Professional Documents
Culture Documents
ABIGAIL 2010_Diffuse Alveolar Hemorrhage
Uploaded by
Rafael JustinoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ABIGAIL 2010_Diffuse Alveolar Hemorrhage
Uploaded by
Rafael JustinoCopyright:
Available Formats
Diffuse Alveolar Hemorrhage
Abigail R. Lara and Marvin I. Schwarz
Chest 2010;137;1164-1171
DOI 10.1378/chest.08-2084
The online version of this article, along with updated information and
services can be found online on the World Wide Web at:
http://chestjournal.chestpubs.org/content/137/5/1164.full.html
Chest is the official journal of the American College of Chest
Physicians. It has been published monthly since 1935.
Copyright2010by the American College of Chest Physicians, 3300
Dundee Road, Northbrook, IL 60062. All rights reserved. No part of
this article or PDF may be reproduced or distributed without the prior
written permission of the copyright holder.
(http://chestjournal.chestpubs.org/site/misc/reprints.xhtml)
ISSN:0012-3692
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
CHEST Recent Advances in Chest Medicine
Diffuse Alveolar Hemorrhage
Abigail R. Lara, MD; and Marvin I. Schwarz, MD, FCCP
Diffuse alveolar hemorrhage (DAH) is often a catastrophic clinical syndrome causing respiratory
failure. Recognition of DAH often requires BAL as symptoms are nonspecific, hemoptysis is
absent in up to one-third of patients, and radiographic imaging is also nonspecific and similar to
other acute alveolar filling processes. Once the diagnosis is established, the underlying cause
must be established in order to initiate treatment. This review discusses the diagnosis of the
underlying histologies and the clinical entities that are responsible for DAH as well as treatment
options. CHEST 2010; 137(5):1164–1171
Abbreviations: ANCA 5 antineutrophilic cytoplasmic autoantibodies; DAH 5 diffuse alveolar hemorrhage;
IPH 5 idiopathic pulmonary hemosiderosis; MPA 5 microscopic polyangiitis; MPO 5 myeloperoxidase; PR3 5 proteinase 3;
SLE 5 systemic lupus erythematosus; WG 5 Wegener granulomatosis
Bleeding from the lung originates from the bron-
chial vessels, the pulmonary vessels, or the micro-
small vessel vasculitis known as pulmonary capillaritis,
usually seen with seropositive systemic vasculitides,
circulation of the lung. Bleeding of bronchial origin is or a connective tissue disorder, bland pulmonary
usually a result of bronchiectasis or endobronchial hemorrhage, and diffuse alveolar damage due to a
malignancy. Pulmonary hemorrhage originating from number of injuries including drugs, coagulation disor-
the small, medium, and large pulmonary vessels is ders, and infections. Pulmonary capillaritis may also
most commonly due to systemic vasculitis, which can be a small vessel vasculitis limited to the lung. BAL
also involve the microcirculation. Vasculitides involv- confirms the clinical diagnosis of DAH; however, a sur-
ing the microvasculature is known as pulmonary gical lung biopsy may be required to confirm the
capillaritis. Diffuse alveolar hemorrhage (DAH) is underlying histology. In general, surgical lung biopsy
a clinicopathologic syndrome describing the accumu- is considered if DAH is associated with negative
lation of intraalveolar RBCs originating from the serology and not a part of a systemic disease. Treatment
alveolar capillaries. All causes of DAH have the is directed at the underlying diagnosis and typically
common denominator of an injury to the alveolar includes corticosteroids, immunosuppressive agents,
microcirculation. The clinical syndrome includes and occasionally plasmapheresis.
hemoptysis, anemia, diffuse radiographic pulmonary
infiltrates, and hypoxemic respiratory failure, which
can be severe. DAH is associated with a number
of clinical entities and several histologic subtypes. Definition
The most common underlying histology of DAH is of a DAH is recognized by the clinical constellation
of hemoptysis, anemia, diffuse radiographic pulmo-
Manuscript received August 27, 2009; revision accepted September nary infiltrates, and hypoxemic respiratory failure.
19, 2009. The underlying histopathology of DAH includes
Affiliations: From the Division of Pulmonary Sciences and Critical
Care, University of Colorado Health Sciences Center, Denver, CO. the presence of intraalveolar RBCs and fibrin and
Correspondence to: Marvin I. Schwarz, MD, FCCP, University of the eventual accumulation of hemosiderin-laden
Colorado Health Sciences Center, Division of Pulmonary Sciences macrophages, which may take up to 48 to 72 h to
and Critical Care, 4200 E 9th Ave, Box C272, Denver, CO 80262;
e-mail: marvin.schwarz@ucdenver.edu accumulate. Of the histologies that are associated
© 2010 American College of Chest Physicians. Reproduction with DAH (pulmonary capillaritis, bland pulmonary
of this article is prohibited without written permission from the hemorrhage, diffuse alveolar damage, and miscella-
American College of Chest Physicians (www.chestpubs.org/
site/misc/reprints.xhtml). neous histology) pulmonary capillaritis is the most
DOI: 10.1378/chest.08-2084 common.
1164 Recent Advances in Chest Medicine
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
Pulmonary capillaritis has a unique histopathologic (13%), idiopathic pulmonary hemosiderosis (IPH) (13%),
appearance consisting of an interstitial neutrophilic collagen vascular diseases (13%), and microscopic
predominant infiltration, fibrinoid necrosis of the polyangiitis (MPA) (9%). In another series, isolated
alveolar and capillary walls, and leukocytoclasis.1 The pauciimmune pulmonary capillaritis was the most
infiltrating neutrophils undergo cytoclasis, nuclear common cause of DAH associated with capillaritis.6 In
debris accumulates within the interstitium, and there recipients of hematopoietic stem cell transplantation,
is a subsequent loss of the integrity of the alveolar- DAH was reported to occur in 5% of 3,806 patients.7
capillary basement membrane (Fig 1). It is the disrup-
tion of the alveolar-capillary basement membranes that
results in the accumulation of RBCs in alveolar spaces. Clinical Presentation and Diagnosis
There is a distinction between pulmonary capillaritis
and pulmonary vasculitis. Pulmonary vasculitis refers to DAH appears at any age and often with an estab-
inflammation of the lung vessels of any size, whereas lished associated disease. DAH may also be the initial
pulmonary capillaritis is confined to the microcircula- manifestation of an underlying systemic disease. The
tion of the lung (alveolar capillaries, arterioles, and cardinal sign of DAH, hemoptysis, may be a dramatic
venules). However, both may be seen in systemic vascu- event or evolve over days to weeks; however, it may
litides and the connective tissue diseases. be initially absent in up to 33% of DAH cases. The
Recently, there has been an effort to change the natural course is unpredictable and varies in severity
eponym of Wegener granulomatosis (WG) to a more but always should be considered a potentially life-
scientific nomenclature of antineutrophilic cytoplas- threatening event. The symptoms of DAH, other
mic autoantibodies (ANCA)-associated granulomatous than hemoptysis, are nonspecific and include fever,
vasculitis.2-4 This is not the first time that an eponym chest pain, cough, and dyspnea. Nonpulmonary signs
has undergone a change (eg, Loeffler Syndrome and and symptoms are those that accompany the underly-
simple pulmonary eosinophilia).5 Although the sugges- ing systemic disease. In addition to history, physical
tion to develop an alternative name for WG may have examination, and routine laboratory studies, directed
evolved after the association of Dr Wegener and the serologic testing for connective tissue disease and
Nazi regime, it is our opinion that the alternative should systemic vasculitis is useful for establishing the
be used because it serves to describe the pathology, diagnosis (Table 2). In up to one-third of patients
and eponyms do not describe the disease process. with DAH, hemoptysis is absent and the diagnosis is
established after sequential BAL reveals worsening
RBC counts.8 Moreover, a falling hematocrit should
Etiology alert the clinician to the possibility of DAH. The chest
radiograph findings are nonspecific and consist of an
Injury to the alveolar microcirculation resulting in alveolar filling process that can be a patchy, focal, or
DAH may be localized to the lung (inhalation injuries, diffuse alveolar filling process (Fig 2). Chest CT scans
diffuse alveolar damage) or associated with a systemic confirm the chest radiographic findings and more
disorder (vasculitis or connective tissue disease). The accurately define the extent of disease. Flexible bron-
causes of DAH are listed in Table 1. There is a spectrum choscopy should be performed to establish the clinical
of disorders associated with DAH, but no prospective diagnosis of DAH and to exclude infections. Progres-
studies estimate its relative frequency. A review of sively hemorrhagic BAL found in serial samples is
34 cases of histopathologically confirmed DAH indi- diagnostic of DAH but not the underlying cause.
cated that capillaritis occurred in 88% of the cases. Surgical lung biopsy may be required to establish the
In one report, the most common clinical cause of DAH cause if serologic testing or clinical history is unre-
was WG (32%), followed by Goodpasture syndrome vealing. Transbronchial biopsies are usually insufficient.
