Professional Documents
Culture Documents
07 (2022) Pediculosis Is A Risk Factor For Iron Deficiency Anaemia
07 (2022) Pediculosis Is A Risk Factor For Iron Deficiency Anaemia
Uploaded by
juliabatis04Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
07 (2022) Pediculosis Is A Risk Factor For Iron Deficiency Anaemia
07 (2022) Pediculosis Is A Risk Factor For Iron Deficiency Anaemia
Uploaded by
juliabatis04Copyright:
Available Formats
Open Access Case
Report DOI: 10.7759/cureus.22403
Pediculosis Is a Risk Factor for Iron Deficiency
Anaemia
Review began 01/27/2022
Hussain A. Al Ghadeer 1 , Fadi Busaleh 1 , Hassan M. Albahrani 1 , Alla M. Albisher 1 , Abdulaziz AlHassan 1 ,
Review ended 02/12/2022 Hassan M. AlAmer 1 , Hassan M. Alibrahim 1 , Ahmed H. Alherz 1 , Abdullah F. Al Muaibid 1 , Tawfiq M.
Published 02/20/2022 Aljubran 1
© Copyright 2022
Al Ghadeer et al. This is an open access 1. Pediatrics, Maternity and Children Hospital, Al-Ahsa, SAU
article distributed under the terms of the
Creative Commons Attribution License CC-
Corresponding author: Hussain A. Al Ghadeer, hu.alghadeer@gmail.com
BY 4.0., which permits unrestricted use,
distribution, and reproduction in any
medium, provided the original author and
source are credited.
Abstract
Pediculosis capitis is obligate ectoparasite that lives and feeds on host blood, affecting commonly children.
Lice are transmitted easily and respond to topical treatment with good personal hygiene. Chronic infestation
can lead to different complications such as bacterial infection dermatitis and anaemia. Haematological
complications are not reported frequently. We report a case series of five patients presented with a clear
manifestation of anaemia with heavy lice infestation. Laboratory evaluation revealed microcytic
hypochromic anaemia (red blood cell indices) with low serum iron levels and other causes that were
excluded. All patients who were admitted received blood transfusions. There was not a possible explanation
for this severe anaemia other than head lice.
Categories: Pediatrics, Infectious Disease, Hematology
Keywords: saudi arabia, alahsa, profound anaemia., iron deficiency anaemia, head lice, pediculosis capitis
Introduction
Pediculosis capitis, a common skin condition known as head lice, is considered a general public issue caused
by Pediculus humanus (Pediculus humanus capitis) infestation. It is contagious and transmitted
through direct contact (head-to-head) or indirect contact through sharing clothes, towels and other
personal items [1]. Although it is affecting all age groups but is frequently seen in the first decade of life [2].
The prevalence of pediculosis depends on several factors: socioeconomic, demographic, educational, and
hygiene [3]. Pediculus humanus is a holoparasite blood-feeding human ectoparasite that survives on its host
[4]. This results in a blood loss of 0.7 mL/day. Although a small amount of blood loss is insignificant in a
healthy child, chronic and heavy infestation causes significant blood loss that leads to anaemia [5].
No definitive relationship between iron deficiency anaemia and pediculosis has been found. Limited
literatures reported iron deficiency anaemia in patients with heavy and chronic infestation without apparent
cause of anaemia. This is the first case series in the paediatric age group that describes five siblings
presented with profound anaemia due to lice infestation.
Case Presentation
This case series describes five female siblings aged between 6-13 years presented on the same day to a
pediatric emergency department in Maternity and Children's Hospital, Al-Ahsa, Saudi Arabia. They live in an
area that is 300 km away from Al-Ahsa with poor socioeconomic status. All of them did not know to have any
significant medical or surgical illnesses and there was no family history of inherited, genetic or
haematological diseases.
They had a similar clinical presentation with a history of generalized fatigability and pallor for one month
(Table 1). It was associated with non-productive cough and pagophagia for four days and one of them had a
syncopal attack lasting for a few minutes. It was also associated with head lice infestation for two weeks and
subjective fever that responded to paracetamol. They denied any history of dyspnoea, syncope, dizziness,
headache, change in bowel habit (diarrhea, constipation, bleeding) or urine (dysuria, frequency, urgency,
proteinuria and hematuria). There was no history of ingestion of herbal or chemical medications. They had
no history of weight loss, anorexia or eating disorder. They were not known to have an allergy neither they
were on regular medication.
