl typhoid and Pullorum disease, poultry diseases caused by host-specific Salmonella biovars,
21 are addressed in chapter 3.3.11.
22 Detection of the agent: Diagnosis is based on the isolation and identification of the organism
23 either from tissues collected aseptically at necropsy or from faeces, rectal swabs or, environmental
24 samples, food products and feedstuffs; . Prior or current infection of animals by some serovars may
25 also be diagnosed serologically. When infection of the reproductive organs or abortion occurs, it is
26 necessary usual to culture fetal stomach contents, placenta and vaginal swabs and, in the case of
27 poultry, embryonated eggs or ovary/oviduct.
28 Salmonellae may be isolated using a variety of techniques that may include pre-enrichment to
29 resuscitate and multiply sub-lethally damaged salmonellae organisms, enrichment media that
30 contain inhibitory substances to suppress competing organisms and selective plating agars to
31 differentiate salmonellae from other enterobacteria. Alternative methods such as polymerase chain
32 reaction and immunological detection of Salmonella antigens can also be used, according to
33 legislative requirements.
34 Various biochemical, serological and molecular tests can be applied to the pure culture to provide a
35 definitive confirmation of an isolated strain. Salmonellae possess antigens designated somatic (O),
36 flagellar (H) and virulence (Vi), which may be identified by specific typing sera, and the serovar
37 may be determined by reference to the antigenic formulae in the White-Kauffmann–Le Minor
38 scheme. Many laboratories may need to send isolates to a reference laboratory for the
39 identification of the serotype and further characterisation. Alternative serotyping methods, including
40 multi-locus sequence typing (MLST)-include various methods based on molecular approaches,
41 such as microarray or whole genome sequencing, which are increasingly used. Phage-typing
42 schemes are also available for some serovars, but are less commonly used than in former years,
43 having been largely superseded by molecular methods.
44 Serological tests: Serological tests should be conducted on a statistically representative sample
45 of the population and results are not always indicative of active infection. In the laboratory, the tube
46 agglutination test is the method of choice for export and diagnostic purposes for samples from all
1
1 Although certain diseases caused by Salmonella are included in some individual species sections of the OIE List, this
2 chapter covers several species and thus gives a broader description.
3 OIE Terrestrial Manual 2022 1
47 species of farm animals. Enzyme-linked immunosorbent assays are available for some serovars
48 and may be used for serological diagnosis and surveillance, especially in poultry and pigs.
49 Salmonella vaccination may compromise the diagnostic value of serological tests.
50 Requirements for vaccines: Inactivated and live vaccines are available commercially. In the case
51 of the Inactivated vaccines, they usually contain oil or alhydrogel adjuvants to improve their
52 efficacy.
53 A. INTRODUCTION
54 Salmonellosis is an infectious disease of humans and animals, clinically characterised by septicaemia, acute
55 enteritis or chronic enteritis, septicaemia or abortion. Animals may be infected without being overtly ill.
56 Salmonellae are primarily intestinal bacteria and may be shed continuously or intermittently within the faeces,
57 resulting in contamination of the environment (Barrow & Methner, 2013).
58 1. Causal Nature and Classification and nomenclature of the pathogen agent
59 The genus Salmonella consists of only two species: S. enterica and S. bongori (Grimont & Weill, 2007).
60 Salmonella enterica is divided into six subspecies, which are distinguishable by certain biochemical
61 characteristics and susceptibility to lysis by bacteriophage Felix O1. These subspecies are:
Original subgenera Current nomenclature
• Subspecies I = subspecies enterica
• Subspecies II = subspecies salamae
• Subspecies IIIa = subspecies arizonae
• Subspecies IIIb = subspecies diarizonae
• Subspecies IV = subspecies houtenae
• Subspecies VI = subspecies indica
62 For the serovars of S. bongori, the symbol V was retained to avoid confusion with the serovar names of
63 S. enterica subsp. enterica.
64 Strains of Salmonella are classified into serovars on the basis of extensive diversity of lipopolysaccharide (LPS)
65 or; O antigens) and flagellar protein or (H antigens) in accordance with the White-Kauffmann–Le Minor scheme
66 (Grimont & Weil, 2007); currently more than 2600 serovars are recognised (Issenhuth-Jeanjean et al., 2014)., but
67 there are also a number of stable monophasic variant clones of several serovars, and the list of serovars has not
68 been updated for over 10 years. The most common serovars that cause infections in humans and food animals
69 belong to subspecies enterica. The serovars of the other subspecies are more likely to be found in cold-blooded
70 animals and in the environment, but are occasionally associated with human disease. Some serovars of
71 subspecies arizonae and subspecies diarizonae may cause disease in turkeys and sheep and others may be
72 carried by reptiles and amphibians. In accordance with the White-Kauffmann–Le Minor scheme, only serovars of
73 subspecies enterica bear a name, e.g. S. enterica subsp. enterica serovar Enteritidis, or S. enterica serovar
74 Enteritidis, or, in short, S. Enteritidis. Serovars of other subspecies of S. enterica, monophasic variants and those
75 of serovars within S. bongori are designated only by their antigenic formula (e.g. Salmonella IV 48:g.z51).
76 Changes to serovar classification may occur when different O antigens are expressed due to colony form
77 variation or lysogenation lysogeny by bacteriophage(s) or when different flagellae are produced expressed as a
78 result of phase variation or deletions or mutations in genes coding for flagellae or expression mechanisms.
79 2. Description and impact of the disease
80 The course of infection, the clinical signs, the post-mortem findings and epidemiological patterns vary according
81 to the serovar and the animal species involved. Most serovars can cause disease in a wide range of animal
82 species (Barrow & Methner, 2013 Jajere, 2019), but some serovars are host-specific, e.g. S. Typhi in humans and
83 S. Abortusovis in sheep. Other serovars are host-adapted e.g. S. Choleraesuis in pigs and S. Dublin in cattle.
84 Host-specific and host-adapted serovars often cause septicaemic disease. In poultry, the host-specific diseases
85 Pullorum disease or bacillary white diarrhoea and fowl typhoid are used to describe the host-specific infections
86 caused by S. Gallinarum, biovars Pullorum and S. Gallinarum, Gallinarum (Barrow & Neto, 2011), respectively.
87 Fowl typhoid and Pullorum disease are covered in detail in chapter 3.3.11.
88 In humans, young children, the aged and those people who are immunologically compromised or taking proton
89 pump inhibitors are most susceptible to salmonellosis. The disease can affect all species of domestic animals;
90 young animals and pregnant animals are particularly susceptible. A wide range of clinical signs, including acute
4 OIE Terrestrial Manual 2022 2
5 Chapter 3.10.7. – Salmonellosis
91 septicaemia, acute or chronic diarrhoea, respiratory disease, abortion, and arthritis, may be seen. Chicks and
92 turkey poults of less than 1 week of age are highly susceptible to Salmonella infection and may occasionally
93 exhibit clinical signs including anorexia, adipsia, depression, ruffled feathers, huddling together, somnolence,
94 dehydration, white diarrhoea and pasted vents with considerable mortality as a result, but even in young poultry,
95 subclinical infection is most likely. In calves, septicaemic infection with the host-adapted S. Dublin serovar occurs
96 mainly at 2–6 weeks of age. The calves are dull, pyrexic, are anorexic, have diarrhoea with blood and mucus in
97 the faeces, may have pneumonia or necrosis of distal extremities, and often become quickly dehydrated and die if
98 appropriate treatment is not given in a timely manner. In pregnant cows, infection with S. Dublin is a common
99 cause of abortion. Pigs infected with the host-adapted S. Choleraesuis may show clinical illness, are anorexic,
100 have a high fever, become lethargic and the extremities may appear cyanotic. show signs of septicaemia that can
101 result in death without any preceding clinical signs. However, more commonly, clinical signs of affected pigs are
102 anorexia, high fever, lethargy, shallow cough, difficulty in breathing and cyanotic extremities. Salmonella
103 Typhimurium is also a common cause of salmonellosis in cattle and weaned pigs.
104 Many animals, especially poultry and pigs, but also cattle and sheep, may be infected but show no clinical illness
105 (Barrow & Methner, 2013 Jajere, 2019). Such animals may be important have a central role in relation to the
106 spread of the infection between and within flocks and herds. Salmonellosis has been recognised in all countries,
107 but non-typhoidal infection appears to be most prevalent in areas of intensive animal husbandry, especially of
108 poultry or and pigs (Barrow & Methner, 2013 Jajere, 2019).
109 3. Zoonotic risk and potential, biosafety and biosecurity requirements
110 Human salmonellosis is one of the most common and economically important zoonotic diseases. The Centers for
111 Disease Control and Prevention (CDC) estimates that salmonellosis causes more than 1.2 1.35 million illnesses
112 each year in the United States of America, with more than 23,000 26,500 hospitalisations and 450 429 deaths
113 (CDC, 2013; 2021). A recent study in Australia reported that in 2015, there were nearly 91,000 non-typhoidal
114 salmonellosis cases, of which over 4300 were hospitalised and 19 patients died, at a total societal cost of over
115 100 million US dollars (Ford et al., 2019). The most common cause of infection with Salmonella is eating
116 contaminated foods including raw or undercooked eggs or egg products, meat, poultry and pig meat,
117 contaminated fresh fruit and vegetables and soft cheeses made from unpasteurised milk.
118 Salmonella can also be spread to people through contact with infected birds, livestock, reptiles, amphibians, and
119 rodents, dogs and cats. These animals may carry the bacteria even when apparently healthy. Many serovars,
120 including some that are host-adapted such as S. Choleraesuis and S. Dublin, have been shown to cause serious
121 disease in humans. Abattoir workers, animal attendants and veterinarians may be infected directly during the
122 course of their work when in contact with infected animals. Laboratory personnel may also acquire the infection if
123 safe working practices are not implemented. To prevent occurrences of laboratory infections, the biosafety and
124 biosecurity measures in veterinary diagnostic and animal facilities should be adhered to All laboratory
125 manipulations with live cultures or potentially infected or contaminated material must be performed at an
126 appropriate biosafety and containment level as determined by biological risk analysis (see Chapter 1.1.4
127 Biosafety and biosecurity: Standard for managing biological risk in the veterinary laboratory and animal facilities).
128 4. Differential diagnosis
129 Signs in young birds with generalised salmonellosis closely resemble those seen in Pullorum disease, fowl
130 typhoid and those of other acute septicaemic illnesses caused by a wide variety of bacteria including Escherichia
131 coli. In all avian species arthritis caused by Salmonella infection may be mistaken for synovitis or bursitis caused
132 by other infections. Septicaemic salmonellosis in pigs caused by S. Choleraesuis may be mistaken for hog
133 cholera. Septicaemic salmonellosis in calves or weaned pigs may be confused with colibacillosis, although the
134 latter disease occurs usually at a younger age. The acute enteric form of salmonellosis in calves may resemble
135 coccidiosis. Abortions in sheep may be caused not only by S. Abortusovis, but also by Chlamydia abortus,
136 Campylobacter spp., Coxiella burnetii, Chlamydophila abortus, Brucella ovis or other pathogens.
137
6 OIE Terrestrial Manual 2022 3
7 Chapter 3.10.7. – Salmonellosis
138 B. DIAGNOSTIC TECHNIQUES
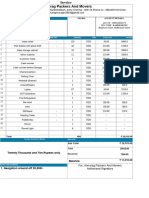
139 Table 1. Test methods available for the diagnosis of salmonellosis and their purpose
Purpose
Method Population Individual animal Immune status in
Contribute to Confirmation Prevalence
freedom freedom from individual animals or
eradication of clinical of infection –
from infection prior to populations post-
policies cases surveillance
infection movement vaccination
Detection of the agent(a)
Salmonella
+++ +++ +++ +++ +++ –
isolation
Rapid
alternative
+ + + + + –
methods, e.g.
PCR
Detection of immune response
SAT ++ – ++ – + ++
ELISA ++ – +++ + ++ ++
140 Key: +++ = recommended for this purpose; ++ recommended but has limitations;
141 + = suitable in very limited circumstances; – = not appropriate for this purpose.
142 PCR = polymerase chain reaction-based tests; SAT = serum agglutination test; ELISA = enzyme-linked immunosorbent assay.