With recurrent episodes of DAH, interstitial fibrosis
or an obstructive lung disease most compatible with
emphysema can evolve.9,10
Specific Disorders Associated With DAH
Isolated Pauciimmune Pulmonary Capillaritis
Isolated pauciimmune pulmonary capillaritis is a
small-vessel vasculitis that is confined to the lung and
Figure 1. Polymorphoneutrophils invading the capillary walls
(arrowhead) (A). RBC accumulation in the alveolar spaces and without clinical or serologic features of an associated sys-
leukocytoclasis (arrows) (B). temic disease. In a series of 29 cases of biopsy-confirmed
www.chestpubs.org CHEST / 137 / 5 / MAY, 2010 1165
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
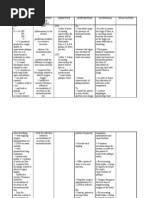
Table 1—Etiology and Histology of Diffuse Alveolar is unknown but is reported to occur most commonly
Hemorrhage before the age of 30 years. In the pediatric popula-
Pulmonary capillaritis
tion the incidence is reported to be 0.24 in 1 million.13
ANCA-associated granulomatous vasculitis The histology lacks evidence of capillaritis and the
Microscopic polyangiitis alveolar basement membranes are thickened but
Isolated pulmonary capillaritis (ANCA positive and negative) remain intact. Recurrent episodes of DAH lead to
SLE
release of iron into the lung resulting in an abundance
Rheumatoid arthritis
Mixed connective tissue disorder of hemosiderin-laden macrophages.11,14 In advanced
Scleroderma cases of IPH, the lungs develop a distinctive brown
Polymyositis color due to the abundance of hemosiderin and
Primary antiphospholipid antibody syndrome have varying degrees of consolidation and fibrosis.
Henoch-Schönlein purpura
The cause and pathogenesis is unknown; however,
Behçet Syndrome
IgA nephropathy an immune process may be involved as IPH appears
Goodpasture syndrome to respond to immunosuppressant therapy. Although
Idiopathic glomerulonephritis (pauciimmune or immune IPH was included as a syndrome with DAH, it
complex-related) should be noted that it is a rare entity distinct in his-
Acute lung transplant rejection
Idiopathic pulmonary fibrosis
tology from other causes of DAH resulting from the
Diphenylhydantoin microcirculation.
Retinoic acid toxicity
Autologous bone marrow transplantation
Myasthenia gravis ANCA-Associated Granulomatous Vasculitis
Cryoglobulinemia
Ulcerative colitis
ANCA-associated granulomatous vasculitis is a
Propylthiouracil systemic vasculitis characterized by granulomatous
Bland pulmonary hemorrhage inflammation of the upper and lower respiratory tract,
IPH necrotizing vasculitis, and the presence of ANCA.
Goodpasture syndrome The ANCA associated with ANCA-associated granu-
SLE
Coagulation disorders
lomatous vasculitis is an antibody directed against
Trimellitic anhydride cytoplasmic proteinase 3 (PR3).15 Demographic data
Isocyanate exposure obtained from the WG Etanercept Trial varied
Penicillamine between the patients with limited vs severe disease.
Amiodarone Patients with DAH were defined as having severe
Nitrofurantoin
Mitral stenosis
disease, were older (mean age of 50 6 16 vs 41 6
Subacute bacterial endocarditis 16 years), and were more likely to be men. DAH was
Polyglandular autoimmune syndrome identified in 25% of the patients with more severe
Multiple myeloma disease.16 The pathogenesis of PR3-ANCA-positive
Diffuse alveolar damage vasculitis involves the cellular immune pathways
Bone marrow transplantation
Crack cocaine inhalation
resulting in granulomatous inflammation.15 The
Cytotoxic drug therapy percentage expression of PR3 on the surface of neu-
SLE trophils in patients with ANCA-associated granu-
Radiation therapy lomatous vasculitis correlates with higher rates of
ARDS
relapse.17 A retrospective analysis found rising titers
ANCA 5 antineutrophilic cytoplasmic autoantibodies; IPH 5 idiopathic of cytoplasmic-ANCA to have high sensitivity and
pulmonary hemosiderosis; SLE 5 systemic lupus erythematosus.
specificity (93% and 97%, respectively) in predicting
relapse or the presence of active disease.18,19 However,
a recent prospective study had a specificity of 75%
pulmonary capillaritis, isolated pauciimmune pulmo-
and a sensitivity of 71% for predicting relapse using
nary capillaritis was the most common cause of DAH.11
rising titers.20 Patients with persistently high titers of
Overall, patients with isolated pauciimmune pulmo-
PR3-ANCA after remission tend to have a higher risk
nary capillaritis tend to have a better prognosis when
of relapse than those who are ANCA negative.21 Current
compared with DAH occurring in the setting of a
treatment is concentrated for the induction of remission
systemic vasculitis or collagen vascular disease.
using corticosteroids and cyclophosphamide. Mainte-
IPH nance therapy after remission is achieved either with
methotrexate or azathioprine. Recently rituximab, a
IPH is a rare syndrome in which repeated episodes chimeric anti-CD20 monoclonal antibody, has been
of DAH occur resulting in chronic anemia and pulmo- shown to induce remission in patients with refractory
nary fibrosis.12 The incidence in the adult population ANCA-associated granulomatous vasculitis, but should
1166 Recent Advances in Chest Medicine
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
Table 2—Serologic and Radiologic Evaluation of
Diffuse Alveolar Hemorrhage
Nonspecific findings
Leukocytosis
Any cause
Thrombocytopenia
Cytotoxic drugs
Antiphospholipid syndrome
SLE
Increased sedimentation rate
Any cause
Urine red blood cell casts
Any systemic vasculitis
SLE, mixed connective tissue disease
Goodpasture syndrome
Abnormal PT, PTT, INR
SLE
Coagulation disorders
Drugs
Chest radiographic and CT scan infiltrates
Patchy or diffuse, often with apical and peripheral sparing
Any cause
Air bronchograms
Any cause
Specific findings
ANA
Connective tissue disease
Rheumatoid factor
Connective tissue disease
ANCA-associated granulomatous vasculitis
Cytoplasmic-ANCA
ANCA-associated granulomatous vasculitis
Microscopic polyangiitis (less common)
Perinuclear-ANCA
Microscopic polyangiitis
ANCA-associated granulomatous vasculitis
Specific radiologic findings on chest radiograph and/or CT scan
Kerley B lines
PVOD, mitral stenosis
Nodules, cavities
WG
Rheumatoid arthritis
ANA 5 antinuclear antibody; INR 5 international normalized ratio;
PT 5 prothrombin time; PTT 5 partial thromboplastin time; PVOD 5
pulmonary veno-occlusive disease; WG 5 Wegener granulomatosis. Figure 2. Chest radiograph (A) and chest CT scan (B) showing
See Table 1 for expansion of other abbreviations. diffuse nonspecific alveolar infiltrates in a patient with diffuse
alveolar hemorrhage.