How to cite this article
Al Ghadeer H A, Busaleh F, Albahrani H M, et al. (February 20, 2022) Pediculosis Is a Risk Factor for Iron Deficiency Anaemia. Cureus 14(2):
e22403. DOI 10.7759/cureus.22403
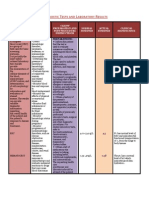
Patient A Patient B Patient C Patient D Patient E
Age (years) 6 8 12 12 13
Clinical features
Symptoms
Pallor + + + + +
Fatigability + + + + +
Dyspnoea + + + + +
Syncope - + - - -
Bleeding - - - - -
Menstrual cycle - - - - +++
Headache - - + - +
Dizziness - - + - +
Pagophagia + + + + +
Palpitation + + + + +
Chest pain - - - - -
Weight loss - - - - -
Sings
Pallor + + + + +
Jaundice + + + + +
Tachypnoea + + + + +
Tachycardia + + + + +
Hypotension - - - - -
Active bleeding (from the scalp) + + + + +
Change in urine colour - - - - -
Hematemesis - - - - -
Organomegaly - - - - -
TABLE 1: The clinical presentation of the patients
On examination, they looked ill, pale with dark spots distributed all over the body (blood on crust). Notable
head lice infestation with copious nits on the scalp, which was associated with scratch marks with injured
scalp, was identified. Their vital signs revealed tachycardia and tachypnoea, others were within the normal
level. Systemic examination was unremarkable. There was no lice infestation on the rest of the body and
pubis other than the head.
Laboratory tests revealed that all of them had a similar finding of microcytic hypochromic anaemia with
mild anisocytosis (Table 2). The iron profile showed a low iron level which confirmed the diagnosis of iron
deficiency anaemia. The stool culture test for occult blood and ova was negative. The biochemical and
coagulation profile was normal. The test was negative for Heinz body, hemoglobin (Hb) H disease.
Patient Patient Patient Patient Patient
Laboratory tests
A B C D E
Complete Blood Count (CBC) Reference level
2022 Al Ghadeer et al. Cureus 14(2): e22403. DOI 10.7759/cureus.22403 2 of 5
Haemoglobin 3 3.8 5.6 4.2 2.9 11.5-13.5 g/dL
White blood cells 5.22 5.48 10.12 2.41 11.71 4.5-13.5 x 103/mL
Red blood cells 2.04 2.40 3.63 2.79 2.37 4-5.2 x 106/uL
Haematocrit 11.6 14.3 20.7 15.7 12.5 35-40%
Platelets 389 346 475 292 501 150-350 x 103/mL
Mean corpuscular volume (MCV) 56.9 59.6 57 56.3 52.7 77-86 fL
Mean corpuscular haemoglobin (MCH) 14.7 15.8 15.4 15.1 12.2 27-31 pg
Mean corpuscular haemoglobin
25.9 26.6 27.1 26.8 23.2 31-34 g/dL
concentration (MCHC)
Red Cell Distribution Width (RDW) 20.1 18.2 19.2 21 26.9 11.5-15%
Reticulocyte 0.51 1.18 1.05 0.6 2.2 0.5-1
Iron Profile
Iron 1.9 1.6 2.2 2.01 2.1 Ferritin: 14-79 ng/mL, Iron: 2.8-22.9 mcmol/L
Total iron-binding capacity 64.85 61.22 79.28 73.40 69 45-72 mcmol/L
Blood Chemistry tests
Blood Urea Nitrogen 5 3.88 3 2.91 3.2 2.6-6.8 mmol/L
<12 years: 27.40-53.93 mcmol/L, <15 years:
Creatinine 42.02 54.30 36.22 54.74 39
39.78-71.61 mcmol/L
Aspartate Aminotransferase (AST) 37 19 19 17 22 18-36 U/L
Alanine Aminotransferase (ALT) 20 21 22 20 11.4 9-25 U/L
Calcium (Ca) 1.95 1.98 2.26 2.18 2.21 2.3-2.6 mmol/L
Sodium (Na) 136 134 140 135 142 136-143 mmol/L
Potassium (K) 3.3 3.4 3.7 3.9 4.05 3.5-5.1 mmol/L
Chloride (Cl) 99 98 103 97 109.8 101-107 mmol/L
Magnesium (Mg) 0.93 0.90 0.74 0.86 0.80 0.86-1.17 mmol/L
Phosphate (Ph) 1.1 1.2 1 1.1 0.96 1.3-1.9 mmol/L
<10 years: 192-321 U/L, <15 years: 157-272
Lactate Dehydrogenase (LDI) 311 251 257 253 277
U/L
Inflammatory Marker
Erythrocyte Sedimentation Rate (ESR) 30 47 19 27 47 0-10 mm/hr
C-Reactive Protein (CRP) Negative Negative Negative Negative Negative 0.1-1 mg/L
Coagulation Profile
Prothrombin Time (PT) 11.8 12..3 11.8 13 14.3 12.7-16.1 seconds
Partial Thromboplastin Time (PTT) 28.9 31.5 25 35 40 33.9-46.1 seconds
International Normalized Ratio (INR) 0.98 1.1 1 1.03 1.2 0.97-1.30
Haematological workup
Heinz body Negative Negative Negative Negative Negative
Haemoglobin H Negative Negative Negative Negative Negative
