Professional Documents
Culture Documents
Perineal Diseases
Uploaded by
Yalin Abouhassira0 ratings0% found this document useful (0 votes)
2 views4 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views4 pagesPerineal Diseases
Uploaded by
Yalin AbouhassiraCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
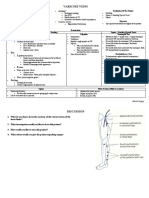
PERINEAL DISEASES
Disease Etiopathogenesis Clinical Diagnosis Treatment
Haemorrhoids dilated veins of the Degrees: Conservative therapy
arteriovenous blood vessels & I degree – falls into the lumen of anoscope • Bowel movement correction
connective tissue in the anal (diet, habits)
canal that may abnormally II degree – drops out during • Anal hygiene
enlarge or protrude. bowel movements, goes back in on its own • Medications:
o Anal lubrication
Etiopathogenesis III degree – drop out during o Stool softeners
1. Increasing blood pressure on bowel movements, hand help is needed to bring o Flavonoids!
hemorrhoidal vessels it back in For acute disease: NSAIDS,
a. Obstipation painkiller
2. Full-blooded anal area: IV degree/ rectal prolapse – prolapsing
a. Squat, spicy food, continually, cannot be reduced Invasive (I-II degree)
alcohol, pregnancy 1. Infrared Photocoagulation
3. Weakness of connective Internal Haemorrhoids External 2. Injection of sclerosant,
tissue: • Often painless. Haemorrhoids 1. Inspection – most painful 3. Rubber band ligation (Barron
a. Aging, pregnancy • bleeding after • Severely painful haemorrhoids, thrombosed, procedure)
4. Mechanic – crack of piles defecation (blood is perianal mass ulcerated or not, are seen on a. Gold standard
holding connective tissue noted on toilet tissue) • Bleeding inspection of the anus. For I-II degree
bundles • Perianal mass Examination:
5. Vessel theory • Pruritis prolapsed, 2. Anoscope – is essential in Surgery (Hemorrhoidectomy):
• mucus discharge thrombosed,
evaluating painless or bleeding
4. Milligan morgan (open surgery)
Disease forms: • a sensation of infiltrated a. III-IV degree
• Chronic hemorrhoidal disease hemorrhoidal piles haemorrhoids. b. Failure of invasive
incomplete evacuation
• Acute hemorrhoidal disease • Ulceration- Grade IV treatment.
(thrombosis of hemorrhoidal 3. Sigmoidoscopy or colonoscopy –
piles) Complications: Rectal bleeding should be 5. Long’s procedure (circular
• Bleeding hemorrhoids Internal: prolapse→ accumulation of mucus & attributed to haemorrhoids only stapler)
causing secondary anemia fecal debris in external anal tissue→ irritation & after more serious conditions are a. For II-III degree
inflammation. excluded (e.g. cancer) b. For internal haemorrhoids
only
External: For acute disease:
- Acutely thrombosed (due to excessive - only start with surgery if only one
straining)→ necrosis of overlying skin & node is inflamed (otherwise do
bleeding. conservative)
- Strangulation of haemorrhoid - Surgery done 3-4 days after start
of inflammation
Anal fissure a longitudinal break or tear in the skin • Sharp, severe pain during Inspection: Conservative treatment:
of the anal canal distal to the dentate and after defecation • superficial or deep anal canal skin defect • Adequate fibre and water
line • Rectal bleeding (bright red (anterior/lateral/posterior) • Stool softeners (docusate)
& minimal)- blood on toilet • Wide raised edges • Nitroglycerin – 0,2- 0,3% ointment
