Professional Documents
Culture Documents
Chemotherapy Plus Percutaneous Radiofrequency Ablation in Patients With Inoperable Colorectal Liver Metastases
Uploaded by
Haya RihanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chemotherapy Plus Percutaneous Radiofrequency Ablation in Patients With Inoperable Colorectal Liver Metastases
Uploaded by
Haya RihanCopyright:
Available Formats
Online Submissions: http://www.wjgnet.
com/1948-5204office World J Gastrointest Oncol 2011 April 15; 3(4): 60-66
wjgo@wjgnet.com ISSN 1948-5204 (online)
doi:10.4251/wjgo.v3.i4.60 © 2011 Baishideng. All rights reserved.
BRIEF ARTICLE
Chemotherapy plus percutaneous radiofrequency ablation
in patients with inoperable colorectal liver metastases
Joseph Sgouros, James Cast, Krishna K Garadi, Maria Belechri, David J Breen, John RT Monson,
Anthony Maraveyas
Joseph Sgouros, Krishna K Garadi, Maria Belechri, Antho- RESULTS: Thirteen patients were included in the ad-
ny Maraveyas, Academic Department of Oncology, Castle Hill junctive chemotherapy trial and 17 in the other two. At
Hospital, Cottingham, HU16 5JQ, United Kingdom inclusion they had 1-4 liver metastases (up to 6.5 cm
Joseph Sgouros, “Agii Anargiri” Cancer Hospital, N Kifissia, in size). Two patients died during chemotherapy. All pa-
14564, Greece tients in the adjunctive chemotherapy trial and 44% in
James Cast, David J Breen, Radiology Department, Castle
the primary chemotherapy studies had their metastases
Hill Hospital, Cottingham, HU16 5JQ, United Kingdom
John RT Monson, Division of Colorectal Surgery, Department
ablated. Median PFS and overall survival in the adjunc-
of Surgery University of Rochester Medical Center, 601 Elm- tive study were 13 and 24 mo respectively while in the
wood Avenue, Box SURG, Rochester, NY 14642, United States primary chemotherapy studies they were 10 and 21 mo
Author contributions: Cast J, Breen DJ, Monson JRT and respectively. Eighty one percent of the patients had tu-
Maraveyas A designed the studies; Sgouros J, Cast J, Garadi mour relapse in at least one previously ablated lesion.
KK, Belechri M, Breen DJ, Monson JRT and Maraveyas A
performed the research; Sgouros J and Maraveyas A wrote the CONCLUSION: Chemotherapy plus RFA in patients
paper; Cast J, Garadi KK, Belechri M, Breen DJ and Monson with low volume inoperable colorectal liver metastases
JRT reviewed the paper. seems safe and relatively effective. The high local recur-
Correspondence to: Joseph Sgouros, MD, “Agii Anargiri” rence rate is of concern.
Cancer Hospital, N Kifissia, 14564,
Greece. josephsgouros@yahoo.co.uk
© 2011 Baishideng. All rights reserved.
Telephone: +30-694-7961576 Fax: +30-210-8003946
Received: August 15, 2010 Revised: February 10, 2011
Accepted: February 17, 2011 Key words: Chemotherapy; Colorectal cancer; Liver
Published online: April 15, 2011 metastases; Radiofrequency ablation
Peer reviewer: Stefan Boeck, MD, Department of Internal Med-
icine III, Klinikum Grosshadern, Ludwig-Maximilians-University
of Munich, Marchioninistr 15, Munich D-81377, Germany
Abstract
AIM: To access the efficacy of chemotherapy plus ra- Sgouros J, Cast J, Garadi KK, Belechri M, Breen DJ, Monson
diofrequency ablation (RFA) as one line of treatment in JRT, Maraveyas A. Chemotherapy plus percutaneous radiofre-
inoperable colorectal liver metastases. quency ablation in patients with inoperable colorectal liver me-
tastases. World J Gastrointest Oncol 2011; 3(4): 60-66 Avail-
METHODS: Eligible patients were included in three able from: URL: http://www.wjgnet.com/1948-5204/full/v3/i4/
Phase Ⅱ studies. In the first study percutaneous RFA 60.htm DOI: http://dx.doi.org/10.4251/wjgo.v3.i4.60
was used first followed by 6 cycles of 5-fluorouracil,
leucovorin and irinotecan combination (FOLFIRI) (ad-
junctive chemotherapy trial). In the other two, che-
motherapy (FOLFIRI or 5-fluorouracil, leucovorin and
INTRODUCTION
oxaliplatin combination) up to 12 cycles was used first
with percutaneous RFA offered to responding patients Liver represents the most common site of metastases for
(primary chemotherapy trials). patients with colorectal cancer. Fifteen to twenty percent
WJGO|www.wjgnet.com 60 April 15, 2011|Volume 3|Issue 4|
Sgouros J et al . Chemotherapy and radiofrequency ablation in colorectal liver metastases
of patients at initial presentation have synchronous liver could be treated with RFA and in whom irinotecan had al-
metastases and up to 40% will develop metachronous ready failed, we started a third study where 5-fluorouracil,
liver metastases despite surgery and adjuvant treatment[1]. oxaliplatin combination was used. Preliminary safety and
Often liver is the sole site of disease recurrence. For these survival data of the first 10 patients included in our pro-
patients the best available treatment, offering the only spective Phase Ⅱ work have been previously reported[11].
chance of cure, is surgical resection of the metastases Here we present the mature analysis, the efficacy and the
combined with chemotherapy either in the neo-adjuvant toxicity of the combination of the two treatments with
or in the adjuvant setting[2]. This group of patients, treated data from all participating patients included. Results of the
with both modalities seems has a 35% 5-year progression three studies are presented together as the final accrual was
free survival (PFS), a 50% 5-year overall survival and a not as had been anticipated.
median survival of around 60 mo[3].
