Professional Documents
Culture Documents
Document 22
Uploaded by
nicolasdanica0180 ratings0% found this document useful (0 votes)
2 views3 pagesOriginal Title
Document-22
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views3 pagesDocument 22
Uploaded by
nicolasdanica018Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Dianna Grachelle A.
Dy BSN- 4
ACTIVITY-2
1. State several immunodeficiency’s disease define and classify them whatever they are
primary or secondary.
- Primary Immunodeficiency are usually present at birth and are genetic
disorders that are usually hereditary. They typically become evident during
infancy or childhood. These are the examples
• Severe Combined Immunodeficiency (SCID): This is a severe disorder that
affects both T and B cells, leading to a nearly complete inability to fight
infections.
• Common Variable Immunodeficiency (CVID): This disorder primarily
affects B cells, leading to low antibody levels and increased susceptibility to
infection.
• DiGeorge Syndrome: This disorder is caused by a defect in several genes,
leading to poor development of several body systems. Immune system
problems can occur due to issues with the development of the thymus gland.
• Hyper-IgM Syndrome: This is a condition that disrupts the normal
production of antibodies, leading to a higher susceptibility to infections,
especially in the respiratory and gastrointestinal systems.
• Wiskott-Aldrich Syndrome: This is a rare X-linked recessive disease
characterized by eczema, thrombocytopenia (low platelet count), immune
deficiency, and bloody diarrhea (secondary to the thrombocytopenia).
- Secondary Immunodeficiencies, also known as acquired
Immunodeficiencies, are not genetic and occur when an outside source such as
a virus, chemotherapy, or malnutrition, suppresses or destroys the immune
system. Examples include:
• Acquired Immunodeficiency Syndrome (AIDS): Caused by the human
immunodeficiency virus (HIV), which attacks T cells, weakening the immune
system.
• Immunodeficiency due to medication or treatment: Some medications,
like corticosteroids or chemotherapy drugs, can suppress the immune system.
• Malnutrition: Lack of proper nutrients can lead to a weakened immune
system, as the body requires adequate nutrition for immune cells to function
correctly.
2. Explain hypersensitivity. What is immediate and delayed hypersensitivity?
- Hypersensitivity refers to an exaggerated or inappropriate immune response
to a substance that is normally harmless or would not cause an immune
response in most people. These substances, known as allergens, can include
pollen, dust mites, certain foods, medications, or insect stings, among others.
• Hypersensitivity reactions are classified into four types: Type I, Type II,
Type III, and Type IV. The first three types are considered immediate
hypersensitivity reactions, while Type IV is considered a delayed
hypersensitivity reaction.
Immediate Hypersensitivity (Type I, II, III):
1. Type I Hypersensitivity: Also known as anaphylactic or allergic reactions.
These reactions occur rapidly, usually within minutes of exposure to an
allergen. They are mediated by IgE antibodies and can cause symptoms such
as hives, itching, runny nose, and in severe cases, anaphylaxis. Common
examples include hay fever, food allergies, and some types of asthma.
2. Type II Hypersensitivity: Also known as cytotoxic hypersensitivity. These
reactions involve IgG or IgM antibodies directed against antigens present on
the surface of cells or other tissue components, leading to cell damage or
destruction. Examples include autoimmune hemolytic anemia and
Goodpasture's syndrome.
3. Type III Hypersensitivity: Also known as immune complex-mediated
hypersensitivity. These reactions involve the formation of immune complexes
(antigen-antibody complexes) that deposit in tissues and trigger inflammation
and tissue damage. Examples include systemic lupus erythematosus and
rheumatoid arthritis.
Delayed Hypersensitivity (Type IV):
Type IV Hypersensitivity: Also known as cell-mediated or delayed-type
hypersensitivity. These reactions are mediated by T cells rather than
antibodies and typically take 48-72 hours to develop. They involve the
activation of T cells by antigens, leading to an inflammatory response and, in
some cases, tissue damage. Examples include contact dermatitis (such as
poison ivy rash) and the tuberculin skin test reaction.
3. Show a summary flow of anaphylaxis
- Anaphylaxis is a severe, potentially life-threatening allergic reaction that can
occur rapidly after exposure to an allergen. Here's a simplified flow of how
anaphylaxis occurs:m
• Exposure to Allergen: The individual comes into contact with an allergen.