Haemoglobin electrophoresis Normal Normal Normal Normal Normal
Stool analysis- profile
All normal, no abnormality detected
2022 Al Ghadeer et al. Cureus 14(2): e22403. DOI 10.7759/cureus.22403 3 of 5
TABLE 2: Laboratory investigations
They were initially admitted in the Paediatric Intensive Care Unit (PICU), received packed red blood cells
(PRBCs) for normalization of haemoglobin levels. Then they were transferred to the general ward, and
started on oral ferrous sulfate and folic acid for iron deficiency anaemia and showered with permethrin
shampoo for head lice infestation. The patients were discharged on daily ferrous sulfate and permethrin
shampoo with regular follow-up with Paediatric Infectious Diseases.
Discussion
Lice are obligate human ectoparasites that survive and complete their life cycle on the host’s blood and
favour humid areas [4]. There are two distinct types of lice species that need humans as a host. Pthirus pubis
(pubic lice, carb lice), considered as a sexually transmitted disease (STD), predominantly infests genital hair.
Pediculus humanus (P. humanus) is composed of two ecotypes: P. humanus corporis lice infest the body and
P. humanus capitis lice infest the head [6,7]. Lice is a health issue worldwide due to its high prevalence and
spread through direct or indirect contact. Female lice live up to 30 days on a host, deposit 10 nits daily and
survive up to four days on objects that affirm their ease of transmission [1]. They usually affect the age group
of 3-11 years particularly in females due to the culture of long hair [2]. In this current series, all of the
patients were infested by pediculosis capitis, which are predominantly seen on heads, without apparent lice
on other areas like the pubis or body. The patients are female siblings living within the same house and all of
them had severe head lice except their parents. Lice are transmitted rapidly among children in the first
decade of life through direct contact during playing, sleeping or through indirect contact during sharing
personal items.
The clinical presentation of head lice is pruritis which leads to injured scalp, excoriation
and lymphadenopathy. Complications of head lice resulting from parasitism are secondary bacterial
infection, dermatitis, local post-therapeutic dermatitis and chronic anaemia. Diagnosis is established by the
evidence of living lice, nits on hair shafts [8,9]. Dermoscopy is used to differentiate nits comprising nymphs
from empty nits (pseudonymphs) [10]. All of our patients presented with symptomatic anaemia in the form
of pallor, generalized fatigability, dizziness and pagophagia. Syncopal attack was seen in the elder sister (13
years old) during the period of menstruation, which exacerbated the symptom. As there is a concurrent head
lice infestation, with the exclusion of other causes of anaemia, head lice are the causative reason of iron
deficiency anaemia through chronic active blood loss by lice.
Management of head lice necessitates the elimination of living lice and nits. Non-pharmacological
treatment consists of mechanical removal and combing with a nit comb every 2-3 days to prevent
reinfestation. Ensure good personal hygiene, disinfection of clothes at a temperature greater than 53.5°C
(128.3°F) and other personal items shouldn’t be shared. Pharmacological treatment consisting of applying
topical pediculicide includes pyrethrins permethrin 1% lotion [11]. Although shaving of the scalp is a simple
and effective method, it is not recommended because of psychological distress on the child [12]. At the time
of presentation, all of our patients received packed red blood cells due to severe symptomatic anaemia and a
significant drop in haemoglobin levels. Topical permethrin is applied and it is advised to repeat it after 10
days with general measurements to prevent reinfestation.