However, not all patients with metastatic disease con-
fined to the liver, even those with low disease burden, are MATERIALS AND METHODS
candidates for liver resection. Quite often liver involve- Patient selection
ment from the metastases is so extensive that safe resec- The target group for our Phase Ⅱ work was patients with
tion delivering clear resection margins (one of the most colorectal cancer with had liver-only metastases which,
important prognostic factors for good final outcome[4]) is after discussion at the multidisciplinary team meeting,
not possible. At other times resection is not possible for was deemed inoperable for anatomical reasons or due to
anatomical reasons or due to patients’ comorbidities. comorbidities but was potentially treatable with RFA and
In patients who cannot have a surgical procedure, chemotherapy. To select patients with a high chance of
systemic therapy (chemotherapy with targeted agents) is total ablation, patients were deemed eligible for one of the
the treatment of choice, but it is given with a palliative above studies if they had fewer than seven liver metastas-
intent. Median survival in patients with liver only unre- es of maximum diameter 5 cm where RFA was given first
sectable metastases, treated with the current agents, has or 7cm where chemotherapy was delivered first. Protocols
not been precisely defined. However, it probably does not were subsequently amended to reduce the maximum di-
differ much from the median survival of patients who ameter of the liver metastases eligible for ablation to 3.5
have inoperable metastases to other organs or metastases cm as the injection of hypertonic saline prior to the RFA
to other organs in addition to inoperable liver metastases for large lesions (a method used to increase the necrosis
(around 20 to 24 mo)[5,6]. In an attempt to improve sur- diameter) was abandoned. Other inclusion criteria were
vival in patients with inoperable colorectal liver metasta- adequate liver and renal function and adequate perform-
ses, many investigators have used regional therapies such ance status (0 or 1 by WHO performance status scale).
as transarterial chemoembolization, intrahepatic arterial Previous chemotherapy was allowed (either adjuvant or
chemotherapy and radiofrequency ablation (RFA)[7-9]. for metastatic disease) providing it was ceased four weeks
In the latter technique, a probe is inserted intraopera- before the trial. In cases where there was prior exposure
tively, laparoscopically or percutaneously into the target to irinotecan or oxaliplatin, patients received oxaliplatin or
metastases and a monopolar alternating electric current irinotecan respectively. Patients who had prior resection
is delivered directly into the target tissue. This causes of liver metastases or prior RFA treatment were also eli-
electrons in the tissue to vibrate back and forth at a high gible. All patients had to sign a consent form prior to the
frequency, leading to the production of heat and thereby commencement of the treatment.
causing cell death[10].
Results of the use of RFA in colorectal liver metasta- Treatment plan
ses have been reported from many centres with promising As already mentioned, in one study RFA of the liver
outcomes and they have been recently reviewed by Stang metastases was done first, followed by chemotherapy (ad-
et al[9]. Most of the papers reviewed in this article were clin- junctive chemotherapy study). In the other two studies,
ical series where RFA was used as a single modality. Che- chemotherapy was delivered initially with RFA to follow
motherapy had already failed or it was used upon further (primary chemotherapy studies). In the adjunctive che-
progression. There was wide variability in the results with motherapy study and in the first primary chemotherapy
the median local progression time in patients who had only study, the chemotherapy regime used was 5-fluorouracil,
RFA varying between 3.5 and 9 mo, systemic PFS varying leucovorin and irinotecan combination (FOLFIRI) fort-
between 6 and 13 mo and median overall survival vary- nightly while in the second primary chemotherapy study
ing between 24 and 59 mo[9]. It seemed reasonable to us the 5-fluorouracil, leucovorin and oxaliplatin combina-
to study the combination of systemic chemotherapy with tion (FOLFOX) regime was used, again every two weeks.
RFA as one line of treatment, trying to determine whether Both regimes were used as per the FOCUS trial through a
PFS could be increased compared to RFA only. Initially venous device (Hickman catheter or peripherally inserted
we started two Phase Ⅱ studies where RFA was given first central catheter)[12]. In the adjunctive chemotherapy study,
in one study and in the other chemotherapy first (in both chemotherapy was given for six cycles, while in both
studies we used the 5-fluorouracil, irinotecan combina- primary chemotherapy studies patients could receive 12
tion). As later it became obvious that we had patients that cycles in total provided they were responding to chemo-
WJGO|www.wjgnet.com 61 April 15, 2011|Volume 3|Issue 4|
Sgouros J et al . Chemotherapy and radiofrequency ablation in colorectal liver metastases
therapy, with radiological assessment every 4 cycles to tients were included in the primary FOLFIRI study and
identify the earliest possible opportunity for RFA. 8 (5 of whom had already participated in the two previ-
The percutaneous RFA technique we used has been ously mentioned studies) in the primary FOLFOX study.
described before[13]. It was undertaken using a water- Patients’ characteristics are shown in Table 1 and the main
cooled RFA system (Radionics, Burlington, Mass, USA) point to note is the geriatric nature of this population
under ultrasound or computer tomography guidance and which reflects the decision-making quandaries (both in
under sedation with midazolam and fentanyl. For some terms of co-morbidities, mostly vascular, but also patient
larger lesions hypertonic saline was injected prior to the preference) in these patients, despite relatively pauci-
RFA to increase the necrosis diameter. Subjects remained metastatic disease. Patients participating in the adjunctive
in-patients for 24 h to make sure no acute complications chemotherapy study tended to have fewer and smaller
developed and they underwent further imaging 3-5 d later liver metastases compared to the patients included in the
as out-patients to assess total ablation of metastases. two primary chemotherapy studies.
