Professional Documents
Culture Documents
TP 6
TP 6
Uploaded by
sri noviantiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TP 6
TP 6
Uploaded by
sri noviantiCopyright:
Available Formats
MINIREVIEW
crossm
Mycobacterial Taxonomy
Betty A. Forbes
Department of Pathology, Virginia Commonwealth University Medical Center, Richmond, Virginia, USA
ABSTRACT This article summarizes the most recent (since 2012) taxonomic changes
in the genus Mycobacterium. Only those mycobacteria that have been isolated from Accepted manuscript posted online 7
December 2016
human specimens are included in this summary.
Citation Forbes BA. 2017. Mycobacterial
KEYWORDS human specimens, mycobacteria, taxonomy taxonomy. J Clin Microbiol 55:380 –383. https://
doi.org/10.1128/JCM.01287-16.
Editor Colleen Suzanne Kraft, Emory University
C urrently, there are over 170 recognized species of Mycobacterium, the only genus
in the family Mycobacteriaceae. Organisms belonging to this genus are quite
diverse with respect to their ability to cause disease in humans; some are strict
Copyright © 2017 American Society for
Microbiology. All Rights Reserved.
Address correspondence to baforbes@vcu.edu.
pathogens, while others are opportunistic pathogens or nonpathogenic. Similar to
other major groups of bacteria, the mycobacteria have undergone an extraordinary
expansion in the number of different species over the last 2 decades, due in large part
to the discriminatory power of gene sequencing, which phenotypic methods cannot
achieve. This discriminatory power is such that phenotypic traits, i.e., biochemical and
cultural characteristics, are no longer acceptable for the identification of mycobacteria.
Paralleling the increasing number of mycobacterial species, infections caused by the
nontuberculous mycobacteria (NTM), in particular, are also increasing on a worldwide
level (1). For laboratories identifying mycobacteria isolated from clinical specimens, it is
essential that these organisms are accurately identified for proper clinical management.
As more clinical laboratories use molecular or other methods, such as mass spectrom-
etry, for identification, our understanding of clinical significance will change and evolve
as the number of case reports regarding the “new” species increase; it may well be that
Downloaded from https://journals.asm.org/journal/jcm on 15 March 2024 by 114.125.217.38.
the role of many of the newly described mycobacterial species has been underesti-
mated either because of misidentification or because the species were unrecognized.
Toward this end, it is imperative for clinical microbiologists to keep up to date with the
rapidly evolving taxonomy of the mycobacteria. The intent of this minireview is to
provide a single reference for diagnostic laboratories regarding new, clinically relevant
changes in taxonomy pertaining to the genus Mycobacterium.
METHODS
Only those newly recognized mycobacterial species recovered from human clinical
material and reported between January 2012 and December 2015 are summarized
here. These new species were identified using a combination of reference materials. A
valuable resource was the List of Prokaryotic Names with Standing in Nomenclature
(http://www.bacterio.net/-allnamesmr.html). In addition, a combination of reference
materials was used, including the Manual of Clinical Microbiology, 11th edition, chapters
30 through 32; the International Journal of Systematic and Evolutionary Microbiology;
and the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed), using “nov. sp.
Mycobacterium” as the search term.
RESULTS
Table 1 summarizes new Mycobacterium species identified between January 2012
and December 2015. For each species, the human source(s) from which the new species
was isolated, its clinical relevance, and noteworthy growth characteristics are noted. In
addition, information on whether 16S rRNA gene sequencing identified the species is
February 2017 Volume 55 Issue 2 Journal of Clinical Microbiology jcm.asm.org 380
Minireview Journal of Clinical Microbiology
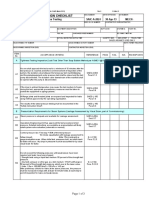
TABLE 1 New mycobacterial species (family: Mycobacteriaceae) recovered between January 2012 and December 2015
Unique 16S
rRNA gene? If
not, gene
Scientific name (year sequence
identified) Sourcea Clinical relevance Growth characteristics alternative References
M. alsense (2015) Sputum Infection Slow grower; weak yellow pigment Yes 2, 3
on Lowenstein Jensen medium,
not Middlebrook 7H11; most
closely related to M. szulgai and
M. malmoense
M. celeriflavum (2015) Sputum Undetermined; colonizer Rapid grower; scotochromogen Yes 1, 4
(rough, pale yellow); most
closely related to M. flavescens
and M. novocastrense
M. engbaekii (2013) Urine, gastric wash fluid, Undetermined; colonizer Slow grower; most closely related Yes 1, 5
bronchial aspirate to M. terrae complex (namely, M.