Conclusions
Iron deficiency anaemia is the most common type of anaemia worldwide. Usually, it is caused by dietary
insufficiency, malabsorptive diseases like celiac disease or chronic blood loss as in gastrointestinal bleeding.
Chronic blood loss is usually related to the gastrointestinal system due to inflammatory conditions or
mechanical causes such as a gastric ulcer. Pediculosis capitis is a hematophagic organism that causes
minimal blood loss, but a chronic infestation can be associated with a significant blood loss and presented
with iron deficiency anaemia as presented in our case. This should alert the physician to correlate the
relationship between chronic infestation and hematophagic organisms as a possible cause of iron deficiency
anaemia.
Additional Information
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In
compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services
info: All authors have declared that no financial support was received from any organization for the
submitted work. Financial relationships: All authors have declared that they have no financial
relationships at present or within the previous three years with any organizations that might have an
interest in the submitted work. Other relationships: All authors have declared that there are no other
relationships or activities that could appear to have influenced the submitted work.
2022 Al Ghadeer et al. Cureus 14(2): e22403. DOI 10.7759/cureus.22403 4 of 5
References
1. Burkhart CN, Burkhart CG: Fomite transmission in head lice. J Am Acad Dermatol. 2007, 56:1044-1047.
10.1016/j.jaad.2006.10.979
2. Motovali-Emami M, Aflatoonian MR, Fekri A, Yazdi M: Epidemiological aspects of Pediculosis capitis and
treatment evaluation in primary-school children in Iran. Pak J Biol Sci. 2008, 11:260-264.
10.3923/pjbs.2008.260.264
3. Nazari M, Fakoorziba MR, Shobeiri F: Pediculus capitis infestation according to sex and social factors in
Hamedan, Iran. Southeast Asian J Trop Med Public Health. 2006, 3:95-98.
4. Veracx A, Rivet R, McCoy KD, Brouqui P, Raoult D: Evidence that head and body lice on homeless persons
have the same genotype. PLoS One. 2012, 7:e45903. 10.1371/journal.pone.0045903
5. Speare R, Canyon DV, Melrose W: Quantification of blood intake of the head louse: Pediculus humanus
capitis. Int J Dermatol. 2006, 45:543-546. 10.1111/j.1365-4632.2005.02520.x
6. Badiaga S, Brouqui P: Human louse-transmitted infectious diseases . Clin Microbiol Infect. 2012, 18:332-
337. 10.1111/j.1469-0691.2012.03778.x
7. Sonthalia S, Varma S, Jha AK: Dermoscopy of pubic louse . Indian Dermatol Online J. 2019, 10:90-91.
10.4103/idoj.IDOJ_35_18
8. Meinking TL: Clinical update on resistance and treatment of Pediculosis capitis . Am J Manag Care. 2004,
10:264-268.
9. Nutanson I, Steen CJ, Schwartz RA, Janniger CK: Pediculus humanus capitis: an update. Acta
Dermatovenerol Alp Pannonica Adriat. 2008, 17:147-159.
10. Badri T, Hammami H, Benmously R, Mokhtar I, Fenniche S: Dermoscopic diagnosis of pediculosis capitis .
Acta Dermatovenerol Alp Pannonica Adriat. 2010, 19:45-46.
11. Sangaré AK, Doumbo OK, Raoult D: Management and treatment of human lice. Biomed Res Int. 2016,
2016:8962685. 10.1155/2016/8962685
12. Centers for Disease Control and Prevention. Head lice: treatment . (2018). Accessed: November 21, 2018:
https://www.cdc.gov/parasites/lice/head/treatment.html.