Etiopathogenesis: paper • Skin tags (2xd)
I0 : • Perianal pruritis • Vasodilator therapy: Calcium
• Trauma of anal canal skin • Chronic constipation DRE: channel blockers (verapamil)
o Chronic spasm/ ↑ tone of the • Pain • Botulinum toxin
internal anal sphincter • Spasm of the internal anal sphincter
o Chronic constipation (Hard stool)/ *If persistent symptoms after
diarrhea Anoscope: >8weeks of conservative treatment→
o Anal sex do endoscopy to check for IBD
o Vaginal delivery
90% located at the posterior Surgical treatment:
commissure Indications:
- Fissure more than 1 year
II0 : - Inefective conservative treatment
• Due to underlying disease
o Previous anal surgery Operations
o IBD • Sphincterotomy (lateral, posterior)
o Infection • Sphincterotomy
o Impaired blood supply to the anal • Fissurectomy (excision of fissure)
mucosa • Dilatation of the anal sphincter
o Non-healing ulcer
Locate lateral/anterior to posterior
commissure
Rectal prolapse one or more layers of the rectum • Painless rectal mass Inspection: Mucosal prolapse:
protrude through the anus • Fecal incontinence Done when patient squats or strains • Reduction- digital repositioning of
• Constipation • Partial: radial folds present in mucosa rectum
At risk ages: <3yrs, female: 60-70yrs, • Pruritis around anus • Complete- concentric mucosal folds • Injection sclerotherapy
male: <40yrs • Rectal bleeding
DRE: anal sphincter weakness and mass Full thickness prolapse:
Etiopathogenesis: Video defecography: barium is instilled into the • Laparoscopic rectopexy
• ↑ intraabdominal pressure rectum & video recording is made of anorectal with/without sigmoidectomy –
o excessive straining, constipation region during the process of defectaion. rectum put back in
• weakness of pelvic floor muscle • Delrome procedure- done in childre
o Old age, multiple pregnancies Proctoscopy, Colonoscopy- prior to surgery • Altmaier procedure- excison pf
• Cystic fibrosis in children prolapsed rectum
Paraproctitis a purulent inflammation of the cellular tissues Local symptoms • Inspection • Surgical incision &
surrounding the rectum (symptoms of inflammation) • Palpation drainage
• Pain • DRE- very painful • Analgesics
Classification: • Swelling • CT- best option • Stool softeners
According to According to origin: • Red-coloured skin • MRI→ for deeper abscess, fistula
time: • Non-specific • Fever • Transanal US
• Acute (cryptoglandular) • Loss of function
• Chronic • Specific (actinomycosis, General symptoms Forms
(anorectal TB, syphilis) • Raised body fever (a) Subcutaneous (most common in children)
fistula) • Traumatic • Symptoms of intoxication (b) Submucous
(c) Ischiorectal
*Obstruction of anal
(d) Pelviorectal
glands by thick
debris→stasis & bacterial
overgrowth→ abscess
formation
Anorectal an abnormal connection between • Purulent drainage (from anal Classification: • Incision – for low fisula
fistula the epithelialized surface of the canal or surrounding According to count According to • Fistulotomy – for low fisula
anal canal and the perianal skin perianal skinn) of opening: relationship with • Fistulectomy – fistula excised out
• Pain during defecation Complete fistula sphincters: fully
*Abscess extends into perirectal • History of recurrent abscess (internal and external • Intrasphincteric • Setons
spaces→ possible fistula • Secondary openings can be openings and fistula • Transsphincteric o Cutting seton