hiberniae); pigmented (some
show pink photochromogenic
pigmentation)
M. fragae (2013) Sputum Undetermined; colonizer Slow grower; smooth colonies, Yes 1, 6
unpigmented; closely related to
M. celatum
“M. franklinii”b (2015) Respiratory tract, skin, Infection; colonizer Rapid grower; nonpigmented; No; rpoB, hsp65 1, 7, 8
granulomatous liver closely related to M.
lesion, central line chelonae/abscessus
infection
“M. fukienense”b (2013) Respiratory tract Undetermined; colonizer Rapid grower; nonpigmented; No; hsp65 1, 9
closely related to M.
chelonae/abscessus
M. heraklionense (2013) Respiratory: BAL and Undetermined; colonizer Slow grower; nonpigmented; Yes 1,5
sputum closely related to M. terrae
complex, namely, to M.
arupense; optimal growth temp
25–37°C
M. iranicum (2013) Sputum, BAL, CSF, hand Infection; colonizer Rapid grower; scotochromogen; Yes 1,10–14
wound, peritoneal closely related to M. gilvum
fluid
M. koreense (2012) Sputum Undetermined Slow grower; nonpigmented; Yes 1,15
Downloaded from https://journals.asm.org/journal/jcm on 15 March 2024 by 114.125.217.38.
closely related to M. triviale
M. longobardum (2013) Sputum, bone Respiratory, colonizer; Slow grower; most closely related Yes 1,5,16
osteomyelitis to M. terrae complex
M. paragordonae Sputum Undetermined Slow grower; scotochromogen; Yes 1,17
(2014) closely related to M. gordonae
M. parakoreense (2013) Sputum Undetermined Slow grower; yellow or Yes 1,18
nonpigmented; closely related to
M. koreense
M. yongonense (2013) Sputum, BAL, stool Infection; colonizer Slow grower; nonpigmented; No; hsp65 1,19,20
closely related to M.
intracellulare
aBAL, bronchoalveolar lavage fluid; CSF, cerebrospinal fluid.
bCurrently a nonvalidated species.
included. In addition, brief summaries of case reports for some of the new species are
provided in Table 2.
DISCUSSION
Accurate identification of the mycobacteria is a challenge, particularly in light of the
extraordinary number of species in the genus. It has become clear that identification of
mycobacteria based on phenotypic and culture traits is poorly reproducible, time
consuming, and lacking in sufficient discriminatory power (21). As a result, this ap-
proach to mycobacterial identification has been abandoned for the most part. Al-
though the introduction of numerous new species over recent years might seem
daunting to clinical laboratories that identify mycobacteria, accurate identification is
February 2017 Volume 55 Issue 2 jcm.asm.org 381
Minireview Journal of Clinical Microbiology
TABLE 2 Brief summaries of clinical case reports for new Mycobacterium species
Organism Infections Reference
M. alsense Bronchopneumonia in two 70-yr-old subjects; both responded to antimycobacterial therapy 2
“M. franklinii” Although 26 clinical isolates were obtained, medical histories were provided for only 6 7
patients; 2 patients had sinusitis, and 4 patients had lower respiratory tract symptoms; all
patients with respiratory tract symptoms had underlying pulmonary disease
M. iranicum Isolated 3 times from the hand wound of an 18-yr-old male with a history of long-term steroid 10
treatment due to renal transplantation; treated with amikacin and clinically improved
An organism grew from culture of a BAL specimen from a 60-yr-old female with pneumonia; 10
patient responded to amikacin and ciprofloxacin
Peritoneal dialysis-related peritonitis in a 68-yr-old male with diabetic nephropathy who 13
responded to appropriate antimycobacterial therapy
HIV-infected patient admitted initially with mild fever, wt loss, chronic chest pain, and 14
nonproductive cough; no AFBa smear was done; patient’s fever and chest pain remained
unchanged; after bronchoscopy, 2 of 3 BAL specimens were AFB smear positive, and 3 of 3
were culture positive for a rapidly growing mycobacterium; a standard antituberculosis
regimen was started, but patient did not improve; after 1 mo, a sputum specimen was
negative for AFB, and 1 BAL specimen was positive by microscopy and culture for M.