(a)
143 A combination of agent detection methods applied on the same clinical sample is recommended.
144 1. Detection of the agent
145 The frequency of sampling and the type of samples obtained will depend largely on the objectives of the testing
146 programme, import and export monitoring or international trade regulations, clinical findings, level of detection or
147 precision of prevalence estimates required, cost and availability of sampling resources and laboratory facilities.
148 General guidelines on the collection, submission and storage of diagnostic or survey samples, the sample size,
149 the information to be sent with the samples and the packaging and transportation of samples are described in
150 Chapters 1.1.2 and 1.1.3 of this Terrestrial Manual.
151 Individual samples for bacteriological tests are collected as aseptically as possible and in the case of clinical
152 disease or routine monitoring, samples should be collected before any antibiotic treatment has commenced.
153 Clinical samples are preferably collected during the acute phase of the disease or as soon as possible after
154 death. In the case of flocks of poultry or other avian species, environmental samples, such as naturally pooled
155 faeces, litter and dust or drag or boot swabs from floor surfaces (Carrique-Mas & Davies, 2008), or large, moist
156 fabric swabs may be the most cost-effective way to identify infected flocks, and can also be useful for other types
157 of livestock unit. In dairy herds, milk filters can be a useful sample type. For smaller animal species, it may be
158 preferable to submit a representative number of sick or recently dead animals to the laboratory (WHO, 1994).
159 Host-adapted serovars are usually more difficult to isolate from faeces so if these are suspected, infected tissues
160 should be cultured where possible.
161 Particular attention should be given to the isolation of salmonellae from animals with subclinical infection, as these
162 may only excrete shed bacteria intermittently and in low numbers. An increased sample size, increased number of
163 samples representing more individuals, combined in some cases with pooling of samples to reduce the cost, and
164 repeat sampling can provide an increased diagnostic sensitivity, but pooling can also reduce detection if the
165 sample prevalence or concentration of target bacteria is low. As bacteria are usually clustered in faecal samples,
166 a thorough mixing of the sample before culture may also increase the sensitivity of the procedure (Cannon &
167 Nicholls, 2002). Bacteriological and also serological methods may be used to identify infected flocks or herds ,
168 rather than to identify and infected individual animals.
169 1.1. Culture
170 There are numerous methods for isolation and detection of Salmonella in use world-wide (Fricker,
171 1987; Harvey & Price, 1974; Lee et al., 2015; Park et al., 2014; Reissbrodt, 1995). Some of the more
172 common methods are described below. The culture techniques and media that may work best in a
173 particular diagnostic situation depend on a variety of factors, including the Salmonella serovar, source
8 4 OIE Terrestrial Manual 2022
9 Chapter 3.10.7. – Salmonellosis
174 and type of specimens, animal species of origin, experience of the microbiologist, and availability of
175 selective enrichment and selective plating media.
176 All culture media should be subjected to quality control and must support growth of the suspect
177 organism Salmonella from a small inoculum in the presence of a relevant sample matrix or competing
178 flora. The routine use of a reference strain in parallel with routine samples may lead to cross-
179 contamination of samples if careless techniques are used; therefore, a rare serovar with typical growth
180 characteristics that are similar to the highest priority target strains should be used. It is also possible to
181 use strains with antimicrobial resistance or other markers, such as fluorescence.
182 The increasing application of external quality assurance programmes has led to greater use of
183 international standard methods, such as ISO 6579:2002, even though this-1:2017 (as amended in
184 2020). The modified semi-solid Rappaport–Vassiliadis (MSRV) agar-based method has not been
185 validated for faecal and environmental food, /feed and environmental samples and was intended for
186 foodstuffs and feeding stuffs (ISO, 2002). A standard is the required method for detection of
187 Salmonella from primary animal production has been published, and the ISO method has now been
188 adopted (ISO, 2007). and optional for food or feeding stuffs. The basis of the standard method is pre-
189 enrichment in buffered peptone water, followed by mandatory selective enrichment on MSRV agar and
190 for samples of primary production, whereas for food and feedstuffs the prescribed selective enrichment
191 is Müller–Kauffmann tetrathionate broth (MKTTn) and Rappaport–Vassiliadis-soya (RVS) broth or
192 MSRV, then isolation is carried out on xylose-lysine-deoxycholate (XLD) agar and an additional plate
193 medium of choice, which is based on a different biochemical indicator. This method MSRV agar has
194 also been shown to be highly effective for animal feed, animal environmental samples and meat
195 products, and is simpler and less expensive than the full ISO method detection of motile salmonellae.
196 Diagnostic methods and assays should be validated as described in Chapter 1.1.6 Principles and
197 methods of validation of diagnostic assays for infectious diseases.
198 1.1.1. Pre-enrichment media
199 The number of salmonellae in faeces from asymptomatic animals, environmental samples,
200 animal feed and food is usually often low, and sometimes damaged, thus it is often necessary to
201 use pre-enrichment media, such as buffered peptone water to assist isolation maximise
202 detection. This may allow the small numbers of salmonellae, which may otherwise be killed by
203 the toxic effect of selective enrichment media, to multiply, and it may help to resuscitate
204 salmonellae that have been sub-lethally damaged, e.g. by freezing, heating, desiccation, or
205 exposure to biocides or organic acids (Harvey & Price, 1974). For intermittent shedders If acid-
206 treated samples are being tested, it can be advantageous to increase the buffering capacity of
207 the pre-enrichment medium. For highly absorptive samples or fresh faeces and intestinal
208 contents, increasing the ratio of broth to sample weight can improve detection. For intermittent
209 shedder animals, it is advantageous to test at least three consecutive faecal samples.
210 1.1.2. Selective enrichment media
211 Enrichment media are liquid or semi-solid agar media containing additives that selectively
212 permit salmonellae to grow while inhibiting the growth of other bacteria. Examples of selective
213 enrichment media are tetrathionate, as in Müller–Kauffmann broth, selenite cystine, brilliant
214 green broth, RSV RVS broth and MSRV agar. Some additives, however, are also can be
215 relatively toxic to certain serovars of Salmonella, e.g. selenite inhibits S. Choleraesuis, and
216 brilliant green is toxic to many strains of S. Dublin. Elevated temperatures have also been used
217 to increase the selectivity, with a temperature of 43°C being used in some laboratories, although
218 this may be inhibitory with some media, e.g. tetrathionate.
219 With Rappaport–Vassiliadis at 43°C temperature-sensitive strains, especially S. Dublin, are
220 inhibited and 41.5°C is now recommended for incubation of RSV RVS broth-based media and
221 MSRV agar. Selective motility enrichment media such as MSRV agar or diagnostic semi-solid
222 Salmonella medium (DIASALM) are commonly used to increase the sensitivity of the
223 Salmonella isolation procedure (Voogt et al., 2001). Use of at least two selective enrichment
224 broths media is recommended for maximum recovery, and detection of mixed serovar
225 contamination, with one incubated at 37°C and the other at a suitable higher temperature. The
226 formulation of the medium, which may vary between suppliers, or even between batches in
227 some cases, temperature and duration of incubation, and the volume of the samples used to
228 inoculate the medium, may all serve to influence the isolation rate, and these variables should
229 always be taken into account. The selectivity of these media is based on the motility of the
230 organism, the presence of malachite green dye and novobiocin, and a high concentration of
231 magnesium chloride. The semi-solid medium allows motility to be detected as halos of growth
232 spreading within the agar from the site of inoculation. If there is no such growth, the sample can
233 often be considered to be negative for Salmonella without further plating. Non-motile strains
10 OIE Terrestrial Manual 2022 5
11 Chapter 3.10.7. – Salmonellosis
234 however cannot be detected using semi-solid selective enrichment. Additives, such as
235 ferrioxamine E, may be added to selective enrichment media to enhance isolation of Salmonella
236 from iron or nutrient-limited samples such as eggs, water or soil (Reissbrodt, 1995) or antibiotics
237 such as novobiocin may be added to suppress most Gram-positive organisms or other Gram-
238 negative bacteria, such as Proteus. Specific antibiotics can be added to enhance the isolation of
239 antimicrobial resistant Salmonella strains.
240 1.1.3. Selective plating media
241 These are solid, selective agars that permit differential growth to varying degrees. They inhibit
242 growth of bacteria other than Salmonella and give information on some of the principal
243 differential biochemical characteristics – usually non-lactose fermentation and hydrogen
244 sulphide (H2S) production. The results are read after 24 and 48 hours of culture at 37°C.
245 Salmonellae form characteristic colonies on such media that are usually distinguishable from
246 the colonies of other bacteria on the plate, with the possible exceptions of Proteus,
247 Pseudomonas, Citrobacter and Hafnia. Lactose-fermenting salmonellae may occasionally be
248 isolated and H2S production may be variable. Such atypical strains may be more effectively
249 detected when semi-solid motility media are used for selective enrichment. Examples are the
250 modified semi-solid MSRV and DIASALM. The selectivity of these media is based on the
251 motility of the organism, the presence of malachite green dye and novobiocin, and a high
252 concentration of magnesium chloride. The semi-solid medium allows motility to be detected as
253 halos of growth away from the site of inoculation. DIASALM medium is particularly useful for the
254 detection of atypical strains as presumptive confirmation by slide agglutination testing using
255 polyvalent O, H or specific antisera can be carried out on liquid from the growth zone in the
256 plate. Also, Plates such as desoxycholate-citrate agar (DCA), brilliant green agar (BGA) or
257 bismuth-sulphite agar can be used, but these are subject to a higher frequency of false-positive
258 colonies. Salmonella Abortusovis is a slow-growing serovar and it is usual to incubate plates for
259 up to 72 hours and to use the non-selective blood agar. Examples of, or minimally selective
260 plating media are BGA, XLD MacConkey agar, DCA, and bismuth-sulphite agar. A wide range
261 of chromogenic agars such as Rambach agar and SMID (Salmonella detection and
262 identification agar) are now also available for the selective isolation of salmonellae. Many of
263 these may aid differentiation of suspect colonies, especially from faecal samples, but must be
264 validated for the sample matrices, culture systems and serovar range targeted as sensitivity can
265 be poor in some circumstances., e.g. for host-adapted or some arizonae or diarizonae serovars.
266 Certain chromogenic agar media, such as Brilliance or Rapid, may, however, be more efficient
267 for detection of biochemically atypical salmonellae.
268 1.1.4. Example test procedures for isolation of Salmonella from food, feedstuffs, faecal and
269 environmental samples
270 i) Add a 10–25 g sample to at least ×10 volume of buffered peptone water at ambient
271 temperature. (NB: for many host-adapted serovars and some arizonae serovars, it is
272 preferable to add the sample to selective enrichment medium, such as selenite cysteine
273 broth, and to test tissue samples where possible [including by direct plating]; see culture
274 method for S. Pullorum/Gallinarum (biovars Gallinarum and Pullorum) in Chapter 3.3.11
275 Fowl typhoid and Pullorum disease.)
276 ii) Incubate in pre-warmed buffered peptone water for 16–20 hours at 37 34–38°C.
277 iii) Inoculate 15–20 ml MSRV agar or DIASALM in a 90 mm diameter Petri dish with 0.1 ml
278 incubated buffered peptone water, preferably as three separate drops.
279 iv) Inoculate 10 ml Müller–Kauffmann tetrathionate broth with 1 ml incubated buffered
280 peptone water broth.
281 v) Incubate MSRV or DIASALM at 41 40.5–42.5°C and tetrathionate broth at 37 34–38°C
282 (ensure that a reputable brand. The higher end of tetrathionate the temperature range for
283 both pre-enrichment and selective enrichment is recommended for improved isolation of
284 Salmonella from faecal and intestinal samples, or environmental samples with a complex
285 flora. The lower part of the range may be more suitable for use at 37°C is used) some
286 food/feed and dry environmental samples.
287 vi) After 24 and 48 hours of selective enrichment, plate out MSRV or DIASALM by taking 1 µl
288 loop of material from the edge of the turbid growth zone and streaking over one plate of
289 chromogenic agar (e.g. Rambach agar) or BGA plus novobiocin and one plate of XLD
290 agar.
12 6 OIE Terrestrial Manual 2022
13 Chapter 3.10.7. – Salmonellosis
291 vii) Plate out 10 µl of tetrathionate broth on one plate of chromogenic agar (e.g. Rambach
292 agar) or BGA plus novobiocin and XLD agar.
293 viii) Incubate plates at 37 34–38°C for 24 21–27 hours.