formation→ bacteraemia & sepsis seen tract) • Extrasphincteric o Elastic seton- if inflamed tissue
(used for 2-3 months until
Incomplete fistula *Classification only inflammation ↓)
(internal fistula for complete fistula
opening and the • Fistulectomy (take out fistula tract)
tract) + anoplasty (close internal hole with
rectal wall)- done if not much
damage to sphincter (no
incontinence) but ↑ risk of
recurrence
Diagnosis:
• Fistula probe with methylene blue- can see
depth, main opening and direction
• Pelvic MRI- to see involved sphincters
• Endoscopy (sigmoidoscopy)
You might also like
- Neuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansDocument29 pagesNeuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansAngelaTrinidad100% (2)
- Integumentry PDFDocument17 pagesIntegumentry PDFMehul RathoreNo ratings yet
- GYNE 2.01a Lower Genital Tract Infections PDFDocument12 pagesGYNE 2.01a Lower Genital Tract Infections PDFMiguel Domingo100% (1)
- SurgeryDocument13 pagesSurgerykarendelarosa06100% (2)
- Anal and Perianal ConditionsDocument58 pagesAnal and Perianal ConditionsYonas YemidiralemNo ratings yet
- PERILIGHT EXPOSUREperinealcare Enema PDFDocument7 pagesPERILIGHT EXPOSUREperinealcare Enema PDFDanna Uy100% (1)
- Burn Lecture NotesDocument5 pagesBurn Lecture NotesJerlyn Lopez100% (1)
- Colonic Irrigation: Holistic Cleansing and DetoxificationDocument5 pagesColonic Irrigation: Holistic Cleansing and DetoxificationVijaya RaniNo ratings yet
- Benign Anorectal Conditions: Ahmed Badrek-AmoudiDocument20 pagesBenign Anorectal Conditions: Ahmed Badrek-AmoudiAna De La RosaNo ratings yet
- Cracking The MRCS Viva A Revision GuideDocument554 pagesCracking The MRCS Viva A Revision GuideAnonymous ZUW1pT100% (1)
- 1 Inguinal Hernia EditedDocument34 pages1 Inguinal Hernia EditedNadhirah ZulkifliNo ratings yet
- Revised Case Report - HemorrhoidsDocument47 pagesRevised Case Report - Hemorrhoidschristina_love08100% (2)
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- UlcerDocument135 pagesUlcerMahir RathodNo ratings yet
- Kuliah EmergensiDocument66 pagesKuliah EmergensiRifqi RamdhaniNo ratings yet
- Lecture 15 Bowl EliminationDocument72 pagesLecture 15 Bowl EliminationIsbelNo ratings yet
- EnemaDocument16 pagesEnemaFil AquinoNo ratings yet
- A Case Study On CholedocholithiasisDocument81 pagesA Case Study On Choledocholithiasischristelle6cadiente67% (9)
- Peripheral Vascular DiseaseDocument53 pagesPeripheral Vascular DiseaseShenbagam Mahalingam100% (1)
- ENEMA (2) FinalsDocument37 pagesENEMA (2) FinalsAngel CauilanNo ratings yet
- Necrotizing Fasciitis..By DR Kassahun GirmaDocument49 pagesNecrotizing Fasciitis..By DR Kassahun GirmaKassahun Girma GelawNo ratings yet
- Hemorrhoids: Ginesha Hafidzy GarishahDocument35 pagesHemorrhoids: Ginesha Hafidzy GarishahrizqinadiaNo ratings yet
- IV CannulationDocument13 pagesIV CannulationshifaNo ratings yet
- Fungal Infections: Major Predisposing FactorsDocument6 pagesFungal Infections: Major Predisposing FactorsIsabel CastilloNo ratings yet
- Tumors of The Head and NeckDocument5 pagesTumors of The Head and NeckMiguel CuevasNo ratings yet
- Genital Tract InjuryDocument24 pagesGenital Tract InjuryAbdulJabar Riadh100% (1)
- Arterial Diseases 2010Document25 pagesArterial Diseases 2010viKиҼswAяAи LiиGaMNo ratings yet