This could be a certain food, medication, insect sting, or other substance that
the person is allergic to.
• Immune Response Activation: The person's immune system overreacts to the
allergen. It produces immunoglobulin E (IgE) antibodies that bind to the
allergen and to mast cells and basophils in the body.
• Release of Chemical Mediators: The binding of IgIgEo mast cells and
basophils triggers these cells to release chemical mediators, including
histamine and other substances.
• Onset of Symptoms: These chemical mediators cause blood vessels to widen
(leading to a drop in blood pressure), airways to narrow (making breathing
difficult), and other symptoms such as skin reactions (like hives and swelling),
gastrointestinal symptoms (like vomiting and diarrhea), and heart palpitations.
• Severe Reaction: If not treated promptly, the reaction can become severe,
leading to anaphylactic shock. This involves a severe drop in blood pressure,
loss of consciousness, and potentially, death.
• Treatment: Immediate treatment with epinephrine (adrenaline) is needed to
reverse the symptoms. This is usually administered as an injection. Further
medical treatment may be needed, including oxygen, intravenous fluids, and
other medications.
4. Explain in summary autoimmunity
- Autoimmunity refers to a condition in which the immune system mistakenly
attacks and damages the body's own cells, tissues, or organs as if they were
foreign substances. Normally, the immune system is designed to protect the
body from harmful invaders like bacteria and viruses, but in autoimmunity, it
loses the ability to distinguish between self and non-self.
• Loss of Self-Tolerance: In autoimmunity, the immune system fails to
recognize certain parts of the body as "self" and begins to mount an immune
response against them.
• Autoantibody Production: The immune system produces autoantibodies,
which are antibodies that target the body's own cells, tissues, or organs. These
autoantibodies can cause inflammation and damage to the affected tissues.
• Inflammatory Response: The immune system activates immune cells, such
as T cells and macrophages, which release inflammatory substances. These
substances contribute to tissue damage and further immune response.
• Organ-Specific or Systemic Autoimmune Diseases: Autoimmunity can
lead to various types of autoimmune diseases. Some autoimmune diseases
target specific organs or tissues, such as the thyroid (Hashimoto's thyroiditis)
or joints (rheumatoid arthritis). Others, like systemic lupus erythematosus
(SLE), affect multiple organs throughout the body.
• Environmental and Genetic Factors: The exact cause of autoimmunity is
not fully understood, but it is believed to involve a combination of genetic
predisposition and environmental triggers. Certain genetic factors can increase
the risk of developing autoimmune diseases, while environmental factors like
infections, hormones, and stress may trigger or exacerbate the immune
response.
• Treatment Approaches: Treatment for autoimmune diseases focuses on
managing symptoms, reducing inflammation, and suppressing the immune
response. This can include medications to control immune activity, lifestyle
changes, and sometimes, specific treatments targeted at the affected organs.
