Professional Documents
Culture Documents
Doxy VS Azit For Chlamydia
Uploaded by
Kane Aldrich C. CONDINOOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Doxy VS Azit For Chlamydia
Uploaded by
Kane Aldrich C. CONDINOCopyright:
Available Formats
Clinical Infectious Diseases
Major Article
Doxycycline Versus Azithromycin for the Treatment of
Rectal Chlamydia in Men Who Have Sex With Men:
A Randomized Controlled Trial
Julia C. Dombrowski,1,2 Michael R. Wierzbicki,3 Lori M. Newman,4 Jonathan A. Powell,3 Ashley Miller,5 Dwyn Dithmer,2 Olusegun O. Soge,6 and
Kenneth H. Mayer7,8
1
Department of Medicine, University of Washington, Seattle, Washington, USA; 2HIV/STD Program, Public Health—Seattle & King County, Seattle, Washington, USA; 3The Emmes Company, LLC,
Rockville, Maryland, USA; 4Division of Microbiology and Infectious Diseases, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, Maryland, USA; 5FHI 360,
Durham, North Carolina, USA; 6Departments of Medicine and Global Health, University of Washington, Seattle, Washington, USA; 7Fenway Health, Boston, Massachusetts, USA; and 8Department
of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
Background. Azithromycin and doxycycline are both recommended treatments for rectal Chlamydia trachomatis (CT) infec-
tion, but observational studies suggest that doxycycline may be more effective.
Methods. This randomized, double-blind, placebo-controlled trial compared azithromycin (single 1-g dose) versus doxycy-
cline (100 mg twice daily for 7 days) for the treatment of rectal CT in men who have sex with men (MSM) in Seattle and Boston.
Participants were enrolled after a diagnosis of rectal CT in clinical care and underwent repeated collection of rectal swabs for nucleic
acid amplification testing (NAAT) at study enrollment and 2 weeks and 4 weeks postenrollment. The primary outcome was microbi-
ologic cure (CT-negative NAAT) at 4 weeks. The complete case (CC) population included participants with a CT-positive NAAT at
enrollment and a follow-up NAAT result; the intention-to-treat (ITT) population included all randomized participants.
Results. Among 177 participants enrolled, 135 (76%) met CC population criteria for the 4-week follow-up visit. Thirty-three partici-
pants (19%) were excluded because the CT NAAT repeated at enrollment was negative. Microbiologic cure was higher with doxycycline
than azithromycin in both the CC population (100% [70 of 70] vs 74% [48 of 65]; absolute difference, 26%; 95% confidence interval [CI],
16–36%; P < .001) and the ITT population (91% [80 of 88] vs 71% [63 of 89]; absolute difference, 20%; 95% CI, 9–31%; P < .001).
Conclusions. A 1-week course of doxycycline was significantly more effective than a single dose of azithromycin for the treat-
ment of rectal CT in MSM.
Clinical Trials Registration. NCT03608774.
Keywords. Chlamydia trachomatis; sexually transmitted diseases; rectal infection; sexual and gender minorities; therapeutics.
Incidence rates of sexually transmitted infections (STIs) among Rectal CT can lead to urethral CT infections in male partners
men who have sex with men (MSM) in the United States have [4] and increases the risk of HIV acquisition by approximately
risen substantially over the last decade [1]. Rectal Chlamydia 2-fold [5, 6]. Thus, effective detection and treatment of rectal
trachomatis (CT) is the most common bacterial STI among CT is central to chlamydia control among MSM and may con-
MSM [1, 2], but because it rarely causes symptoms, the infec- tribute to HIV prevention.
tion often remains undetected in the absence of extragenital Although the 2015 STI treatment guidelines from the Centers
screening. National surveillance data demonstrated 10–21% test for Disease Control and Prevention (CDC) recommend both
positivity for rectal CT among MSM in STI clinics in 2018 and doxycycline and azithromycin as first-line treatments for rectal
18% among MSM in human immunodeficiency virus (HIV) CT [7], retrospective studies suggest that doxycycline is more ef-
care in 2013–2014 [1, 3]. Among a nonclinical population of fective. A meta-analysis of 8 observational studies estimated the
asymptomatic MSM recruited in 5 cities, 7% had rectal CT [2]. efficacy of a 7-day course of doxycycline to be 99.6% (95% con-
fidence interval [CI], 98.6–100%) compared with 82.9% (76.0–
89.8%) for single-dose azithromycin [8]. However, the relative
effectiveness of these regimens remains uncertain without a
Received 23 October 2020; editorial decision 7 February 2021; published online 19 February prospective study. Definitive data are needed to inform clin-
2021.
Correspondence: J. C. Dombrowski, 325 Ninth Ave, Box 359777, Seattle, WA 98104 ical practice, particularly because many clinicians prefer to use
(jdombrow@uw.edu). azithromycin due to the simplicity of a single-dose regimen [9].
Clinical Infectious Diseases® 2021;73(5):824–31 We conducted a randomized controlled trial (RCT) of single-
© The Author(s) 2021. Published by Oxford University Press for the Infectious Diseases Society
of America. All rights reserved. For permissions, e-mail: journals.permissions@oup.com. dose azithromycin versus a 7-day course of doxycycline for the
DOI: 10.1093/cid/ciab153 treatment of rectal CT in MSM.