not be considered as first-line therapy in Wegener-
associated DAH.22 Plasma exchange has also shown
usefulness if instituted early in the disease course.23-25 patients who survive an episode of DAH their 1-year
and 5-year survival is reduced to 82% and 68%,
MPA respectively.26-28 MPA can be distinguished from
ANCA-associated granulomatous vasculitis by sero-
MPA is a systemic vasculitis that is confined to the logically demonstrating a perinuclear-ANCA directed
microvessels and is always associated with a focal against neutrophil myeloperoxidase (MPO-ANCA).
segmental necrotizing glomerulonephritis. It is dis- Unlike ANCA-associated granulomatous vasculitis,
tinguished from ANCA-associated granulomatous the level of MPO-ANCA titers is not associated with
vasculitis by the absence of upper airway involve- disease activity.29 Recent animal studies suggest that
ment. DAH due to pulmonary capillaritis occurs in MPO-ANCA, and to a lesser degree PR3-ANCA, may
up to one-third of patients and represents the only mediate disease by activating the alternative comple-
pulmonary manifestation of MPA. DAH increases ment pathway, a self-sustaining pathway, and may
the mortality of MPA. In the acute setting, 30% of lend new insight into the severity of disease in ANCA-
patients do not survive an episode of DAH; in those positive diseases.30 Surgical lung biopsy is usually not
www.chestpubs.org CHEST / 137 / 5 / MAY, 2010 1167
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
necessary in patients with suspected DAH in the set- Other Connective Tissue Diseases
ting of ANCA-positive disease provided infection has
DAH with underlying pulmonary capillaritis is an
been excluded. Treatment, as with ANCA-associated
infrequent occurrence in mixed connective tissue
granulomatous vasculitis, is glucocorticoids, cyclo-
disease, rheumatoid arthritis, polymyositis, dermato-
phosphamide, and plasmapheresis, and is the recom-
myositis, primary antiphospholipid syndrome, and
mended regimen for induction of remission.31
scleroderma.42-54 The DAH may be the presenting
Recombinant factor VIIa has been used to treat severe
manifestation or complicate a preexisting disease.
DAH in MPA with unremitting respiratory failure.
Treatment options are similar to those outlined for
The mechanism of factor VIIa treatment is the
DAH in SLE.
enhancement of thrombin generation on the surface
of activated platelets at the sites of hemorrhage.32
Goodpasture Syndrome (Antiglomerular
Basement Membrane Antibody Disease)
Systemic Lupus Erythematosus
Goodpasture syndrome, also known as antiglomer-
DAH occurs in 4% of patients with systemic ular basement membrane antibody disease-associated
lupus erythematosus (SLE) admitted to the hospital DAH, is likely the result of autoantibodies directed
and pulmonary capillaritis is usually the underlying against the NC1 domain of the a3 chain of the base-
cause.8 In an immunosuppressed patient with SLE, ment membrane collagen type 4.55 The clinical
infectious pneumonia should be excluded as the expression of the disease occurs only in the lungs
cause of DAH.33 In the majority of DAH associated and the kidneys. DAH is common in antiglomerular
with SLE, glomerulonephritis is also present, and basement membrane disease, particularly in cigarette
in 80% the DAH occurs in patients with known smokers. It is postulated that smoking mediates dam-
SLE.8 These are most often young females with a age to the alveolar basement membrane, thus allow-
mean age of 27 years. The mortality had been previ- ing the development of autoantibodies.56,57 Bland
ously reported to be as high as 50%; however, with hemorrhage is the most common underlying histol-
the use of aggressive treatment with glucocorticoids ogy, but pulmonary capillaritis is sometimes seen.58
and cyclophosphamide, the mortality associated Patients with Goodpasture syndrome tend to be men
with DAH in SLE is declining.8,34,35 DAH is distin- in their 20s who also smoke. More than 90% of patients
guished from acute lupus pneumonitis using with Goodpasture disease have circulating anti-
sequential BAL. Acute lupus pneumonitis presents basement membrane antibodies. In patients with
with similar clinical and radiographic features as negative circulating antibasement membrane antibod-
DAH; however, it also has systemic symptoms typi- ies, a lung or renal biopsy with immunofluorescence
cal of an SLE flare and may be the only manifes- revealing linear antibody deposition within the alveo-
tation of the initial presentation of SLE. 36 The lar or glomerular basement membrane confirms the
histologic appearance of acute lupus pneumonitis is diagnosis.59 However, in up to 10% of patients with
varied and includes diffuse alveolar damage, orga- Goodpasture syndrome, DAH is present without renal
nizing pneumonia, nonspecific cellular pneumoni- involvement and is identical to isolated pulmonary
tis, or a combination of these histologic patterns, capillaritis. Lung biopsy with immunofluorescence
but capillaritis is not present.37 Immune complexes studies distinguishes the two.60,61 Treatment with
are frequently found in the lung. The deposition of immunosuppression and plasma exchange has improved
immune complexes and the activation of comple- outcomes in these patients.62 Rituximab, a chimeric
ment within the lung are central to the development anti-CD20 monoclonal antibody that has shown effi-
of parenchymal disease in SLE.38 Methylpredniso- cacy in the treatment of rheumatoid arthritis, should
lone is recommended (1-2 mg/kg/d in divided be considered in patients with ANCA-associated vas-
doses). High-dose pulse methylprednisolone (1 g culitis that is refractory to standard therapy.63,64 Treat-
given in divided doses for 3 days) can be given to ment with rituximab results in depletion of B cells
those with DAH or acute lupus pneumonitis. Esca- that produce pathogenic autoantibodies and reduces
lating treatment in steroid-resistant DAH includes the cellular interaction by decreasing both the pro-
azathioprine, cyclophosphamide, or intravenous g duction of cytokines that maintain mononuclear cells
globulin. The combination of high-dose intravenous and the production of immune complex formations
methylprednisolone and cyclophosphamide anec- that help to sustain the disease.65
dotally is the most effective combination. In refrac-
tory cases, plasmapheresis has been used; however,
Lung Allograft Rejection
survival does not appear to be improved.35,39-41 In a
patient with SLE who has established DAH, recur- Pulmonary capillaritis as a form of acute lung trans-
rences are to be expected. plant rejection was first described in five patients in
1168 Recent Advances in Chest Medicine
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
1998.66 Since then, the mechanism of the acute rejec- establishment of diagnosis, and aggressive treatment
tion with DAH has been studied further.67-69 A necro- likely decreases the morbidity and mortality associ-
tizing, pauciinflammatory septal capillary injury ated with untreated or unrecognized DAH.
pattern was noted. Immunofluorescent staining
revealed a septal capillary deposition of antibodies
specific for complement factors and immunoglobulin Acknowledgments
subtypes.67 Differentiating between acute cellular
Financial/nonfinancial disclosures: The authors have reported
rejection and posttransplant capillaritis requires tissue to CHEST that no potential conflicts of interest exist with any
biopsy and can be found concomitantly in . 50% of companies/organizations whose products or services may be
cases. Isolated pulmonary capillaritis, however, is an discussed in this article.
infrequent occurrence (approximately 10% of all biop-
sies performed; M. Zamora, personal communication).
Treatment consists of IV corticosteroids and plasma- References
pheresis in severe cases.69-72 1. Colby TV, Fukuoka J, Ewaskow SP, Helmers R, Leslie KO.
Pathologic approach to pulmonary hemorrhage. Ann Diagn
Bone Marrow Transplant Pathol. 2001;5(5):309-319.
2. Matteson EL, Woywodt A. Eponymophilia in rheumatology.
Pulmonary complications develop in 30% to 60% of Rheumatology (Oxford). 2006;45(11):1328-1330.
all bone marrow transplant recipients and are the cause 3. Woywodt A, Matteson EL. Wegener’s granulomatosis—
of death in up to 60%.73,74 DAH occurs in approximately probing the untold past of the man behind the eponym.