- Anal, Perianal, and Pilonidal Diseases - Oct - 2023 2Document15 pagesAnal, Perianal, and Pilonidal Diseases - Oct - 2023 2qq8kx98kt2No ratings yet
- Sinus and FistulaDocument3 pagesSinus and FistulaAndrew BonusNo ratings yet
- A 6 Phlebitis and Infiltration ScalesDocument1 pageA 6 Phlebitis and Infiltration ScalesSorin Alexandru LucaNo ratings yet
- UC & Crohn's DiseaseDocument3 pagesUC & Crohn's DiseaseYalin AbouhassiraNo ratings yet
- Perineum L3Document26 pagesPerineum L3Yousif AlaaNo ratings yet
- HemorrhoidsDocument14 pagesHemorrhoidsRafiq jalalNo ratings yet
- Post-Partal Complications Tone: Uterine Atony Classifications of Perineal LacerationDocument4 pagesPost-Partal Complications Tone: Uterine Atony Classifications of Perineal LacerationFebelyn PollentesNo ratings yet
- Integumentry Dermatitis Bacterial Impetigo Cellulitis Abscess DefDocument17 pagesIntegumentry Dermatitis Bacterial Impetigo Cellulitis Abscess DefMehul RathoreNo ratings yet
- Romeo NCP 3 - 1565309152Document3 pagesRomeo NCP 3 - 1565309152Kaye OrtegaNo ratings yet
- Hazards of IV TherapyDocument21 pagesHazards of IV TherapyFaraz Qurban RajperNo ratings yet
- Paediatric RashesDocument15 pagesPaediatric RashesAaron Nameer Abrar RahmanNo ratings yet
- haemorrhoids-GI BleedingDocument64 pageshaemorrhoids-GI BleedingWinda LiraNo ratings yet
- Diabetic Foot UlcerDocument6 pagesDiabetic Foot UlcerHengkai NeoNo ratings yet
- Chroni C Lymphocy Tic Leukemia - Cutane Ous B-Cell Lymphom A - Cutane Ous T-Cell Lymphom A - Follicul Ar Lymphom A - Walden Strom Macroglo BulinemiaDocument2 pagesChroni C Lymphocy Tic Leukemia - Cutane Ous B-Cell Lymphom A - Cutane Ous T-Cell Lymphom A - Follicul Ar Lymphom A - Walden Strom Macroglo BulinemiaCharissa Magistrado De LeonNo ratings yet
- Wound Healing and Its DisordersDocument39 pagesWound Healing and Its Disordersmahdi aljamalNo ratings yet
- Gangrene of ExtremitiesDocument31 pagesGangrene of ExtremitiesUsaid SulaimanNo ratings yet
- Disorder of Venous Circulation of ExtremitiesDocument47 pagesDisorder of Venous Circulation of ExtremitiesJicko Street HooligansNo ratings yet
- GynecoDocument3 pagesGynecoanne laureNo ratings yet
- RectalDocument2 pagesRectalanne laureNo ratings yet
- Causes of Acute PeritonitisDocument6 pagesCauses of Acute PeritonitisYalin AbouhassiraNo ratings yet
- UcellosisDocument4 pagesUcellosisyandraNo ratings yet
- Revision 21.7.23-Y3Document7 pagesRevision 21.7.23-Y3leexinyiNo ratings yet
- Anorectal SurgeryDocument12 pagesAnorectal SurgerySabi ShopNo ratings yet
- 3.open, AtlsDocument18 pages3.open, AtlsZeinab HusseinNo ratings yet
- 01.38-40 - (PED) - Dengue Fever and Viral Exanthems-Fabian - de CastroDocument12 pages01.38-40 - (PED) - Dengue Fever and Viral Exanthems-Fabian - de CastrobNo ratings yet
- (Gyne) 1.5 Benign Gynecologic Lesion - Dr. Co (Aish)Document7 pages(Gyne) 1.5 Benign Gynecologic Lesion - Dr. Co (Aish)earl.dejesusNo ratings yet
- Thromboembolic DiseaseDocument1 pageThromboembolic DiseaseDiana RoseroNo ratings yet
- Acute Gingival Lesions NewDocument42 pagesAcute Gingival Lesions NewdhathriNo ratings yet
- Perianal Conditions: Infective Inflammatory Complications of Above Others TumoursDocument27 pagesPerianal Conditions: Infective Inflammatory Complications of Above Others TumoursKamran khanNo ratings yet
- Anorectal DisorderDocument41 pagesAnorectal DisorderMuhammadNo ratings yet