294 ix) Check up to five suspect colonies (red/pink with reddening of the media on BGA, crimson
295 with pale borders or orange/colourless on Rambach agar medium on BGA, red with black
296 centre (or occasionally translucent red in the case of H 2S negative strains) on XLD agar)
297 biochemically, using composite media such as TSI, LDC and urea, or commercial
298 biochemical tests test kits, and by slide agglutination with polyvalent ‘O’ (A-S) and poly ‘H’
299 (phase 1 and phase 2 antisera). Confirm to the serogroup level by using poly ‘O’ and poly
300 ‘H’ (phase 1 and phase 2) specific ‘O’ group antiserum or composite. The combination of
301 the biochemical media. and serological results can provide confirmation of Salmonella
302 spp. Sero-grouping alone is not sufficient to rule out false positives because of cross-
303 reactions with polyvalent sera, e.g. by Citrobacter or Enterobacter spp. Multiple Composite
304 biochemical tests, polymerase chain reaction (PCR) or matrix assisted laser desorption
305 ionisation time of flight (MALDI-ToF) mass spectrometry can also provide confirmation of
306 Salmonella spp.
307 x) Subculture strongly suspect colonies that do not agglutinate with poly H antisera on to
308 non-selective media then repeat testing. If a strong poly ‘O’ and poly ‘H’ agglutination can
309 be obtained, this is sufficient for presumptive confirmation. Biochemically and serologically
310 confirmed isolates can then be submitted to a reference laboratory for serotyping. If
311 agglutination results are unclear then carry out further biochemical testing using composite
312 media, such as TSI or use ONPG (o-nitrophenyl-beta-d-galactopyranoside) and urea or
313 commercial biochemical test kits.
314 This method differs from ISO 6579:2002 and its Annex D method in that it allows for inoculation
315 of DIASALM in place of MSRV for selective enrichment and uses the chromogenic Rambach
316 agar as its first plating agar. However, it provides the possibility of additional detection by
317 combining elements of broth and semi-solid agar enrichment (Carrique-Mas et al., 2009).
318 1.2. Quantification methods
319 Salmonella from infected tissues can be enumerated by direct plating, but most probable number
320 (MPN) techniques are necessary for faecal, feed or environmental samples. A miniaturised MPN
321 method has been described (and listed by ISO, 2012 (ISO/TS 6579-2:17-2; ISO, 2012) based on
322 Fravalo et al., (2003). Furthermore, quantitative real-time PCR methods have also been developed
323 (Zhang et al., 2020).
324 1.3. Identification of suspect colonies
325 Suspect colonies are subcultured onto selective and non-selective agars to ensure the absence of
326 possible contaminants, such as Proteus spp. If there is an abundant pure growth, suspect colonies
327 may be tested by slide agglutination with polyvalent Salmonella-typing antisera (Ellis et al., 1976). In
328 some cases, the suspect colony may not agglutinate or may auto-agglutinate and it is necessary to use
329 biochemical tests to confirm the identity. These tests can be performed using peptone water sugars or
330 commercial systems or composite media (such as triple sugar iron agar [TSI]), can be used to screen
331 organisms]) (Ewing, 1986). It is particularly important to ensure that Salmonella cultures used for
332 determination of antimicrobial resistance of live vaccine testing are not mixed with other organisms
333 such as Pseudomonas that are more likely to be multi-resistant or to mask auxotropism. MALDI-TOF is
334 also an acceptable and rapid method for identification of Salmonella (Dieckmann & Malorney, 2011).
335 The determination of the O factor(s) and the H antigen(s), and in special circumstances the Vi antigen
336 (present in S. Typhi, S. Paratyphi C and S. Dublin), is performed by direct slide agglutination or tube
337 agglutination using specific antisera. In the case of biphasic organisms, it is necessary to determine
338 both H phases, by the use of phase inversion – this involves passage through semi-solid agar
339 containing antiserum to the known phase. Screening is facilitated by the availability of antisera directed
340 against several factors, which can be pursued further by the use of monovalent typing sera. More
341 details on serotyping of Salmonella are described in ISO/TR (2014) 6579-3:2014 2017-3 and by
342 Grimont & Weill (2007). While many laboratories can identify the more common serovars, it is usually
343 necessary to use the facilities of a reference laboratory to confirm the identity of an isolate, including or
344 to conduct phage typing, if serovar-specific typing phages are available, and for genetic
345 characterisation. Additional biochemical or PCR tests may be necessary to identify some serovar
346 variants, e.g. d-tartrate fermentation, which can be used to differentiate S. Paratyphi B var. Java (d-
347 tartrate +) from S. Paratyphi B. Isolates should also be tested for their sensitivity to a range of
348 antimicrobial agents as there is increasing concern about the emergence of new multiple resistant
349 strains harbouring (transferable) resistance genes to cephalosporins, colistin and fluoroquinolones
14 OIE Terrestrial Manual 2022 7
15 Chapter 3.10.7. – Salmonellosis
350 (Figueiredo et al., 2015; Greene et al., 2008 Antonelli et al., 2019; Jajere, 2019). Live vaccine strains
351 are also commonly identified by antimicrobial resistance markers or biochemical changes such as
352 auxotrophism or roughness, as well as by commercial PCR kits or published PCR assays.
353 1.4. Immunological and nucleic acid recognition methods
354 Numerous alternative Salmonella detection methods are in use and some are commercially available.
355 These include immunomagnetic separation (IMS) (Park et al., 2011), reverse transcriptase real-time
356 (RT)-PCR (Park et al., 2014), enzyme-linked immunosorbent assay (ELISA) (Barrow, 1992; Wang et
357 al., 2015), real time PCR (Malorny et al., 2004), quantitative PCR (Piknova et al., 2005) and microarray
358 analysis (Porwollik et al., 2004; Rasooly & Herold, 2008). These methods may be used to identify
359 specific Salmonella serovars (Maurischat et al., 2015a) or to distinguish live vaccine strains from
360 Salmonella serovars infecting the flock or herd (Maurischat et al., 2015b). Some consist of a
361 combination of methods such as a two-step enrichment and real-time PCR (Krascseniscová et al.,
362 2008). Conventional or real-time quantitative PCR, sometimes including simultaneous identification of
363 key serovars (Heymans et al., 2018; Zhang et al., 2020), loop-mediated isothermal amplification
364 (LAMP) methods (Yang et al., 2018), enzyme-linked immunodiagnostic assays (Cetin et al., 2019) are
365 available. Many of these methods have not been fully validated for faecal and environmental samples,
366 although some progress has been made (Eriksson & Aspan, 2007; Malorny & Hoorfar, 2005). These ;
367 Heymans et al., 2018) and in the EU it is possible to validate alternative methods for statutory use by
368 following ISO16140-2, via an authorised certified organisation accreditation body. These rapid methods
369 are more suited to analysis of human foodstuffs, where inhibitors of the PCR reactions and competing
370 or cross-reacting organisms are not as problematic as for faeces. Optimisation of PCR detection
371 necessitates suitable DNA extraction techniques and controls to detect inhibition, which may reduce
372 the sensitivity of the test in some cases (Jensen et al., 2013; Kanki et al., 2009), though there is . One
373 of the main advantage of these methods in comparison with the cultural ones is their rapidity, and they
374 can be a role for rapid methods valuable diagnostic tool in test and release of batches of Salmonella-
375 free food and animal feedstuffs. The rapid methods are usually more expensive than conventional
376 culture, but can be economically viable for initial screening of materials where a low prevalence of
377 contamination is expected or where materials, such as feedstuffs, are held pending a negative test. An
378 enrichment/IMS method linked with enzyme-linked immunosorbent assay (ELISA) or PCR can identify
379 most Salmonella contamination within 24 hours (Wang et al., 2018). As currently none of the rapid
380 methods has been shown to be suitable for direct detection of low numbers of Salmonella in samples,
381 non-selective or selective enrichment stages are usually required (Oliveira et al., 2003). Typically this
382 introduces more steps and operator time in the detection procedure. For DNA-based methods,
383 inhibition of the PCR reaction by elements of the test sample matrix, especially in the case of faeces, is
384 problematic and requires suitable DNA extraction techniques and controls to detect inhibition, which
385 may reduce the sensitivity of the test in some cases (Jensen et al., 2013). There are many variations
386 and developments in rapid methods for Salmonella detection, but none has been shown to
387 satisfactorily replace culture in all circumstances.
388 In contrast, molecular methods for serotyping or subtyping Salmonella isolates are increasingly widely
389 used (EFSA, 2013) and some for outbreak investigation and source attribution (Munck et al., 2020).
390 Some kits using these methods are suitable for use in small laboratories that lack the facilities of a
391 reference laboratory. It is important that kits used have been fully validated in accordance with chapter
392 1.1.6. (Diep et al., 2019) and one is registered by the OIE. Multiplex PCR or whole genome
393 sequencing-based methods may be used to identify specific Salmonella serovars (Maurischat et al.,
394 2015a) or to distinguish live vaccine strains from Salmonella serovars infecting the flock or herd
395 (Maurischat et al.,2015b; Tang et al., 2019). A new ISO standard (ISO 16140-6 :2019) covers validation
396 of (sub)typing methods and is a prerequisite for such methods to be used to replace Salmonella
397 serotyping in statutory EU control programmes. It is important that kits used have been fully validated
398 in accordance with chapter 1.1.6. Kits should preferably be selected from those listed on the OIE
399 Register2.
400 2. Serological tests
401 2.1. Serological identification of infected animals, flocks and herds
402 A number of serological tests have been developed for the diagnosis of Salmonella infections in
403 animals. In poultry, the whole blood test, which uses a stained antigen, and the serum agglutination
404 test (SAT) have been used successfully for over 50 years for the identification of flocks infected with
405 S. Pullorum/ Gallinarum/ (biovars Gallinarum and Pullorum) (see Chapter 3.3.11). Because
406 S. Enteritidis possesses the same group D somatic antigen as S. Pullorum/ Gallinarum and is thought
407 to originate from it a common ancestor (Thomson et al., 2008), the whole blood test and related tests
2
16 http://www.oie.int/en/scientific-expertise/registration-of-diagnostic-kits/the-register-of-diagnostic-kits/
17 8 OIE Terrestrial Manual 2022
18 Chapter 3.10.7. – Salmonellosis
408 can be used for the diagnosis of S. Enteritidis infection, but the sensitivity is low. In recent years, Other
409 tests, such as the ELISA (Barrow, 1994 Feld et al., 2000) have been developed for the diagnosis of S.
410 Enteritidis and S. Typhimurium infections in poultry and for other serovars in farm animals. The ELISA
411 has been used effectively to identify serologically S. Dublin carrier cattle and can be applied to bulk
412 milk for screening dairy herds. An ELISA that includes somatic antigens from a mix of serovars (“mix-
413 ELISA”) is used in Denmark, Germany, the Netherlands, the United Kingdom, and some other several
414 countries on serum or tissue fluid released by freezing then thawing muscle samples to detect
415 Salmonella infections in pigs (Nielsen et al., 1998). A similar test can be used to detect antibodies to
416 S. Enteritidis and S. Typhimurium in egg yolk from unvaccinated commercial laying flocks. Several
417 ELISAs are available as commercial kits, but their performance can be variable (Van der Heijden,
418 2001). Some ELISAs are now in routine use and a number are available commercially. There is a need
419 for standardisation of their use and, to this end, panels of control sera are available commercially from
420 Denmark3 and the Netherlands4.
421 2.2. Factors affecting serological diagnosis
422 1. Serological methods should be used to identify infected flocks/herds rather than to identify
423 infected individual animals, although repeated herd tests can be used as an aid to selective
424 culling of chronic carrier animals. Serological tests are normally designed to detect a limited range
425 of Salmonella serovars or serogroups.
426 2. It is well recognised that some animals with a positive serological response may no longer be
427 infected with Salmonella organisms, and in countries with a low prevalence of salmonellosis
428 specificity issues mean that most positive results will be false. Animals that are actively excreting
429 shedding salmonellae may be serologically negative in the early stages of disease and some
430 individual infected animals never seroconvert. Animals that are serologically positive may have
431 ceased to excrete shed salmonellae although circulating immunoglobulin concentrations may
432 remain high. Other, especially in latent carrier animals, but other animals on the farm may still be
433 shedding intermittently. Serologically negative animals may result from a recent infection causing
434 excretion and shedding before immunoglobulin production is maximal, or infection with less
435 invasive serovars. Animals that have been infected recently would, in all probability, eventually be
436 detected serologically by an appropriate monitoring programme throughout the life of the
437 flock/herd but there are often cost limitations to the application of effective monitoring
438 programmes.