Rheumatology (Oxford). 2006;45(10):1303-1306.
5% of allogeneic and autologous recipients and has a 4. Woywodt A, Haubitz M, Haller H, Matteson EL. Wegener’s
reported mortality rate ranging from 50% to 100%.7,75 granulomatosis. Lancet. 2006;367(9519):1362-1366.
Of the recipients that develop DAH as a pulmonary 5. Sharma OP, Bethlem EP. The pulmonary infiltration with
complication and survive, the 6-month76 mortality eosinophilia syndrome. Curr Opin Pulm Med. 1996;2(5):380-389.
is 38%.77 6. Travis WD, Colby TV, Lombard C, Carpenter HA. A
clinicopathologic study of 34 cases of diffuse pulmonary hem-
The frequency of DAH does not appear to vary sig- orrhage with lung biopsy confirmation. Am J Surg Pathol.
nificantly with the type of hematopoietic stem cell 1990;14(12):1112-1125.
transplant, with a reported frequency of 1% to 21% 7. Afessa B, Tefferi A, Litzow MR, Krowka MJ, Wylam ME,
in autologous and 2% to 17% in allogeneic hematopoi- Peters SG. Diffuse alveolar hemorrhage in hematopoietic
etic stem cell transplant recipients.7 Risk factors for stem cell transplant recipients. Am J Respir Crit Care Med.
2002;166(5):641-645.
the development of DAH in bone marrow transplant 8. Zamora MR, Warner ML, Tuder R, Schwarz MI. Diffuse
recipients include older age, total body radiation, alveolar hemorrhage and systemic lupus erythematosus. Clinical
myeloablative conditioning regimens, and severe acute presentation, histology, survival, and outcome. Medicine
graft-vs-host disease.7,78 Clinically, these patients (Baltimore). 1997;76(3):192-202.
present with hemoptysis less frequently compared 9. Schwarz MI, Mortenson RL, Colby TV, et al. Pulmonary
capillaritis. The association with progressive irreversible
with other causes of DAH with a rate of approxi- airflow limitation and hyperinflation. Am Rev Respir Dis.
mately 15%.76,77 Protective strategies, such as reduc- 1993;148(2):507-511.
ing the intensity of the conditioning regimen, do not 10. Hunt DP, Weil R, Nicholson AG, Burke MM, Du Bois RM,
appear to decrease the risk of DAH.7 The pathogen- Wells AU. Pulmonary capillaritis and its relationship to
esis of DAH in bone marrow transplant recipients development of emphysema in hypocomplementaemic urti-
carial vasculitis syndrome. Sarcoidosis Vasc Diffuse Lung Dis.
has yet to be clearly established, but it has been 2006;23(1):70-72.
suggested that tissue injury, inflammation, and the 11. Jennings CA, King TE Jr, Tuder R, Cherniack RM, Schwarz MI.
associated cytokine release play important roles. Diffuse alveolar hemorrhage with underlying isolated, pauci-
Lung biopsy reveals diffuse alveolar damage and immune pulmonary capillaritis. Am J Respir Crit Care Med.
DAH.79 The majority of patients with DAH require 1997;155(3):1101-1109.
12. Ioachimescu OC, Sieber S, Kotch A. Idiopathic pulmonary
mechanical ventilation and corticosteroids are the haemosiderosis revisited. Eur Respir J. 2004;24(1):162-170.
mainstay of treatment, although their effectiveness 13. Kjellman B, Elinder G, Garwicz S, Svan H. Idiopathic pul-
remains uncertain.74,78 monary haemosiderosis in Swedish children. Acta Paediatr
Scand. 1984;73(5):584-588.
14. Green RJ, Ruoss SJ, Kraft SA, Duncan SR, Berry GJ, Raffin TA.
Summary Pulmonary capillaritis and alveolar hemorrhage. Update on
diagnosis and management. Chest. 1996;110(5):1305-1316.
DAH is a clinicopathologic syndrome that results 15. Franssen CF, Stegeman CA, Kallenberg CG, et al.
from a variety of conditions and should be considered Antiproteinase 3- and antimyeloperoxidase-associated vascu-
litis. Kidney Int. 2000;57(6):2195-2206.
a life-threatening event. Once believed to be a rare 16. Stone JH; Wegener’s Granulomatosis Etanercept Trial
syndrome, DAH is being recognized with increasing Research Group. Limited versus severe Wegener’s granu-
frequency. A systematic approach to early recognition, lomatosis: baseline data on patients in the Wegener’s
www.chestpubs.org CHEST / 137 / 5 / MAY, 2010 1169
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
Granulomatosis Etanercept Trial. Arthritis Rheum. 2003; 35. Cañas C, Tobón GJ, Granados M, Fernández L. Diffuse
48(8):2299-2309. alveolar hemorrhage in Colombian patients with systemic lupus
17. Rarok AA, Stegeman CA, Limburg PC, Kallenberg CG. erythematosus. Clin Rheumatol. 2007;26(11):1947-1949.
Neutrophil membrane expression of proteinase 3 (PR3) is 36. Matthay RA, Schwarz MI, Petty TL, et al. Pulmonary mani-
related to relapse in PR3-ANCA-associated vasculitis. J Am festations of systemic lupus erythematosus: review of twelve
Soc Nephrol. 2002;13(9):2232-2238. cases of acute lupus pneumonitis. Medicine (Baltimore).
18. van der Woude FJ, Rasmussen N, Lobatto S, et al. 1975;54(5):397-409.
Autoantibodies against neutrophils and monocytes: tool for 37. Boulware DW, Hedgpeth MT. Lupus pneumonitis and anti-
diagnosis and marker of disease activity in Wegener’s granu- SSA(Ro) antibodies. J Rheumatol. 1989;16(4):479-481.
lomatosis. Lancet. 1985;1(8426):425-429. 38. Churg A, Franklin W, Chan KL, Kopp E, Carrington CB.
19. Tervaert JW, van der Woude FJ, Fauci AS, et al. Association Pulmonary hemorrhage and immune-complex deposi-
between active Wegener’s granulomatosis and anticytoplas- tion in the lung. Complications in a patient with systemic
mic antibodies. Arch Intern Med. 1989;149(11):2461-2465. lupus erythematosus. Arch Pathol Lab Med. 1980;104(7):
20. Boomsma MM, Stegeman CA, van der Leij MJ, et al. 388-391.
Prediction of relapses in Wegener’s granulomatosis by mea- 39. Hoshi K, Matsuda M, Ishikawa M, et al. Successful treatment
surement of antineutrophil cytoplasmic antibody levels: a pro- of fulminant pulmonary hemorrhage associated with systemic
spective study. Arthritis Rheum. 2000;43(9):2025-2033. lupus erythematosus. Clin Rheumatol. 2004;23(3):252-255.
21. Sanders JS, Huitma MG, Kallenberg CG, Stegeman CA. 40. Cheema GS, Quismorio FP Jr. Interstitial lung disease
Prediction of relapses in PR3-ANCA-associated vasculi- in systemic lupus erythematosus. Curr Opin Pulm Med.
tis by assessing responses of ANCA titres to treatment. 2000;6(5):424-429.
Rheumatology (Oxford). 2006;45(6):724-729. 41. Badsha H, Teh CL, Kong KO, Lian TY, Chng HH. Pulmonary
22. Keogh KA, Ytterberg SR, Fervenza FC, Carlson KA, hemorrhage in systemic lupus erythematosus. Semin Arthritis
Schroeder DR, Specks U. Rituximab for refractory Wegener’s Rheum. 2004;33(6):414-421.
granulomatosis: report of a prospective, open-label pilot trial. 42. Schwarz MI, Sutarik JM, Nick JA, Leff JA, Emlen JW,
Am J Respir Crit Care Med. 2006;173(2):180-187. Tuder RM. Pulmonary capillaritis and diffuse alveolar hem-
23. Sugimoto T, Deji N, Kume S, et al. Pulmonary-renal syndrome, orrhage. A primary manifestation of polymyositis. Am J Respir
diffuse pulmonary hemorrhage and glomerulonephritis, asso- Crit Care Med. 1995;151(6):2037-2040.
ciated with Wegener’s granulomatosis effectively treated with 43. Schwarz MJK, Talmadge, E. Interstitial Lung Disease. 2nd
early plasma exchange therapy. Intern Med. 2007;46(1):49-53. ed. St. Louis, MO: Mosby-Year Book; 1993.
