Professional Documents
Culture Documents
8 - DeMartino 2021 Better Version
Uploaded by
sounak299Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8 - DeMartino 2021 Better Version
Uploaded by
sounak299Copyright:
Available Formats
Research
JAMA Pediatrics | Original Investigation
A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease
The Medicaid Perspective
Patrick DeMartino, MD; Meredith B. Haag, MD, MPH; Alyssa R. Hersh, MD, MPH;
Aaron B. Caughey, MD, MPH, PhD; Joshua A. Roth, PhD, MHA
Editorial page 565
IMPORTANCE Hundreds of gene therapies are undergoing clinical testing and are likely to be Supplemental content
priced more than $1 million per course of treatment. The association that high prices will have
with insurance coverage of gene therapy remains unclear. Gene therapy for sickle cell disease
has shown early success and would be one of the first gene therapies available for a relatively
large population.
OBJECTIVES To estimate the budget impact and affordability of a gene therapy for severe
sickle cell disease from the perspective of US Medicaid programs with the highest prevalence
of sickle cell disease while exploring the impact of an annuity payment model.
DESIGN, SETTING, AND PARTICIPANTS A budget impact analysis was performed from January 1
to May 31, 2020, for a sickle cell disease gene therapy from the perspective of 10 state
Medicaid plans with a 5-year time horizon, using state-level disease prevalence data from
2012. Disease prevalence, Medicaid enrollment, and expenditures were derived from the
available literature. The eligible population was based on modified clinical trial inclusion
criteria including individuals aged 13 to 45 years with severe disease.
EXPOSURES The gene therapy was assumed to be administered to 7% of the eligible
population annually and was curative (no subsequent disease-related expenditures). The
gene therapy price was $1.85 million in the base case, and baseline disease-related
expenditures were $42 200 per year.
MAIN OUTCOMES AND MEASURES The main outcomes were total budget impact and budget
impact per member per month in years 1 through 5. One-way sensitivity analysis was used to
evaluate uncertainty of market diffusion, size of eligible population, price of therapy, and cost
of routine care.
RESULTS An estimated 5464 Medicaid enrollees would be eligible for the gene therapy
nationally, with 2315 individuals in the 10 Medicaid programs of interest (16 per 100 000
enrollees). The model projected a mean 1-year budget impact of $29.96 million per state
Medicaid program in the sample ($1.91 per member per month). A 5-year annuity payment
reduced the short-term budget impact.
CONCLUSIONS AND RELEVANCE This study suggests that a gene therapy for severe sickle cell
disease is likely to produce a considerable budget impact for many Medicaid plans while
potentially offering substantial benefit to patients. Payers may need to take steps to ensure
affordability and access. Gene therapy for sickle cell disease is likely to provide an early Author Affiliations: Division of
demonstration of the unique financial challenges associated with this emerging drug class. Pediatric Hematology and Oncology,
Department of Pediatrics, Oregon
Health & Science University,
Doernbecher Children’s Hospital,
Portland (DeMartino, Haag); Oregon
Health & Science University,
Department of Obstetrics and
Gynecology, Portland (Hersh,
Caughey); University of Washington
School of Pharmacy, Fred Hutchinson
Institute for Cancer Outcomes
Research, Seattle (Roth).
Corresponding Author: Patrick
DeMartino, MD, Division of Pediatric
Hematology and Oncology,
Department of Pediatrics, Oregon
Health & Science University, 707 SW
JAMA Pediatr. 2021;175(6):617-623. doi:10.1001/jamapediatrics.2020.7140 Gaines St, Portland, OR 97239
Published online March 22, 2021. Corrected on June 7, 2021. (demartip@ohsu.edu).