824 • cid 2021:73 (1 September) • Dombrowski et al
METHODS sex acts, condom use, lubricant use, and douching. Research
Study Design
staff observed participants taking the dose of azithromycin (or
The study was a randomized, double-blind, placebo-controlled placebo) plus 1 dose of doxycycline (or placebo) but did not
clinical trial among MSM with rectal CT detected by a nucleic otherwise provide adherence support. At follow-up visits, ad-
acid amplification test (NAAT) in clinical care. We randomized herence to the study medications was assessed by self-report
study participants to azithromycin (single 1-g oral dose) or dox- and, if available, pill count from returned study drug. We col-
ycycline (100 mg orally twice daily for 7 days) plus matching lected limited data on adverse events since the safety profile of
placebo. Participants repeated rectal swabs for CT NAAT at the both study medications is well documented.
time of study enrollment and 2 weeks and 4 weeks after enroll- Rectal swabs were collected by the study clinician or
ment. The study was conducted at the Public Health—Seattle & self-collected by participants in the clinic per clinic standard
King County Sexual Health Clinic in Seattle, Washington, and practice. In addition, after February 2019, participants could
Fenway Health in Boston, Massachusetts. mail in self-collected rectal swabs at the 2- and 4-week time
The primary outcome was the proportion of participants with points. Prior studies and CDC guidelines support the use of
patient-collected swabs as comparable to clinician-collected
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
microbiologic cure (CT-negative NAAT) in each study arm at 4
weeks (visit 3). Secondary outcomes included the proportion swabs for rectal CT diagnosis [7, 11–13]. Participants with a
of participants with microbiologic cure at 2 weeks and the pro- positive or indeterminate rectal CT NAAT result at the final
portion with microbiologic cure at 2 and 4 weeks stratified by study visit were notified by an unblinded clinician who ensured
infection with lymphogranuloma venereum (LGV) biovar CT. appropriate re-treatment. The NAAT results from the 2-week
Exploratory outcomes included the proportion of participants visit were not released during the study or used for clinical care.
with microbiologic cure in subgroups defined by HIV status,
Laboratory Methods
medication adherence, and rectal symptoms. We explored the
All laboratory testing was performed in the University of
impact of antacid and rectal lubricant or douche use on treat-
Washington (UW) Global Health STI Laboratory. CT NAAT
ment effectiveness based on the hypothesis that these might
was conducted using the Aptima Combo 2 Assay (Hologic, Inc,
alter the concentration of azithromycin in the rectum [10].
San Diego, CA, USA). All specimens positive for CT at the time
Population of study enrollment were tested using a validated LGV poly-
Eligible individuals were male sex at birth (inclusive of any merase chain reaction (PCR) [14].
gender identity), 18 years or older, had at least 1 male sex partner
in the past 12 months, and agreed to abstain from condomless Sample Size
receptive anal sex during the study. Participants were excluded The trial utilized a 2-staged group sequential design using
if they had a clinical diagnosis of acute proctitis [7], concom- O’Brien-Fleming boundaries with 1 semi-blinded interim anal-
itant untreated gonorrhea or primary or secondary syphilis, ysis of the primary outcome once half the target evaluable pop-
known allergy to tetracyclines or macrolide antibiotics, or had ulation had been enrolled with primary endpoint data and a
received antimicrobial therapy active against CT within 21 days stopping rule based on efficacy. An overall type I error rate of
of the positive rectal CT NAAT result or between the date of the 5% was set for the analyses. To determine the sample size, we
test and study enrollment. assumed a range of cure rates of doxycycline and azithromycin
consistent with published studies. A sample size of 246 parti-
Randomization and Blinding cipants would have more than 80% power to detect a 10% or
Participants were randomized to a treatment arm in a 1-to-1 greater difference across a range of cure rates. Anticipating 10%
ratio using site-stratified, permuted, blocked randomization. ineligibility for the primary analysis, the enrollment target was
Participants, clinical study staff, data entry personnel, and lab- 274 participants. We calculated the probability of stopping the
oratory personnel were blinded to treatment assignment. The trial at the interim analysis to be less than 1% if the cure pro-
study drug was provided in identical kits with overencapsulated portions were equal and 23% if cure proportions of doxycycline
pills and identical placebos containing lactose monohydrate. and azithromycin were 97% and 87%, respectively.
Study Visit Procedures Statistical Analysis
During the enrollment visit, clinicians assessed whether parti- The primary, secondary, and exploratory study outcomes were
cipants had rectal symptoms, such as discomfort, irritation, or analyzed in the complete case (CC) population, which included
itching; examined inguinal lymph nodes; collected information participants with a CT-positive NAAT at enrollment and at the
on HIV status and antiretroviral therapy or pre-exposure pro- corresponding follow-up time point. Additionally, we evaluated
phylaxis (PrEP); and collected information on sexual behavior the primary and secondary outcomes in the intention-to-treat
in the past 60 days, including partner number, anal and other (ITT) population, which included all enrolled participants,
Rectal Chlamydia Treatment Study • cid 2021:73 (1 September) • 825
and the per-protocol (PP) population, which included parti- Seventy six percent of enrolled participants (n = 135) met CC
cipants who met the CC population criteria and reported no population criteria at 4 weeks, and the most common exclusion
condomless anal intercourse or receipt of antibiotics effective reason (n = 33; 19% of all enrolled) was a negative result on
against CT during the study, sufficiently adhered to the study the CT NAAT repeated at enrollment. This proportion did not
medication, and completed a 4-week study visit in the specified differ substantially between the 2 study sites (17% and 21%).
time frame. In the absence of a defined minimally effective reg- Ninety-four participants were included in the PP population,
imen of doxycycline for the treatment of rectal CT, we defined with condomless receptive anal sex during the study being the
“sufficient adherence” a priori as completing the first doses of most common reason for exclusion from the PP population
study medication under observation and reporting at least 9 ad- among participants included in the CC population (n = 25; 19%
ditional doses of doxycycline/placebo within 10 days. of the CC population).
For the primary analysis comparing 4-week microbiologic The median age of participants was 34 years, and 95% iden-
cure outcomes in the 2 treatment groups in the CC population, tified as cisgender men (Table 1). Sixty-three percent were
a 2-sided Pearson chi-square test was used with significance White, 21% were Hispanic/Latino, 5% were Black, and 4% were
levels defined by the O’Brien-Fleming boundaries. To derive Asian or Pacific Islander. Over half of participants (54%) were
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
the P value, the point estimate, and CI for the difference in cure HIV-seronegative and taking HIV PrEP and 15% were HIV-
proportions, stage-wise ordering of the sample space was used seropositive. A minority had rectal symptoms (18%) or inguinal
[15]. The resulting P value, median unbiased estimate, and CI lymphadenopathy (4%).