24. Nguyen T, Martin MK, Indrikovs AJ. Plasmapheresis for dif- 44. Tazelaar HD, Viggiano RW, Pickersgill J, Colby TV. Interstitial
fuse alveolar hemorrhage in a patient with Wegener’s granu- lung disease in polymyositis and dermatomyositis. Clinical
lomatosis: case report and review of the literature. J Clin features and prognosis as correlated with histologic findings.
Apher. 2005;20(4):230-234. Am Rev Respir Dis. 1990;141(3):727-733.
25. Klemmer PJ, Chalermskulrat W, Reif MS, Hogan SL, Henke 45. Griffin MT, Robb JD, Martin JR. Diffuse alveolar haemor-
DC, Falk RJ. Plasmapheresis therapy for diffuse alveolar hem- rhage associated with progressive systemic sclerosis. Thorax.
orrhage in patients with small-vessel vasculitis. Am J Kidney 1990;45(11):903-904.
Dis. 2003;42(6):1149-1153. 46. Nishi K, Myou S, Ooka T, Fujimura M, Matsuda T. Diffuse
26. Guillevin L, Durand-Gasselin B, Cevallos R, et al. Microscopic cutaneous systemic sclerosis associated with pan-serositis, dis-
polyangiitis: clinical and laboratory findings in eighty-five seminated intravascular coagulation, and diffuse alveolar hae-
patients. Arthritis Rheum. 1999;42(3):421-430. morrhage. Respir Med. 1994;88(6):471-473.
27. Lauque D, Cadranel J, Lazor R, et al. Microscopic polyangii- 47. Bar J, Ehrenfeld M, Rozenman J, Perelman M, Sidi Y, Gur H.
tis with alveolar hemorrhage. A study of 29 cases and review Pulmonary-renal syndrome in systemic sclerosis. Semin Arthritis
of the literature. Groupe d’Etudes et de Recherche sur les Rheum. 2001;30(6):403-410.
Maladies “Orphelines” Pulmonaires (GERM“O”P). Medicine 48. Horiki T, Fuyuno G, Ishii M, et al. Fatal alveolar hemorrhage
(Baltimore). 2000;79(4):222-233. in a patient with mixed connective tissue disease presenting
28. Schwarz MI, Brown KK. Small vessel vasculitis of the lung. polymyositis features. Intern Med. 1998;37(6):554-560.
Thorax. 2000;55(6):502-510. 49. Schwarz MI, Zamora MR, Hodges TN, Chan ED, Bowler RP,
29. Falk RJ, Nachman PH, Hogan SL, Jennette JC. ANCA glom- Tuder RM. Isolated pulmonary capillaritis and diffuse alveo-
erulonephritis and vasculitis: a Chapel Hill perspective. Semin lar hemorrhage in rheumatoid arthritis and mixed connective
Nephrol. 2000;20(3):233-243. tissue disease. Chest. 1998;113(6):1609-1615.
30. Xiao H, Schreiber A, Heeringa P, Falk RJ, Jennette JC. 50. Torralbo A, Herrero JA, Portolés J, Barrientos A. Alveolar
Alternative complement pathway in the pathogenesis of dis- hemorrhage associated with antineutrophil cytoplasmic
ease mediated by anti-neutrophil cytoplasmic autoantibodies. antibodies in rheumatoid arthritis. Chest. 1994;105(5):1590-
Am J Pathol. 2007;170(1):52-64. 1592.
31. Jayne D, Rasmussen N, Andrassy K, et al; European Vasculitis 51. Gertner E, Lie JT. Pulmonary capillaritis, alveolar hemor-
Study Group. A randomized trial of maintenance therapy for rhage, and recurrent microvascular thrombosis in primary
vasculitis associated with antineutrophil cytoplasmic autoanti- antiphospholipid syndrome. J Rheumatol. 1993;20(7):1224-
bodies. N Engl J Med. 2003;349(1):36-44. 1228.
32. Betensley AD, Yankaskas JR. Factor VIIa for alveolar hemor- 52. Asherson RA, Cervera R, Piette JC, et al. Catastrophic
rhage in microscopic polyangiitis. Am J Respir Crit Care Med. antiphospholipid syndrome. Clinical and laboratory features
2002;166(9):1291-1292. of 50 patients. Medicine (Baltimore). 1998;77(3):195-207.
33. Rojas-Serrano J, Pedroza J, Regalado J, et al. High prevalence 53. Gertner E. Diffuse alveolar hemorrhage in the antiphos-
of infections in patients with systemic lupus erythematosus pholipid syndrome: spectrum of disease and treatment.
and pulmonary haemorrhage. Lupus. 2008;17(4):295-299. J Rheumatol. 1999;26(4):805-807.
34. Santos-Ocampo AS, Mandell BF, Fessler BJ. Alveolar hem- 54. Wiedermann FJ, Mayr A, Schobersberger W, et al. Acute respi-
orrhage in systemic lupus erythematosus: presentation and ratory failure associated with catastrophic antiphospholipid
management. Chest. 2000;118(4):1083-1090. syndrome. J Intern Med. 2000;247(6):723-730.
1170 Recent Advances in Chest Medicine
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
55. Salama AD, Pusey CD. Immunology of anti-glomerular base- ents: treatment and effect on allograft function. J Heart Lung
ment membrane disease. Curr Opin Nephrol Hypertens. Transplant. 2005;24(12):2091-2097.
2002;11(3):279-286. 68. Magro CM, Klinger DM, Adams PW, et al. Evidence that
56. Donaghy M, Rees AJ. Cigarette smoking and lung haemor- humoral allograft rejection in lung transplant patients is
rhage in glomerulonephritis caused by autoantibodies to not histocompatibility antigen-related. Am J Transplant.
glomerular basement membrane. Lancet. 1983;2(8364):1390- 2003;3(10):1264-1272.
1393. 69. Magro CM, Deng A, Pope-Harman A, et al. Humorally medi-
57. Lazor R, Bigay-Gamé L, Cottin V, et al; Groupe d’Etudes ated posttransplantation septal capillary injury syndrome as a
et de Recherche sur les Maladies Orphelines Pulmonaires common form of pulmonary allograft rejection: a hypothesis.
(GERMOP); Swiss Group for Interstitial and Orphan Lung Transplantation. 2002;74(9):1273-1280.
Diseases (SIOLD). Alveolar hemorrhage in anti-basement 70. Sibley RK, Berry GJ, Tazelaar HD, et al. The role of trans-
membrane antibody disease: a series of 28 cases. Medicine bronchial biopsies in the management of lung transplant
(Baltimore). 2007;86(3):181-193. recipients. J Heart Lung Transplant. 1993;12(2):308-324.
58. Lombard CM, Colby TV, Elliott CG. Surgical pathology of 71. Robinson JA. Apheresis in thoracic organ transplantation.
the lung in anti-basement membrane antibody-associated Ther Apher. 1999;3(1):34-39.
Goodpasture’s syndrome. Hum Pathol. 1989;20(5):445-451. 72. Bittner HB, Dunitz J, Hertz M, Bolman MR III, Park SJ.
59. Magro CM, Morrison C, Pope-Harman A, Rothrauff SK, Hyperacute rejection in single lung transplantation—case
Ross P Jr. Direct and indirect immunofluorescence as a diag- report of successful management by means of plasmaphere-
nostic adjunct in the interpretation of nonneoplastic medical sis and antithymocyte globulin treatment. Transplantation.
lung disease. Am J Clin Pathol. 2003;119(2):279-289. 2001;71(5):649-651.
