Professional Documents
Culture Documents
Baldwin Tub Ulo Interstitial
Uploaded by
drryanalwyn0 ratings0% found this document useful (0 votes)
6 views36 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views36 pagesBaldwin Tub Ulo Interstitial
Uploaded by
drryanalwynCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 36
Tubulointerstitial Diseases
Mark D. Baldwin D.O., FACOI, FASN
Professor and Chair Department of Internal Medicine
Pacific Northwest University
Yakima, Washington
ACOI Internal Medicine Board Review 2019
Disclosures
• None, just working for The Man
Case
• A 49 y.o. WF presents for follow up on a new patient visit. She has a
hx of HTN for which she takes valsartan 160 mg daily and GERD for
which she takes omeprazole 20 mg. BID. She is a non smoker and
drinks rarely.
• Her exam is unremarkable BP 132/82 and mild obesity was noted.
• LAB: Na 133, K 3.4, Cl 100, bicarb 21, BUN 33, creatinine 2.9, glucose,
LFTs, CBC, lipids were WNL
• UA SG 1.014, +leukocyte esterase, no blood, protein or nitrite, micro
4-10 WBCs, 02 RBCs no bacteria and C&S neg.
Features of Tubulointerstitial Disease
1. Proteinuria- usually less than 1 Gm/da
2. Anemia-due to low level of Erythropoietin
3. Acidosis-RTA’s are common
4. Hypertension-common
5. Urinalysis-WBC’s and WBC casts seen
6. Electrolyte Abnormalities-Na and K
Many of the above features are seen at relatively mild elevations of
Serum Creatinine
Features of Glomerular Disease
1. Proteinuria->3 Gm/da
2. Anemia-uncommon until late
3. Acidosis-uncommon until late
4. Hypertension-may occur at any time
5. Urinalysis-may see Oval Fat Bodies
6. Electrolytes-May see low Na
Unlike Tubulointerstitial Disease, many of these feature do not occur
until late in the course of the underlying disease.
Types of Tubulointerstitial Disease
1. Acute Interstitial Nephritis
2. Chronic Interstitial Nephritis
3. Acute Tubular Necrosis
4. Renal Tubular Acidosis
5. Multiple Myeloma
Chronic Interstitial Nephritis (CIN)
• A chronic condition involving fibrosis of the interstitium and tubular
destruction
• Chronic low grade inflammation leads to tubular injury and fibrosis
• Macroscopically normal kidneys
• The final common pathway of most chronic renal diseases
Causes of Chronic Interstitial Nephritis
• Mechanical: ureteral reflux, obstruction, stones, infection, neurogenic
bladder, medullary cystic disease, Alport’s
• Drugs: NSAIDs, Lithium, PPI’s, cyclosporine, tacrolimus, indinavir, cisplatin
• Heavy Metals: Hg, Pb, Cd, arsenic, gold, uranium, too much Ozzy
• Metabolic: hyperuricemia, hypercalcemia, hypokalemia, hyperoxaluria,
cytinosis
• Radiation
• Immune mediated: ANCA, SLA, Sjorgren's, sarcoid
• Vascular: atherosclerotic renal disease
• Heme/Onc: myeloma, amyloid, lymphoma, sickle cell, PNH
• Late glomerular disease
• Aristolochic acid: Balkan nephropathy, Chinese herb nephropathy
Aristolochic acid
• Acute exposure: Chinese herb nephropathy-AKI, rapid decline in renal
function
• Chronic exposure: Balkan endemic nephropathy-CIN/CKD slow
decline over years from chronic exposure
Debelle Kidney Int 2008;74: 158-169
Aristolochic acid Nephrotoxicity
Debelle Kidney Int 2008;74: 158-169
Clinical Features of CIN
• Usually Asymptomatic
• STERILE PYURIA-The Hallmark of CIN
• Anemia
• Acidosis-Renal Tubular Acidosis