are reported here. For the analyses of the 4-week and 2-week
outcomes in the ITT and PP populations, a significance level of Microbiologic Cure
5% was used. For ITT analyses, subjects with missing cure out- Microbiologic cure at 4 weeks was higher with doxycycline than
comes were classified as treatment failures and outcomes were azithromycin in all analysis populations (Table 2). In the CC
imputed as microbiologic failures. population, the cure proportion was 100% (95% CI, 90–100%)
For exploratory analyses, we conducted subgroup analyses of in the doxycycline arm versus 74% (95% CI, 56–86%) in the
the 4-week cure outcomes stratified by HIV status, LGV biovar azithromycin arm, with an absolute difference of 26% (95%
status, rectal symptoms (symptomatic or asymptomatic), adher- CI, 16–36%; P < .001). In the ITT population, the cure rate for
ence, and antacid medication use. Based on the high level of ef- doxycycline was 91% (95% CI, 83–95%) versus 71% (95% CI,
fectiveness in the doxycycline treatment group, we decided post 61–79%) for azithromycin (P < .001). Cases imputed as treat-
hoc to report the comparisons only within the azithromycin ment failures in the doxycycline group were driven by loss to
arm and excluded the adherence comparison. follow-up (n = 7); only 1 participant had a positive NAAT at
4 weeks.
Human Research Protections
At the 2-week follow-up visit, doxycycline was more effective
The study protocol was approved by Institutional Review than azithromycin in all analysis populations. The absolute dif-
Boards at the UW and Fenway Health. The study is regis- ference between doxycycline and azithromycin was 11% (95%
tered at ClinicalTrials.gov (NCT03608774). A Data and Safety CI, 0–22%) in the CC population, 7% (95% CI, −4 to 17%) in
Monitoring Board (DSMB) provided oversight, including re- the ITT population, and 15% (95% CI, 4–27%) in the PP popu-
view of data at specified times during the study for participant lation. Among participants who received doxycycline, the pro-
and overall study progress, semi-blinded interim analysis re- portion with microbiologic cure was lower at 2 weeks than at
sults, serious adverse events, and, at the conclusion of the trial, 4 weeks, but the opposite pattern was observed in participants
safety data. who received azithromycin (Figure 2). Among participants in
the CC population who received azithromycin, 8 of 56 (14%)
who had a negative NAAT at 2 weeks had a positive NAAT
RESULTS
again at 4 weeks.
Study Population The LGV PCR was positive in CT specimens from 8 parti-
Between July 2018 and February 2020, 177 participants were en- cipants (6% of the 4-week CC population). These were equally
rolled and randomized to doxycycline or azithromycin (Figure distributed between the study arms (n = 4 in each). Among par-
1). Enrollment ended after the DSMB recommended stopping ticipants in Seattle, 6 (6% of 104) had LGV-biovar infections
based on efficacy in accordance with the prespecified stopping versus 2 (3% of 73) in Boston. All participants with LGV-biovar
rule for the interim analysis. Enrolled subjects who were on- CT who received doxycycline had microbiologic cure at both
going follow-up at the time of the interim analysis were not in- 2 and 4 weeks, as did 3 of 4 (75%) who received azithromycin
cluded in the analysis provided to the DSMB. The data from (25% absolute difference; 95% CI, −.28 to .70). Among parti-
these subjects were incorporated in the analyses reported in this cipants with non-LGV CT biovars, the absolute difference be-
study [16, 17]. tween study arms was 26% (95% CI, .15–.38).
826 • cid 2021:73 (1 September) • Dombrowski et al
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
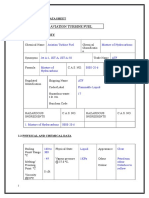
Figure 1. Study flow chart. Abbreviations: CC, complete case; CT, Chlamydia trachomatis; ITT, intention-to-treat; NAAT, nucleic acid amplification testing; PP, per
protocol.
Medication Adherence and Sexual Behavior Sexual behavior between enrollment and follow-up did not
In the CC population at 4 weeks, 131 of 135 participants (97%) differ between treatment assignment groups (Table 3). Overall,
met the definition of sufficient adherence to the 7-day course 75 participants (45% of those with follow-up data) reported
of doxycycline/placebo. Among 4 who reported insufficient ad- having receptive anal sex and 25 (14%) reported condomless
herence, 2 were randomized to each treatment, and all had mi- anal sex.
crobiologic cure at 4 weeks.
Rectal Chlamydia Treatment Study • cid 2021:73 (1 September) • 827
Table 1. Demographic and Baseline Clinical Characteristics of Participants
Doxycycline Azithromycin All Subjects
(n = 88)a (n = 89) (n = 177)
Gender, n (%)
Cisgender male 83 (94) 85 (96) 168 (95)
Transgender, nonbinary, other 4 (5) 4 (4) 8 (5)
Age, mean (SD), years 34 (12) 34 (11) 34 (11)
Race/ethnicity, n (%)
White 58 (66) 54 (61) 112 (63)
Black 5 (6) 3 (3) 8 (5)
Asian or Pacific Islander 13 (15) 12 (14) 25 (14)
American Indian or Alaska Native 1 (1) 1(1) 2 (1)
Multiracial 6 (7) 16 (18) 22 (12)
Missing 5 (6) 3 (3) 8 (5)
Ethnicity, n (%)
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
Hispanic or Latino 21 (24) 16 (18) 37 (21)
Not Hispanic or Latino 67 (76) 71 (80) 138 (78)
Unknown 0 2 (2) 2 (2)
HIV statusb; ART and PrEP status, n (%)
Positive, on ART 14 (16) 12 (14) 26 (15)
Positive, not on ART 0 0 0
Negative, on PrEP 44 (50) 52 (58) 96 (54)
Negative, not on PrEPc 29 (33) 22 (25) 51 (29)
Missing 1 (1) 3 (3) 4 (2)
Rectal symptoms,d n (%)
Yes 13 (15) 18 (20) 31 (18)
No 74 (84) 71 (80) 145 (82)
Inguinal lymphadenopathy,d n (%)
Yes 4 (5) 3 (3) 7 (4)
No 83 (94) 86 (97) 169 (95)
Abbreviations: ART, antiretroviral therapy; HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis.
a
One participant in the doxycycline group did not have baseline data available.
b
Based on participant self-report.
c
At baseline; 6 subjects started PrEP between study entry and follow-up visits.
d
Symptoms that met the clinical definition of proctitis were excluded.