60. Mathew TH, Hobbs JB, Kalowski S, Sutherland PW, Kincaid- 73. Matulis M, High KP. Immune reconstitution after hematopoi-
Smith P. Goodpasture’s syndrome: normal renal diagnostic etic stem-cell transplantation and its influence on respiratory
findings. Ann Intern Med. 1975;82(2):215-218. infections. Semin Respir Infect. 2002;17(2):130-139.
61. Tobler A, Schürch E, Altermatt HJ, Im Hof V. Anti-basement 74. Afessa B, Peters SG. Chronic lung disease after hematopoi-
membrane antibody disease with severe pulmonary haemor- etic stem cell transplantation. Clin Chest Med. 2005;26(4):
rhage and normal renal function. Thorax. 1991;46(1):68-70. 571-586, vi.
62. Levy JB, Turner AN, Rees AJ, Pusey CD. Long-term out- 75. Lewis ID, DeFor T, Weisdorf DJ. Increasing incidence of dif-
come of anti-glomerular basement membrane antibody dis- fuse alveolar hemorrhage following allogeneic bone marrow
ease treated with plasma exchange and immunosuppression. transplantation: cryptic etiology and uncertain therapy. Bone
Ann Intern Med. 2001;134(11):1033-1042. Marrow Transplant. 2000;26(5):539-543.
63. Edwards JC, Szczepanski L, Szechinski J, et al. Efficacy of 76. Afessa B, Tefferi A, Litzow MR, Peters SG. Outcome of dif-
B-cell-targeted therapy with rituximab in patients with rheu- fuse alveolar hemorrhage in hematopoietic stem cell trans-
matoid arthritis. N Engl J Med. 2004;350(25):2572-2581. plant recipients. Am J Respir Crit Care Med. 2002;166(10):
64. Stasi R, Stipa E, Del Poeta G, Amadori S, Newland AC, 1364-1368.
Provan D. Long-term observation of patients with anti- 77. Gupta S, Jain A, Warneke CL, et al. Outcome of alveolar
neutrophil cytoplasmic antibody-associated vasculitis treated hemorrhage in hematopoietic stem cell transplant recipients.
with rituximab. Rheumatology (Oxford). 2006;45(11):1432- Bone Marrow Transplant. 2007;40(1):71-78.
1436. 78. Majhail NS, Parks K, Defor TE, Weisdorf DJ. Diffuse alveo-
65. Silverman GJ, Weisman S. Rituximab therapy and autoim- lar hemorrhage and infection-associated alveolar hemorrhage
mune disorders: prospects for anti-B cell therapy. Arthritis following hematopoietic stem cell transplantation: related and
Rheum. 2003;48(6):1484-1492. high-risk clinical syndromes. Biol Blood Marrow Transplant.
66. Badesch DB, Zamora M, Fullerton D, et al. Pulmonary capil- 2006;12(10):1038-1046.
laritis: a possible histologic form of acute pulmonary allograft 79. Roychowdhury M, Pambuccian SE, Aslan DL, et al. Pulmonary
rejection. J Heart Lung Transplant. 1998;17(4):415-422. complications after bone marrow transplantation: an autopsy
67. Astor TL, Weill D, Cool C, Teitelbaum I, Schwarz MI, study from a large transplantation center. Arch Pathol Lab
Zamora MR. Pulmonary capillaritis in lung transplant recipi- Med. 2005;129(3):366-371.
www.chestpubs.org CHEST / 137 / 5 / MAY, 2010 1171
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
Diffuse Alveolar Hemorrhage
Abigail R. Lara and Marvin I. Schwarz
Chest 2010;137; 1164-1171
DOI 10.1378/chest.08-2084
This information is current as of February 18, 2012
Updated Information & Services
Updated Information and services can be found at:
http://chestjournal.chestpubs.org/content/137/5/1164.full.html
References
This article cites 78 articles, 24 of which can be accessed free at:
http://chestjournal.chestpubs.org/content/137/5/1164.full.html#ref-list-1
Cited Bys
This article has been cited by 2 HighWire-hosted articles:
http://chestjournal.chestpubs.org/content/137/5/1164.full.html#related-urls
Permissions & Licensing
Information about reproducing this article in parts (figures, tables) or in its entirety can be
found online at:
http://www.chestpubs.org/site/misc/reprints.xhtml
Reprints
Information about ordering reprints can be found online:
http://www.chestpubs.org/site/misc/reprints.xhtml
Citation Alerts
Receive free e-mail alerts when new articles cite this article. To sign up, select the
"Services" link to the right of the online article.
Images in PowerPoint format
Figures that appear in CHEST articles can be downloaded for teaching purposes in
PowerPoint slide format. See any online figure for directions.
Downloaded from chestjournal.chestpubs.org by guest on February 18, 2012
© 2010 American College of Chest Physicians
You might also like
- 2010 Hemorragia Alveolar DifusaDocument8 pages2010 Hemorragia Alveolar DifusaCecilia Requejo TelloNo ratings yet
- Sdra Reconocimiento Actual 2021Document16 pagesSdra Reconocimiento Actual 2021NATHALY JOVANA CONTRERAS HERRERANo ratings yet
- Acute Respiratory Distress Syndrome - Background, Pathophysiology, EtiologyDocument5 pagesAcute Respiratory Distress Syndrome - Background, Pathophysiology, EtiologyARHNo ratings yet
- Pulmonary EmbolismDocument25 pagesPulmonary EmbolismRaymund VadilNo ratings yet
- "Imitators" of The ARDS Implications For Diagnosis and Treatment Acute Lung Injury (ALI) and ARDS (ALI/ARDS)Document22 pages"Imitators" of The ARDS Implications For Diagnosis and Treatment Acute Lung Injury (ALI) and ARDS (ALI/ARDS)Odett EzzatNo ratings yet
- Hemoptysis Diagnosis and ManagementDocument9 pagesHemoptysis Diagnosis and ManagementSYAFIRA LAILA NURULITANo ratings yet
- Transfusion-Related Acute Lung Injury - StatPearls - NCBI BookshelfDocument5 pagesTransfusion-Related Acute Lung Injury - StatPearls - NCBI Bookshelfindahmsafitri3No ratings yet
- Acute Respiratory Distress SyndromeDocument21 pagesAcute Respiratory Distress Syndromemisseve252100% (1)
- ARDS EngDocument25 pagesARDS EngTofik ShehajNo ratings yet
- Acute Pulmonary Edema - NEJMDocument4 pagesAcute Pulmonary Edema - NEJMSuzika Dewi0% (1)
- Congenital Diaphragmatic Hernia: Review Open AccessDocument15 pagesCongenital Diaphragmatic Hernia: Review Open AccessPutri YingNo ratings yet
- Emergency Department Guide to Diagnosing and Treating Pleural DiseaseDocument25 pagesEmergency Department Guide to Diagnosing and Treating Pleural DiseaseEdgardo Vargas AlvarezNo ratings yet
- SDL 18 Interstitial Lung Disease BMS16091064Document8 pagesSDL 18 Interstitial Lung Disease BMS16091064Jonathan YeohNo ratings yet
- Hamman Rich SyndromeDocument7 pagesHamman Rich SyndromeGerardo Armando EsparzaNo ratings yet
- Hypoxemic Resp. FailureDocument52 pagesHypoxemic Resp. FailureLovely Acabado TampocoNo ratings yet
- ID Faktor Faktor Yang Berhubungan Dengan Buang Air Besar Di Jamban Di Desa GunungsaDocument14 pagesID Faktor Faktor Yang Berhubungan Dengan Buang Air Besar Di Jamban Di Desa GunungsaRSU DUTA MULYANo ratings yet
- Ards 2Document7 pagesArds 2LUCIBELLOT1No ratings yet