iranicum; patient improved rapidly on amikacin and ciprofloxacin for 3 mo
M. longobardum Osteomyelitis of the elbow in a 71-yr-old male 14
M. yongonense First description of the species and its association with pulmonary infection, from the sputum 19
of a patient with unspecified lung disease, was in South Korea
74-yr-old woman presented with fatigue, diarrhea, and wt loss; chest x-ray revealed a cavitary 20
lesion; cultures of sputum and stool grew M. yongonense; a BAL specimen was also AFB
smear positive and grew the same organism
aAFB, acid-fast bacilli.
critical for proper diagnosis and management of infections and for outbreak investi-
gation.
This need was illustrated in recent reports of serious infections in patients who had
undergone open cardiac surgery in which a contaminated heater-cooler device was
used during extracorporeal circulation. These infections, occurring in patients in Europe
and the United States, were caused by Mycobacterium chimaera, a nontuberculous
mycobacterium ubiquitous in soil and water (22). This organism is a slow-growing NTM
species included in the M. avium complex (MAC). Initially, strains of this organism were
identified by a commercial probe assay as Mycobacterium intracellulare. In-depth inves-
Downloaded from https://journals.asm.org/journal/jcm on 15 March 2024 by 114.125.217.38.
tigation of these strains in 2004 revealed that the organisms were in fact distinct from
M. intracellulare and belonged to a previously unidentified species within the MAC,
namely, M. chimaera (23). Without delineation of this new species, this organism might
have been misidentified and recognition of its association with heater-cooler devices in
the operating room possibly delayed. Despite the already large number of species of
this genus, there is little doubt that this number will continue to increase and that some
newly described species will be recognized to cause infection in humans.
REFERENCES
1. Tortoli E. 2014. Microbiological features and clinical relevance of new bacterium isolated from clinical specimens. Int J Syst Evol Microbiol
species of the genus Mycobacterium. Clin Microbiol Rev 27:727–752. 65:510 –515. https://doi.org/10.1099/ijs.0.064832-0.
https://doi.org/10.1128/CMR.00035-14. 5. Tortoli E, Gitti Z, Klenk HP, Lauria S, Mannino R, Mantegani P, Mariottini A,
2. Richter E, Tortoli E, Fischer A, Hendricks O, Engel R, Hillemann D, Neonakis I. 2013. Survey of 150 strains belonging to the Mycobacterium
Schubert S, Kristiansen JE. 2007. Mycobacterium alsiense, a novel, slowly terrae complex and description of Mycobacterium engbaekii sp. nov., Myco-
growing species isolated from two patients with pulmonary disease. J bacterium heraklionense sp. nov. and Mycobacterium longobardum sp. nov.
Clin Microbiol 45:3837–3839. https://doi.org/10.1128/JCM.01097-07. Int J Syst Evol Microbiol 63:401–411. https://doi.org/10.1099/ijs.0.038737-0.
3. Tortoli E, Richter E, Borroni E, Cabibbe AM, Capitolo E, Cittaro D, Engel R, 6. Ramos JP, Campos CE, Caldas PC, Ferreira NV, da Silva MV, Redner P,
Hendricks O, Hillemann D, Kristiansen JE, Mariottini A, Schubert S, Cirillo Campelo CL, Vale SF, Barroso EC, Medeiros RF, Montes FC, Galvao TC,
DM. 2016. Mycobacterium alsense sp. nov., a scotochromogenic slow Tortoli E. 2013. Mycobacterium fragae sp. nov., a non-chromogenic
grower isolated from clinical respiratory specimens. Int J Syst Evol species isolated from human respiratory specimens. Int J Syst Evol
Microbiol 66:450 – 456. https://doi.org/10.1099/ijsem.0.000744. Microbiol 63:2583–2587. https://doi.org/10.1099/ijs.0.046862-0.