HIV Status, Rectal Symptoms, and Antacid Medication Use rectal symptoms at baseline, 79% (95% CI, 52–92%) had cure
Among 8 HIV-seropositive participants randomized to with azithromycin compared with 73% (37 of 51; 95% CI,
azithromycin, all were cured at 4 weeks (100%; 95% CI, 59–83%) in those without symptoms. One participant in the
68–100%) compared with 70% (38 of 54; 95% CI, 57–81%) of azithromycin group who reported using antacid medication
HIV-seronegative participants. Among 14 participants with had a positive NAAT at 4 weeks.
Table 2. Microbiologic Cure at 4 Weeks, by Treatment Group, in Each Analysis Population
Complete Case Populationa Intent-to-Treat Populationb Per Protocol Populationc
Doxycycline Azithromycin Doxycycline Azithromycin Doxycycline Azithromycin
(n = 70) (n = 65) (n = 88) (n = 89) (n = 46) (n = 48)
Participants with microbiologic cure, n 70 48 80 63 46 37
Participants with microbiologic cure, % (95% CI) 100 (90–100) 74 (56–86) 91 (83–95) 71 (61–79) 100 (92- 100) 77 (63–87)
Difference in proportion, % 26 (16–36) 20 (9 – 31) 23 (11 – 37)
P value <.001 <.001 <.001
Abbreviations: CI, confidence interval; CT, Chlamydia trachomatis; NAAT, nucleic acid amplification testing.
a
Participants who had positive rectal CT NAAT at baseline and follow-up microbiologic data.
b
All enrolled participants.
c
Participants who had a positive rectal CT NAAT at baseline, follow-up microbiologic data, reported no condomless anal intercourse or receipt of antibiotics effective against CT during the
study, adhered sufficiently to study medication, and completed visit 3 within the time frame specified in the protocol.
828 • cid 2021:73 (1 September) • Dombrowski et al
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
Figure 2. Comparison of 2-week and 4-week cure percentage by treatment group and analysis population.
Safety and Tolerance DISCUSSION
One serious adverse event occurred, which was unrelated to the
In this randomized placebo-controlled trial, we found that a
study. Additionally, 1 participant assigned doxycycline and 2 as-
7-day course of doxycycline was significantly more effective
signed azithromycin reported vomiting the study medication, 1
than a single dose of azithromycin for the treatment of rectal
of whom (assigned azithromycin) terminated study participa-
CT in MSM, with point estimate cure proportions of 100% for
tion early.
Table 3. Follow-up Sexually Transmitted Infection and Sexual History by Treatment Group
All Subjects
Doxycycline Azithromycin (n = 177),
(n = 88), n (% of total) (n = 89), n (% of total) n (% of total)
Any STI since enrollment
No 84 (97) 85 (96) 169 (96)
Yes 3 (3) 4 (4) 7 (4)
Sexual behaviors during the study
Any receptive anal sex 37 (45) 38 (45) 75 (45)
Condomless receptive anal sex 15 (17) 10 (11) 25 (14)
Rimming 18 (22) 30 (35) 48 (29)
Fisting 2 (2) 4 (5) 6 (4)
Lubricant use during receptive anal sex
No 47 (57) 48 (56) 95 (57)
Yes 35 (43) 37 (44) 72 (43)
Silicone-based 20 (67)a 25 (76) 45 (71)
Water-based 17 (57) 12 (36) 29 (46)
Saliva 17 (57) 19 (58) 36 (57)
Ejaculate 4 (13) 4 (12) 8 (13)
Oil 3 (10) 3 (9) 6 (10)
Other/unknown 5 (17) 7 (21) 12 (19)
Rectal douches
No 52 (63) 52 (61) 104 (62)
Yes 30 (37) 33 (39) 63 (38)
Water 29 (97)a 32 (97) 61 (97)
Fleet enema 6 (20) 4 (12) 10 (16)
The denominator for percentages is the number of subjects with follow-up sexual history data. Abbreviation: STI, sexually transmitted infection.
a
The denominators for lubricant and douche types are the number of persons who reported using lubricants or douches, respectively.
Rectal Chlamydia Treatment Study • cid 2021:73 (1 September) • 829
doxycycline and 74% for azithromycin in the CC population and infections refutes the idea that LGV-biovar infections account
91% for doxycycline and 71% for azithromycin in the ITT popu- for the inadequacy of azithromycin.
lation. Only 1 of 88 participants randomized to doxycycline had Different host–microbe interactions in the rectal environ-
a positive NAAT at 4 weeks, with the remainder of noncures in ment than in the genital tract may alter the effect of azithromycin
the ITT population reflecting loss to follow-up. Although the on CT. The pattern of NAAT clearance we observed with
proportion of participants with microbiologic cure in the dox- azithromycin was the opposite of that expected with progres-
ycycline arm increased from 2 to 4 weeks postenrollment, the sive bacterial clearance. This is consistent with, but not proof of,
proportion with cure in the azithromycin arm decreased from recrudescent infection following a period of transient bacterial
2 to 4 weeks. Infection with LGV-biovar CT was uncommon. latency [23]. The positive-negative-positive pattern could also
Both treatments were safe and well tolerated. indicate reinfection, but this would not be expected to differ be-
Our main study finding confirms the results of previous tween arms in a placebo-blinded RCT nor do our behavioral
observational studies [8, 9]. However, the effectiveness of data suggest differential reinfection.