• Hypo or hyperkalemia
• Minimal Proteinuria
• Hypertension
Chronic Interstitial Nephritis
Chronic Interstitial Nephritis
Treatment of CIN
• Do NOT give antibiotics for pyuria unless there is bacteria present-this
is a chronic inflammatory condition, NOT an infection
• BP control-The MOST important treatment
• ACE-I or ARBs-The drugs of choice
• Anemia control
• Acidosis control
• Phosphorus control
Renal Tubular Acidosis (RTA)
• Distal Type I RTA -associated with Chronic Urinary Tract Obstruction,
Bicarb<15*NAG, hypokalemia, urine pH>5.5
• Proximal Type II RTA -associated with Fanconi’s Syndrome Bicarb 15-21*NAG,
hypokalemia, urine pH>5.5
• Distal Type IV RTA- Most common RTA, Seen w/ DM and CKD, NAG, Hyperkalemia
urine pH<5.5
• All RTA have +UAG
* Point of differentiation, NAG non anion gap acidosis
Myeloma and the Kidney
• 10% of all hematological malignancies
• Plasma cell clone of Immunoglobulins usually IgG
• Renal, Cardiac and Liver are the most common organs involved
• Renal impairment-acute or chronic- is commonly seen ~50% of cases
with severe involvement in 15-20% of cases
• Proteinuria-globulin or albuminuria is seen in >80% of cases
• Myeloma can involve the vascular, glomerular or tubular/interstitial
segments of the kidney
• Frequent cause of mortality and morbidity
Pathophysiology
• Plasma cell clones leading to IgG light chains, heavy chains can be
seen
• Can see clonal IgA, D, M or E variants of myeloma
• Light chain or fragments deposited in a tissues
• Kappa or lambda light chains
• Amyloid (AL) can be deposited
• Tubular obstruction
• Tubular dysfunction- Fanconi’s Syndrome & Proximal Type 2 RTA
• AKI of multiple etiologies
Renal Effects
• Glomerular: Amyloid light chain (AL) or heavy chain (AH) amyloidosis, Light Chain
Deposition Disease (LCDD) or Heavy Chain Deposition Disease (HCDD) plasma cell
infiltration
• Tubular: Cast nephropathy “Myeloma kidney”, tubular dysfunction,
hypercalcemia, hyperuricemia, contrast induced AKI
• Interstitial: Plasma cell infiltration, pyelonephritis
Amyloid MM v LCDD
• Amyloid myeloma (AL):
• lambda>kappa, +congo red, +fibrils on EM
• Light chain deposition disease(LCDD): kappa>lambda, -congo red, -
fibrils on EM
Cast Nephropathy
• Most common cause of renal failure in myeloma
• Globulin light chains are filtered at the glomerulus
• Can exceed 10-20 grams/day and are toxic to the tubular cells,
negative dipstick d/t globulins not albumin
• Light chain are partially reabsorbed damaging to proximal tubular
cells and delivered distally, combing with Tamm-Horsfell protein
produced in the thick ascending limb occluding the tubule
• Obstructing casts lead to inflammation, fibrosis and tubular rupture
Presentation
• >50 years old
• Males>females
• African Americans >other groups
• Long history of back pain or “arthritic” pain
• Pathological fractures
• Fatigue
• Anemia
• Infection
• Renal failure
Multiple Myeloma Laboratory Findings
• Elevated BUN and Creatinine
• Hypercalcemia
• Hyperuricemia
• Normocytic Normochromic Anemia, Rouleaux formation
• Serum Protein Electrophoresis/ Urine Protein Electectrophoresis
positive for elevations in the Gamma fraction-M spike
• Low Anion Gap
• Urinalysis may show NO Protein, unless Sulfa salicylic Acid test is
done, which will be positive.