4. Shahraki AH, Cavusoglu C, Borroni E, Heidarieh P, Koksalan OK, Cabibbe 7. Simmon KE, Brown-Elliott BA, Ridge PG, Durtschi JD, Mann LB, Slechta
AM, Hashemzadeh M, Mariottini A, Mostafavi E, Cittaro D, Feizabadi MM, ES, Steigerwalt AG, Moser BD, Whitney AM, Brown JM, Voelkerding KV,
Lazarevic D, Yaghmaei F, Molinari GL, Camaggi A, Tortoli E. 2015. Myco- McGowan KL, Reilly AF, Kirn TJ, Butler WR, Edelstein PH, Wallace RJ, Jr,
bacterium celeriflavum sp. nov., a rapidly growing scotochromogenic Petti CA. 2011. Mycobacterium chelonae-abscessus complex associated
February 2017 Volume 55 Issue 2 jcm.asm.org 382
Minireview Journal of Clinical Microbiology
with sinopulmonary disease, northeastern USA. Emerg Infect Dis 17: chromogenic species closely related to Mycobacterium triviale. Int J Syst
1692–1700. https://doi.org/10.3201/eid1709.101667. Evol Microbiol 62:1289 –1295. https://doi.org/10.1099/ijs.0.033274-0.
8. Lourenço Nogueira C, Simmon KE, Chimara E, Cnockaert M, Carlos 16. Hong SK, Sung JY, Lee HJ, Oh MD, Park SS, Kim EC. 2013. First case of
Palomino J, Martin A, Vandamme P, Brown-Elliott BA, Wallace R, Jr, Mycobacterium longobardum infection. Ann Lab Med 33:356 –359.
Cardoso Leao S. 2015. Mycobacterium franklinii sp. nov., a species closely https://doi.org/10.3343/alm.2013.33.5.356.
related to members of the Mycobacterium chelonae-Mycobacterium ab- 17. Kim BJ, Hong SH, Kook YH, Kim BJ. 2014. Mycobacterium paragordonae
scessus group. Int J Syst Evol Microbiol 65:2148 –2153. https://doi.org/ sp. nov., a slowly growing, scotochromogenic species closely related to
10.1099/ijs.0.000234. Nogueira). Mycobacterium gordonae. Int J Syst Evol Microbiol 64:39 – 45. https://
9. Zhang YY, Li YB, Huang MX, Zhao XQ, Zhang LS, Liu WE, Wan KL. 2013. doi.org/10.1099/ijs.0.051540-0.
Novel species including Mycobacterium fukienense sp. is found from 18. Kim BJ, Hong SH, Yu HK, Park YG, Jeong J, Lee SH, Kim SR, Kim K, Kook
tuberculosis patients in Fujian Province, China, using phylogenetic anal- YH, Kim BJ. 2013. Mycobacterium parakoreense sp. nov., a slowly growing
ysis of Mycobacterium chelonae/abscessus complex. Biomed Environ Sci non-chromogenic species related to Mycobacterium koreense, isolated
26:894 –901. from a human clinical specimen. Int J Syst Evol Microbiol 63:2301–2308.
10. Shojaei H, Daley C, Gitti Z, Hashemi A, Heidarieh P, Moore ER, Naser AD, https://doi.org/10.1099/ijs.0.045070-0.
19. Kim BJ, Math RK, Jeon CO, Yu HK, Park YG, Kook YH, Kim BJ. 2013.
Russo C, van Ingen J, Tortoli E. 2013. Mycobacterium iranicum sp. nov., a
Mycobacterium yongonense sp. nov., a slow-growing non-chromogenic
rapidly growing scotochromogenic species isolated from clinical speci-
species closely related to Mycobacterium intracellulare. Int J Syst Evol
mens on three different continents. Int J Syst Evol Microbiol 63:
Microbiol 63:192–199. https://doi.org/10.1099/ijs.0.037465-0.
1383–1389. https://doi.org/10.1099/ijs.0.043562-0.