azithromycin in our study (74%; 95% CI, 56–86%) was even One reason that many clinicians prefer to use azithromycin
lower than estimated in pooled results of retrospective studies for CT treatment is concern about inadequate patient adher-
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
(83%; 95% CI, 76–90%) and well below the 95% threshold gen- ence to a week-long doxycycline regimen. Our study did not
erally considered acceptable for STI treatment. Our findings yield sufficient data to examine the impact of adherence, in
were comparable to those of a prospective study of women with part because we used generous parameters to define sufficient
CT, most of whom had concomitant rectal and urogenital in- adherence, but this concern should not be a barrier to using
fections, which found approximately 96% microbiologic cure doxycycline in practice. It is unlikely that imperfect adherence
with doxycycline and 79% with azithromycin at the rectum in a typical clinic population would negate the difference in ef-
[18]. Forthcoming results from an Australian study of rectal CT fectiveness between the 2 treatments. Moreover, some evidence
in MSM will add to the body of evidence on this topic [19]. suggests that doxycycline is effective even with imperfect adher-
Taken together, the existing studies conclusively demonstrate ence and at lower doses than typically used in the treatment of
that doxycycline is superior to azithromycin for the treatment genitourinary CT infections [24, 25].
of rectal CT. The limitations of our study include the number of parti-
Approximately 20% of the study participants had a nega- cipants with LGV-biovar infections, which was too small to
tive NAAT repeated at the enrollment visit after a recent pos- draw conclusions about the effectiveness of either regimen for
itive NAAT in clinical care. This could be due to participants the treatment of LGV-biovar CT. Our study population was
receiving antibiotics outside of the study, false-positive tests in almost entirely cisgender male, and the relevance of our find-
the clinic or false-negative tests at study entry, or spontaneous ings for transgender people and women with rectal CT is un-
clearance. In the absence of treatment, rectal CT infection can certain. We studied only 2 regimens and were thus unable to
last for weeks to months, but the duration of infection varies judge the impact of alternate dosing of azithromycin, such as
widely between individuals [20]. The natural history of CT in- the weekly 3-dose regimen recommended by the World Health
fection is not well understood and is an important topic for fu- Organization for the treatment of LGV [26].
ture research. In summary, this study demonstrated that a 7-day course
The mechanism of azithromycin treatment failure in rectal of doxycycline is substantially more effective than single-dose
CT is not known but is not likely due to antibiotic resistance, azithromycin for the treatment of rectal CT. Azithromycin per-
inadequate tissue penetration of the drug, or the prevalence formed so poorly that, even in the context of expected imperfect
of LGV biovars. Azithromycin resistance among CT has never adherence in real-world use, doxycycline should be the recom-
been conclusively demonstrated, and 1 prior report of re- mended treatment for rectal CT in MSM.
sistance was refuted with additional laboratory testing [21].
Notes
A pharmacokinetic study demonstrated that drug concentra-
Acknowledgments. The authors thank the individuals who participated in
tions of azithromycin in rectal tissue after a single azithromycin this study and the study staff who contributed to it. The authors specifically
dose remain above the minimum inhibitory concentration for acknowledge Melinda Tibbals at the National Institutes of Health; Angela
CT for at least 14 days [10]. Animal studies have also shown LeClair, Rushlenne Pascual, Tamara Bass, Laura Rishel, and Jennifer Morgan
at the University of Washington; Mo Drucker and Valerie Rugulo at Fenway
that azithromycin is ineffective in treating gastrointestinal CT
Health; Martine Policard, Aditi Sharma, Keven Huang, Logan Richlak, and
infections, even though it is effective for genital infections, de- Bruno Dos Santos at Emmes; Ginger Pittman and Linda McNeil at FHI
spite comparable drug levels in both anatomic tracts [22]. Our 360; Drs Jeanne Marrazzo and Edward Hook at the University of Alabama,
finding that LGV-biovar CT was uncommon in the study pop- Birmingham (UAB); the scientific review committee members of the UAB
Sexually Transmitted Infections Clinical Trials Group; Dr Timothy Menza,
ulation and that azithromycin was substantially less effective currently with the Oregon State Department of Health; and the San Francisco
than doxycycline for the treatment of non–LGV-biovar CT Department of Public Health Laboratory for technical assistance.
830 • cid 2021:73 (1 September) • Dombrowski et al
Financial support. This work was supported by the National Institutes Neisseria gonorrhoeae in men who have sex with men and women. Sex Transm
of Health (National Institute of Allergy and Infectious Diseases contract Dis 2009; 36:493–7.
HHSN272201300014I, protocol 17–0092). 12. Sexton ME, Baker JJ, Nakagawa K, et al. How reliable is self-testing for gonorrhea
and chlamydia among men who have sex with men? J Fam Pract 2013; 62:70–8.
Potential conflicts of interest. O. O. S. has participated in research sup-
13. Dodge B, Van Der Pol B, Reece M, et al. Rectal self-sampling in non-clinical
ported by grants to the University of Washington from Hologic, Inc, and
venues for detection of sexually transmissible infections among behaviourally bi-
SpeeDx, Inc. J. C. D. has participated in research funded by grants to the sexual men. Sex Health 2012; 9:190–1.
University of Washington from Hologic, Inc. All other authors report no po- 14. Siedner MJ, Pandori M, Leon SR, et al.; NIMH Collaborative HIV/STD Prevention
tential conflicts. All authors have submitted the ICMJE Form for Disclosure Trial Group. Facilitating lymphogranuloma venereum surveillance with the use of
of Potential Conflicts of Interest. Conflicts that the editors consider relevant real time polymerase chain reaction. Int J STD AIDS 2007; 18:506–7.
to the content of the manuscript have been disclosed. 15. Jennison C, Turnbull BW. Group sequential methods with applications to clinical
trials. Boca Raton, FL: Chapman & Hall, 2000.
16. Whitehead J. Overrunning and underrunning in sequential clinical trials. Control
References Clin Trials 1992; 13:106–21.
1. Centers for Disease Control and Prevention. Sexually transmitted disease sur- 17. Sooriyarachchi MR, Whitehead J, Matsushita T, Bolland K, Whitehead A.
veillance 2018. 2019. Available at: https://www.cdc.gov/std/stats18/default.htm. Incorporating data received after a sequential trial has stopped into the final anal-
Accessed 21 September 2020. ysis: implementation and comparison of methods. Biometrics 2003; 59:701–9.