Evaluation of response Efficacy in the adjunctive chemotherapy study
We determined response to chemotherapy using the re- The 13 patients in the adjunctive chemotherapy study
sponse evaluation criteria in solid tumours (RECIST)[14]. had a total of 20 liver metastases (the maximum diam-
The RFA technique was deemed successful if the post- eter of 18 lesions was smaller than 3.5 cm) ablated and
procedure scan revealed a roughly spherical area of non- subsequently received 3-6 (median 6) cycles of FOLF-
enhancement in the area of the treated metastasis. The IRI. RFA was well tolerated with mild local pain occur-
procedure was also classified as successful even if there ring in some patients. The initial radiological result of
was some symmetrical peripheral enhancement (thought metastasis ablation was not satisfactory for 4 lesions
to be normal reactive changes following ablation). (one larger than 3.5 cm) in 4 different patients. In two
cases the procedure was repeated and the radiological
Patient follow up outcome was then satisfactory (overall good radiological
Following completion of treatment, patients were fol- result in 90% of the metastases ablated) (Table 2). Most
lowed up at regular intervals. In most cases computer patients completed the planned course of 6 cycles of
tomography scans of the thorax, abdomen and pelvis as chemotherapy with only minor side-effects. As can be
well as the tumour markers CEA and CA19-9 were car- seen in Table 3, one patient discontinued chemotherapy
ried out every three months until progression or death. early as he developed bacterial endocarditis requiring a
prolonged course of antibiotics. Another patient died
Statistical analysis suddenly during treatment. The cause of death was de-
PFS was measured from inclusion in the study to pro- termined post-mortem as acute cardiomyopathy and was
gression or death (in case death occurred prior to docu- thought to be related to 5-fluorouracil toxicity.
mented progression) and overall survival (OS) from Median PFS and overall survival of these patients
inclusion in the study to death. Statistical comparisons, were 13 (95% CI: 3.1-22.9) and 24 mo (95% CI: 17-31.1)
where needed, were carried out using the Chi-square respectively. For 60% of the patients, the site of initial
and Fisher’s exact test. The Kaplan-Meier method was progression was only in at least one liver lesion previously
used to calculate progression free and overall survival treated with RFA, for 10% both in RFA-treated lesions
curves[15]. The SPSS statistical package was used and a P and at other sites and for 30% of patients only in other
value of < 0.05 was considered statistically significant organs.
for all analyses. The expected end point of the stud-
ies was PFS of 12.5 mo. That was based on data dating Efficacy in the primary chemotherapy studies
from around 2000 (when our trials commenced) indi- The 17 patients who participated in the two primary
cating median PFS in a study using RFA alone[16], and chemotherapy studies (one patient participated in both
on the hypothesis that chemotherapy would cause an studies) received 2-12 cycles of chemotherapy. Chemo-
increase of 25% on the PFS achieved with RFA alone. A therapy was generally well tolerated. One patient discon-
sample size calculation was not performed. tinued treatment early due to deterioration of her general
The protocols received local research ethics commit- condition thought to be related to the chemotherapy
tee approval (regulatory numbers 06/00/095, 06/00/096 (FOLFOX group) and one patient as died due to sepsis
and 12/02/14) and were run under the Doctors and while on chemotherapy (FOLFIRI group). As can be seen
Dentists Exemption scheme (DDX). in Table 3, 22% of patients responded to chemotherapy
and in another 55% of patients their disease remained
stable. In 8 cases (44%) with a total of 11 liver metastases
RESULTS (7 with maximum diameter ≤ 3.5 cm), RFA was carried
Patient characteristics out subsequently. Ablation was not carried out in patients
Between September 2000 and August 2004, 13 patients with progressive disease, in patients with stable disease
participated in the adjunctive chemotherapy study, 10 pa- but with metastases which could not be safely ablated and
WJGO|www.wjgnet.com 62 April 15, 2011|Volume 3|Issue 4|
Sgouros J et al . Chemotherapy and radiofrequency ablation in colorectal liver metastases
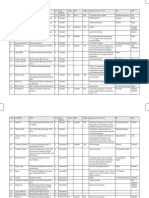
Table 1 Baseline characteristics of the patients
Characteristic Adjunctive chemotherapy Primary FOLFIRI Primary FOLFOX
group (n = 13) group (n = 10) group (n = 8)
Age (yr)
Range 47-84 54-80 60-84
Median 77 68.5 80
Sex (%)
Male 9 (69.0) 7 (70.0) 3 (37.5)
Female 4 (31.0) 3 (30.0) 5 (62.5)
Stage of cancer at initial presentation (%)
Stage Ⅰ 2 (15.5) 0 2 (25.0)
Stage Ⅱ 5 (38.5) 4 (40.0) 0
Stage Ⅲ 6 (46.0) 1 (10.0) 1 (12.5)
Stage Ⅳ 0 4 (40.0) 5 (62.5)
Missing data 0 1 (10.0)
Previous chemotherapy
Yes (adjuvant) 10 2 3
Yes (for metastatic disease) 0 0 5
No 3 8 3
Previous RFA
Yes 0 0 5
No 13 10 3
Liver metastases per patient at inclusion
Range 1-3 1-4 1-4
Median 1 2 1
1
Max diameter of larger metastasis per patient at inclusion (cm)
Range 1.5-5.5 1.7-6.5 2.8-5.5
Mean 3 4.2 4.5
1
Sum of the maximum diameters of liver metastases per patient at inclusion (cm)
Range 2-8 1.7-9.9 3.9-14.6
Mean 4.1 6.4 6.6
1
There was statistically significant difference between the adjunctive chemotherapy group and the two primary chemotherapy groups. FOLFIRI: 5-fluoro-
uracil, leucovorin and irinotecan combination; FOLFOX: 5-fluorouracil, leucovorin and oxaliplatin combination; RFA: Radiofrequency ablation.
Table 2 Distribution of radiofrequency ablation administration and efficacy in the three different patient’s groups
Characteristic Adjunctive chemotherapy Primary FOLFIRI Primary FOLFOX
group (n = 13) group (n = 10) group (n = 8)
Patients who had RFA 13 4 4
Metastases treated with RFA 20 7 4
Metastases per patient treated with RFA
Range 1-3 1-3 1-1
Median 1 2 1
Metastases with good radiological result after first attempt (%) 16 (80.0) 3 (43.0) 3 (75.0)
Metastases with good result following further RFA attempts 2 3 0
Metastases with good radiological result in total (%) 18 (90.0) 6 (86.0) 3 (75.0)
FOLFIRI: 5-fluorouracil, leucovorin and irinotecan combination; FOLFOX: 5-fluorouracil, leucovorin and oxaliplatin combination; RFA: Radiofrequency
ablation.