- SeminarDocument32 pagesSeminarsachin84mittalNo ratings yet
- Hemorrhoids, ParaproctitisDocument56 pagesHemorrhoids, ParaproctitisСандагсүрэн СандагдоржNo ratings yet
- Anorectal DisordersDocument59 pagesAnorectal DisordersdasdasfNo ratings yet
- Varicose - VeinsDocument40 pagesVaricose - VeinsBibi MariamNo ratings yet
- Blood CollectionDocument4 pagesBlood Collectionmgcapuyon8596valNo ratings yet
- Varicose Veins: Short History Positioning of The PatientDocument2 pagesVaricose Veins: Short History Positioning of The PatientAshan BopitiyaNo ratings yet
- Micp Midterms ReviewerDocument7 pagesMicp Midterms ReviewerReichelle Anne QuibinNo ratings yet
- Hemorrhoids 1Document19 pagesHemorrhoids 1susulemani3No ratings yet
- Hematology VenipunctureDocument1 pageHematology VenipuncturecassseeeyyyNo ratings yet
- General Surgery IntroductionDocument1 pageGeneral Surgery IntroductionAndrew BonusNo ratings yet
- Body Temperature Measurement: Home Search Collections Journals About Contact Us My IopscienceDocument27 pagesBody Temperature Measurement: Home Search Collections Journals About Contact Us My IopscienceBobby IgnatichNo ratings yet
- Surgery and Post OpDocument96 pagesSurgery and Post OpNguyễn Nhật HoàngNo ratings yet
- Positioning of The Patient For Abdominal ExaminationDocument8 pagesPositioning of The Patient For Abdominal ExaminationDoctor Saleem RehmanNo ratings yet
- Hirschsprung Disease Case Study: Maecy P. Tarinay BSN 4-1Document5 pagesHirschsprung Disease Case Study: Maecy P. Tarinay BSN 4-1Maecy OdegaardNo ratings yet
- Problem 5 Git Aldi FDocument158 pagesProblem 5 Git Aldi Faldi firdausNo ratings yet
- Blood Presure: SOP Vital SignDocument3 pagesBlood Presure: SOP Vital SignFitria NorkhalidaNo ratings yet
- Pathophysiology of Internal HemorrhoidsDocument9 pagesPathophysiology of Internal HemorrhoidsIgor DemićNo ratings yet
- Case Presentation (October 3)Document54 pagesCase Presentation (October 3)Ayessa Camelle DumileNo ratings yet
- Human Thermoregulation and Measurement of Body Temperature in Exercise and Clinical SettingsDocument7 pagesHuman Thermoregulation and Measurement of Body Temperature in Exercise and Clinical SettingsGriffin MulofwaNo ratings yet
- SapnaDocument20 pagesSapnabiru kumarNo ratings yet
- York Mason Procedure PDFDocument12 pagesYork Mason Procedure PDFMohammed Mustafa ShaatNo ratings yet
- Rectal Suppository AdministrationDocument4 pagesRectal Suppository AdministrationCes Blanco LicerioNo ratings yet
- Hondel Desiree Van DenDocument108 pagesHondel Desiree Van DenDaffa Ardhi100% (1)
- Digestive SystemDocument45 pagesDigestive SystemEzequiel ManluluNo ratings yet
- Causes of Anal Sphincter DamageDocument4 pagesCauses of Anal Sphincter DamageHadi ZavarehNo ratings yet
- HemorroidsDocument2 pagesHemorroidsJunbieNoynayNo ratings yet
- Case Presentation 1Document18 pagesCase Presentation 1api-390677852No ratings yet
- Ulcerative ColitisDocument18 pagesUlcerative ColitisKyle Ü D. CunanersNo ratings yet
- DDS Glycerin Supp PostlabDocument33 pagesDDS Glycerin Supp PostlabGRACE MAR CABAHUGNo ratings yet
- NCM 116 NB - Care of Clients With Problem in Nutrition and Gi, Metabolism and Endocrine, PerceptionDocument4 pagesNCM 116 NB - Care of Clients With Problem in Nutrition and Gi, Metabolism and Endocrine, PerceptionSureen RegularNo ratings yet
- CHHi PDocument13 pagesCHHi PBamo MuhammadNo ratings yet