2. Johnson Jones ML, Chapin-Bardales J, Bizune D, et al. Extragenital chlamydia 18. Dukers-Muijrers NHTM, Wolffs PFG, De Vries H, et al. Treatment effectiveness
and gonorrhea among community venue-attending men who have sex with of azithromycin and doxycycline in uncomplicated rectal and vaginal chlamydia
men—five cities, United States, 2017. MMWR Morb Mortal Wkly Rep 2019; trachomatis infections in women: a multicenter observational study (FemCure).
Downloaded from https://academic.oup.com/cid/article/73/5/824/6144986 by guest on 30 January 2024
68:321–325. Clin Infect Dis 2019; 69:1946–54.
3. Patel MR, Brooks JT, Tie Y, Garg S, Bradley H. Prevalence of gonorrhea and chla- 19. Lau A, Kong F, Fairley CK, et al. Treatment efficacy of azithromycin 1 g single
mydia testing by anatomical site among men who have sex with men in HIV dose versus doxycycline 100 mg twice daily for 7 days for the treatment of rectal
Medical care, United States, 2013–2014. Sex Transm Dis 2017; 45:25–27. chlamydia among men who have sex with men—a double-blind randomised con-
4. Chambers LC, Morgan JL, Lowens MS, et al. Cross-sectional study of urethral trolled trial protocol. BMC Infect Dis 2017; 17:35.
exposures at last sexual episode associated with non-gonococcal urethritis among 20. Chow EP, Camilleri S, Ward C, et al. Duration of gonorrhoea and chlamydia in-
STD clinic patients. Sex Transm Infect 2019; 95:212–8. fection at the pharynx and rectum among men who have sex with men: a system-
5. Barbee LA, Khosropour CM, Dombrowksi JC, Golden MR. New human immu- atic review. Sex Health 2016; 13:199–204.
nodeficiency virus diagnosis independently associated with rectal gonorrhea and 21. Suchland RJ, Geisler WM, Stamm WE. Methodologies and cell lines used for anti-
chlamydia in men who have sex with men. Sex Transm Dis 2017; 44:385–9. microbial susceptibility testing of Chlamydia spp. Antimicrob Agents Chemother
6. Jones J, Weiss K, Mermin J, et al. Proportion of incident human immunodefi- 2003; 47:636–42.
ciency virus cases among men who have sex with men attributable to gonorrhea 22. Yeruva L, Melnyk S, Spencer N, Bowlin A, Rank RG. Differential susceptibilities
and chlamydia: a modeling analysis. Sex Transm Dis 2019; 46:357–63. to azithromycin treatment of chlamydial infection in the gastrointestinal tract and
7. Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually cervix. Antimicrob Agents Chemother 2013; 57:6290–4.
transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 23. Lewis ME, Belland RJ, AbdelRahman YM, et al. Morphologic and molecular eval-
64:1–137. uation of Chlamydia trachomatis growth in human endocervix reveals distinct
8. Kong FY, Tabrizi SN, Fairley CK, et al. The efficacy of azithromycin and doxy- growth patterns. Front Cell Infect Microbiol 2014; 4:71.
cycline for the treatment of rectal chlamydia infection: a systematic review and 24. Bachmann LH, Stephens J, Richey CM, Hook EW 3rd. Measured versus self-reported
meta-analysis. J Antimicrob Chemother 2015; 70:1290–7. compliance with doxycycline therapy for chlamydia-associated syndromes: high ther-
9. Khosropour CM, Dombrowski JC, Barbee LA, Manhart LE, Golden MR. apeutic success rates despite poor compliance. Sex Transm Dis 1999; 26:272–8.
Comparing azithromycin and doxycycline for the treatment of rectal chlamydial 25. Lau CY, Qureshi AK. Azithromycin versus doxycycline for genital chlamydial
infection: a retrospective cohort study. Sex Transm Dis 2014; 41:79–85. infections: a meta-analysis of randomized clinical trials. Sex Transm Dis 2002;
10. Kong FY, Rupasinghe TW, Simpson JA, et al. Pharmacokinetics of a single 1g dose 29:497–502.
of azithromycin in rectal tissue in men. PLoS One 2017; 12:e0174372. 26. World Health Organization. WHO guidelines for the treatment of chlamydia
11. van der Helm JJ, Hoebe CJ, van Rooijen MS, et al. High performance and accept- trachomatis. 2016. Available at: https://www.who.int/reproductivehealth/publi-
ability of self-collected rectal swabs for diagnosis of Chlamydia trachomatis and cations/rtis/chlamydia-treatment-guidelines/en/. Accessed 21 September 2020.