in one more patient who withdrew her consent. For 5 le- Survival times in patients of all groups who had received
sions (one with diameter > 3.5 cm) the initial radiological chemotherapy and RFA
result was not satisfactory. Three of them were re-treated Overall all 13 patients from the adjunctive chemotherapy
(at least two further attempts for each lesion) with a final study and 8 (out of 18) from the two primary chemother-
satisfactory radiological result (overall good radiological apy trials were exposed to both modalities. Median PFS
result 73%) (Table 2). RFA was well tolerated with mild and overall survival in these patients were 11 and 29 mo
pain in the right hypochondrium being the most frequent respectively, significantly longer than for the rest of our
side-effect of the procedure. patients who received only chemotherapy (median PFS
Median PFS of participants in the primary chemothera- and overall survival 3 and 7 mo respectively).
py studies was 10 mo (95% CI: 7-13). All patients who had
RFA, relapsed in at least one ablated lesion and 33.3% of
them simultaneously developed extrahepatic progression. DISCUSSION
Median overall survival was 21 mo (95% CI: 18.3-23.7). We have presented here the final results of our three
WJGO|www.wjgnet.com 63 April 15, 2011|Volume 3|Issue 4|
Sgouros J et al . Chemotherapy and radiofrequency ablation in colorectal liver metastases
Table 3 Distribution of chemotherapy administration, efficacy and toxicity in the three different patient’s groups
Characteristic Adjunctive chemotherapy group (n = 13) Primary FOLFIRI group (n = 10) Primary FOLFOX group (n = 8)
Chemotherapy cycles given per patient
Range 3-6 2-12 3-12
Median 6 7 8
Response to chemotherapy (%)
CR/PR - 2 (20.0) 2 (25.0)
SD - 5 (50.0) 5 (62.5)
PD - 2 (20.0) 1 (12.5)
Not applicable 13 1 (10.0) 0
Discontinuation of chemotherapy
Due to death 1 1 0
Due to toxicity 1 0 1
CR: Complete response; PR: Partial response; SD: Stable disease; PD: Progressive disease; FOLFIRI: 5-fluorouracil, leucovorin and irinotecan combination;
FOLFOX: 5-fluorouracil, leucovorin and oxaliplatin combination; RFA: Radiofrequency ablation.
phase Ⅱ studies where chemotherapy and RFA were of the two treatment modalities is superior to chemo-
given in a sequential way in patients with small volume therapy only seems to be supported by the final results
inoperable colorectal liver metastases. To the best of our of the CLOCC study where systemic therapy with FOL-
knowledge this is the first full report of a prospectively FOX plus or minus bevacizumab was compared to the
designed study using both modalities in this patient- same systemic therapy plus RFA in patients with color-
category. ectal cancer and fewer than nine liver metastases[18]. The
A limitation of the data presented is the small num- results of this EORTC multicenter study showed that
ber of patients included in each study. At the design of patients treated with chemotherapy and RFA had longer
these studies, it was anticipated that more patients would median PFS than patients treated only with chemothera-
participate in each trial but it became apparent that for py (16.8 mo vs 9.9 mo).
only a small minority of patients with low volume liver Of concern is the high recurrence rate (81.25%) at the
disease a resection would either not be indicated, not ablated lesions which did not seem to be related to the
possible or would be turned down by the patient. There- size of the metastases. More worrying is the fact that lo-
fore a summative report was thought the only way lessen cal recurrence was documented in all patients who had
this numerical limitation and thereby reach useful clinical RFA once their metastases were down-sized with primary
conclusions. chemotherapy. This recurrence rate is higher than those
Treatment was reasonably well tolerated. Apart from reported in previously published studies although great
mild pain occurring in a few patients and for a few days variation exists. For example, in two studies where laparo-
following the local ablative technique, no other side- scopic RFA was used, the recurrence rate of the lesions
effects or complications developed in patients treated ablated ranged between 6.7% and 28%[19,20] while in two
with subcutaneous RFA. other studies where patients had the procedure percutane-
Chemotherapy was similarly well tolerated although ously, local recurrence rate was approximately 50%[21,22].
two patients died during treatment (mortality 6.4%) and In a meta-analysis published after our studies were closed,
another two discontinued treatment early due to com- Mulier et al[23] showed that the two most important factors
plications related directly or indirectly to chemotherapy. predicting low recurrence rates in primary or metastatic
Mortality for this geriatric population treated with che- liver tumours treated with RFA are the surgical approach
motherapy seems to be in line with literature figures[17]. for placing the electrodes and lesions smaller than 3 cm.
We found that PFS in the adjunctive chemotherapy Neither of these criteria was met in our current studies
group was 13 mo and in the primary chemotherapy group and this possibly played a part in the high local recurrence
10 mo. We can not conclude that the combination that rate. It seems that the chemotherapy used in the current
uses RFA initally is superior to the combination using trials did not affect the high local recurrence rate.
chemotherapy initially as patients in the primary chemo- In conclusion the combination of RFA with chemo-
therapy studies had larger liver metastases and also almost therapy in patients with low volume inoperable colorec-
50% of the patients were unable to receive RFA treatment. tal liver metastases can be safely delivered and seems to
The primary end point of 12.5 mo median PFS in be relatively effective. The CLOCC study may perhaps
our patients was met only in the adjunctive chemother- answer the question of whether the combination is bet-
apy study. Patients who participated in the two primary ter than chemotherapy only. It would also very interest-
chemotherapy studies had a shorter median PFS, prob- ing if the combination treatment were to be compared
ably attributable to the fact they had higher tumour bur- with RFA as sole treatment treatment in different arms
den and less than 50% were able to have RFA in addition of a Phase Ⅲ trial. For such a study only patients with
to chemotherapy. The suggestion that the combination metastases smaller than 3 cm should be included.