2022 Al Ghadeer et al. Cureus 14(2): e22403. DOI 10.7759/cureus.22403 5 of 5
You might also like
- Ninja Nerd AnemiaDocument13 pagesNinja Nerd AnemiaAndra Bauer100% (4)
- Referat (PPT) - Hiperleukositosis & LeukostasisDocument16 pagesReferat (PPT) - Hiperleukositosis & LeukostasisShapira alNo ratings yet
- Hematology PDFDocument11 pagesHematology PDFMaybelline TanNo ratings yet
- SICKLE CELL ANAEMIA A Dismissed Constant DISEASE of Expanding Worldwide WellbeingDocument6 pagesSICKLE CELL ANAEMIA A Dismissed Constant DISEASE of Expanding Worldwide WellbeingInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Pharmaceutical Sciences: A Case-Control Study of Prevalence of Anaemia Among Patients With Type 2 DiabetesDocument5 pagesPharmaceutical Sciences: A Case-Control Study of Prevalence of Anaemia Among Patients With Type 2 DiabetesiajpsNo ratings yet
- Anemia 3Document10 pagesAnemia 3Ranhie Pen'ned CendhirhieNo ratings yet
- Hematological DisordersDocument4 pagesHematological DisordersMahreen UmatiyaNo ratings yet
- Nurs 300 - Disease BrochureDocument2 pagesNurs 300 - Disease Brochureapi-224141758No ratings yet
- Nutrients 14 01168Document18 pagesNutrients 14 01168oscarNo ratings yet
- Apeced Syndrome (Family Observation)Document5 pagesApeced Syndrome (Family Observation)IJAR JOURNALNo ratings yet
- 10.1007@s00431 020 03597 5 1Document19 pages10.1007@s00431 020 03597 5 1manguloNo ratings yet
- Hemosiderosis - Practice Essentials, Pathophysiology, EtiologyDocument4 pagesHemosiderosis - Practice Essentials, Pathophysiology, EtiologyIrfan FathurrahmanNo ratings yet
- Hemolytic Uremic Syndrome A Case ReportDocument3 pagesHemolytic Uremic Syndrome A Case ReportAna-Mihaela BalanuțaNo ratings yet
- Iron Deficiency, Pasricha, Lancet, 2021Document16 pagesIron Deficiency, Pasricha, Lancet, 2021Monserrat Díaz ZafeNo ratings yet
- Original Contributions: Severe Iron Deficiency Anemia and Lice InfestationDocument4 pagesOriginal Contributions: Severe Iron Deficiency Anemia and Lice InfestationashNo ratings yet
- KimimiDocument2 pagesKimimiishaNo ratings yet
- JIDA SickleCellDocument6 pagesJIDA SickleCellpooja singhNo ratings yet
- 64 anemiaIBDguidelinesDocument10 pages64 anemiaIBDguidelinesdwiwidyapNo ratings yet
- J Bahria Univ Med Dent Coll 2020 10 1 72 76 EngDocument5 pagesJ Bahria Univ Med Dent Coll 2020 10 1 72 76 EngFortuneNo ratings yet
- Sickle Cell AnemiaDocument16 pagesSickle Cell AnemiaTel MagcamitNo ratings yet
- Keywords: Addison's Disease, Adrenoleukodystrophy, Hemochromatosis, Hyperpigmentation, PrednisoloneDocument3 pagesKeywords: Addison's Disease, Adrenoleukodystrophy, Hemochromatosis, Hyperpigmentation, PrednisoloneLeslie CruzNo ratings yet
- Ijsrp p9924Document6 pagesIjsrp p9924Maheen ShahzadNo ratings yet
- Diagnosis and Treatment of Diffuse Interstitial Lung DiseasesDocument21 pagesDiagnosis and Treatment of Diffuse Interstitial Lung Diseaseswajeeh rehmanNo ratings yet
- Tugas Behcet SyndromDocument6 pagesTugas Behcet SyndromIsmy HoiriyahNo ratings yet
- An Evidence Based Clinical Case Study To Assess Effectiveness of Homoeopathy in Case of AnemiaDocument6 pagesAn Evidence Based Clinical Case Study To Assess Effectiveness of Homoeopathy in Case of AnemiaEditor IJTSRD0% (1)
- Anaemia in The Elderly: Acta Clinica Belgica December 2008Document12 pagesAnaemia in The Elderly: Acta Clinica Belgica December 2008Juan ZamoraNo ratings yet
- Shields 2012Document4 pagesShields 2012aghniajolandaNo ratings yet
- Hidrosefalus KongenitalDocument8 pagesHidrosefalus KongenitalSebastiano SegaNo ratings yet