- Congenital Diaphragmatic Hernia: Orphanet Journal of Rare Diseases January 2012Document16 pagesCongenital Diaphragmatic Hernia: Orphanet Journal of Rare Diseases January 2012danny anantaNo ratings yet
- Srda 2016 PDFDocument14 pagesSrda 2016 PDFGeibel Reis JrNo ratings yet
- Pulmonary Edema - StatPearls - NCBI BookshelfDocument7 pagesPulmonary Edema - StatPearls - NCBI BookshelfriyanasirNo ratings yet
- Fisiopatologia de SDRADocument19 pagesFisiopatologia de SDRARuben HerediaNo ratings yet
- ARDS: Acute Respiratory Distress Syndrome Pathophysiology & TreatmentDocument17 pagesARDS: Acute Respiratory Distress Syndrome Pathophysiology & TreatmentAnastasia CebotariNo ratings yet
- Symposium Papers: What Is The Acute Respiratory Distress Syndrome?Document7 pagesSymposium Papers: What Is The Acute Respiratory Distress Syndrome?Zulkifli SalimNo ratings yet
- Transfusion-Related Acute Lung Injury (Trali) : Description and IncidenceDocument9 pagesTransfusion-Related Acute Lung Injury (Trali) : Description and IncidenceNanda SilvaNo ratings yet
- Noncardiogenic Pulmonary EdemaDocument19 pagesNoncardiogenic Pulmonary EdemaCláudio CalixtoNo ratings yet
- Imaging findings of pulmonary edema: Part 1. Cardiogenic pulmonary edema and acute respiratory distress syndromeDocument11 pagesImaging findings of pulmonary edema: Part 1. Cardiogenic pulmonary edema and acute respiratory distress syndromeOlivia Chandra DeviNo ratings yet
- Dr. Rajmani: Assistant Professor Department of Medicine J.L.N. Medical College, Ajmer (Raj.)Document63 pagesDr. Rajmani: Assistant Professor Department of Medicine J.L.N. Medical College, Ajmer (Raj.)Ashish SoniNo ratings yet
- Pleural Effusion in Adults—Etiology, Diagnosis, and Treatment (24.05.2019)Document10 pagesPleural Effusion in Adults—Etiology, Diagnosis, and Treatment (24.05.2019)lordiroh1No ratings yet
- SiñomulmonDocument14 pagesSiñomulmonDra Daphne Rivero GallegosNo ratings yet
- Interstitial Lung DiseasesDocument80 pagesInterstitial Lung Diseasespavithranmbbs100% (1)
- Pulmonary Hemorrhage-1Document20 pagesPulmonary Hemorrhage-1ELDHOSE RAJUNo ratings yet
- Massive Hemoptysis: Resident Grand RoundsDocument7 pagesMassive Hemoptysis: Resident Grand RoundsEko CahyonoNo ratings yet
- Pi Is 0749070421000439Document21 pagesPi Is 0749070421000439Vlady78No ratings yet
- COPD and Pulmonary Thromboembolism (For Galley Proof)Document6 pagesCOPD and Pulmonary Thromboembolism (For Galley Proof)Ram AdhikariNo ratings yet
- Acute Respiratory Distress SyndromeDocument17 pagesAcute Respiratory Distress SyndromeSanjeet SahNo ratings yet
- 44 PulmonaryhemorrhageDocument7 pages44 PulmonaryhemorrhageGreen HanauNo ratings yet
- Rare and Interesting Cases in Pulmonary MedicineFrom EverandRare and Interesting Cases in Pulmonary MedicineRating: 4 out of 5 stars4/5 (1)
- Patrones Tomograficos Epid PDFDocument28 pagesPatrones Tomograficos Epid PDFYony Morales LeonNo ratings yet
- Pulmonary HemorrhageDocument6 pagesPulmonary HemorrhageSubas SharmaNo ratings yet
- The Acute Respiratory Distress Syndrome: Review SeriesDocument10 pagesThe Acute Respiratory Distress Syndrome: Review Seriesadek07No ratings yet
- ARDS and Pul Edema SeminarDocument48 pagesARDS and Pul Edema SeminaryohannesNo ratings yet
- Diagnosis and Treatment of Diffuse Interstitial Lung DiseasesDocument21 pagesDiagnosis and Treatment of Diffuse Interstitial Lung Diseaseswajeeh rehmanNo ratings yet
- Thorax00193 0009 PDFDocument10 pagesThorax00193 0009 PDFhotmart ventasNo ratings yet
- 712 PDFDocument74 pages712 PDFAnonymous h0DxuJTNo ratings yet
- Congenital Lobar EmphysemaDocument3 pagesCongenital Lobar Emphysemamadimadi11No ratings yet
- Edema Pulmo JurnalDocument14 pagesEdema Pulmo JurnalOlivia Chandra DeviNo ratings yet
- Presentasi Radiologi Edema ParuDocument19 pagesPresentasi Radiologi Edema ParuFia100% (1)
- Acute Respiratory Distress SyndromeDocument77 pagesAcute Respiratory Distress SyndromeAnnisa Dyah ChairiniNo ratings yet
- Pulmonary Embolism and Deep Vein Thrombosis: ArticleDocument13 pagesPulmonary Embolism and Deep Vein Thrombosis: ArticleSeriana Kombong DatuNo ratings yet
- handa2018Document18 pageshanda2018rocio enriquezNo ratings yet
- Pulmonary Edema II: Noncardiogenic Pulmonary EdemaDocument31 pagesPulmonary Edema II: Noncardiogenic Pulmonary EdemaGita Helvia SariNo ratings yet
- How Does COPD Differ From AsthmaDocument2 pagesHow Does COPD Differ From AsthmaRenz AducaNo ratings yet
- Acute Pulmonary OdemaDocument9 pagesAcute Pulmonary OdemaAnonymous ysrxggk21cNo ratings yet
- Saddle Pulmonary Embolism: A Rare Case of Proximal Pulmonary EmbolismDocument3 pagesSaddle Pulmonary Embolism: A Rare Case of Proximal Pulmonary EmbolismIJAR JOURNALNo ratings yet
- Noncardiogenic Pulmonary Edema in Small AnimalsDocument17 pagesNoncardiogenic Pulmonary Edema in Small AnimalsKaren PMNo ratings yet
- Fluid Therapy and Acute Respiratory Distress Syndrome: Jisoo Lee,, Keith Corl,, Mitchell M. LevyDocument9 pagesFluid Therapy and Acute Respiratory Distress Syndrome: Jisoo Lee,, Keith Corl,, Mitchell M. LevyLuis HernándezNo ratings yet
- Acute Respiratory Distress Syndrome: Pathophysiology and Therapeutic OptionsDocument10 pagesAcute Respiratory Distress Syndrome: Pathophysiology and Therapeutic OptionsviviNo ratings yet
- Non-Cardiogenic Pulmonary EdemaDocument7 pagesNon-Cardiogenic Pulmonary EdemadarmariantoNo ratings yet
- Definition of Noncardiogenic Pulmonary Edemanoncardiogenic Pulmonary Edema Is IdentifiedDocument35 pagesDefinition of Noncardiogenic Pulmonary Edemanoncardiogenic Pulmonary Edema Is IdentifiedAya EyadNo ratings yet
- POLIN 2009_Bubble CPAP- A Clash of Science Culture and ReligionDocument2 pagesPOLIN 2009_Bubble CPAP- A Clash of Science Culture and ReligionRafael JustinoNo ratings yet
- MIEDEMA 2013_Effect of Nasal Continuous and Biphasic Positive Airway Pressure on Lung Volume in Preterm InfantsDocument7 pagesMIEDEMA 2013_Effect of Nasal Continuous and Biphasic Positive Airway Pressure on Lung Volume in Preterm InfantsRafael JustinoNo ratings yet
- GUPTA 2009_A RCT of post extubation BCPAP versus infant flow driver CPAP in preterm infants with RDSDocument8 pagesGUPTA 2009_A RCT of post extubation BCPAP versus infant flow driver CPAP in preterm infants with RDSRafael JustinoNo ratings yet
- BURG 2014_Cross-sectional changes in lung volume measured by electrical impedance tomography are representative for the whole lung in ventilated preterm infantsDocument8 pagesBURG 2014_Cross-sectional changes in lung volume measured by electrical impedance tomography are representative for the whole lung in ventilated preterm infantsRafael JustinoNo ratings yet