WJGO|www.wjgnet.com 64 April 15, 2011|Volume 3|Issue 4|
Sgouros J et al . Chemotherapy and radiofrequency ablation in colorectal liver metastases
6 Cassidy J, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A,
ACKNOWLEDGMENTS Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Cou-
The authors thank the patients for participating in these ture F, Sirzén F, Saltz L. Randomized phase III study of
capecitabine plus oxaliplatin compared with fluorouracil/
studies and the staff of the Hull Cancer Unit Trials office
folinic acid plus oxaliplatin as first-line therapy for meta-
for their support and hard work. Also Aventis for an un- static colorectal cancer. J Clin Oncol 2008; 26: 2006-2012
restricted grant. 7 Vogl TJ, Zangos S, Eichler K, Yakoub D, Nabil M. Colorec-
tal liver metastases: regional chemotherapy via transarterial
chemoembolization (TACE) and hepatic chemoperfusion:
COMMENTS an update. Eur Radiol 2007; 17: 1025-1034
8 Dizon DS, Schwartz J, Kemeny N. Regional chemotherapy:
Background a focus on hepatic artery infusion for colorectal cancer liver
Chemotherapy and radiofrequency ablation are used in the treatment of metastases. Surg Oncol Clin N Am 2008; 17: 759-771, viii
colorectal liver metastases. Usually radiofrequency ablation is used once che- 9 Stang A, Fischbach R, Teichmann W, Bokemeyer C, Brau-
motherapy has failed. Limited data exist regarding the use of both treatment mann D. A systematic review on the clinical benefit and role
modalities as a single line of treatment. of radiofrequency ablation as treatment of colorectal liver
Research frontiers metastases. Eur J Cancer 2009; 45: 1748-1756
There is one randomised study by EORTC comparing chemotherapy plus Ra- 10 Johnson DB, Cadeddu JA. Radiofrequency interstitial tu-
diofrequency ablation (RFA) to chemotherapy only but so far results have been mor ablation: dry electrode. J Endourol 2003; 17: 557-562
published in an abstract form. 11 White TJ, Cast J, Breen D, Smyth EF, Hartley JE, Monson
Innovations and breakthroughs JRT, Maraveyas A. Phase II trial of CPT-11/5FU/FA chemo-
The current article is the first paper with results of the efficacy and tolerability of therapy following radiofrequency ablation for patients with
the combination of chemotherapy and RFA collected prospectively. low volume inoperable colorectal liver metastases with the
Applications intent to achieve total gross disease ablation-a preliminary
The results of this paper show that the combination of chemotherapy and RFA report. Proc Am Soc Clin Oncol 2003; 22 :A1398
in patients with colorectal liver metastases is safe. Confirmatory studies are 12 Seymour MT, Maughan TS, Ledermann JA, Topham C,
needed for establishing its efficacy. James R, Gwyther SJ, Smith DB, Shepherd S, Maraveyas A,
Ferry DR, Meade AM, Thompson L, Griffiths GO, Parmar
Terminology MK, Stephens RJ. Different strategies of sequential and com-
RFA is a technique where a probe is inserted into the target metastases and a bination chemotherapy for patients with poor prognosis
monopolar alternating electric current is delivered directly into the target tissue. advanced colorectal cancer (MRC FOCUS): a randomised
This causes electrons in the tissue to vibrate back and forth at a high frequency, controlled trial. Lancet 2007; 370: 143-152
leading to the production of heat and thereby causing cell death 13 White TJ, Roy-Choudhury SH, Breen DJ, Cast J, Maraveyas
Peer review A, Smyth EF, Hartley JE, Monson JR. Percutaneous radio-
The patient number is rather low, and the study population in this pooled analy- frequency ablation of colorectal hepatic metastases – initial
sis is heterogeneous. However, these trials were conducted well, each patient experience. An adjunct technique to systemic chemotherapy
gave written informed consent and local research ethics committee approval for those with inoperable colorectal hepatic metastases. Dig
was also obtained. Adequate statistical methods were applied and of note, the Surg 2004; 21: 314-320
authors also discussed the main limitations of their analysis within the discus- 14 Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan
sion section appropriately. The obtained data are presented adequately and the RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom
results are discussed within the current scientific standard of CRC research. AT, Christian MC, Gwyther SG. New guidelines to evaluate
the response to treatment in solid tumors. European Orga-
nization for Research and Treatment of Cancer, National
REFERENCES Cancer Institute of the United States, National Cancer Insti-
tute of Canada. J Natl Cancer Inst 2000; 92: 205-216
1 Alexander HR Jr, Berlin J, Garofalo M. Metastatic cancer
15 Kaplan E, Meier P. Nonparametric estimation from incom-
to the liver. In: De Vita VT Jr, Lawrence TS, Rosenberg SA,
plete observations. J Am Stat Assoc 1958; 53: 457-481
editors. Cancer: Principles and Practice of Oncology. Phila-
16 de Baere T, Elias D, Dromain C, Din MG, Kuoch V, Ducreux
delphia, PA: Lippincott Williams & Wilkins, 2008: 2493-2510
M, Boige V, Lassau N, Marteau V, Lasser P, Roche A. Radio-
2 Nordlinger B, Van Cutsem E, Gruenberger T, Glimelius B,
frequency ablation of 100 hepatic metastases with a mean
Poston G, Rougier P, Sobrero A, Ychou M. Combination of