- Deficiencia de HierroDocument16 pagesDeficiencia de HierroCamilo CaceresNo ratings yet
- Hydatid Cyst Case ReportDocument10 pagesHydatid Cyst Case ReportAbdullah ZakiNo ratings yet
- JGH Open - 2022 - Eyoum BilleDocument15 pagesJGH Open - 2022 - Eyoum BilleJust some one Just some oneNo ratings yet
- Keratitis Ichthyosis Deafness (KID) SyndromeDocument4 pagesKeratitis Ichthyosis Deafness (KID) Syndromeali nazzalNo ratings yet
- Wiskott Aldrich Syndrome Case ReportDocument2 pagesWiskott Aldrich Syndrome Case ReportResearch ParkNo ratings yet
- 4.WJV 1 108Document8 pages4.WJV 1 108noordin MukasaNo ratings yet
- Haemolytic Uraemic SyndromeDocument6 pagesHaemolytic Uraemic SyndromeValerii GavrilutaNo ratings yet
- Sle FinalDocument41 pagesSle FinalAsniah Hadjiadatu Abdullah100% (1)
- Sickle Cell Anemia Term PaperDocument4 pagesSickle Cell Anemia Term Paperaflsmmmgx100% (1)
- A 4 Year Old Boy With Lemierre S Syndrome Caused B 2020 Journal of InfectionDocument3 pagesA 4 Year Old Boy With Lemierre S Syndrome Caused B 2020 Journal of InfectionDip ShitNo ratings yet
- Pediatric Diabetes InsipidusDocument4 pagesPediatric Diabetes InsipidusLissaberti AmaliahNo ratings yet
- 18 - Causas de Anemia en La VejezDocument10 pages18 - Causas de Anemia en La VejezFernandoVignoloNo ratings yet
- Wa0017.Document9 pagesWa0017.CHAMBI MAMANI JESSICA BETTYNo ratings yet
- Antibiotic-Associated Bloody Diarrhea in Infants: Clinical, Endoscopic, and Histopathologic ProfilesDocument5 pagesAntibiotic-Associated Bloody Diarrhea in Infants: Clinical, Endoscopic, and Histopathologic ProfilesdNo ratings yet
- Artigo Ingles SalomanDocument8 pagesArtigo Ingles SalomanBiomédica Fabiane IngrideNo ratings yet
- Study of Sickle Cell Anemia NewDocument12 pagesStudy of Sickle Cell Anemia NewS.NagarajanNo ratings yet
- A Case of Kikuchi-Fujimoto Disease Associated WithDocument10 pagesA Case of Kikuchi-Fujimoto Disease Associated Withفرجني موغNo ratings yet
- Iron Deficiency Anemia and Malnutrition in Pediatrics in Saudi Arabia: A Review ArticleDocument6 pagesIron Deficiency Anemia and Malnutrition in Pediatrics in Saudi Arabia: A Review ArticleIJAR JOURNALNo ratings yet
- Pediatric Acute Anemia PDFDocument6 pagesPediatric Acute Anemia PDFpurwanto nugrohoNo ratings yet
- Allergy: Vogt-Koyanagi-Harada Disease in An 8-Year-Old BoyDocument6 pagesAllergy: Vogt-Koyanagi-Harada Disease in An 8-Year-Old BoyErna HidayatNo ratings yet
- Periorbital Edema: A Puzzle No More?: ReviewDocument10 pagesPeriorbital Edema: A Puzzle No More?: ReviewJavier Infantes MolinaNo ratings yet
- 3rd Clinical CaseDocument4 pages3rd Clinical CasejoidaNo ratings yet
- Iron Deficiency Anaemia Revisited: M. D. Cappellini, K. M. Musallam & A. T. TaherDocument18 pagesIron Deficiency Anaemia Revisited: M. D. Cappellini, K. M. Musallam & A. T. TaherJhonyHinojosaNo ratings yet
- Case Bok Anemia - FinaldocxDocument14 pagesCase Bok Anemia - FinaldocxChristine DoloyayaNo ratings yet
- Hereditary SpherocytosisDocument39 pagesHereditary SpherocytosisjoannaNo ratings yet
- When An Exanthem Misleads The Diagnosis Association of Incomplete Kawasaki and Covid 19 A Case ReportDocument3 pagesWhen An Exanthem Misleads The Diagnosis Association of Incomplete Kawasaki and Covid 19 A Case ReportHerald Scholarly Open AccessNo ratings yet
- Fluid and ElectrolytesDocument135 pagesFluid and ElectrolytesLindsay PinedaNo ratings yet
- Journal of Internal Medicine - 2019 - Cappellini - Iron Deficiency Anaemia RevisitedDocument18 pagesJournal of Internal Medicine - 2019 - Cappellini - Iron Deficiency Anaemia RevisitedRaúl Joaquín Espinoza del CarmemNo ratings yet