You might also like
- Big Question: What Happens When Immune System Overreacts?Document42 pagesBig Question: What Happens When Immune System Overreacts?Louloun MoussignacNo ratings yet
- Immune Disorders..Ppt FairDocument79 pagesImmune Disorders..Ppt FairSumi SebastianNo ratings yet
- Autoimmune DiseasesDocument70 pagesAutoimmune DiseasesAdebisi OluwatomiwaNo ratings yet
- Immuno-Pharmacology: Dr. Harshika Patel Pharmacology and Therapeutics II Date:23/05/2018 Time: 11am - 1pmDocument90 pagesImmuno-Pharmacology: Dr. Harshika Patel Pharmacology and Therapeutics II Date:23/05/2018 Time: 11am - 1pmBob MuneneNo ratings yet
- How To Position Finerenone in The Treatment Algorithm For Type 2 Diabetes With Renal Complication - GPMPDocument27 pagesHow To Position Finerenone in The Treatment Algorithm For Type 2 Diabetes With Renal Complication - GPMPTaufiqurrokhman RofiiNo ratings yet
- Medstar Pediatrics - 2nd EditionDocument649 pagesMedstar Pediatrics - 2nd Editionmy Lord Jesus100% (3)
- 7 Allergic DiseasesDocument49 pages7 Allergic Diseasescrystyneldove100% (3)
- Khan Hypersensitivity Reactions Final 2011Document56 pagesKhan Hypersensitivity Reactions Final 2011Poptarts83No ratings yet
- Autoimun MekanismeDocument22 pagesAutoimun MekanismeMeity ElvinaNo ratings yet
- Diseases of ImmunityDocument11 pagesDiseases of ImmunityRAFAELLA SALVE MARIE GAETOSNo ratings yet
- Hypersensitivity StatesDocument40 pagesHypersensitivity StatesMorrison NjageNo ratings yet
- Nursing Management of A Client With Immunological Disorders: M.N Priyadarshanie BSC in NursingDocument47 pagesNursing Management of A Client With Immunological Disorders: M.N Priyadarshanie BSC in NursingClarissa Cabudoc OronosNo ratings yet
- Disorders and Diseases of Immune SystemDocument21 pagesDisorders and Diseases of Immune SystemWijesiri D WNo ratings yet
- Patho Gy 2 PrrsentationDocument16 pagesPatho Gy 2 PrrsentationAyeshaNo ratings yet
- AnaphylacticDocument20 pagesAnaphylacticAlumita RayawaNo ratings yet
- Chapter 20 Tolerance and Auto Immune DiseaseDocument32 pagesChapter 20 Tolerance and Auto Immune Diseasehusseinabdullahahmad99No ratings yet
- Reactions To Drugs Are AllergicDocument5 pagesReactions To Drugs Are AllergicMuhammad HuzeafaNo ratings yet
- Module. Immunity - Infection Fall 2019Document44 pagesModule. Immunity - Infection Fall 2019Christyl RealreconizerealNo ratings yet
- Immunlogical DisorderDocument36 pagesImmunlogical DisorderSameen NasirNo ratings yet
- Hypersensitivity: Nasrullah M.Phil BiotechnologyDocument16 pagesHypersensitivity: Nasrullah M.Phil BiotechnologyNasrullahNo ratings yet
- Allergy and HypersensitivityDocument73 pagesAllergy and HypersensitivityAdi PomeranzNo ratings yet
- Hypersensitivity ReactionsDocument2 pagesHypersensitivity ReactionsLourdette TorrefielNo ratings yet
- Hypersensitivity Reactions ChiniotiDocument11 pagesHypersensitivity Reactions ChiniotiAbdullah DoulaNo ratings yet
- Activity 14 Understanding Immune SystemDocument20 pagesActivity 14 Understanding Immune SystemKendrix Aguiluz FlorendoNo ratings yet
- Auto ImmunityDocument38 pagesAuto ImmunityMau studioNo ratings yet
- Figure 12.2there Are Four Types of Hypersensitivity Reaction Mediated by Immunological Mechanisms That Cause Tissue DamageDocument11 pagesFigure 12.2there Are Four Types of Hypersensitivity Reaction Mediated by Immunological Mechanisms That Cause Tissue DamagewicellecheeNo ratings yet
- DocumentDocument19 pagesDocumentbaroque.nacNo ratings yet
- Hypersenstivity Type 1 and Type 11Document34 pagesHypersenstivity Type 1 and Type 11Dil NavabNo ratings yet