follow-up of more than 1 year. AJR Am J Roentgenol 2000;
surgery and chemotherapy and the role of targeted agents
in the treatment of patients with colorectal liver metastases: 175: 1619-1625
recommendations from an expert panel. Ann Oncol 2009; 20: 17 Folprecht G, Seymour MT, Saltz L, Douillard JY, Hecker H,
985-992 Stephens RJ, Maughan TS, Van Cutsem E, Rougier P, Mitry
3 Mitry E, Fields AL, Bleiberg H, Labianca R, Portier G, Tu D, E, Schubert U, Köhne CH. Irinotecan/fluorouracil combina-
Nitti D, Torri V, Elias D, O'Callaghan C, Langer B, Marti- tion in first-line therapy of older and younger patients with
gnoni G, Bouché O, Lazorthes F, Van Cutsem E, Bedenne L, metastatic colorectal cancer: combined analysis of 2,691 pa-
Moore MJ, Rougier P. Adjuvant chemotherapy after poten- tients in randomized controlled trials. J Clin Oncol 2008; 26:
tially curative resection of metastases from colorectal can- 1443-1451
cer: a pooled analysis of two randomized trials. J Clin Oncol 18 Ruers T, Punt CJ, van Coevorden F, Borel Rinkes I, Leder-
2008; 26: 4906-4911 mann JA, Poston GJ, Bechstein W, Lentz M, Mauer M,
4 Power DG, Kemeny NE. Role of adjuvant therapy after re- Nordlinger B. Final results of the EORTC randomized study
section of colorectal cancer liver metastases. J Clin Oncol 2010; 40004 (CLOCC) evaluating the benefit of radiofrequency ab-
28: 2300-2309 lation (RFA) combined with chemotherapy for unresectable
5 Van Cutsem E, Köhne CH, Hitre E, Zaluski J, Chang Chien colorectal liver metastases (CRC LM). J Clin Oncol 2010; 28:
CR, Makhson A, D'Haens G, Pintér T, Lim R, Bodoky G, 15s, (supply; abstract 3526)
Roh JK, Folprecht G, Ruff P, Stroh C, Tejpar S, Schlichting M, 19 Machi J, Oishi AJ, Sumida K, Sakamoto K, Furumoto NL,
Nippgen J, Rougier P. Cetuximab and chemotherapy as ini- Oishi RH, Kylstra JW. Long-term outcome of radiofrequency
tial treatment for metastatic colorectal cancer. N Engl J Med ablation for unresectable liver metastases from colorectal can-
2009; 360: 1408-1417 cer: evaluation of prognostic factors and effectiveness in first-
WJGO|www.wjgnet.com 65 April 15, 2011|Volume 3|Issue 4|
Sgouros J et al . Chemotherapy and radiofrequency ablation in colorectal liver metastases
and second-line management. Cancer J 2006; 12: 318-326 2001; 221: 159-166
20 Siperstein A, Garland A, Engle K, Rogers S, Berber E, Fo- 22 Liu CH, Arellano RS, Uppot RN, Samir AE, Gervais DA,
routani A, String A, Ryan T, Ituarte P. Local recurrence after Mueller PR. Radiofrequency ablation of hepatic tumours:
laparoscopic radiofrequency thermal ablation of hepatic effect of post-ablation margin on local tumour progression.
tumors. Ann Surg Oncol 2000; 7: 106-113 Eur Radiol 2010; 20: 877-885
21 Solbiati L, Livraghi T, Goldberg SN, Ierace T, Meloni F, 23 Mulier S, Ni Y, Jamart J, Ruers T, Marchal G, Michel L. Local
Dellanoce M, Cova L, Halpern EF, Gazelle GS. Percutane- recurrence after hepatic radiofrequency coagulation: multi-
ous radio-frequency ablation of hepatic metastases from variate meta-analysis and review of contributing factors. Ann
colorectal cancer: long-term results in 117 patients. Radiology Surg 2005; 242: 158-171
S- Editor Wang JL L- Editor Hughes D E- Editor Ma WH
WJGO|www.wjgnet.com 66 April 15, 2011|Volume 3|Issue 4|
You might also like
- Radiotherapy of Liver CancerFrom EverandRadiotherapy of Liver CancerJinsil SeongNo ratings yet
- P1 Functional Outcomes and Health-Related QualityDocument11 pagesP1 Functional Outcomes and Health-Related Qualityernitaranterupang79No ratings yet
- Role For Locoregional Therapies For Non-Colorectal Gastrointestinal MalignanciesDocument18 pagesRole For Locoregional Therapies For Non-Colorectal Gastrointestinal MalignanciesDR. SUMANTRA RAYNo ratings yet
- FLOT 3 QuimioterapiaDocument8 pagesFLOT 3 Quimioterapiaerica corral corralNo ratings yet
- Magic TrailDocument10 pagesMagic Trailchootu509No ratings yet
- RT Urothelial Carcinomas Radu MitricaDocument37 pagesRT Urothelial Carcinomas Radu MitricaStirNo ratings yet
- Debiri 1Document12 pagesDebiri 1paquidermo85No ratings yet
- Cytoreductive Surgery and IntraperitonealDocument11 pagesCytoreductive Surgery and IntraperitonealJorge FallasNo ratings yet
- A Case of Simultaneous Resection of Recurrent Colorectal Liver Metastases As Part of Colorectal Cancer Treatment JourneyDocument4 pagesA Case of Simultaneous Resection of Recurrent Colorectal Liver Metastases As Part of Colorectal Cancer Treatment JourneyAthenaeum Scientific PublishersNo ratings yet
- Leijssen 2018Document10 pagesLeijssen 2018Luis Angel Garcia RuizNo ratings yet
- s13014 015 0495 4Document6 pagess13014 015 0495 4produxing 101No ratings yet
- 01 HepatogastroDocument3 pages01 Hepatogastroyacine26No ratings yet
- Annals Case Reports PDF Final Final.25.05.l22.Document13 pagesAnnals Case Reports PDF Final Final.25.05.l22.rossbar13No ratings yet
- Hepatectomy Versus Stereotactic Body Radiotherapy For Primary Early Hepatocellular Carcinoma A Propensity-Matched Analysis in A Single InstitutionDocument8 pagesHepatectomy Versus Stereotactic Body Radiotherapy For Primary Early Hepatocellular Carcinoma A Propensity-Matched Analysis in A Single Institutiondongjun daiNo ratings yet
- Simultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDocument8 pagesSimultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDr Shiv ChopraNo ratings yet