- ORENSTEIN 2002_Cystic fibrosis- A 2002 updateDocument9 pagesORENSTEIN 2002_Cystic fibrosis- A 2002 updateRafael JustinoNo ratings yet
- ALVIRA 2017_Can We Understand the Pathobiology of Bronchopulmonary DysplasiaDocument11 pagesALVIRA 2017_Can We Understand the Pathobiology of Bronchopulmonary DysplasiaRafael JustinoNo ratings yet
- HOUGH 2014_Lung recruitment and endotracheal suction in ventilated preterm infants measured with electrical impedance tomographyDocument7 pagesHOUGH 2014_Lung recruitment and endotracheal suction in ventilated preterm infants measured with electrical impedance tomographyRafael JustinoNo ratings yet
- NARASIMHAN_Pulmonary haemorrhage in neonatesDocument3 pagesNARASIMHAN_Pulmonary haemorrhage in neonatesRafael JustinoNo ratings yet
- BIBAN 2012_Exogenous surfactant replacement- how to deliver itDocument6 pagesBIBAN 2012_Exogenous surfactant replacement- how to deliver itRafael JustinoNo ratings yet
- NEWHOUSE 1999_Asthma therapy with aerosolsDocument4 pagesNEWHOUSE 1999_Asthma therapy with aerosolsRafael JustinoNo ratings yet
- MIEDEMA 2011_Changes in lung volume and ventilation during surfactant treatment in ventilated preterm infantsDocument6 pagesMIEDEMA 2011_Changes in lung volume and ventilation during surfactant treatment in ventilated preterm infantsRafael JustinoNo ratings yet
- SOLALIGUE 2017 - 1 Recent Advances in Our Understanding of The Mechanisms of Late Lunf Development and BPDDocument190 pagesSOLALIGUE 2017 - 1 Recent Advances in Our Understanding of The Mechanisms of Late Lunf Development and BPDRafael JustinoNo ratings yet
- LISTA 2012_Surfactant and mechanical ventilationDocument3 pagesLISTA 2012_Surfactant and mechanical ventilationRafael JustinoNo ratings yet
- BURG 2016_Effect of Minimally Invasive Surfactant Therapy on Lung Volume and Ventilation in Preterm InfantsDocument6 pagesBURG 2016_Effect of Minimally Invasive Surfactant Therapy on Lung Volume and Ventilation in Preterm InfantsRafael JustinoNo ratings yet
- Uropean Consensus Guidelines On The Management of Respiratory Distress Syndrome: 2022 UpdateDocument21 pagesUropean Consensus Guidelines On The Management of Respiratory Distress Syndrome: 2022 UpdateLuis Ruelas SanchezNo ratings yet
- neuroprotective MgSO4Document6 pagesneuroprotective MgSO4Rafael JustinoNo ratings yet
- ISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary DysplasiaDocument9 pagesISAYAMA 2017 - Revisiting The Definition of Bronchopulmonary DysplasiaRafael JustinoNo ratings yet
- Ultrasound in Obstet Gyne - 2002 - Laudy - The Fetal Lung 1 Developmental AspectsDocument7 pagesUltrasound in Obstet Gyne - 2002 - Laudy - The Fetal Lung 1 Developmental AspectsRafael JustinoNo ratings yet
- LCP4805-mc Mehta Vs Union of IndiaDocument60 pagesLCP4805-mc Mehta Vs Union of Indiatech hutNo ratings yet
- Is College For Everyone - RevisedDocument5 pagesIs College For Everyone - Revisedapi-295480043No ratings yet
- NCP For Ineffective Airway ClearanceDocument3 pagesNCP For Ineffective Airway ClearanceJennelyn BayleNo ratings yet
- Economics I Course Manual 2022Document13 pagesEconomics I Course Manual 2022Mridula BansalNo ratings yet
- Human, AGV or AIV? An Integrated Framework For Material Handling System Selection With Real-World Application in An Injection Molding FacilityDocument10 pagesHuman, AGV or AIV? An Integrated Framework For Material Handling System Selection With Real-World Application in An Injection Molding FacilitymertikNo ratings yet
- Swift Group Technical HandbookDocument8 pagesSwift Group Technical HandbookLukasz WilkNo ratings yet
- AISD Fees Structure for 2023-24 Academic YearDocument2 pagesAISD Fees Structure for 2023-24 Academic YearKawsar AlamNo ratings yet
- Gept reading試題Document13 pagesGept reading試題Bateman Patrick100% (1)
- Bankable Project FinalDocument32 pagesBankable Project FinalSanjay Baria0% (1)
- 07 - Toshkov (2016) Theory in The Research ProcessDocument29 pages07 - Toshkov (2016) Theory in The Research ProcessFerlanda LunaNo ratings yet
- Trollbloods Warmachine/Hordes Cross StitchDocument8 pagesTrollbloods Warmachine/Hordes Cross StitchGraeme DawsonNo ratings yet
- Virtualization Types: OS, Hardware Emulation, and ParavirtualizationDocument7 pagesVirtualization Types: OS, Hardware Emulation, and ParavirtualizationvinoopnvNo ratings yet
- Importance of Education: March 2015Document4 pagesImportance of Education: March 2015AswiniieNo ratings yet
- Quiz Microeconomics BECO201 Date 30/10/2017 Name: IDDocument5 pagesQuiz Microeconomics BECO201 Date 30/10/2017 Name: IDAA BB MMNo ratings yet
- Metrology Instruments Calibration Guide: Mitutoyo Asia PacificDocument6 pagesMetrology Instruments Calibration Guide: Mitutoyo Asia PacificLuis Eduardo García MaltosNo ratings yet
- B&A Performance AnalysisDocument16 pagesB&A Performance AnalysisNathalia Caroline100% (1)
- Women in PoliticsDocument13 pagesWomen in PoliticsMusa M. KamaraNo ratings yet
- BuellRetailCatalog en USDocument76 pagesBuellRetailCatalog en USErcüment Kayacık100% (2)
- The Irish Light 10Document28 pagesThe Irish Light 10Twinomugisha Ndinyenka RobertNo ratings yet
- Value-Added ProductsDocument7 pagesValue-Added ProductsTendai MutisiNo ratings yet
- 515 AMA Must DO QuestionsDocument217 pages515 AMA Must DO QuestionsVenkataRajuNo ratings yet
- M 003927Document78 pagesM 003927Eder RinasNo ratings yet
- DK1. 03. VERB Present - To Be - Talking About Yourself, NumbersDocument4 pagesDK1. 03. VERB Present - To Be - Talking About Yourself, NumbersTL TLNo ratings yet
- Flexible Architectural Design and User Participation: January 2012Document5 pagesFlexible Architectural Design and User Participation: January 2012amlaNo ratings yet
- Group Arrival ProceduresDocument3 pagesGroup Arrival Proceduresashlesha thopteNo ratings yet
- Document PDFDocument16 pagesDocument PDFnelson_herreraNo ratings yet
- (RHSA 124) : Monitoring and Managing Linux ProcessesDocument56 pages(RHSA 124) : Monitoring and Managing Linux ProcessesRomeo SincereNo ratings yet
- PESTLE analysis of M&S UK retail challengesDocument1 pagePESTLE analysis of M&S UK retail challengesMac Corleone0% (1)
- A Detailed Lesson Plan in English 10: Prepared By: Aira C. Mirandilla L. ObjectivesDocument11 pagesA Detailed Lesson Plan in English 10: Prepared By: Aira C. Mirandilla L. ObjectivesMae Mallapre100% (10)
- 1 Vkip 113Document595 pages1 Vkip 113flopo72No ratings yet