439 3. Newborn animals are immunologically immature and do not respond serologically to the somatic
440 LPS antigen until 2–3 weeks of age. They do, however, produce a serological response to the
441 flagellar protein antigens. Cattle may be unresponsive until about 10–12 weeks of age, and
442 suckling pigs may fail to develop an immune response or have an antibody response that reflects
443 maternal immunity. Differential responses involving different antibody classes (IgM, IgA, IgG) can
444 be used in pigs to help differentiate recent infection from infection that occurred some time ago,
445 but this is often not useful for herd testing where individuals are usually at different stages of
446 infection. Most tests are based on IgG and raised antibody levels typically appear 1–3 weeks after
447 infection and last 2–3 months.
448 Chickens may also acquire anti-Salmonella antibodies passively from their parents via the
449 antibodies in egg yolk sac; this may indicate an infected or vaccinated parent flock. Mammals can
450 acquire maternally derived antibodies via the colostrum.
451 4. Immunisation has been used for many years to aid control of certain Salmonella infections in farm
452 animals, and if diagnostic serology is to be used, it is necessary to differentiate the vaccine
453 response from that of actual infection. Many live vaccines given orally do not provoke a significant
454 serum antibody response in the majority of animals, but there may be occasional exceptions that
455 are difficult to interpret. Injectable killed vaccines used for control of S. Enteritidis Salmonella in
456 chickens may produce a very prolonged antibody response. Live marker vaccines have been
457 produced and can be distinguished from field challenge strains because, depending on the
458 adjuvant used. No true DIVA (detection of infection in vaccinated animals) test is readily available
459 for specific identification of their antimicrobial resistances the antibody response to rifampicin and
460 by real-time PCR assays (Maurischat et al., 2015b) vaccination, but in the case of S. Gallinarum/
461 (biovars Gallinarum and Pullorum), combined use of a LPS and flagella-based ELISA can help
462 exclude the possibility of a false positive reaction in a flock vaccinated for S. Enteritidis.
463 5. The effect of antibiotic therapy on the serological response remains unclear. Some workers found
464 reduced titres following therapy whereas others found no effect. Serology, however, may be a
3
19 Statens Serum Institut, Copenhagen, Denmark (www.ssi.dk)
4
20 GD, Deventer, the Netherlands (www.gddeventer.com)
21 OIE Terrestrial Manual 2022 9
22 Chapter 3.10.7. – Salmonellosis
465 more useful diagnostic technique for salmonellosis than culture if antimicrobial therapy has been
466 used.
467 6. Over 2600 different Salmonella serovars exist. Depending on the antigen and test used,
468 serological cross-reactions between different serovars may occur, e.g. S. Typhimurium, S.
469 Abortusequi, S. Pullorum Gallinarum and S. Enteritidis. In some cases cross-reactions may also
470 occur as a result of exposure to organisms other than Salmonella.
471 7. In poultry, egg yolk may be tested for immunoglobulins to Salmonella, and eggs may provide a
472 method to screen flocks. This approach is used for monitoring commercial laying flocks in
473 Denmark. In cattle, milk may be tested for anti-Salmonella antibodies to screen dairy herds.
474 8. The use of filter-paper discs for serum collection obviates the necessity to separate serum. The
475 discs also provide long-term storage and reduce transport costs to the laboratory. The sensitivity
476 of the test may be slightly reduced compared with tests carried out on fresh serum.
477 2.3. The whole blood test
478 The whole blood test provides a rapid test for fowl typhoid and Pullorum disease that can be used on
479 the farm. The sensitivity of the whole blood test is low and in inexperienced hands false-positive and
480 false-negative results may be recorded. For a detailed description of the whole blood test, see chapter
481 3.3.11.
482 2.4. Rapid slide agglutination test
483 Serum (0.02 ml) is mixed with polyvalent crystal-violet-stained antigen (0.02 ml). The tile is rocked
484 gently for 2 minutes, after which the test is read. The test components are stored at 4°C and must have
485 reached room temperature before being used.
486 Test sera should be free from contamination and haemolysis. It may be helpful to centrifuge serum
487 samples that have been stored for any period of time.
488 If nonspecific false-positive reactions are suspected, positive/suspicious sera may be retested after
489 heat-inactivation at 56°C for 30 minutes.
490 2.5. Serum agglutination test
491 The SAT is relatively insensitive, and many older animals may have low levels of agglutinins in their
492 sera caused by enterobacteria other than Salmonella. Single samples are of little diagnostic value
493 except for initial screening on a herd basis. Paired samples are needed as the minimum requirement
494 for confirmation of active infection. The test is relatively inexpensive simple; the antigens can be readily
495 prepared and expensive equipment is not necessary. The SAT can be adapted to the microtitre format
496 and can be readily used to determine somatic and flagellar titres. It is advisable to use standard sera
497 and other confirmatory methods for quality control of the purity and immunogenicity of SAT antigen
498 preparation(s) that are not dependant on sera produced from those antigens. This method has been
499 used for identification of exposure to various Salmonella serovars, e.g. S. Typhimurium, S. Enteritidis,
500 S. Dublin, S. diarizonae in turkeys, and S. Abortusequi.
501 2.5.1. Preparation of somatic antigen
502 i) Plate out the Salmonella culture from the appropriate stock culture onto a blood agar base
503 (BAB) plate, or other suitable medium, for single colony growth. Incubate overnight at
504 37°C (±2°C).
505 ii) Select a smooth colony and carry out a slide agglutination test to ensure that the required
506 somatic antigen is present.
507 iii) Using a sterile loop, inoculate a nutrient agar slope in a universal container from the
508 selected colony.
509 iv) Incubate the culture for 8–12 hours at 34–38°C 37°C (±2°C).
510 v) Using a Pasteur pipette, wash off the culture, preferably inside a safety cabinet, with
511 approximately 2 ml of absolute alcohol, and transfer into a sterile universal container.
512 vi) Leave the antigen for 4–6 hours at room temperature to enable the alcohol to kill the
513 bacteria and detach flagella.
514 vii) Spin the universal container in a bench-top centrifuge for 5 minutes at 1000 g. Pour off the
515 liquid and add enough phenol saline to make the antigen up to an opacity equivalent to
23 10 OIE Terrestrial Manual 2022
24 Chapter 3.10.7. – Salmonellosis
516 Brown’s tube No. 2 (approximately 108 colony-forming units/ml) or other appropriate
517 standard.
518 viii) Carry out standard titration with known serum to ensure that the antigen is positive for the
519 required factor.
520 ix) Store in a refrigerator at 4°C until required.
521 2.5.2. Preparation of flagellar antigens
522 i) Plate out the appropriate Salmonella stock culture on to a BAB plate, or other appropriate
523 medium. Incubate overnight at 34–38°C 37°C (±2°C).
524 ii) Passage in semi-solid agar (about 0.3%) in a Craigie’s tube, or other suitable container, to
525 induce optimum expression of the appropriate flagellar antigen. If the serovar is biphasic,
526 H antiserum corresponding to the phase to be suppressed is added to the agar.
527 iii) Use slide agglutination to check that the Salmonella is in the required phase. If this is
528 correct, inoculate a loop of culture into 20 ml of nutrient broth. Incubate for 12–18 hours at
529 34–38°C 37°C (±2°C) for optimum growth. (If the phase is incorrect, re-passage through
530 semi-solid agar.)
531 iv) Pipette 250 µl of 40% formaldehyde into the antigen suspension (use gloves and
532 preferably work in a safety/fume cabinet), and leave overnight.
533 v) Test the antigen by SAT using the appropriate typing serum.
534 2.5.3. Test procedure
535 i) It is easiest to screen the sera at a dilution of 1/20; 0.25 ml of antigen is added to 0.25 ml
536 of serum pre-diluted to 1/10 in normal saline.
537 ii) The tests are incubated in a water bath at 50°C for 24 hours in the case of somatic
538 antigens and for 4 hours for the flagellar antigens. The dilution and time of incubation will
539 vary depending on the antisera that are used.
540 iii) Sera that give a positive reaction are then diluted from 1/20 to 1/320 and retested with the
541 appropriate antigen.
542 2.6. Enzyme-linked immunosorbent assays for Salmonella Enteritidis
543 Two main basic systems are available for detection of IgG (IgY) specific for S. Enteritidis: the indirect
544 ELISA and the competitive ‘sandwich type’ ELISA (Barrow, 1994 Barrow& Methner, 2013).
545 The indirect ELISA involves the use of a detecting antigen coated on to the wells of a microtitre plate.
546 After the application of a blocking reagent to reduce nonspecific binding, test samples are applied to
547 the wells. Specifically bound antibody in the sample is detected by an antibody/enzyme conjugate. A
548 variety of antigens, including LPS, flagella, SEF14 fimbriae, outer membrane proteins and crude whole
549 cell antigen preparations have been used.
550 The competitive sandwich ELISA employs a specific reagent – a monoclonal antibody (MAb) or
551 polyclonal antibody – for coating antigen to wells. This is then followed by a pure or crude antigen
552 preparation. Test samples are applied followed by conjugated antibody, which will not bind to the
553 antigen if the sample contained specific antibodies. The assay time can be shortened by adding both
554 test sample and conjugate together. MAbs have been prepared for LPS, flagella and SEF14 for
555 S. Enteritidis.
556 There are advantages and disadvantages to both systems. The indirect assay is simpler and reagents
557 are available for all Salmonella serovars of chickens, turkeys, ducks and mammalian hosts. The
558 competitive ELISA can be applied to all animal species and in general shows higher specificity.
559 However, reagents are not available commercially for all most serovars. There are also some affinity
560 problems and it may be less sensitive than the indirect assays. In the field, both systems have
561 produced false-positive reactions and in some cases screening with an indirect LPS ELISA may be
562 followed by confirmation with a flagellar competitive ELISA. This combination has been used to
563 differentiate S. Enteritidis field infection from a vaccinal response to S. Gallinarum 9R vaccine, which
564 lacks flagellar antigens.
565 Both types of assay may be used with serum, egg yolk or reconstituted dried blood eluted from filter
566 paper discs. A mix-ELISA (or meat-juice ELISA), is used in Denmark and other countries to detect
567 Salmonella infections in pigs (Nielsen et al., 1998 Van der Heijden, 2001). This ELISA contains the ‘O’
25 OIE Terrestrial Manual 2022 11
26 Chapter 3.10.7. – Salmonellosis
568 LPS antigens 1, 4, 5, 6, 7 and 12, from S. Typhimurium and S. Choleraesuis, which enables it to detect
569 serologically up to 95% of the Salmonella serogroups found in pigs in most European countries. Group
570 D antigens have also been added to some ELISA kits. Serum is used to screen breeding and
571 multiplying herds, whereas for pigs in the abattoir, the assay is usually performed on the tissue fluid
572 (‘meat-juice’) that is liberated when a frozen 10 g muscle sample is thawed. This approach is used in
573 most countries, but serum collected from the major blood vessels of the viscera can provide more
574 sensitive and specific results.
575 With some ELISAs differentiation can be made between infections produced by Salmonella serovars
576 from different serogroups. Some cross-reaction occurs can occur between groups B and D and other
577 invasive serovars. There is, however, usually a greater antibody response when LPS from the
578 homologous serovar is used in the ELISA. The optimal method for choosing a ‘cut-off’ absorbance
579 value, above which sera are designated as having come from an S. Enteritidis-infected flock, without
580 producing an unacceptable level of false-positive tests, has not yet been decided on and agreed upon
581 internationally, and in the EU, ELISA testing is less commonly used because of the extensive use of
582 vaccination against S. Enteritidis and S. Typhimurium, particularly in laying hen and broiler breeder
583 flocks.
584 ELISAs are readily adapted to automation and hence to large-scale testing programmes. A major
585 problem is that expensive equipment is necessary and many of the reagents are also expensive.
586 Several commercial ELISA kits for S. Enteritidis, S. Typhimurium and Group B/C mix-ELISAs are
587 available. An ELISA kit for S. Abortusovis has recently been added to the OIE register of diagnostic
588 kits5; there is a need for a similar validated test for S. Abortusequi.