- Oral Candidiasis: A Short Review and A Case Report: December 2018Document5 pagesOral Candidiasis: A Short Review and A Case Report: December 2018RAfii KerenNo ratings yet
- Anemia Ferropenica Rev2019Document18 pagesAnemia Ferropenica Rev2019Albamis MojicaNo ratings yet
- JBMR 37 2602Document13 pagesJBMR 37 2602Juanjo Moreno LópezNo ratings yet
- AngularcheilitisDocument3 pagesAngularcheilitisfelaxis fNo ratings yet
- Ankylosing Spondylitis HLA-B27 and Klebsiella - AnDocument32 pagesAnkylosing Spondylitis HLA-B27 and Klebsiella - AnbciebienNo ratings yet
- Bombay Blood Group - Case ReportDocument3 pagesBombay Blood Group - Case ReportPremier PublishersNo ratings yet
- Dialysis & TransplantsDocument23 pagesDialysis & TransplantsKhadija Ali100% (1)
- A & P HESI QuizletDocument6 pagesA & P HESI QuizletDeshaun JacksonNo ratings yet
- Final DX ResultsDocument9 pagesFinal DX ResultszysheaiNo ratings yet
- Mixing Studies-: aPTT or PT 1:1 MixDocument12 pagesMixing Studies-: aPTT or PT 1:1 MixVimal NishadNo ratings yet
- One Mark FMDocument4 pagesOne Mark FMragulraj6699No ratings yet
- Transport in Plants and Animals.Document126 pagesTransport in Plants and Animals.Kiama GitahiNo ratings yet
- Anatomy and Physiology 2 Lab ManualDocument129 pagesAnatomy and Physiology 2 Lab ManualMAJEETH மஜீத் TIRUNELVELINo ratings yet
- Accurasi Perhitungan PlateletDocument68 pagesAccurasi Perhitungan PlateletMaria Yosefina HeraNo ratings yet
- Thesis - Iron Deficiency AnemiaDocument5 pagesThesis - Iron Deficiency Anemiaafaybiikh100% (2)
- Doctors and Experts About Distilled WaterDocument35 pagesDoctors and Experts About Distilled Waterartisanicview100% (2)
- Supplementary Philosophy Course, Nos. 1-14Document32 pagesSupplementary Philosophy Course, Nos. 1-14jehid777No ratings yet
- Physical Education Nine Ten English VersionDocument149 pagesPhysical Education Nine Ten English Versiondsafg87g87gawdwNo ratings yet
- Anatomy and Physiology of Farm AnimalsDocument157 pagesAnatomy and Physiology of Farm AnimalsOliver Talip100% (1)
- Mispa Count Service ManualDocument76 pagesMispa Count Service Manuallemanhcuong1503No ratings yet
- Gas TransportDocument10 pagesGas TransportDaveNo ratings yet
- Mat & Sat-07Document30 pagesMat & Sat-07RamNagalNo ratings yet
- Alifax Roller 20pnuser Manualrev1920211029Document87 pagesAlifax Roller 20pnuser Manualrev1920211029ZainalAbidinNo ratings yet
- MISTRAL PresentationDocument13 pagesMISTRAL PresentationPERFUZIJANo ratings yet
- Pathophysiology Schematic Diagram and NarrativeDocument15 pagesPathophysiology Schematic Diagram and NarrativeKathrina CraveNo ratings yet
- PST / JEST Test General Science Class 7 Unit.1 Human Organ SystemsDocument28 pagesPST / JEST Test General Science Class 7 Unit.1 Human Organ SystemsNawab AliNo ratings yet
- Blood: Types of Blood Cells and Their Average NumberDocument32 pagesBlood: Types of Blood Cells and Their Average NumberSumayya KabeerNo ratings yet
- PowerPoint Presentation Resp and CircDocument7 pagesPowerPoint Presentation Resp and CircRobelle RelativoNo ratings yet
- Sickle Cell DiseaseDocument8 pagesSickle Cell DiseaseShafieyah ShafiefieNo ratings yet
- 1.4 The Lymphatic System: Prepared By: Ling Mei TengDocument15 pages1.4 The Lymphatic System: Prepared By: Ling Mei TengJuliet LingNo ratings yet
- Venous Thromboembolism in PregnancyDocument10 pagesVenous Thromboembolism in Pregnancydr.diverNo ratings yet
- Terumo Capiox FXDocument6 pagesTerumo Capiox FXShuhengNo ratings yet