(Reprinted) 617
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
Research Original Investigation A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease
M
any gene therapies under development may soon
provide novel curative options for a host of malig- Key Points
nant and nonmalignant conditions. Hundreds of such
Question What will be the short-term budget impact of a gene
therapies are undergoing clinical testing and an estimated 40 therapy for sickle cell disease among Medicaid programs with the
to 50 will enter the market by 2030.1 Currently, the commer- highest prevalence of the disease?
cially available therapies are indicated for a small number of
Findings This budget impact analysis estimated a mean 1-year
patients while having exceptionally high prices—exceeding $1
budget impact of $29.96 million per state Medicaid program, or
million per treatment. The unparalleled price and potentially $1.91 per member per month increase in spending, in the 10 states
curative single administration presents various challenges to of interest.
the existing reimbursement system in the US.2 As demon-
Meaning This study suggests that gene therapy for sickle cell
strated by direct-acting antivirals (DAAs) for hepatitis C, a cost-
disease will likely present affordability challenges to several
effective therapy may still create affordability challenges for Medicaid plans.
payers balancing short-term budgets.3 The assessment of value
(cost effectiveness) and affordability (budget impact) do not
need to occur in tandem and, in some circumstances, early con- impact of a gene therapy for severe SCD from the perspective
sideration of affordability may be essential. of the 10 state Medicaid plans with the highest prevalence of
Although clinical benefit and accrued savings may make SCD; (2) describe how uncertainty in the size of the eligible
a given therapy financially tenable in the long run, what if a population, market diffusion, and pricing are associated with
patient changes health plans after a chronic disease is cured budget impact; and (3) examine how an alternative payment
with a high-cost durable therapy? Is the original insurer en- model is associated with short-term cost.
titled to the long-term accrued savings? Although several al-
ternative payment models have been proposed, much uncer-
tainty remains and there is unlikely to be a one-size-fits-all
approach.4,5
Methods
Sickle cell disease (SCD) affects approximately 100 000 in- Overview
dividuals in the US.6 Despite improvements with comprehen- A budget impact analysis was performed from January 1 to May
sive care and hydroxyurea treatment, quality of life remains 31, 2020, for an SCD gene therapy from the perspective of 10
inferior when compared with many other chronic diseases,7,8 state Medicaid plans with a 5-year time horizon. The annual
and median survival is less than 50 years for individuals with budget impact was calculated as the estimated one-time cost
hemoglobin SS or hemoglobin Sß0 genotypes.9 Only alloge- of the gene therapy less the annual savings from patients hav-
neic hematopoietic stem cell transplantation (HSCT) offers a ing previously received the intervention. Key model assump-
cure, although its use is limited owing to toxic effects and dif- tions included the percentage of patients with SCD with a se-
ficulty finding well-matched donors. The recent approvals of vere phenotype, cost of the gene therapy, and annual market
L-glutamine, voxelotor, and crizanlizumab for SCD also de- diffusion rate for the therapy (Table 1).13,17,18 State-level dis-
serve acknowledgment, although their clinical utility ap- ease burden based on published Centers for Medicare & Med-
pears modest.10-12 The profound morbidity from SCD is asso- ic aid Services data are detailed in the eTable in the
ciated with significant spending, with lifetime SCD-related Supplement.16 The state-level SCD prevalence data are from
health care expenditures exceeding $550 000 per person in 2012 (most recent available). The total budget for each Med-
2020 US dollars.13 ic aid program was available v ia The Kaiser Family
Gene therapy for severe SCD appears promising, with one Foundation.19 No institutional review board approval was re-
lentiviral-based therapy demonstrating early efficacy in the on- quired because the analysis used publicly available data with
going phase 1/2 trial HGB-206.14,15 The early data suggest that no protected health information.
this therapy may markedly improve the lives of individuals with
SCD. A gene therapy using the same lentiviral vector received Perspective and Population
conditional approval from the European Medicines Agency in The 10 state Medicaid programs with the highest prevalence
2019 for the treatment of transfusion-dependent β-thalas- of SCD included in the study were (descending order of preva-
semia. It appears that a gene therapy for SCD may soon enter lence): Mississippi; Alabama; South Carolina; Georgia; Wash-
the US market, presenting an option for a relatively large popu- ington, DC; Louisiana; Virginia; North Carolina; Florida; and
lation in comparison with existing gene therapies for other dis- Maryland. Six of the 10 states have not adopted Medicaid ex-
eases. However, this therapy is likely to cost more than $1 mil- pansion under the Patient Protection and Affordable Care Act.