589 Ideally these should be validated by international ring trials before adoption for surveillance purposes.
590 An example of a validated in-house ELISA is the one developed at the OIE Reference Laboratory at
591 APHA Weybridge6 (see Table in Part 4 of this Terrestrial Manual for address).
592 The requirements are given below.
593 2.6.1. Equipment
594 PVC plates; appropriate pipettes and measuring cylinders; ultrawash microtest plate washer;
595 ELISA plate reader; test filter of 405–410 nm and reference filter of 630 nm.
596 2.6.2. Antigen
597 i) Phenol-extracted S. Enteritidis LPS is available commercially. This is reconstituted in 1 ml
598 deionised water and stored at –20°C in 100-µl aliquots in phosphate buffered saline (PBS),
599 pH 7.2, at a concentration of 2.5 mg/ml. For use, the antigen should be thawed in coating
600 buffer at the appropriate concentration.
601 ii) The LPS antigen can also be prepared by the technique of Westphal & Luderitz (1954)
602 and standardised as to its carbohydrate concentration by the method of Gerhardt (1981),
603 and adjusted to 1000 µg/ml.
604 2.6.3. Serum and conjugate diluent
605 Add bovine serum albumin (BSA) (2 g) and Tween 20 (0.05 ml) to PBS (100 ml). (Alternatively,
606 powdered milk [1 g] can replace the BSA.) Store at 4°C and make fresh solutions every week.
607 i) Coating buffer
608 Add sodium carbonate (1.59 g) and sodium bicarbonate (2.93 g) to deionised water
609 (1 litre) and adjust to pH 9.6. Store at 4°C and renew every 2 weeks.
610 ii) Substrate buffer
611 Make a 10% (v/v) solution of diethanolamine in deionised water. The diethanolamine
612 should be pre-warmed to 37°C before dispensing, and the pH of the solution should be
613 adjusted to pH 9.8 with 1 M hydrochloric acid. Store at 4°C and renew every 2 weeks.
614 iii) Enzyme conjugate
5
27 https://www.oie.int/en/what-we-offer/veterinary-products/diagnostic-kits/the-register-of-diagnostic-kits/
6
28 https://www.oie.int/en/what-we-offer/expertise-network/reference-laboratories/#ui-id-3
29 12 OIE Terrestrial Manual 2022
30 Chapter 3.10.7. – Salmonellosis
615 Goat anti-chicken immunoglobulin conjugated to alkaline phosphatase or other species
616 anti-chicken globulin. Store at 4°C diluted in diluent at the appropriate concentration and
617 renew every week.
618 iv) Enzyme substrate
619 Dissolve one tablet of p-nitrophenyl phosphate disodium (5 mg) in substrate buffer (5 ml)
620 no earlier than 30 minutes before dispensing, and store in the dark.
621 2.7. Standards
622 i) Positive control antiserum prepared by intramuscular inoculation of four 1-week-old specific
623 pathogen free (SPF) chickens with an inoculum containing 10 6 S. Enteritidis. The serum is
624 subsequently obtained 3–4 weeks later when antibody titres are maximal.
625 ii) Negative control serum A from four 1-week-old SPF birds.
626 iii) Negative control serum B from 58 1-week-old breeders known to be free from Salmonella
627 infections. Pool the sera and store in 100 µl volumes at –20°C.
628 C. REQUIREMENTS FOR VACCINES
629 1. Background
630 1.1. Rationale and intended use of the product
631 Many inactivated vaccines are used against salmonellosis caused by different serovars in various
632 animal species, including a combined S. Enteritidis and S. Typhimurium vaccine for use in poultry, and
633 a more recent vaccine that also includes S. Infantis. Inactivation is usually achieved by either heating
634 or the use of formalin and an adjuvant, such as alhydrogel or mineral oil. Live vaccines have also been
635 used in a number of countries; these include the semi-rough strains, such as 9R for fowl typhoid and
636 HWS51 for S. Dublin infections (Mastroeni et al., 2001). Other attenuated vaccines include auxotrophic
637 and ‘metabolic drift’ mutants, which are used to prevent Salmonella infections in farm animals in
638 Germany and Europe, particularly for S. Enteritidis and S. Typhimurium in poultry and S. Typhimurium
639 in pigs the United Kingdom and other countries. Mutant vaccines attenuated rationally by molecular
640 biological gene-deletion techniques have been developed for poultry and other species; these include
641 aroA mutants and strains with mutations in the genes encoding adenylate cyclase (cya) and the cyclic
642 adenosine monophosphate receptor protein (crp) (Desin et al., 2013; Hassan & Curtiss III, 1997
643 Redweik et al., 2020). Attenuation of live vaccines is essential to limit intestinal replication and
644 persistence in the animals and environment, ideally without influencing the immunogenicity, but such
645 attenuation is unlikely to have no impact on the vaccinal response (Redweik et al., 2020). Guidelines
646 for the production of veterinary vaccines are given in Chapter 1.1.8 Principles of veterinary vaccine
647 production. The guidelines given here and in chapter 1.1.8 are intended to be general in nature and
648 may be supplemented by national and regional requirements. Most vaccines are produced as highly
649 industrial commercial processes and are regulated by national veterinary medicines licensing
650 regulatory approval authorities. Smaller quantities of emergency herd vaccines or autogenous vaccines
651 are produced by private laboratories and vaccine manufacturers, but each production has to be
652 specifically licensed approved.
653 2. Outline of production and minimum requirements for conventional vaccines
654 2.1. Characteristics of the seed
655 2.1.1. Biological characteristics
656 For killed or live vaccines, the bacterial strain should be an organism as closely related to
657 currently circulating field strains as possible. It should be carefully chosen from cases of severe
658 clinical disease, and virulence and antigen production should be assessed. It is best to evaluate
659 a panel of potential strains in this way before testing the final selection. The final vaccinal strain
660 should be identified by historical records and characterised by stable phenotypic or genetic
661 markers. Live vaccinal strains should be marked by stable characters allowing distinction from
662 wild strains. Markers, such as resistance to antimicrobials, for example rifampicin, or
663 auxotrophism, may be used. Attenuation of virulence should be stable and preferably obtained
664 by two independent defined mutations. The stability of live vaccine strains can be verified by
31 OIE Terrestrial Manual 2022 13
32 Chapter 3.10.7. – Salmonellosis
665 regular checks using a sensitive molecular fingerprinting and micro-array techniques, preferably
666 whole genome sequencing.
667 2.1.2. Quality criteria (sterility, purity, freedom from extraneous agents)
668 i) Sterility and purity
669 The vaccine strain must be checked as follows:
670 a) Staining of a smear of bacterial suspension on a glass slide using the Gram stain.
671 b) Homogeneity of culture on non-selective media.
672 c) Metabolic requirements as indicated by biochemical tests.
673 d) Detection of molecular markers, serotype and phage type, if applicable.
674 e) Agglutination with specific antiserum.
675 f) The vaccine culture and any adjuvants, preservatives or other materials must be
676 microbiologically sterile and non-toxic at the concentrations used.
677 ii) Safety
678 The LD50 (50% lethal dose) or ID 50 (50% infectious dose) may be determined in mice or
679 preferably signs of more mild adverse reactions should be checked in the target species.
680 Ten times the field dose of live vaccine or twice the dose for killed vaccines must be given
681 to the target species at the recommended age and by the recommended route. The
682 animals are observed for absence of adverse reactions. Stability and non-reversion to
683 virulence after serial passages in susceptible species should be shown for live vaccines. It
684 is also necessary to consider repeat vaccination. Live vaccine should be shown not to
685 persist for long in vaccinated animals and in the environment where they are farmed, or be
686 transmitted to milk or eggs that may be consumed, and the method of application should
687 not present a hazard to operators. Live vaccines should not be used in commercial laying
688 flocks during the laying period unless eggs are processed by heat treatment.
689 iii) Efficacy
690 Laboratory experiments and field trials should be used to show that the vaccine is
691 effective. The laboratory experiments consist of vaccination–challenge tests in the target
692 species at the recommended dose and age. The efficacy data can also be used as the
693 basis for a batch potency test. Field trials are more difficult to undertake with respect to
694 testing efficacy because of difficulties with standardising the challenge and providing
695 appropriate controls.
696 iv) Environmental aspects
697 Live vaccine strains should be tested for their ability to persist in the environment and
698 infect non-target species such as rodents and wild birds that are likely to be exposed.
699 Prolonged survival of some live vaccines in faeces and litter may present an unacceptable
700 environmental hazard when the material is removed from the animal houses. Live
701 vaccines should not be used in commercial laying flocks during lay.
702 2.2. Method of manufacture
703 2.2.1. Procedure
704 The seed culture is propagated and maintained using suitable media for growth of Salmonella.
705 The media used should not contain serum or animal tissues (unless permitted by national
706 regulations). Culture may be on solid medium, in Roux flasks, or in liquid medium, in which case
707 large-scale fermentation equipment may be used. Iron limitation or low temperature incubation
708 on a minimal media may enhance LPS antigen production by the vaccine strain.
709 Vaccine must be produced in suitable clean rooms to which only approved personnel have
710 access. Care must be taken to avoid cross-contamination between areas where live organisms
711 are processed and other areas. Contamination from operators or the environment must be
712 avoided and vaccine preparation should take place in a separate area from diagnostic culture
713 work. Operators must not work with vaccine whilst ill and must not be subject to
714 immunosuppressive conditions or medications. Personnel must be provided with suitable
715 protective clothing in production areas and in animal rooms.
33 14 OIE Terrestrial Manual 2022
34 Chapter 3.10.7. – Salmonellosis
716 Seed-lot cultures are prepared from the primary seed-lot, and the number of passages is
717 dependent on the validation of the process. The vaccine may be prepared by inoculation of a
718 suitable medium, such as nutrient broth, with a fresh culture and incubation on a shaker at 37°C
719 for 24 hours, with or without aeration. The organisms are harvested by sedimentation or
720 centrifugation. Alternatively, the organisms may be grown on and harvested from a solid
721 medium, such as nutrient agar. In the case of live vaccines, the suspension is diluted in PBS,
722 pH 7.0, and may be freeze-dried.
723 The time of inactivation of dead vaccines should be at least 33% more than that taken to reduce
724 the viable number to an undetectable level. The inactivation process must be applied to the
725 whole volume of the vaccine cell harvest and confirmed by a sensitive culture method.
726 Preservatives, excipient for lyophilisation, stabiliser for multidose containers or other substances
727 added to or combined with a vaccine preparation must have no deleterious effect on the
728 immunising potency of the product.
729 2.2.2. Requirements for substrates and media
730 All chemicals and growth media used should be guaranteed to be fit for purpose and checked
731 by the use of suitable controls.
732 2.2.3. In-process controls
733 The following points require attention:
734 i) Visual control of the suspension, homogeneity by Gram stain, culture on non-selective
735 medium.
736 ii) Slide agglutination with specific antisera.
737 iii) Titration of bacteria by turbidimetry or plate count.
738 iv) Test of effective inactivation (killed vaccine) by plating on non-selective medium or use of
739 a medium that gives optimum chance of recovery e.g. production medium with
740 neutralisation of the inactivating compound.
741 v) Titration of viable bacteria (living vaccine) before and after lyophilisation.
742 2.2.4. Final product batch tests
743 i) Sterility/purity
744 Tests for sterility and freedom from contamination of biological materials intended for
745 veterinary use are found in chapter 1.1.9 of this Terrestrial Manual.
746 ii) Safety
747 A laboratory test that has previously shown a correlation with safety in the target species
748 may be used to determine the absence of deleterious effects on vaccinated animals. Each
749 batch should be tested in the target species at the recommended age and route, using at
750 least twice the field dose for killed vaccines and ten times the dose for live vaccines.
751 Observations are made on any adverse effects on the demeanour and health of the
752 vaccinated animals and an assessment is made of tissue reactions at the injection site.
753 iii) Batch potency
754 Potency is tested using vaccination–challenge assay in mice or other species, including (if
755 practicable) the target species and immunological response in target species. Many
756 Salmonella vaccines are intended for use in poultry so these should be used for potency
757 and safety tests.
758 2.3. Requirements for authorisation regulatory approval
759 2.3.1. Safety requirements
760 Certain killed vaccines may occasionally cause abortion in pregnant animals because of their
761 LPS content, and likewise live vaccines should be used with caution in pregnant animals. It is
762 often necessary, however, to vaccinate pregnant animals to provide maternal immunity for their
763 offspring. It may be useful to include endotoxin assay in the safety test programme so that the
35 OIE Terrestrial Manual 2022 15
36 Chapter 3.10.7. – Salmonellosis
764 levels can be compared with those shown to be safe in the double-dose tests. Vaccines may
765 also cause swelling at the site of injection, particularly if an oil-emulsion adjuvant is used.