Serology
• Serum protein electrophoresis/urine protein electrophoresis
• Free light chain assay
• Immunofixation: quantifies IgA, IgD, IgE, IgM, IgG
• Cytogenic analysis: karyotyping
• Flow cytometry
Congo Red “Apple green birefringence”
Renal Myeloma
Glomerular Amyloid Cast Nephropathy
Amyloid Fibrils EM
Radiographs
Treatment of Myeloma Renal Disease
• Assure hydration status with alkalization of the urine but avoid fluid
overload
• Allopurinol
• Bortezomib-dexamethasone-cyclophosphamide or
• Bortezomib-thalidomide-dexamethasone can decrease light chain
production and may improve cast nephropathy
• Dialysis if needed (poor outcomes)
• ?role of plasmapheresis
Hypercalcemia of Malignancy
• Malignancy: Thyroid, lung, breast, Mechanisms:
renal cell, prostate, myeloma, 1. Direct bone invasion/osteolysis
leukemias/lymphomas, Tumor lysis
syndrome 2. Elevated PTHrP
• Very poor prognostic sign 3. Humoral hypercalcemia of
malignancy: production of
• Always (or almost always) presents cytokines/osteoclast activating
with dehydration factors-releasing Ca++ from bone
4. Excess Calcitriol-like factors
(increased GI absorption)
granulomatous diseases (Sarcoid, TB)
Presentation
• Decreased cognition, fatigue
• Anorexia, N,V, constipation
• Abdominal and bone pain
• Pancreatitis
• Short QT, ST changes pseudo MI pattern
• HTN
• AKI, Nephrogenic DI
N AM J Med Sci 2011;7(11): 483-493.
Hypercalcemia of Malignancy
Reagan P, AJKD 2014;63:141-147 Mundy G JASN 2008;19:672-675
Treatment of Hypercalcemia of Malignancy
1. Aggressive IV Normal saline: 4. Bisphosphonates (if renal
a. Restores BP, perfusion function is normal and
phosphorus is not elevated)
b. Increased Na/water delivery to
the kidney decreases 5. Steroids
reabsorption of Na and Ca++ 6. Denosumab
2. Once hydrated: Loop diuretic
(reduces Ca uptake in the TAL) do
NOT use Thiazides!!!!! WHY?
3. Calcitonin
Treatment of Hypercalcemia of Malignancy
Intervention Onset Duration
Normal saline 2-4l/da Immediate 2-3 days
Calcitonin 4-8 U/kg SQ 6-12 hours 4-6 hours 2-3 days
Loop diuretic (once hydrated!) ~5-10 minutes 1-4 hours
Bisphosphonates 48 hours ~3 weeks
Corticosteroids 7 days ~7days
Denosumab 7-10 day 3 months
Sternlicht Ther Clin Risk Manag 2015; 11: 1779-1788
Tubulointerstitial Diseases-Conclusions
• Often overlooked as a cause of Chronic Renal Disease
• Look for Drug causes or Sepsis as a cause of Acute Renal
Failure (i.e. AIN or ATN)
• Tubulointerstitial Diseases frequently have electrolyte
abnormalities, acid-base disorders, and anemia as a common
feature.