20. Tortoli E, Mariottini A, Pierotti P, Simonetti TM, Rossolini GM. 2013.
11. Tan JL, Ng HF, Wee WY, Ang MY, Wong GJ, Ngeow YF, Choo SW. 2013.
Mycobacterium yongonense in pulmonary disease, Italy. Emerg Infect Dis
First whole-genome sequence of Mycobacterium iranicum, a newly re-
19:1902–1904.
ported mycobacterial species. Genome Announc 1:e00732-13. https:// 21. Springer B, Stockman L, Teschner K, Roberts GD, Böttger EC. 1996.
doi.org/10.1128/genomeA.00732-13. Two-laboratory collaborative study on identification of mycobacteria:
12. Balakrishnan N, Tortoli E, Engel SL, Breitschwerdt EB. 2013. Isolation of a molecular versus phenotypic methods. J Clin Microbiol 34:296 –303.
novel strain of Mycobacterium iranicum from a woman in the United States. 22. Perkins KM, Lawsin A, Hasan NA, Strong M, Halpin AL, Rodger RR, Moulton-
J Clin Microbiol 51:705–707. https://doi.org/10.1128/JCM.02560-12. Meissner H, Crist MB, Schwartz S, Marders J, Daley CL, Salfinger M, Perz JF.
13. Inagaki K, Mizutani M, Nagahara Y, Asan M, Masamoto D, Sawada O, 2016. Mycobacterium chimaera contamination of heater-cooler devices used
Aono A, Chikamatsu K, Mitarai S. 2016. Successful treatment of perito- in cardiac surgery—United States. MMWR Morb Mortal Wkly Rep 65:
neal dialysis-related peritonitis due to Mycobacterium iranicum. Intern 1117–1118. https://doi.org/10.15585/mmwr.mm6540a6.
Med 55:1929 –1931. https://doi.org/10.2169/internalmedicine.55.5219. 23. Tortoli E, Rindi L, Garcia MJ, Chiaradonna P, Dei R, Garzelli C, Kroppen-
14. Hashemi-Shahraki A, Azarpira S, Shojaei H, Hashemzadeh M, Tortoli E. 2013. stedt RM, Lari N, Mattei R, Mariottini A, Mazzarelli G, Murcia MI, Nanetti
Mycobacterium iranicum infection in HIV-infected patient, Iran. Emerg Infect A, Piccoli P, Scarparo C. 2004. Proposal to elevate the genetic variant
Dis 19:1696–1697. https://doi.org/10.3201/eid1910.130658. MAC-A, included in the Mycobacterium avium complex, to species rank
15. Kim BJ, Jeong J, Lee SH, Kim SR, Yu HK, Park YG, Kim KJ, Kook YH, Kim as Mycobacterium chimaera sp. nov. Int J Syst Evol Microbiol 54:
BJ. 2012. Mycobacterium koreense sp. nov., a slowly growing non- 1277–1285. https://doi.org/10.1099/ijs.0.02777-0.
Betty A. Forbes, Ph.D, is a professor of pathology and internal medicine and
director of the clinical microbiology laboratory at Virginia Commonwealth
University (VCU) Medical Center in Richmond, Virginia. She is a diplomate
of the American Board of Medical Microbiology and a fellow of the Ameri-
can Academy of Microbiology. She has been at VCU Medical Center since
Downloaded from https://journals.asm.org/journal/jcm on 15 March 2024 by 114.125.217.38.
2003. Previously, she served for 20 years as director of clinical microbiology
at Upstate Medical University in Syracuse, New York. Dr. Forbes graduated
from Northwestern University in 1970. She received her Ph.D. in medical
microbiology and immunology from the University of Oklahoma Health
Science Center in Oklahoma City, Oklahoma, and then completed a 2-year
American Board of Medical Microbiology-approved postdoctoral fellow-
ship program at the University of Michigan, St. Joseph Mercy Hospital, in
Ann Arbor, Michigan. Following her formal fellowship training, she held a
joint appointment with the Division of Infectious Disease, Department of
Internal Medicine, and the Clinical Microbiology Laboratory in the Depart-
ment of Pathology, University of Michigan as a research associate for 2 years.
Dr. Forbes has a special interest in mycobacteria and has published exten-
sively in diagnostics for clinical microbiology. She was an editor for Bailey
and Scott’s Diagnostic Microbiology and an editor in chief for Clinical Micro-
biology Reviews, and she has served as an editor for the Journal of Clinical
Microbiology since 2009.