766 i) Target and non-target animal safety
767 Killed vaccines are assessed in a double-dose test, and live vaccines are assessed in a
768 test using ten times the dose, ideally in the target species. Live vaccines should be proven
769 to be harmless in relevant non-target species that could be exposed to vaccine excreted
770 by vaccinated animals.
771 ii) Reversion to virulence for attenuated/live vaccines
772 Live vaccines shall be shown in replication tests in target species to not revert to virulent
773 strains during a suitably large number of replications. Mutations, especially undefined
774 mutations, should be shown to be stable and checks on stability can be made by sensitive
775 molecular fingerprinting methods or sequencing. Although the risk is small it is wise not to
776 use live vaccines in a country where the organism in the vaccine has been eradicated.
777 iii) Environmental consideration
778 Live vaccines should not be able to replicate in the environment or persist for more than a
779 short period.
780 2.3.2. Efficacy requirements
781 i) For animal production
782 The duration of immunity is likely to vary considerably between products, vaccination
783 regimes and individual vaccinated animals. Immunity to Salmonella is normally serovar or
784 serogroup specific. Consultation among colleagues suggests that most killed vaccines will
785 provide some protection for 6 months, while some live vaccines given by injection may
786 elicit stronger immunity, which may persist for 1 year or more. It should be remembered,
787 however, that a strong challenge such as that associated with continuously occupied farms
788 or infected rodents may overwhelm vaccinal immunity and commercial live vaccines may
789 be attenuated to reduce environmental survival in a way that reduces the immune
790 response. There may also be problems with ensuring effective oral administration with live
791 vaccines or accuracy of injection with killed and live injectable vaccines. The Salmonella
792 vaccines are intended to limit the extent of clinical disease in the case of ruminants, pigs
793 and S. Gallinarum in poultry. If possible, the potency test should relate to the efficacy of
794 the vaccine in the target species, and suitable criteria should be applied for passing
795 batches. It may be possible to assess killed vaccines by the O-H antibody response
796 produced, although it should be remembered that serum antibodies are only part of the
797 host’s protective mechanism against Salmonella. Alternatively, the potency of the vaccine
798 may be assessed by its effect on challenged vaccinated animals compared quantitatively
799 and statistically with unvaccinated controls.
800 ii) For control and eradication
801 Vaccines for Salmonella are not capable of eradicating infection from herds or flocks but
802 can increase the threshold for infection, reduce the level of excretion shedding of the
803 organism and reduce vertical transmission in poultry that results in contamination of
804 hatching or table eggs. Vaccination is therefore an aid to other eradication and control
805 measures such as culling, all in-all out production, biosecurity and farm hygiene.
806 iii) Stability
807 Information is lacking on the stability of killed vaccines. Stability is affected by storage
808 conditions and by the presence of contaminating microorganisms growing in the product.
809 Chemicals with antimicrobial activity, such as thiomersal, phenol or crystal violet are often
810 included as preservatives in killed bacterial vaccines. The stability is assessed by potency
811 tests repeated at appropriate time intervals. The stability of live vaccines can be assessed
812 by performing counts of the number of viable organisms repeated at appropriate time
813 intervals, and genotyping tests to identify genetic changes during fermentation production.
814 It is recommended that live vaccines that contain Salmonella serovars that are not
815 endemic in a particular region should not be used for control of other serovars (van
816 Immerseel et al., 2013).
817 REFERENCES
37 16 OIE Terrestrial Manual 2022
38 Chapter 3.10.7. – Salmonellosis
818 ANTONELLI P., BELLUCO S., MANCIN M., LOSASSO C. & RICCI A. (2019). Genes conferring resistance to critically
819 important antimicrobials in Salmonella enterica isolated from animals and food: a systematic review of the
820 literature, 2013–2017. Res. Vet. Sci., 126, 59–67.
821 BARROW P.A. (1992). ELISAs and the serological analysis of salmonella infections in poultry: a review. Epidemiol.
822 Infect., 109, 361–369.
823 BARROW P.A. (1994). Serological diagnosis of Salmonella serotype Enteritidis infections in poultry by ELISA and
824 other tests. Int. J. Food Microbiol., 21, 55–68.
825 BARROW P.A. & METHNER U., EDS (2013). Salmonella in Domestic Animals, Second Edition. CAB International,
826 Wallingford, Oxon, UK. ISBN: 9781845939021; doi:10.1079/9781845939021.0000
827 BARROW P.A. & NETO O.F. (2011). Pullorum disease and fowl typhoid – new thoughts on old diseases: a review.
828 Avian Pathol., 40, 1–13.
829 CANNON R.M. & NICHOLLS T.J. (2002). Relationship between sample weight, homogeneity, and sensitivity of fecal
830 culture for Salmonella enterica. Vet. Diagn. Invest., 14, 60–62.
831 CARRIQUE-MAS J.J., BARNES S., MCLAREN I. & DAVIES R. (2009). Comparison of three plating media for the
832 isolation of Salmonella from poultry environmental samples in Great Britain using ISO 6579:2002 (Annex D). J.
833 Appl. Microbiol., 107, 1976–1983.
834 CARRIQUE-MAS J.J. & DAVIES R.H. (2008). Sampling and bacteriological detection of Salmonella in poultry and
835 poultry premises: A review. Rev. sci. tech. Off. int. Epiz., 27, 665–677.
836 CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC) (2021). Salmonella. Available at:
837 https://www.cdc.gov/salmonella/index.html (accessed on 6 January 2021).
838 CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC) (2013). An Atlas of Salmonella in the United States,
839 1968–2011: Laboratory-based Enteric Disease Surveillance. Atlanta, Georgia: US Department of Health and
840 Human Services, CDC, Atlanta, Georgia, USA.
841 CETIN E., TEMELLI S. & EYIGOR A. (2019). Salmonella prevalence and serovar distribution in healthy slaughter
842 sheep and cattle determined by ISO 6579 and VIDAS UP Salmonella methods. J. Food Sci. Technol., 56, 5317–
843 5325.
844 DESIN T.S., KOSTER W. & POTTER A.A. (2013). Salmonella vaccines in poultry: past, present and future. Exp. Rev.
845 Vaccines, 12, 87–96.
846 DIECKMANN R. & MALORNY B. (2011). Rapid screening of epidemiologically important Salmonella enterica subsp.
847 enterica serovars by whole-cell matrix-assisted laser desorption ionization-time of flight mass spectrometry . Appl.
848 Environ. Microbiol., 77, 4136–4146.
849 DIEP B., BARRETTO C., PORTMANN A-C., FOURNIER C., KARCZMAREK A., VOETS G., LI S., DENG X. & KLIJN A.
850 (2019). Salmonella serotyping; comparison of the traditional method to a microarray-based method and an in
851 silico platform using whole genome sequencing data. Front. Microbiol., 10, 2554.
852 ELLIS E.M., WILLIAMS J.E., MALLINSON E.T., SNOEYENBOS G.H. & MARTIN W.J. (1976). Culture Methods for the
853 Detection of Animal Salmonellosis and Arizonosis. Iowa State University Press, Ames, USA.
854 ERIKSSON E. & ASPAN A. (2007). Comparison of culture, ELISA and PCR techniques for salmonella detection in
855 faecal samples for cattle, pig and poultry. BMC Vet. Res., 3, 21–40.
856 EUROPEAN FOOD SAFETY AUTHORITY (EFSA) (2013). EFSA BIOHAZ Panel (EFSA Panel on Biological Hazards).
857 Scientific Opinion on the evaluation of molecular typing methods for major food-borne microbiological hazards
858 and their use for attribution modelling, outbreak investigation and scanning surveillance: Part 1 (evaluation of
859 methods and applications). EFSA Journal, 11, 3502 [84 pp.]. doi:10.2903/j.efsa.2013.350.
860 EWING W.H. (1986). Edwards and Ewing’s Identification of Enterobacteriaceae, Fourth Edition. Elsevier, New
861 York, USA, London, UK, and Amsterdam, the Netherlands.
39 OIE Terrestrial Manual 2022 17
40 Chapter 3.10.7. – Salmonellosis
862 FIGUEIREDO R., HENRIQUES A., SERENO R., MENDOÇA N. & DA SILVA G.J. ( 2015). Antimicrobial resistance and
863 extended-spectrum β-lactamases of Salmonella enterica serotypes isolated from livestock and processed food in
864 Portugal: an update. Foodborne Pathog. Dis., 12, 110–117.
865 FRAVALO P., HASCOET Y., LEFELLIC M., QUEGUINER S., PETTON J. & SALVAT G. (2003). Convenient method for
866 rapid and quantitative assessment of Salmonella enterica contamination: The mini-MSRV MPN technique. J.
867 Rapid Method Automat. Microbiol., 11, 81–88.
868 FRICKER C.R. (1987). The isolation of salmonellas and campylobacters. J. Appl. Bacteriol., 63, 99–116.
869 FELD N.C., EKEROTH L., GRADEL K.O., KABELL S. & MADSEN M. (2000). Evaluation of a serological Salmonella Mix-
870 ELISA for poultry used in a national surveillance programme. Epidemiology & Infection, 125, 263–268.
871 FORD L., HAYWOOD P., KIRK M.D., LANCSAR E., WILLIAMSON D.A. & GLASS K. (2019). Cost of Salmonella Infections
872 in Australia, 2015. J. Food Protection, 82, 1607–1614.
873 GERHARDT P. (1981). Manual of Methods for General Microbiology. American Society for Microbiology,
874 Washington DC, USA, 332–334.
875 GREENE S.K., STUART A.M., MEDALLA F.M., WHICHARD J.M., HOEKSTRA R.M. & CHILLER T.M. (2008). Distribution of
876 multidrug-resistant human isolates of MDR-ACSSuT Salmonella Typhimurium and MDR-AmpC Salmonella
877 Newport in the United States, 2003–2005. Foodborne Pathog. Dis., 5, 669–680.
878 GRIMONT P.A.D. & WEILL F.-X. (2007). Antigenic Formulae of the Salmonella Serovars, Ninth Edition, World
879 Health Organization Collaborating Centre for Reference and Research on Salmonella. Institut Pasteur, Paris,
880 France.
881 HARVEY R.W.S. & PRICE T.H. (1974). Isolation of Salmonellas. Public Health Laboratory Service. Monograph
882 Series 8. Her Majesty’s Stationery Office, London, UK.
883 HASSAN J.O. & CURTISS R. III (1997). Efficacy of a live avirulent Salmonella typhimurium vaccine in preventing
884 colonization and invasion of laying hens by Salmonella typhimurium and Salmonella enteritidis. Avian Dis., 41,
885 783–791.
886 HEYMANS R., VILA A., VAN HEERWAARDEN C.A., JANSEN C.C., CASTELIJN G.A., VAN DER VOORT M. & BIESTA-
887 PETERS E.G. (2018). Rapid detection and differentiation of Salmonella species, Salmonella Typhimurium and
888 Salmonella Enteritidis by multiplex quantitative PCR. PloS one, 13(10), p.e0206316.
889 INTERNATIONAL ORGANIZATION FOR STANDARDIZATION (2002). ISO 6579:2002. Microbiology of food and animal
890 feeding stuffs – Horizontal method for the detection of Salmonella spp., International Organization for
891 Standardization, Geneva, Switzerland.
892 INTERNATIONAL ORGANIZATION FOR STANDARDIZATION (2007). ISO 6579:2002/Amd 1:2007 (Annex D). Detection of
893 Salmonella spp. in animal faeces and in samples of the primary production stage – Horizontal method for the
894 detection of Salmonella spp., International Organization for Standardization, Geneva, Switzerland.
895 INTERNATIONAL ORGANIZATION FOR STANDARDIZATION (2012). ISO/TS 6579-2:2012. Microbiology of food and
896 animal feed – Horizontal method for the detection, enumeration and serotyping of Salmonella – Part 2:
897 Enumeration by a miniaturized most probable number technique, International Organization for Standardization,
898 Geneva, Switzerland.
899 INTERNATIONAL ORGANIZATION FOR STANDARDIZATION (2014). ISO/TR 6579-3:2014. Microbiology of the food chain
900 –- Horizontal method for the detection, enumeration and serotyping of Salmonella – Part 3: Guidelines for
901 serotyping of Salmonella spp., International Organization for Standardization, Geneva, Switzerland.