You might also like
- Pedoman Tatalaksana Sindrom Koroner Akut 2015Document29 pagesPedoman Tatalaksana Sindrom Koroner Akut 2015Vittorio bagscenterNo ratings yet
- Surgical Diseases of Liver1Document54 pagesSurgical Diseases of Liver1DR MOHAMED HEALTH CHANNELNo ratings yet
- Tubules and Interstitium: Diseases of The KidneyDocument46 pagesTubules and Interstitium: Diseases of The Kidneyعوض الكريمNo ratings yet
- Chapter - 2 - C - II Liver CirrhosisDocument39 pagesChapter - 2 - C - II Liver CirrhosisEmmaNo ratings yet
- Tutorial Liver FailureDocument59 pagesTutorial Liver FailureNadhrah zulkifliNo ratings yet
- Prepared By: Dr. Abhishek Garg M.D Resident 3 Year Edited By: Dr. Arun Kumar SharmaDocument43 pagesPrepared By: Dr. Abhishek Garg M.D Resident 3 Year Edited By: Dr. Arun Kumar SharmaVijitha LenkalaNo ratings yet
- CKD by HalimaDocument23 pagesCKD by HalimaRahaf QaliifNo ratings yet
- t2 Kidney DiseaseDocument52 pagest2 Kidney Diseasewany.fyza54No ratings yet
- ANEMIA: CAUSES, SIGNS, AND MANAGEMENTDocument35 pagesANEMIA: CAUSES, SIGNS, AND MANAGEMENTapule geraldhumbleNo ratings yet
- Clinical Case On JaundiceDocument43 pagesClinical Case On JaundicePro fatherNo ratings yet
- Renal Failure-Clinical CaseDocument35 pagesRenal Failure-Clinical Caseyaser773arfat2025No ratings yet
- A Case of Liver Cirrhosis & Hepatic EncephalopathyDocument21 pagesA Case of Liver Cirrhosis & Hepatic EncephalopathyUdayakumar MannangattiNo ratings yet
- GI Quiz 1 NotesDocument8 pagesGI Quiz 1 NotesSara JosephNo ratings yet
- Final GIT Case PresentationDocument53 pagesFinal GIT Case PresentationRovan100% (1)
- Interstitial NephritisDocument21 pagesInterstitial NephritisAhmed RaadNo ratings yet
- Morning Report 9/5/18: Adam Cardullo, MD Pgy - 2Document22 pagesMorning Report 9/5/18: Adam Cardullo, MD Pgy - 2Emily EresumaNo ratings yet
- Renal Failure March 2020Document46 pagesRenal Failure March 2020dicksonsamboNo ratings yet
- Acute Kidney Injury: Erika Phillie T. Chua Internal Medicine ResidentDocument48 pagesAcute Kidney Injury: Erika Phillie T. Chua Internal Medicine ResidenterikaNo ratings yet
- HematuriaDocument42 pagesHematuriaAhmad SobihNo ratings yet
- Kidney Emergency: M. Syamsul BakhriDocument30 pagesKidney Emergency: M. Syamsul BakhrierahadeNo ratings yet
- Approach Nefroritic SXDocument58 pagesApproach Nefroritic SX[ qιlα ]No ratings yet
- Chronic Renal FailureDocument14 pagesChronic Renal FailureyazzzNo ratings yet
- Renal Faliure 1Document50 pagesRenal Faliure 1180045No ratings yet
- Renal Failure PresentationDocument110 pagesRenal Failure PresentationMusa yohana100% (1)
- Acute Renal Failure: DR Grania PriceDocument24 pagesAcute Renal Failure: DR Grania PriceCastro KisuuleNo ratings yet
- Fulminant Hepatic FailureDocument50 pagesFulminant Hepatic FailureSangeeta BSRNo ratings yet
- Jaundice MasterDocument76 pagesJaundice MasterVinoth KumarNo ratings yet
- MS HemaDocument6 pagesMS HemaFrechel Ann Landingin PedrozoNo ratings yet
- Acute Kidney Injury: Dana BabaDocument31 pagesAcute Kidney Injury: Dana Babanaheel98shNo ratings yet
- L25 CLD-2Document55 pagesL25 CLD-2S sNo ratings yet
- 22.AKI ProtocolDocument2 pages22.AKI ProtocolRed DevilNo ratings yet
- CLD FinalDocument17 pagesCLD FinalHervis FantiniNo ratings yet