- JCO 2003 Lin 631 7Document7 pagesJCO 2003 Lin 631 7Adhika Manggala DharmaNo ratings yet
- Nej Mo A 1414882Document9 pagesNej Mo A 1414882Corina Hagiu-RaduNo ratings yet
- Short-Term Surgical and Long-Term Survival Outcomes After Laparoscopic Distal Gastrectomy With D Lymphadenectomy For Gastric CancerDocument7 pagesShort-Term Surgical and Long-Term Survival Outcomes After Laparoscopic Distal Gastrectomy With D Lymphadenectomy For Gastric CancerThế VũNo ratings yet
- Standard surgical procedures and adjuvant therapies for colon cancerDocument46 pagesStandard surgical procedures and adjuvant therapies for colon cancerNadia Iriana DewiNo ratings yet
- A Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerDocument9 pagesA Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerFarizka Dwinda HNo ratings yet
- 2018 Article 6554Document8 pages2018 Article 6554Raíla SoaresNo ratings yet
- Early Detection and Treatment Advances in Primary Liver CancerDocument4 pagesEarly Detection and Treatment Advances in Primary Liver CancerMaria Magdalena Garcia CortesNo ratings yet
- Clinical Outcomes of Laparoscopic Surgery For Transverse and Descending Colon Cancers in A Community SettingDocument6 pagesClinical Outcomes of Laparoscopic Surgery For Transverse and Descending Colon Cancers in A Community SettingpingusNo ratings yet
- Koay 2020Document30 pagesKoay 2020Laura QuirozNo ratings yet
- 2021 Consolidation Theraphy in Esophageal CancerDocument6 pages2021 Consolidation Theraphy in Esophageal CancerykommNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptTera LeverenzNo ratings yet
- Prognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentDocument7 pagesPrognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentChairul Nurdin AzaliNo ratings yet
- CD006039 AbstractDocument3 pagesCD006039 AbstractHeppyMeiNo ratings yet
- Posthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)Document12 pagesPosthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)drsubramanianNo ratings yet
- Pathological complete response in recurrent colon cancer following neoadjuvant radiotherapy and intraperitoneal chemotherapyDocument4 pagesPathological complete response in recurrent colon cancer following neoadjuvant radiotherapy and intraperitoneal chemotherapyAlice AugustinNo ratings yet
- SD Article 3Document6 pagesSD Article 3bogdanotiNo ratings yet
- Meta 4 - de Jong DM - 2022Document13 pagesMeta 4 - de Jong DM - 2022matheus.verasNo ratings yet
- Meta 6 - Khizar - 2023Document11 pagesMeta 6 - Khizar - 2023matheus.verasNo ratings yet
- Bridget N. Fahy, MD, William R. Jarnagin, MD: Ó 2006 Elsevier Inc. All Rights ReservedDocument18 pagesBridget N. Fahy, MD, William R. Jarnagin, MD: Ó 2006 Elsevier Inc. All Rights ReservedprivedNo ratings yet
- Intergroup 0123Document8 pagesIntergroup 0123radonc17No ratings yet
- Gastric Ca With Peritoneal CarcinomatosisDocument11 pagesGastric Ca With Peritoneal Carcinomatosispaolo gasconNo ratings yet
- Glockzin - 2012 - Surgical Oncology Clinics of North AmericaDocument9 pagesGlockzin - 2012 - Surgical Oncology Clinics of North AmericaPraveen RavishankaranNo ratings yet
- Article - Laparoscopic Versus Open Surgery For Rectal Cancer (COLOR II) - Short-Term Outcomes of A Randomised, Phase 3 Trial - 2013Document9 pagesArticle - Laparoscopic Versus Open Surgery For Rectal Cancer (COLOR II) - Short-Term Outcomes of A Randomised, Phase 3 Trial - 2013Trí Cương NguyễnNo ratings yet
- 1 s2.0 S101595841730622X MainDocument7 pages1 s2.0 S101595841730622X Mainyerich septaNo ratings yet
- UreterostomiiDocument7 pagesUreterostomiivlad910No ratings yet
- Livsey 2003Document6 pagesLivsey 2003Migue PerezNo ratings yet
- BiomedJ382173-2563889 070718 PDFDocument4 pagesBiomedJ382173-2563889 070718 PDFgrigmihNo ratings yet
- Survival After Lung Metastasectomy in Colorectal Cancer Patients With Previously Resected Liver MetastasesDocument6 pagesSurvival After Lung Metastasectomy in Colorectal Cancer Patients With Previously Resected Liver MetastasesNurul Dwi UtamiNo ratings yet
- ARTIGO 4 - A Prospective Clinical Trial On Sorafenib Treatment of Hepatocellular Carcinoma Before Liver TransplantationDocument11 pagesARTIGO 4 - A Prospective Clinical Trial On Sorafenib Treatment of Hepatocellular Carcinoma Before Liver TransplantationHenderson NobreNo ratings yet
- Early Recurrence of Carcinoma Gall Bladder After R0 Resection of Stage T1B-T3Document6 pagesEarly Recurrence of Carcinoma Gall Bladder After R0 Resection of Stage T1B-T3IJAR JOURNALNo ratings yet
- The Comparison of Surgery and Chemo-Radio Therapy in Locally Recurrent Colorectal CancerDocument4 pagesThe Comparison of Surgery and Chemo-Radio Therapy in Locally Recurrent Colorectal CancerInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Phase I Trial of Stereotactic Body Radiation TherapyDocument8 pagesA Phase I Trial of Stereotactic Body Radiation TherapyRaul Matute MartinNo ratings yet
- Ha Tace For MMLM 2008Document6 pagesHa Tace For MMLM 2008grigmihNo ratings yet
- Outcomes Following Different Thermal Ablation Strategies in Patients With Unresectable Colorectal Liver MetastaseDocument9 pagesOutcomes Following Different Thermal Ablation Strategies in Patients With Unresectable Colorectal Liver MetastaseNachchakorn DellNo ratings yet