902 INTERNATIONAL ORGANIZATION FOR STANDARDIZATION (2017). ISO 6579-1:2017. Microbiology of food and animal
903 feed – Horizontal method for the detection, enumeration and serotyping of Salmonella – Part 1: Detection of
904 Salmonella spp. International Organization for Standardization, Geneva, Switzerland. Amended 2020.
905 ISSENHUTH-JEANJEAN S., ROGGENTIN P., MIKOLEIT M., GUIBOURDENCHE M., DE PINNA E., NAIR S., FIELDS P.I. &
906 WEILL F. X. (2014). Supplement 2008–2010 (no. 48) to the White–Kauffmann–Le Minor scheme. Res. Microbiol.,
907 165, 526–530.
41 18 OIE Terrestrial Manual 2022
42 Chapter 3.10.7. – Salmonellosis
908 JAJERE S.M. (2019). A review of Salmonella enterica with particular focus on the pathogenicity and virulence
909 factors, host specificity and antimicrobial resistance including multidrug resistance. Vet. World, 12, 504.
910 JENSEN A.N., NIELSEN L.R. & BAGGESEN D.L. (2013). Use of real-time PCR on fecal samples for detection of sub-
911 clinical Salmonella infection in cattle did not improve the detection sensitivity compared to conventional
912 bacteriology. Vet. Microbiol., 163, 373–377.
913 JENSEN M.B.F., SCHJØRRING S., BJÖRKMAN J.T., TORPDAHL M., LITRUP E., NIELSEN E.M. & NISKANEN, T. (2017).
914 External quality assessment for molecular typing of Salmonella 2013–2015: performance of the European
915 national public health reference laboratories. Euro. J. Clin. Microbiol. Infect. Dis., 36, 1923–1932.
916 KANKI M., SAKATA J., TAGUCHI M., KUMEDA Y., ISHIBASHI M., KAWAI T., KAWATSU K., YAMASAKI W., INOUE K. &
917 MIYAHARA M. (2009). Effect of sample preparation and bacterial concentration on Salmonella enterica detection in
918 poultry meat using culture methods and PCR assaying of pre-enrichment broths. Food Microbiol., 26, 1–3.
919 KRASCSENISCOVÁ K., PIKNOVÁ L., KACLIKOVÁ E. & KUCHTA T. (2008). Detection of Salmonella enterica in food
920 using two-step enrichment and real-time polymerase chain reaction. Lett. Microbiol., 46, 483–487.
921 LEE K.M., RUNYON M., HERRMAN T.J., PHILLIPS R. & HSIEH J. (2015). Review of Salmonella detection and
922 identification methods: Aspects of rapid emergency response and food safety. Food Control, 47, 264–276.
923 MALORNY B. & HOORFAR J. (2005). Toward standardization of diagnostic PCR testing of fecal samples: lessons
924 from the detection of salmonellae in pigs. J. Clin. Microbiol., 43, 3033–3037.
925 MALORNY B., PACCASSONI E., FACH P., BUNGE C., MARTIN A. & HELMUTH R. (2004). Diagnostic real-time PCR for
926 detection of Salmonella in food. Appl. Environ. Microbiol., 70, 7046–7052.
927 MASTROENI P., CHABALGOITY J.A., DUNSTAN S.J., MASKELL D.J. & DOUGAN G. (2001). Salmonella: Immune
928 responses and vaccines. Vet. J., 161, 132–164.
929 MAURISCHAT S., BAUMANN B., MARTIN A. & MALORNY B. (2015a). Rapid detection and specific differentiation of
930 Salmonella enterica subsp. enterica Enteritidis, Typhimurium and its monophasic variant 4,[5],12:i:- by real-time
931 multiplex PCR. Int. J. Food Microbiol., 193, 8–14.
932 MAURISCHAT S., SZABO I., BAUMANN B. & MALORNY B. (2015b). Rapid real-time PCR methods to distinguish
933 Salmonella Enteritidis wildtype field isolates from vaccine strains Salmovac SE/Gallivac SE and AviPro
934 Salmonella Vac E. J. Microbiol. Methods, 112, 92–98.
935 MUNCK N., NJAGE P.M.K., LEEKITCHAROENPHON P., LITRUP E. & HALD T. (2020). Application of Whole‐Genome
936 Sequences and Machine Learning in Source Attribution of Salmonella Typhimurium. Risk Analysis, 40, 1693–
937 1705.
938 NIELSEN B., EKEROTH L., BAGER F. & LIND P. (1998). Use of muscle fluid as a source of antibodies for serologic
939 detection of Salmonella infection in slaughter pig herds. J. Vet. Diagn Invest., 10, 158–163.
940 OLIVEIRA S.D., RODENBUSCH M.C. CE, ROCHA S.L.S. & CANAL C.W. (2003). Evaluation of selective and non-
941 selective enrichment PCR procedures for Salmonella detection. Lett. Appl. Microbiol., 36, 217–221.
942 PARK S.H., AYDIN M., KHATIWARA A., DOLAN M.C., GILMORE D.F., BOULDIN J.L., AHN S. & RICKE S.C. (2014).
943 Current and emerging technologies for rapid detection and characterization of Salmonella in poultry and poultry
944 products. Food Microbiol., 38, 250–262.
945 PARK S.H., JARQUIN R., HANNING I., ALMEIDA G. & RICKE S.C. (2011). Detection of Salmonella spp. survival and
946 virulence in poultry feed by targeting the hilA gene. J. Appl. Microbiol., 111, 426–432.
947 PIKNOVA L., KACLIKOVA E., PANGALLO D., POLEK B. & KUCHTA T. (2005). Quantification of Salmonella by 5’-
948 nuclease real-time polymerase chain reaction targeted to fimC gene. Curr. Microbiol., 50, 38–42.
949 PORWOLLIK S., BOYD E.F., CHOY C., CHENG P., FLOREA L., PROCTOR E. & MCCLELLAND M. (2004).
950 Characterization of Salmonella enterica subspecies I genovars by use of microarrays. J. Bacteriol., 186, 5883–
951 5898.
952 RASOOLY A. & HEROLD K.E. (2008). Food microbial pathogen detection and analysis using DNA microarray
953 technologies. Foodborne Pathog. Dis., 5, 531–550.
43 OIE Terrestrial Manual 2022 19
44 Chapter 3.10.7. – Salmonellosis
954 REISSBRODT R. (1995). Conventional and alternative methods for isolation and identification of Salmonella – an
955 overview. Biotest Bull., 5, 143–156.
956 REDWEIK G.A., JOCHUM J. & MELLATA M. (2020). Live Bacterial Prophylactics in Modern Poultry. Front. Vet. Sci., 7,
957 826.
958 TANG Y., DAVIES R. & PETROVSKA-HOLMES L. (2019). Identification of Genetic Features for Attenuation of Two
959 Salmonella Enteritidis Vaccine Strains and Differentiation of These From Wildtype Isolates Using Whole Genome
960 Sequencing. Front. Vet. Sci., 6, 447.
961 THOMSON N.R., CLAYTON D.J., WINDHORST D., VERNIKOS G., DAVIDSON S., CHURCHER C., QUAIL M.A., STEVENS M.,
962 JONES M.A., WATSON M., BARRON A., LAYTON A., PICKARD D., KINGSLEY R.A., BIGNELL A., CLARK L., HARRIS B.,
963 ORMOND D., ABDELLAH Z., BROOKS K., CHEREVACH I., CHILLINGWORTH T., WOODWARD J., NORBERCZAK H., LORD A.,
964 ARROWSMITH C., JAGELS K., MOULE S., MUNGALL K., SANDERS M., WHITEHEAD S., CHABALGOITY J.A., MASKELL D.,
965 HUMPHREY T., ROBERTS M., BARROW P.A., DOUGAN G. & PARKHILL J. (2008). Comparative genome analysis of
966 Salmonella enteritidis Pt4 and Salmonella Gallinarum 287/91 provides insights into evolutionary and host
967 adaptation pathways. Genome Res., 18, 1624–1637.
968 VAN DER HEIJDEN H.M.J.F. (2001). First international ring trial of ELISAs for Salmonella-antibody detection in
969 swine. Berl. Munch. Tierarztl., 114, 389–392. PMID: 11570186.
970 VAN IMMERSEEL F., STUDHOLME D.J., EECKHAUT V., HEYNDRICKX M., DEWULF J., DEWAELE I., VAN HOOREBEKE S.,
971 VAN MEIRHAEGHE H., DUCATELLE R., PASZKEIWICZ K. & TITBALL R.W. (2013). Salmonella Gallinarum field isolates
972 from laying hens are related to the vaccine strain SG9R. Vaccine, 31, 4940–4945.
973 VOOGT N., RAES M., WANNET W.J.B., HENKEN N.M. & VAN DE GIESSEN A.W. (2001). Comparison of selective
974 enrichment media for the detection of Salmonella in poultry faeces. Lett. Appl. Microbiol., 32, 89–92.
975 WANG W., LIU L., SONG S., TANG L., KUANG H. & XU C. (2015). A highly sensitive ELISA and immune-
976 chromatographic strip for the detection of Salmonella typhimurium in milk samples. Sensors, 15, 5281–5292.
977 WANG J., LI Y., CHEN J., HUA D., DENG H., LI Y., LIANG Z. & HUANG J. (2018). Rapid detection of food-borne
978 Salmonella contamination using IMBs-qPCR method based on pagC gene. Braz. J. Microbiol., 49, 320–328.
979 WESTPHAL O. & LUDERITZ O. (1954). Chemische Erforschung von Lipopolysacchariden gramnegativer Bakterien.
980 Angew. Chem., 66, 407–417.
981 WORLD HEALTH ORGANIZATION (WHO) (1994). Guidelines on Detection and Monitoring of Salmonella Infected
982 Poultry Flocks with Particular Reference to Salmonella enteritidis. Wray C. & Davies R.H., eds. WHO, Geneva,
983 Switzerland, ZOON/94.173.
984 YANG Q., DOMESLE K.J. & GE B. (2018). Loop-mediated isothermal amplification for Salmonella detection in food
985 and feed: current applications and future directions. Foodborne Pathog. Dis., 15, 309–331.
986 ZHANG J., KHAN S. & CHOUSALKAR K.K. (2020). Development of PMAxxTM-Based qPCR for the Quantification of
987 Viable and Non-viable Load of Salmonella from Poultry Environment. Front. Microbiol., 11.
988 doi:10.3389/fmicb.2020.581201.
989 *
990 * *
991 NB: There are OIE Reference Laboratories for Salmonellosis
992 (see Table in Part 4 of this Terrestrial Manual or consult the OIE Web site for the most up-to-date list:
993 https://www.oie.int/en/what-we-offer/expertise-network/reference-laboratories/#ui-id-3 ).