Rectal Chlamydia Treatment Study • cid 2021:73 (1 September) • 831
You might also like
- Principles of Pharmacology - The Pathophysiologic Basis of Drug TherapyDocument978 pagesPrinciples of Pharmacology - The Pathophysiologic Basis of Drug TherapyChemistix100% (4)
- Randy WolfeilDocument1 pageRandy WolfeilJillian Lee NadiakNo ratings yet
- Cp-Acpj210021 737..747Document11 pagesCp-Acpj210021 737..747Luis Genaro Garcia AyalaNo ratings yet
- Articles: BackgroundDocument12 pagesArticles: BackgroundCésar Aguirre RomeroNo ratings yet
- A Comparative Study On The Treatment of Cervical Carcinoma by Radiotherapy Alone vs. Radiotherapy WiDocument13 pagesA Comparative Study On The Treatment of Cervical Carcinoma by Radiotherapy Alone vs. Radiotherapy WiIJRASETPublicationsNo ratings yet
- Topical Antibiotics To Prevent Surgical Site Infection After Minor Surgery in Primary CareDocument5 pagesTopical Antibiotics To Prevent Surgical Site Infection After Minor Surgery in Primary CarePitchya WangmeesriNo ratings yet
- Lefamulin SSTIDocument11 pagesLefamulin SSTIashikNo ratings yet
- MedicineDocument5 pagesMedicinepriyanka hermawanNo ratings yet
- Glaser 2017Document7 pagesGlaser 2017Dicky StefanusNo ratings yet
- A Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in AdultsDocument4 pagesA Randomized Controlled Trial of Probiotics For Clostridium Dif Cile Infection in Adults林新中No ratings yet
- Jurnal Interna UTIDocument8 pagesJurnal Interna UTIErdika Satria WahyuonoNo ratings yet
- Doxorubicin 3Document7 pagesDoxorubicin 3Afrian RahmandaNo ratings yet
- Content ServerDocument10 pagesContent ServerAgung WpNo ratings yet
- Neoadjuvant Chemotherapy Vs Upfront Surgery For Gastric Signet Ring Cell Carcinoma A Retrospective, Propensity Score-Matched StudyDocument11 pagesNeoadjuvant Chemotherapy Vs Upfront Surgery For Gastric Signet Ring Cell Carcinoma A Retrospective, Propensity Score-Matched StudyLITTLESWEETKILLERNo ratings yet
- Pristinamycin in Neisseria Gonorrhoeae - BMC Infectious Diseases 2022 (Liu)Document8 pagesPristinamycin in Neisseria Gonorrhoeae - BMC Infectious Diseases 2022 (Liu)Erick CoNo ratings yet
- Comparative Effectiveness of Digital Breast Tomosynthesis For Breast Cancer Screening Among Women 40-64 Years OldDocument8 pagesComparative Effectiveness of Digital Breast Tomosynthesis For Breast Cancer Screening Among Women 40-64 Years OldAmalia fhyNo ratings yet
- Medi 95 E4797Document5 pagesMedi 95 E4797tika apriliaNo ratings yet
- آنتی بیوتیک و آپاندیسDocument4 pagesآنتی بیوتیک و آپاندیسmohammad attarzadehNo ratings yet
- Civ 609Document17 pagesCiv 609Descargar scribdNo ratings yet
- PIIS2214109X20305052Document15 pagesPIIS2214109X20305052Ahsan RaquibNo ratings yet
- Journal BEDAHDocument40 pagesJournal BEDAHmeitikaNo ratings yet
- Ciz 1197Document8 pagesCiz 1197Lindia PrabhaswariNo ratings yet
- Djaa 048Document17 pagesDjaa 048Satra Azmia HerlandaNo ratings yet
- Articulo 2021 - EfectosDocument5 pagesArticulo 2021 - Efectosmilena cedeñoNo ratings yet
- A New Point-Of-Care Test For The Rapid Detection of Urinary Tract InfectionsDocument8 pagesA New Point-Of-Care Test For The Rapid Detection of Urinary Tract InfectionsAntika CahyatiNo ratings yet
- CANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan TangDocument7 pagesCANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan Tangalexmou2008No ratings yet
- Multi-Institutional External Validation of Urinary TWIST1 and NID2 Methylation As A Diagnostic Test For Bladder CancerDocument6 pagesMulti-Institutional External Validation of Urinary TWIST1 and NID2 Methylation As A Diagnostic Test For Bladder CancerFarlinda AlyaNo ratings yet
- Cancer ScreeningDocument8 pagesCancer Screeninglakshminivas PingaliNo ratings yet
- Artículo 3Document7 pagesArtículo 3edunapedNo ratings yet
- 192 2020 Article 4501Document12 pages192 2020 Article 4501Juan Sebastian Martinez OvalleNo ratings yet
- Fmed 08 584813Document12 pagesFmed 08 584813Annisa SetyantiNo ratings yet
- Colorectal BundlesDocument16 pagesColorectal BundlesDamie ChaulaNo ratings yet
- Chinese Medical JoournalDocument10 pagesChinese Medical JoournalTejas DixitNo ratings yet
- Gutjnl 2020 321956.fullDocument9 pagesGutjnl 2020 321956.fullAnonymous UserNo ratings yet
- Antibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.HDocument2 pagesAntibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.Hchebonk13No ratings yet
- Muzii Et Al., 2020Document9 pagesMuzii Et Al., 2020Jonathan LucisNo ratings yet
- Vaginal Dose Is Associated With Toxicity in Image Guided Tandem Ring or Ovoid-Based BrachytherapyDocument7 pagesVaginal Dose Is Associated With Toxicity in Image Guided Tandem Ring or Ovoid-Based BrachytherapyFlor ZalazarNo ratings yet
- Jamainternal Bretthauer 2023 Oi 230055 1692040542.98105Document8 pagesJamainternal Bretthauer 2023 Oi 230055 1692040542.98105Flavio GuimaraesNo ratings yet
- Vaccines 10 01370Document16 pagesVaccines 10 01370Tamanash ChowdharyNo ratings yet
- The Efficacy of Daily Chlorhexidine Bathing For Preventing Healthcare-Associated Infections in Adult Intensive Care UnitsDocument12 pagesThe Efficacy of Daily Chlorhexidine Bathing For Preventing Healthcare-Associated Infections in Adult Intensive Care UnitsKanameMizumiNo ratings yet
- Precision Medicine in Pediatric Oncology: ReviewDocument8 pagesPrecision Medicine in Pediatric Oncology: ReviewCiocan AlexandraNo ratings yet
- A Systematic Literature Review of The Efficacy, Effectiveness, and Safety of FilgrastimDocument14 pagesA Systematic Literature Review of The Efficacy, Effectiveness, and Safety of FilgrastimNo NameNo ratings yet