February 2017 Volume 55 Issue 2 jcm.asm.org 383
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Process - Quality Liposomal CDocument7 pagesProcess - Quality Liposomal Crmans100% (1)
- Main Idea: Multiple ChoiceDocument1 pageMain Idea: Multiple ChoiceHartonoNo ratings yet
- Plutonium by Controlled-Potential Coulometry: Standard Test Method ForDocument9 pagesPlutonium by Controlled-Potential Coulometry: Standard Test Method Forastewayb_964354182No ratings yet
- Vaccination Act, 1919Document6 pagesVaccination Act, 1919owuraniNo ratings yet
- Spectroscopy Catalog 2018-19Document220 pagesSpectroscopy Catalog 2018-19Juan alberto Ganoza GarciaNo ratings yet
- SAIC-A-2024 Rev 6 Leakness Tightness TestDocument3 pagesSAIC-A-2024 Rev 6 Leakness Tightness Testpookkoya thangalNo ratings yet
- Solar Tredmil BicycleDocument19 pagesSolar Tredmil BicycleIshwarjit SinghNo ratings yet
- Compact Stainless Steel Water Regulators Specification SheetDocument2 pagesCompact Stainless Steel Water Regulators Specification SheetWattsNo ratings yet
- (23007451 - Special Matrices) Best Linear Unbiased Estimation For Varying Probability With and Without Replacement SamplingDocument14 pages(23007451 - Special Matrices) Best Linear Unbiased Estimation For Varying Probability With and Without Replacement Samplingjedielso salesNo ratings yet
- 400e 1M PDFDocument4 pages400e 1M PDFLuis RolaNo ratings yet
- Youth Obtain DR Eta 0you Obtained0 WhitDocument350 pagesYouth Obtain DR Eta 0you Obtained0 Whitanonkid100% (1)
- Neurologist Deborah Boland, D.O., MSPT, Named "Physician of The Year"Document3 pagesNeurologist Deborah Boland, D.O., MSPT, Named "Physician of The Year"PR.comNo ratings yet
- Minimizing Error, Maximizing Outcome: The Physician Worklife Study IIDocument34 pagesMinimizing Error, Maximizing Outcome: The Physician Worklife Study IIjuanita_959870013No ratings yet
- Chemistry Viva Questions PDFDocument6 pagesChemistry Viva Questions PDFshubhraNo ratings yet
- Arg Hydr Aufzuege 300 FL 9010501 enDocument20 pagesArg Hydr Aufzuege 300 FL 9010501 enthrivenNo ratings yet
- Account Opening Form: Part-I: Branch To Affix Rubber Stamp of Name and Code NoDocument1 pageAccount Opening Form: Part-I: Branch To Affix Rubber Stamp of Name and Code NoDr. Gollapalli NareshNo ratings yet
- Semana 6 - ExpoDocument6 pagesSemana 6 - Exporosario marcelaNo ratings yet
- Spe 129157 MsDocument16 pagesSpe 129157 MsFelipe BañosNo ratings yet
- Disinfectants Meeting British Standard As of 23 July 2012Document3 pagesDisinfectants Meeting British Standard As of 23 July 2012karen_meadows2782No ratings yet
- Pluggable Connection System picoMAX 60295981Document92 pagesPluggable Connection System picoMAX 60295981Cudritescu VictorNo ratings yet
- Biology Chapter 2 Sexual Reproduction in Flowering PlantsDocument8 pagesBiology Chapter 2 Sexual Reproduction in Flowering PlantsYasir SalahNo ratings yet
- Emmanuel Torres CV.Document4 pagesEmmanuel Torres CV.Mathew Cedeño AvellanNo ratings yet
- Article 14 - Equality Before LawDocument7 pagesArticle 14 - Equality Before LawSri MuganNo ratings yet
- Sci Sum No. 4 (2nd Grading)Document20 pagesSci Sum No. 4 (2nd Grading)Paul Aldrin OlaeraNo ratings yet
- Novel Surgical Approach To AcalvariaDocument2 pagesNovel Surgical Approach To AcalvariaKezia Rachellea MustakimNo ratings yet
- Spool 2Document437 pagesSpool 2swapnil_mahalleNo ratings yet
- IOT Based Accident Detection and PreventionDocument6 pagesIOT Based Accident Detection and PreventionShivani PatilNo ratings yet
- Iso7235 Silencer MeasurementDocument19 pagesIso7235 Silencer Measurementlongkt29No ratings yet
- Risk AssessmentDocument8 pagesRisk AssessmentSubhransu Mohapatra50% (2)
- Tarea 3 de Ingles IIDocument6 pagesTarea 3 de Ingles IINelly SalcedoNo ratings yet