- Urinary System and Male Genital: Fajar L. Gultom Departemen Patologi Anatomik FK UKI December 2017Document50 pagesUrinary System and Male Genital: Fajar L. Gultom Departemen Patologi Anatomik FK UKI December 2017Sona SiburianNo ratings yet
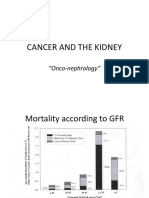
- Cancer and The KidneyDocument29 pagesCancer and The Kidney[ qιlα ]No ratings yet
- Everything You Need to Know About AnemiaDocument50 pagesEverything You Need to Know About Anemia余明謙No ratings yet
- Acute Renal Failure: Anthony R Mato, MDDocument81 pagesAcute Renal Failure: Anthony R Mato, MDasad_channa1No ratings yet
- GIT Cirrhosis Liver in ChildrenDocument37 pagesGIT Cirrhosis Liver in ChildrenDr.P.NatarajanNo ratings yet
- Nephrology: Omar K MRCP IrelandDocument54 pagesNephrology: Omar K MRCP IrelandManmeet SNo ratings yet
- Adult Health Nursing Phase I Thursday 6:00-9:00 PM: Irritable Bowel SyndromeDocument18 pagesAdult Health Nursing Phase I Thursday 6:00-9:00 PM: Irritable Bowel SyndromeLavinia Malazarte CaballeroNo ratings yet
- Dr.P.santhosh Kumar Post GraduateDocument22 pagesDr.P.santhosh Kumar Post GraduateSrilakshmi SathiyaNo ratings yet
- Acute PancreatitisDocument40 pagesAcute PancreatitisMustafa HusainNo ratings yet
- New Psychiatry FAE2016Document120 pagesNew Psychiatry FAE2016omarNo ratings yet
- Kidney Diseases in Children s1Document25 pagesKidney Diseases in Children s1q9tt4ftcxnNo ratings yet
- Chronic Liver Diseases ExplainedDocument49 pagesChronic Liver Diseases ExplainedmogreyNo ratings yet
- Neonatal Renal DiseaseDocument38 pagesNeonatal Renal Diseasesaieefzaman71No ratings yet
- Renal FailureDocument31 pagesRenal Failureapi-195799092No ratings yet
- Liver Cirrhosis: DR Alex MogereDocument51 pagesLiver Cirrhosis: DR Alex MogereGladys Maina100% (1)
- Chronic Kidney InjuryDocument13 pagesChronic Kidney InjuryMaryam MohamedaliNo ratings yet
- MISDC AnaemiaDocument33 pagesMISDC AnaemiawanyNo ratings yet
- Acute Kidney InjuryDocument34 pagesAcute Kidney Injury* mokhtar !!No ratings yet
- Pheo Esrd and NeonateDocument45 pagesPheo Esrd and NeonateLea TanNo ratings yet
- Chronic Kidney DiseaseDocument7 pagesChronic Kidney DiseaseLardel Balbiran LafortezaNo ratings yet
- Renal EmergenciesDocument93 pagesRenal EmergenciesShubham gaurNo ratings yet
- Emergency Medicine Block Seventh Problem: Group 15 Friday, November 3 2017Document94 pagesEmergency Medicine Block Seventh Problem: Group 15 Friday, November 3 2017Stefanie BlueNo ratings yet
- Refreshing renal failureDocument35 pagesRefreshing renal failureaditNo ratings yet
- Cirrhosis and Its Complications: Dr. P. Dienhart, M.D (Gastroenterology) DR - Padma Poddutoori (PGY3, I.M)Document21 pagesCirrhosis and Its Complications: Dr. P. Dienhart, M.D (Gastroenterology) DR - Padma Poddutoori (PGY3, I.M)Kartika FitriNo ratings yet
- 340 Final StudyDocument21 pages340 Final StudyLeah ElizabethNo ratings yet
- LiverDocument30 pagesLiverNisini ImanyaNo ratings yet
- Farmakoterapi Penyakit Gangguan GinjalDocument24 pagesFarmakoterapi Penyakit Gangguan GinjaltiaraNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Acute Interstitial Nephritis 2Document19 pagesAcute Interstitial Nephritis 2Paul SinsNo ratings yet
- Internal Medicine Orals E&a Academia (Exclusive)Document209 pagesInternal Medicine Orals E&a Academia (Exclusive)Shreya SinghNo ratings yet