- Perspectives On Advances in Tuberculosis Diagnostics, Drugs, and VaccinesDocument17 pagesPerspectives On Advances in Tuberculosis Diagnostics, Drugs, and Vaccinesyenny handayani sihiteNo ratings yet
- Urinalisa 2Document10 pagesUrinalisa 2Minggus skilNo ratings yet
- Implementing An Antibiotic Stewardship Program Guidelines by The Infectious Diseases Society of America and The Society For Healthcare Epidemiology of AmericaDocument27 pagesImplementing An Antibiotic Stewardship Program Guidelines by The Infectious Diseases Society of America and The Society For Healthcare Epidemiology of AmericaEnrique AlonsoNo ratings yet
- Procalcitonin and AB DecisionsDocument10 pagesProcalcitonin and AB DecisionsDennysson CorreiaNo ratings yet
- 178-Article Text-718-1-10-20220331Document12 pages178-Article Text-718-1-10-20220331Alda AdeliaNo ratings yet
- 2019 Article 701Document6 pages2019 Article 701Mohammed KhalidNo ratings yet
- Cancer Controversies Clinical Trials Confirm But Don't Innovate-ConDocument3 pagesCancer Controversies Clinical Trials Confirm But Don't Innovate-ConadssaNo ratings yet
- Research Open AccessDocument9 pagesResearch Open Accessandro.alfieriNo ratings yet
- Hepatitis C Virus: Annals of Internal MedicineDocument17 pagesHepatitis C Virus: Annals of Internal MedicineMax CamargoNo ratings yet
- s13054 023 04626 ZDocument8 pagess13054 023 04626 ZDipendra PoudelNo ratings yet
- 1 s2.0 S0960977620302071 MainDocument8 pages1 s2.0 S0960977620302071 MainAchdewa RohmatullahNo ratings yet
- Jurnal AryaDocument8 pagesJurnal AryaaryapanduNo ratings yet
- Liau Et Al. - 2018 - First Results On Survival From A Large Phase 3 Clinical Trial of An Autologous Dendritic Cell Vaccine in Newly DiagDocument9 pagesLiau Et Al. - 2018 - First Results On Survival From A Large Phase 3 Clinical Trial of An Autologous Dendritic Cell Vaccine in Newly DiagJoeyOrpillaNo ratings yet
- Surgery JournalDocument7 pagesSurgery JournalJane Arian BerzabalNo ratings yet
- s13643 022 02135 8 PDFDocument9 pagess13643 022 02135 8 PDFdeaalifiahNo ratings yet
- Clinical Significance of Some Biomarkers in The Detection of Kidney and Bladder CancersDocument11 pagesClinical Significance of Some Biomarkers in The Detection of Kidney and Bladder CancersCentral Asian StudiesNo ratings yet
- WJG 25 59Document11 pagesWJG 25 59tathimirandatorresNo ratings yet
- Minimizing Population Health Loss in Times of Scarce Surgical Capacity During The Coronavirus Disease 2019 Crisis and Beyond: A Modeling StudyDocument10 pagesMinimizing Population Health Loss in Times of Scarce Surgical Capacity During The Coronavirus Disease 2019 Crisis and Beyond: A Modeling StudyAriani SukmadiwantiNo ratings yet
- Fphar 13 970978Document7 pagesFphar 13 970978Claudiu PopescuNo ratings yet
- Maklumat Struktur Pengajian Bachelor of Medical Science (With Credit Exemption)Document2 pagesMaklumat Struktur Pengajian Bachelor of Medical Science (With Credit Exemption)Noraini Mohammad YusufNo ratings yet
- Fireteam ZeroDocument12 pagesFireteam ZeroZee DeckardNo ratings yet
- Abdominal TraumaDocument34 pagesAbdominal Traumalaurz95No ratings yet
- Wco14 AbstractbookDocument392 pagesWco14 AbstractbookSri HariNo ratings yet
- Case Report Orto YP PDFDocument6 pagesCase Report Orto YP PDFYulinda PrimilisaNo ratings yet
- Epidemiological Study of Bloody Diarrhoea Among Children in Baghdad, IraqDocument9 pagesEpidemiological Study of Bloody Diarrhoea Among Children in Baghdad, IraqInternational Medical PublisherNo ratings yet
- ANNEXURE-5 Material Safety Data SheetDocument11 pagesANNEXURE-5 Material Safety Data SheetSuraj KumarNo ratings yet
- CPOBDocument51 pagesCPOBKenzi AlvarioNo ratings yet
- AssignmentDocument5 pagesAssignmentMark Ludwig LabastidaNo ratings yet
- Bruximo PDFDocument44 pagesBruximo PDFcemoaraNo ratings yet
- College of Nursing: Rifadin RifampinDocument4 pagesCollege of Nursing: Rifadin RifampinAnika PleñosNo ratings yet
- Dr. Mukarram Zaidi Letter To AlbertansDocument1 pageDr. Mukarram Zaidi Letter To AlbertansedmontonjournalNo ratings yet
- Plan of Drug Inspector Examination & Syllabus of Drug Inspector ExamDocument2 pagesPlan of Drug Inspector Examination & Syllabus of Drug Inspector ExamPrasanna AnganeNo ratings yet
- Fluid and ElectrolytesDocument179 pagesFluid and ElectrolytesTrixie Al Marie75% (4)
- Sword of DamoclesDocument9 pagesSword of DamoclesshannonNo ratings yet
- SDS - Pilot II With LC - Marine - Protective - English (Uk) - United Kingdom - 637 - 24.01.2013Document13 pagesSDS - Pilot II With LC - Marine - Protective - English (Uk) - United Kingdom - 637 - 24.01.2013NPTNo ratings yet
- Poison Act 1952Document21 pagesPoison Act 1952Devina IreneNo ratings yet
- Immunology Terms - DefinationDocument7 pagesImmunology Terms - DefinationDonesh VarshneyNo ratings yet
- Ma. Lammatao: Trion AKG Marble LLCDocument11 pagesMa. Lammatao: Trion AKG Marble LLCNasir AhmedNo ratings yet
- FACE PckeDocument4 pagesFACE PckeSamiksha SarafNo ratings yet
- Sample OutputDocument110 pagesSample OutputMohana MuraliNo ratings yet
- Prolapso de Cordón 1Document10 pagesProlapso de Cordón 1Jhonatan MendozaNo ratings yet
- Casabar Crislyn Exercise 33 PDFDocument4 pagesCasabar Crislyn Exercise 33 PDFSEAN JODI M. COSEPENo ratings yet
- Iraqi Injury Surveillance System Annual Report 2013Document46 pagesIraqi Injury Surveillance System Annual Report 2013bejarhasanNo ratings yet
- Annotated BibliographyDocument3 pagesAnnotated BibliographyjamiemarzanoNo ratings yet
- Antiphospholipid SyndromeDocument12 pagesAntiphospholipid Syndromeisravg94No ratings yet
- 2 Year Physical Therapy NotesDocument129 pages2 Year Physical Therapy Notesthwiseman94% (17)
- 1-Module 1 Introduction 20181114 RCGDocument46 pages1-Module 1 Introduction 20181114 RCGRoger ChiuNo ratings yet