- Algoritma Kanker KolorektalDocument8 pagesAlgoritma Kanker KolorektalHasan NyambeNo ratings yet
- Nejmoa 0908721Document9 pagesNejmoa 0908721Gustavo BraccoNo ratings yet
- ALLPS SurgeryDocument10 pagesALLPS SurgeryAndres Neira QuezadaNo ratings yet
- Shindoh 2013Document8 pagesShindoh 2013Nikos SerifisNo ratings yet
- Guest Editorial Building On A Consensus: Journal of Surgical Oncology 2008 98:215-216Document91 pagesGuest Editorial Building On A Consensus: Journal of Surgical Oncology 2008 98:215-216Madarasz ZsoltNo ratings yet
- FULLTEXT01 BP SwedenDocument74 pagesFULLTEXT01 BP SwedenGor AdanNo ratings yet
- Adjuvant Versus Salvage Radiotherapy Following Radical Prostatectomy: Do The AUA/ASTRO Guidelines Have All The Answers?Document6 pagesAdjuvant Versus Salvage Radiotherapy Following Radical Prostatectomy: Do The AUA/ASTRO Guidelines Have All The Answers?Anonymous jBoDXi3sNo ratings yet
- Preoperative and Adjuvant Therapies For Upper Gastrointestinal CancersDocument7 pagesPreoperative and Adjuvant Therapies For Upper Gastrointestinal Cancersajaymanvikar007No ratings yet
- Resection of The Primary Colorectal CancDocument7 pagesResection of The Primary Colorectal CancjorgehogNo ratings yet
- View ContentDocument24 pagesView ContentDian AyuNo ratings yet
- Metastatic Pancreatic Carcinoid Causing Gastric ObstructionDocument10 pagesMetastatic Pancreatic Carcinoid Causing Gastric ObstructionMohamed HadzriNo ratings yet
- 1 s2.0 S1051044306000066 MainDocument7 pages1 s2.0 S1051044306000066 MainHaya RihanNo ratings yet
- Transarterial Iodine 131Document7 pagesTransarterial Iodine 131Haya RihanNo ratings yet
- Document 1Document10 pagesDocument 1Haya RihanNo ratings yet
- FTPDocument5 pagesFTPHaya RihanNo ratings yet
- User 'S Manual: 2014-06 GTUM-001 (Rev. 1)Document94 pagesUser 'S Manual: 2014-06 GTUM-001 (Rev. 1)Haya RihanNo ratings yet
- Drug Mechanism of Action Indication Nursing ResponsibilitiesDocument5 pagesDrug Mechanism of Action Indication Nursing ResponsibilitiesShara SampangNo ratings yet
- 2008Document46 pages2008jimmyNo ratings yet
- 2019 - 2020 - Boston Immunization - Hult Immunization FormDocument4 pages2019 - 2020 - Boston Immunization - Hult Immunization FormOscar RomainvilleNo ratings yet
- Cerebral Palsy PDFDocument6 pagesCerebral Palsy PDFprasadNo ratings yet
- Fall Risk Factors For The Learner 1Document13 pagesFall Risk Factors For The Learner 1StokleyCNo ratings yet
- Herbal Cancer Treatment - Sabah Snake GrassDocument6 pagesHerbal Cancer Treatment - Sabah Snake GrassGelo Joson100% (2)
- Untitled 5 PDFDocument6 pagesUntitled 5 PDFDeepak saxenaNo ratings yet
- Brochura UrgoTul AGDocument4 pagesBrochura UrgoTul AGDaniguedesNo ratings yet
- Oral Manifestations of Systemic DiseasesDocument25 pagesOral Manifestations of Systemic Diseasesmicheal1960No ratings yet
- Geriatrics Trauma Power Point Presentation Dr. BarbaDocument23 pagesGeriatrics Trauma Power Point Presentation Dr. BarbagiscaamiliaNo ratings yet
- Doh 1Document3 pagesDoh 1Fitz Dyan TorresNo ratings yet
- Local Anesthetic Systemic Complications and TreatmentDocument35 pagesLocal Anesthetic Systemic Complications and Treatmentsatya_mdsNo ratings yet
- (Pediaii) - 021 - Disorders of The Respiratory TractDocument17 pages(Pediaii) - 021 - Disorders of The Respiratory TractdoktoraronaNo ratings yet
- Firs World Report PDFDocument35 pagesFirs World Report PDFMarv MarvNo ratings yet
- Pharmaceutical Dosage Forms, Drug Delivery Systems and Medical DevicesDocument28 pagesPharmaceutical Dosage Forms, Drug Delivery Systems and Medical Devices陳欣瑩No ratings yet
- A Modified Acid-Fast Staining Method For Rapid Detection ofDocument5 pagesA Modified Acid-Fast Staining Method For Rapid Detection ofWan HafizNo ratings yet
- Step 2 CK (CCSSA) Form 6Document51 pagesStep 2 CK (CCSSA) Form 6Appu ayyalaNo ratings yet
- Bilirubin Metabolism: Hd. - Msc. (Biochemistry)Document18 pagesBilirubin Metabolism: Hd. - Msc. (Biochemistry)MuhamadMarufNo ratings yet
- Tubo Ovarian AbscessDocument18 pagesTubo Ovarian AbscessSyarifah Maharani HidayatNo ratings yet
- Clinical RotationDocument2 pagesClinical RotationDarwin QuirimitNo ratings yet
- STEAM INHALATION and NEBULIZATIONDocument4 pagesSTEAM INHALATION and NEBULIZATIONRenzo GabrielNo ratings yet
- Turkey Position PaperDocument3 pagesTurkey Position PaperBill GatesNo ratings yet
- Donning and Removing Sterile Gloves (Open Method) Preparation RationaleDocument2 pagesDonning and Removing Sterile Gloves (Open Method) Preparation RationalecharmainchavezNo ratings yet
- Cervical Cancer: The Silent KillerDocument19 pagesCervical Cancer: The Silent KillerDennis CosmodNo ratings yet
- Renal Ultrasound ProtocolDocument4 pagesRenal Ultrasound Protocolfouad tabetNo ratings yet
- Flower EsscencesDocument2 pagesFlower EsscencesDivyajyoti DevaNo ratings yet
- Mifepristone & MisoprostolDocument6 pagesMifepristone & MisoprostolnanimadallaNo ratings yet
- Cornea PDFDocument465 pagesCornea PDFputraNo ratings yet
- 离子电渗皮肤给药系统Document9 pages离子电渗皮肤给药系统wannitan5No ratings yet
- Clinical Case NobelReplace Conical Connection Alessandro PozziDocument8 pagesClinical Case NobelReplace Conical Connection Alessandro PozziShyam BhatNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)