994 Please contact the OIE Reference Laboratories for any further information on
995 diagnostic tests, reagents and vaccines for Salmonellosis
996 NB: FIRST ADOPTED IN 1991 AS SALMONELLOSIS (S. ABORTUS OVIS AND S. EQUI) AND SALMONELLOSIS (S.
997 TYPHIMURIUM AND S. ENTERITIDIS); MOST RECENT UPDATES ADOPTED IN 2016.
45 20 OIE Terrestrial Manual 2022
You might also like
- Salmonellosis : NB: Version Adopted by The World Assembly of Delegates of The OIE in May 2010Document19 pagesSalmonellosis : NB: Version Adopted by The World Assembly of Delegates of The OIE in May 2010frankyNo ratings yet
- 1 See The Note in Chapter 2.9.8 Salmonellosis For The Principles Followed Concerning The Nomenclature of SalmonellaDocument17 pages1 See The Note in Chapter 2.9.8 Salmonellosis For The Principles Followed Concerning The Nomenclature of SalmonellaWira RamayadiNo ratings yet
- 07 For Shell 541554Document14 pages07 For Shell 541554frankyNo ratings yet
- II Bacterial DiseasesDocument51 pagesII Bacterial DiseasesSagar AcharyaNo ratings yet
- Rabies FinalDocument5 pagesRabies FinalGINNO OSMILLONo ratings yet
- 2.03.11 Fowl TyphoidDocument11 pages2.03.11 Fowl TyphoidYoni DarmawanNo ratings yet
- Unesco - Eolss Sample Chapters: Veterinary BacteriologyDocument6 pagesUnesco - Eolss Sample Chapters: Veterinary BacteriologyGaluh EnggarNo ratings yet
- FMD Oie 2012Document29 pagesFMD Oie 2012dilipreddygNo ratings yet
- Crimean-Congo Haemorrhagic Fever: CHAPTER 2.1.3BDocument8 pagesCrimean-Congo Haemorrhagic Fever: CHAPTER 2.1.3BWormInchNo ratings yet
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 82 Cryptosporidiosis and CyclosporiasisDocument16 pagesInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 82 Cryptosporidiosis and CyclosporiasissoledadDC329No ratings yet
- Uma Revisão Sobre Leptospitose BovinaDocument9 pagesUma Revisão Sobre Leptospitose BovinaDiovana MachadoNo ratings yet
- SalmonellosisDocument40 pagesSalmonellosispurposef49No ratings yet
- BIO2107 - Tutorial 5 Discussion PointsDocument4 pagesBIO2107 - Tutorial 5 Discussion PointsAjay Sookraj RamgolamNo ratings yet
- 63 - 18 05 Isolation of Salm 220610Document17 pages63 - 18 05 Isolation of Salm 220610demasvebryNo ratings yet
- Salmonellosis 1Document15 pagesSalmonellosis 1BforbatNo ratings yet
- 2.03.11 Fowl TyphoidDocument14 pages2.03.11 Fowl TyphoidSaruediNo ratings yet
- HGJK J LHB, JKDocument4 pagesHGJK J LHB, JKChandra Noor RachmanNo ratings yet
- Rudolph PediatricDocument9 pagesRudolph PediatricMuhammad RezaNo ratings yet
- 2.03.14 Newcastle DisDocument20 pages2.03.14 Newcastle DisErman Satya NugrahaNo ratings yet
- Typhoid FeverDocument13 pagesTyphoid FeverPutri Nilam SariNo ratings yet
- Salmonella, The Host and Disease: A Brief ReviewDocument8 pagesSalmonella, The Host and Disease: A Brief ReviewPedro Albán MNo ratings yet
- Rift Valley Fever: C H A P T E R 2 - 1 - 1 4Document20 pagesRift Valley Fever: C H A P T E R 2 - 1 - 1 4WormInchNo ratings yet
- Reoviridae Birnaviridae: General and Systemic Virology (MICRO - 303)Document11 pagesReoviridae Birnaviridae: General and Systemic Virology (MICRO - 303)Muhammad Arslan UsmanNo ratings yet
- PRRS Guide Web Bulletin - OIEDocument7 pagesPRRS Guide Web Bulletin - OIESimone Rosa DidonéNo ratings yet
- Classical Swine Fever: (Hog Cholera)Document25 pagesClassical Swine Fever: (Hog Cholera)Vini Vidi ViciNo ratings yet
- Summary of The Lecture On Lesson 21Document8 pagesSummary of The Lecture On Lesson 21hari dharshanNo ratings yet
- 3.03.09 Fowl CholeraDocument15 pages3.03.09 Fowl CholeraRay HanNo ratings yet
- A Review of Bovine LeptospirosisDocument12 pagesA Review of Bovine LeptospirosisSteffanie M Clyricia NoachNo ratings yet
- 3.01.05 CCHFDocument9 pages3.01.05 CCHFEl GhazaliNo ratings yet
- Salmonellosisincluding Entericfever: Farah Naz Qamar,, Wajid Hussain,, Sonia QureshiDocument13 pagesSalmonellosisincluding Entericfever: Farah Naz Qamar,, Wajid Hussain,, Sonia QureshiAnak MuadzNo ratings yet
- Salmonella Typhi: ClassificationDocument4 pagesSalmonella Typhi: ClassificationMohammad Tahir KheridNo ratings yet
- EPIDEMIOLOGYDocument3 pagesEPIDEMIOLOGYEdgarNo ratings yet
- Shaho Taha Ali VibrioDocument8 pagesShaho Taha Ali VibrioDlzar AbubakrNo ratings yet
- Prrs Guide Web BulletinDocument7 pagesPrrs Guide Web BulletinJocelyn LunaNo ratings yet
- Viruses in ReptilesDocument12 pagesViruses in ReptilesKhoirina Nur FadhilahNo ratings yet
- L15 SalmonellaDocument19 pagesL15 SalmonellaMohammed RedhaNo ratings yet
- Systemic Gastrointestinal Infections A Clinical OverviewDocument5 pagesSystemic Gastrointestinal Infections A Clinical Overviewheizormayo2008No ratings yet
- Salmonella and ShigellaDocument5 pagesSalmonella and ShigellaRigobertoNo ratings yet
- SalmonelosisDocument10 pagesSalmonelosisCarlos EduardoNo ratings yet
- Infectious Diseases and Parasites of RatitesDocument29 pagesInfectious Diseases and Parasites of Ratitesali hendyNo ratings yet
- 375 FullDocument11 pages375 FullRenata YolandaNo ratings yet
- Pathogenesis of Ruminant Herpesvirus Infections: Monika Engels, Mathias AckermannDocument13 pagesPathogenesis of Ruminant Herpesvirus Infections: Monika Engels, Mathias AckermannRosafina SetyantariNo ratings yet
- Avian Chlamydiosis: Causes, Diagnosis and TreatmentDocument12 pagesAvian Chlamydiosis: Causes, Diagnosis and TreatmentBarnabas1No ratings yet
- OIE 2010 Chapter on Vesicular StomatitisDocument11 pagesOIE 2010 Chapter on Vesicular StomatitisWormInchNo ratings yet
- Pathogenic Cocci Classification and CharacteristicsDocument72 pagesPathogenic Cocci Classification and CharacteristicsManisanthosh KumarNo ratings yet
- Antimicrobial Susceptibility and Minimum Inhibitory Concentration of Salmonella Enterica Isolates From Chickens in SomeDocument11 pagesAntimicrobial Susceptibility and Minimum Inhibitory Concentration of Salmonella Enterica Isolates From Chickens in SomeMonyet...No ratings yet
- Tugas Ilmu Penyakit ViralDocument4 pagesTugas Ilmu Penyakit ViralHelda AudyaNo ratings yet
- Jsimposium Tifoid FeverDocument4 pagesJsimposium Tifoid FeverWawan BwNo ratings yet
- FOOD INFECTIONDocument20 pagesFOOD INFECTIONtesnaNo ratings yet
- The Reoviridae Family: by Luka, Mela IluDocument49 pagesThe Reoviridae Family: by Luka, Mela IluMela LukaNo ratings yet
- Bluetongue: ImportanceDocument8 pagesBluetongue: ImportanceMona Rucita L. ANo ratings yet
- Topic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"Document26 pagesTopic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"deekshit dcNo ratings yet
- Salmon Ellos IsDocument5 pagesSalmon Ellos IsIsak ShatikaNo ratings yet
- A Review On: Salmonellosis and Its Economic and Public Health SignificanceDocument13 pagesA Review On: Salmonellosis and Its Economic and Public Health Significanceamanmalako50No ratings yet
- Prrs (Porcine Reproductive and Respiratory Syndrome) : GijaponDocument43 pagesPrrs (Porcine Reproductive and Respiratory Syndrome) : GijaponFrance GijaponNo ratings yet
- Vesicular StomatitisDocument5 pagesVesicular StomatitisSeby SebastianNo ratings yet
- 2.03.14 Newcastle DisDocument14 pages2.03.14 Newcastle DisdiparayogagalihNo ratings yet
- The Infection Game Supplement: new infections, retroviruses and pandemicsFrom EverandThe Infection Game Supplement: new infections, retroviruses and pandemicsNo ratings yet
- 911 Pigeon Disease & Treatment Protocols!From Everand911 Pigeon Disease & Treatment Protocols!Rating: 4 out of 5 stars4/5 (1)
- Remote Control Panel (RCP) User'S GuideDocument13 pagesRemote Control Panel (RCP) User'S GuideAdrian PuscasNo ratings yet
- Petol Ps 460-5G: Technical SheetDocument2 pagesPetol Ps 460-5G: Technical SheetA MahmoodNo ratings yet
- Art for Ages 1-3 Focuses on DevelopmentDocument3 pagesArt for Ages 1-3 Focuses on DevelopmentPresley AbrauNo ratings yet
- Managerial Economics L4 Consumer BehaviourDocument50 pagesManagerial Economics L4 Consumer BehaviourRifat al haque DhruboNo ratings yet
- The Historical Foundations of Law. Harold BermanDocument13 pagesThe Historical Foundations of Law. Harold BermanespinasdorsalesNo ratings yet
- ADWEA Approved Vendor List - 18.4.2013Document297 pagesADWEA Approved Vendor List - 18.4.2013Anonymous kjvaeVJNNo ratings yet
- EnCORE V13.5 en EnglishDocument138 pagesEnCORE V13.5 en EnglishRommel SaavedraNo ratings yet
- Basic Electronic ComponentsDocument28 pagesBasic Electronic ComponentsJafar ShaikhNo ratings yet
- 5 Tips For Faster Mental Multiplication PDFDocument3 pages5 Tips For Faster Mental Multiplication PDFGonzalo Estrán BuyoNo ratings yet
- DownloadDocument2 pagesDownloadAmit KumarNo ratings yet
- Bee WareDocument49 pagesBee WareJayNo ratings yet
- Java syntax and data types tutorialDocument3 pagesJava syntax and data types tutorialpeter chan100% (1)
- Development PlanningDocument15 pagesDevelopment PlanningSamuelNo ratings yet
- White Paper Leadership To Boost Your Organisations Energy and PerformanceDocument12 pagesWhite Paper Leadership To Boost Your Organisations Energy and PerformanceMorie JinyoungNo ratings yet
- ORPHEUS by GRS Mead - Electronic Text EditionDocument199 pagesORPHEUS by GRS Mead - Electronic Text EditionMartin EuserNo ratings yet
- Carbon Emission and Battery Monitoring SystemDocument17 pagesCarbon Emission and Battery Monitoring SystemIJRASETPublicationsNo ratings yet
- Challenges Faced by Irregular StudentsDocument13 pagesChallenges Faced by Irregular StudentsTicag Teo80% (5)
- Ethylene Yield From Pyrolysis Cracking in Olefin PDocument6 pagesEthylene Yield From Pyrolysis Cracking in Olefin PALL2WINNo ratings yet
- String inverter comparisonDocument4 pagesString inverter comparisonRakesh HateyNo ratings yet
- Pizza Hut Final!Document15 pagesPizza Hut Final!Alisha ParabNo ratings yet
- SCMHRD SM-1Document43 pagesSCMHRD SM-1ShivanirahejaNo ratings yet
- Supply Chain Management On The Crossraod To Sustainability: Logistics Research June 2009Document13 pagesSupply Chain Management On The Crossraod To Sustainability: Logistics Research June 2009AKSHAT GHATIANo ratings yet
- Neolithic Farming Villages Jericho and Catal HuyukDocument1 pageNeolithic Farming Villages Jericho and Catal HuyukPream BoleoNo ratings yet
- Titan InvoiceDocument1 pageTitan Invoiceiamdhanush017No ratings yet
- Why War: Einstein and Freud's Little-Known Correspondence On Violence, Peace, and Human Nature by Maria PopovaDocument24 pagesWhy War: Einstein and Freud's Little-Known Correspondence On Violence, Peace, and Human Nature by Maria PopovaVagueBlurNo ratings yet
- SD Series Digital AC Servo System User Manual GuideDocument66 pagesSD Series Digital AC Servo System User Manual GuideAdnene SaanounNo ratings yet
- Agile Spotify - Team - HomeworkDocument8 pagesAgile Spotify - Team - Homeworksp76rjm7dhNo ratings yet
- Gigabyte 8simlh - Rev 3.02Document32 pagesGigabyte 8simlh - Rev 3.02Denis MartinsNo ratings yet
- DP-10/DP-10T/DP-11/DP-15/DP-18 Digital Ultrasonic Diagnostic Imaging SystemDocument213 pagesDP-10/DP-10T/DP-11/DP-15/DP-18 Digital Ultrasonic Diagnostic Imaging SystemDaniel JuarezNo ratings yet
- Foundations On Expansive Soils: 3.1. BackgroundDocument31 pagesFoundations On Expansive Soils: 3.1. BackgroundbiniNo ratings yet