- General Features of Immune System Immune System: DefinitionDocument17 pagesGeneral Features of Immune System Immune System: Definitionمحمد نعیم اقبالNo ratings yet
- Harmful Effects of ImmunityDocument2 pagesHarmful Effects of ImmunityrakibhelpNo ratings yet
- 1-How Immune System Works1 08 08Document63 pages1-How Immune System Works1 08 08all4one1983100% (1)
- Week 2 Chapter 10: Alterations in Immune FunctionDocument55 pagesWeek 2 Chapter 10: Alterations in Immune FunctionAshley Diane HenryNo ratings yet
- 20223microlab Activity 9 Hypersensitivty ReactionsDocument6 pages20223microlab Activity 9 Hypersensitivty Reactionsmarianneladislao07No ratings yet
- 07 ImmunopathologyDocument4 pages07 Immunopathologylight liNo ratings yet
- UntitledDocument9 pagesUntitledMasar ElfNo ratings yet
- Universidad de Sta. Isabel: Vincentian Learning ModuleDocument10 pagesUniversidad de Sta. Isabel: Vincentian Learning ModuleshinypersonNo ratings yet
- Auto ImmunityDocument44 pagesAuto ImmunityA. PathakNo ratings yet
- Immunological Aspects of Oral DiseasesDocument35 pagesImmunological Aspects of Oral Diseasesمهدي محمدNo ratings yet
- 22 Hypersenitivity & AutoimmuneDocument53 pages22 Hypersenitivity & AutoimmuneAnonymous Bh6y0TuVHiNo ratings yet
- Immunodeficiency Disorder: Supervisor: Dr. Rebar Mohammed Name Student: Nazo Rashid AliDocument12 pagesImmunodeficiency Disorder: Supervisor: Dr. Rebar Mohammed Name Student: Nazo Rashid Alinazo rashid aliNo ratings yet
- AllergyDocument86 pagesAllergyhoor e ainNo ratings yet
- L24 AutoimmDocument35 pagesL24 AutoimmFadli FadelNo ratings yet
- Immunity, Autoimmunity - QsDocument5 pagesImmunity, Autoimmunity - QsMaedehNo ratings yet
- Cell-Mediated & Humoral Immunity PathologyDocument65 pagesCell-Mediated & Humoral Immunity PathologyCrystal GamingNo ratings yet
- Immunology in Health and DiseasesDocument7 pagesImmunology in Health and DiseasesLianneRaoNo ratings yet
- Autoimmune Disease: Duhok Polytechnic University Duhok Technical Institute Department of PharmacyDocument17 pagesAutoimmune Disease: Duhok Polytechnic University Duhok Technical Institute Department of PharmacyRasheed AliNo ratings yet
- Hypersensitivity Rev BWDocument34 pagesHypersensitivity Rev BWGuhanNo ratings yet
- Unit 5 - HypersensitivityDocument7 pagesUnit 5 - HypersensitivitychitraNo ratings yet
- Autoimmune-Disorders PDF Divya Mam PracticalDocument44 pagesAutoimmune-Disorders PDF Divya Mam Practicaltariqahmeda34No ratings yet
- An Allergy Is An Adverse Reaction That The Body Has To A Particular Food or Substance in The EnvironmentDocument15 pagesAn Allergy Is An Adverse Reaction That The Body Has To A Particular Food or Substance in The EnvironmentwengieNo ratings yet
- Seminar On Anaphylaxis 7-6-12Document70 pagesSeminar On Anaphylaxis 7-6-12LIDIYA MOL P VNo ratings yet
- Clinical Immunology DR - TahaDocument106 pagesClinical Immunology DR - TahaYaseen AhmadNo ratings yet
- Immunodefisiency & Autoimmune: Dr. Isbandiyah, SPPDDocument20 pagesImmunodefisiency & Autoimmune: Dr. Isbandiyah, SPPDZaheer HatsyieNo ratings yet
- Veterinary Immunology: Fuad Mohammed (DVM, MSC, Assist. Prof.)Document36 pagesVeterinary Immunology: Fuad Mohammed (DVM, MSC, Assist. Prof.)BEKUMA SHIBIRUNo ratings yet
- Immune FinalDocument53 pagesImmune FinalJaylord VerazonNo ratings yet
- Hypersensitivity ReactionDocument8 pagesHypersensitivity ReactionSuzetteBragaSamuelaNo ratings yet
- Hypersensitivity To Drugs and Their Mechanisms: Name: Mellya Rizki Pitriani Student ID: B1B017031Document10 pagesHypersensitivity To Drugs and Their Mechanisms: Name: Mellya Rizki Pitriani Student ID: B1B017031Mellya RizkiNo ratings yet