- Cilostazol-Induced Acute Kidney Injury in A Patient WithDocument4 pagesCilostazol-Induced Acute Kidney Injury in A Patient WithjharyNo ratings yet
- Case 34-2020: A 74-Year-Old Man With Chronic Kidney Disease: Case Records Massachusetts General HospitalDocument11 pagesCase 34-2020: A 74-Year-Old Man With Chronic Kidney Disease: Case Records Massachusetts General HospitalTomi EscribanoNo ratings yet
- Morpho DopDocument31 pagesMorpho DopSiva Prasad YadavNo ratings yet
- Case Report of Acute and Chronic Interstitial NephritisDocument10 pagesCase Report of Acute and Chronic Interstitial NephritisDoncyNo ratings yet
- Acute Renal FailureDocument28 pagesAcute Renal FailureAs SyarifNo ratings yet
- Drug Induced NephrotoxicityDocument13 pagesDrug Induced NephrotoxicityAgnes BastonNo ratings yet
- 1 - AKI (Important Notes & MCQS)Document13 pages1 - AKI (Important Notes & MCQS)Queen LoleNo ratings yet
- IVMS Cell Biology and Pathology Flash Facts 2Document3,980 pagesIVMS Cell Biology and Pathology Flash Facts 2Marc Imhotep Cray, M.D.No ratings yet
- Aubf M5u1 (Highlighted)Document17 pagesAubf M5u1 (Highlighted)proximusNo ratings yet
- Paediatric Nephrology Syllabus FinalDocument13 pagesPaediatric Nephrology Syllabus FinalClever BarbieNo ratings yet
- Acute NephritisDocument32 pagesAcute NephritisKohinoorKohinoorNo ratings yet
- NephritisDocument21 pagesNephritisruchikaNo ratings yet
- PEDIATRIC NEPHRITIS: CAUSES AND MANAGEMENTDocument35 pagesPEDIATRIC NEPHRITIS: CAUSES AND MANAGEMENTLubinda SitaliNo ratings yet
- Interstitial NephritisDocument21 pagesInterstitial NephritisAhmed RaadNo ratings yet
- Understanding Lupus NephritisDocument21 pagesUnderstanding Lupus Nephritissaritha Oruganti100% (1)
- PPIs and Kidney DiseaseDocument6 pagesPPIs and Kidney DiseaseSonia jolandaNo ratings yet
- Oftal Case StudyDocument11 pagesOftal Case StudyMohamad RaisNo ratings yet
- L 7 NephroDocument6 pagesL 7 NephroAhmed Gh Al-zechrawiNo ratings yet
- Acute Interstitial NephritisDocument36 pagesAcute Interstitial NephritisosaqerNo ratings yet
- Human Physiology Final ProjectDocument37 pagesHuman Physiology Final ProjectAyesha MasoodNo ratings yet
- Approach To Renal BiopsyDocument77 pagesApproach To Renal BiopsySandeep Kumar VushikamallaNo ratings yet
- 2022 - Acute Kidney Injury and Critical Care NephrologyDocument123 pages2022 - Acute Kidney Injury and Critical Care NephrologyEdson MarquesNo ratings yet
- Tubulointerstitial Nephritis - 161269200418Document12 pagesTubulointerstitial Nephritis - 161269200418ተሣለነ ወልድNo ratings yet
- Semio Renal DiaposDocument143 pagesSemio Renal DiaposMaria jose Pesantez abadNo ratings yet
- Interstitial Nephritis: Inflammation of the Renal InterstitiumDocument2 pagesInterstitial Nephritis: Inflammation of the Renal InterstitiumYosi Dwi Saputro Part IINo ratings yet
- Tubulointerstitial nephritis: an overview of kidney diseases involving the tubules and interstitiumDocument34 pagesTubulointerstitial nephritis: an overview of kidney diseases involving the tubules and interstitiumIaros OlgaNo ratings yet
- Passmedicine MRCP Notes-NephrologyDocument73 pagesPassmedicine MRCP Notes-Nephrologysalwabeshir542No ratings yet
- Karen Brechbuhl's notes on acute kidney injury (AKI) diagnosis and classificationDocument11 pagesKaren Brechbuhl's notes on acute kidney injury (AKI) diagnosis and classificationKaren b.No ratings yet