- Autoimmune Disorders: CausesDocument11 pagesAutoimmune Disorders: CausesJenalyn Pilapil SumaelNo ratings yet
- Adverse Drug ReactionDocument16 pagesAdverse Drug ReactionmayankNo ratings yet
- Hypersensitivity Report Diampon Bsn2bDocument17 pagesHypersensitivity Report Diampon Bsn2bclaribelleNo ratings yet
- Microbio. Chapter 16 StudyDocument8 pagesMicrobio. Chapter 16 Studyaphillips1No ratings yet
- Holistic Allergy Management: Self-Care, Diet, and HomeopathyFrom EverandHolistic Allergy Management: Self-Care, Diet, and HomeopathyNo ratings yet
- NMDAR4Document4 pagesNMDAR4Sirly PutriNo ratings yet
- Diabetes Self Management - Fall 2023Document68 pagesDiabetes Self Management - Fall 2023Jair SierraNo ratings yet
- Course 5 Pleuro-Pulmonary Surgical SemiologyDocument23 pagesCourse 5 Pleuro-Pulmonary Surgical SemiologyvladutNo ratings yet
- Silverman-Anderson: Newborn ProfileDocument10 pagesSilverman-Anderson: Newborn ProfileLiel TorresNo ratings yet
- Rmc161e PDFDocument9 pagesRmc161e PDFJesús Alexis Alvarado AbreuNo ratings yet
- Seizures/Epilepsy: Case PersentationDocument14 pagesSeizures/Epilepsy: Case PersentationAbdulmalik AliNo ratings yet
- Health Declaration Form D02Document1 pageHealth Declaration Form D02Hizwani ZainalNo ratings yet
- Obesity JamaDocument16 pagesObesity JamaSrinivas PingaliNo ratings yet
- NCAA Concussion Fact SheetDocument2 pagesNCAA Concussion Fact Sheetelijah edwardsNo ratings yet
- HIFU For Face Treatment - Benefits, Cost, Efficacy & MoreDocument7 pagesHIFU For Face Treatment - Benefits, Cost, Efficacy & Moreahmad saadNo ratings yet
- Aisha TuDocument21 pagesAisha TuDedan GideonNo ratings yet
- STS Chapter 15Document2 pagesSTS Chapter 15Fritz Dela CernaNo ratings yet
- Chapter 6 Dimension of Development Health AwarenessDocument43 pagesChapter 6 Dimension of Development Health AwarenessRechienvhel OccianoNo ratings yet
- 4-Pathogenesis & Virulence LectureDocument25 pages4-Pathogenesis & Virulence Lecturetruch 2022No ratings yet
- Trastornos de Alimentacion CIE 11Document19 pagesTrastornos de Alimentacion CIE 11Elene MezaNo ratings yet
- Electrotherapy PresentationDocument24 pagesElectrotherapy PresentationHamza DibNo ratings yet
- Who Standardized Emergency Unit Form TraumaDocument2 pagesWho Standardized Emergency Unit Form TraumaJm uniteNo ratings yet
- Pro-Choice Perspective On AbortionDocument2 pagesPro-Choice Perspective On AbortionPreacher Of IslamNo ratings yet
- A Case Report: Hypersensitivity Reaction To DrugsDocument5 pagesA Case Report: Hypersensitivity Reaction To DrugsGNNo ratings yet
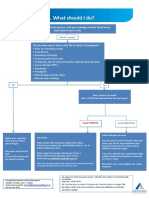
- What To Do If Youre Sick FlowchartDocument1 pageWhat To Do If Youre Sick FlowchartfuckyouNo ratings yet
- 2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryDocument20 pages2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryLéo VidoniNo ratings yet
- 5-Surgical InfectionsDocument46 pages5-Surgical InfectionsAiden JosephatNo ratings yet
- Oncology TestDocument32 pagesOncology TestPhilip Gene II MalacasNo ratings yet
- Chapter 5 ExercisesDocument10 pagesChapter 5 Exercisesshafilcr07No ratings yet
- Connect Core Concepts in Health Big 14th Edition Insel Test BankDocument30 pagesConnect Core Concepts in Health Big 14th Edition Insel Test Banktylerayalaardbgfjzym100% (33)
- Quiz 3 ABpsychDocument2 pagesQuiz 3 ABpsychjerahmeel lavinaNo ratings yet
- 10 Possible Health Benefits of Green TeaDocument2 pages10 Possible Health Benefits of Green TeaGousalyaaNo ratings yet
- Children ConceptsDocument5 pagesChildren ConceptsMARINANo ratings yet