lion, presenting a variety of fiscal challenges to US health care An analysis was also performed for all US Medicaid programs
payers covering large numbers of patients with SCD. At least in aggregate. International Society for Pharmacoeconomics and
55 000 patients with SCD are enrolled in Medicaid nationally.16 Outcomes Research (ISPOR) practice guidelines informed our
We sought to perform a budget impact analysis to esti- design.20
mate the short-term affordability of a gene therapy for severe The population estimated to be eligible for the gene therapy
SCD from the perspective of US Medicaid programs—a payer was based on criteria for HGB-206 trial eligibility.21 This esti-
group likely to experience the greatest budget impact. Our ob- mation was intended to approximate potential product label-
jectives were to (1) estimate the potential short-term budget ing and criteria for coverage. Adapted eligibility criteria were
618 JAMA Pediatrics June 2021 Volume 175, Number 6 (Reprinted) jamapediatrics.com
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease Original Investigation Research
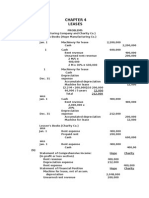
Table 1. Key Model Inputs
Range considered
Parameter Value in sensitivity analysis Source
Patients with SCD with severe 25 10-40 Assumed
phenotype, %
a
Baseline annual expenditure 42 200 17 100-67 250 Kauf et al,13 Arnold et al17
for patient with SCD, $
Cost of single gene therapy 1 850 000 1 440 000-2 170 000 Beasley and Mathias18
treatment per person, $ Abbreviation: SCD, sickle cell disease.
Annual market diffusion rate 7 2-15 Assumed a
Mean of estimates in associated
for gene therapy, %
reference.
Table 2. Budget Impact Analysis, Medicaid Perspective for US and Selected State Programs
Washington, North South
Estimates US Alabama DC Florida Georgia Louisiana Maryland Mississippi Carolina Carolina Virginia
Total No. eligible for 5464 182 44 521 353 245 170 184 260 203 153
gene therapy
No. to receive therapy, 383 13 3 36 25 17 12 13 18 14 11
year 1
No. treated 0.52 1.41 1.18 0.96 1.36 1.11 0.90 1.99 1.02 1.37 1.04
per 100 000 members,
year 1
Budget impact, year 1 707.63 23.58 5.71 67.43 45.67 31.66 22.02 23.77 33.65 26.32 19.76
(million USD), $
Budget impact, year 1 0.12 0.42 0.20 0.29 0.41 0.29 0.19 0.45 0.25 0.42 0.21
(% total Medicaid
spending)
Cost per member per 0.80 2.18 1.81 1.48 2.09 1.81 1.38 3.07 1.57 2.11 1.60
month, year 1, $
Cost per member per 0.53 1.45 1.21 0.98 1.39 1.20 0.92 2.04 1.05 1.41 1.06
month, year 5, $
Budget impact, year 5 471.25 15.70 3.80 44.91 30.42 21.09 14.67 15.83 22.41 17.53 13.16
(million USD), $
Abbreviation: USD, US dollars.
individuals with SCD aged 13 to 45 years with a phenotype of therapy and incurred no SCD-related costs in subsequent years
severe SCD (at least 4 severe pain episodes in 24 months). Our (therapy is fully curative and durable). All individuals remain-
age range for eligibility differs from the clinical trial (12-50 ing in the standard of care state incurred SCD-related expen-
years), but provides a more accurate and conservative esti- ditures. The model considers only direct medical expendi-
mate of the population size by conforming to Centers for Medi- tures associated with SCD and the cost of gene therapy.
care & Medicaid Services age strata. As per the HGB-206 trial, The model provided the annual net budget impact and per-
patients with hemoglobin SCD were excluded using the as- member per-month (PMPM) cost. The PMPM cost was calcu-
sumption that 25% of individuals with SCD have the SC lated as the annual budget impact divided by the total num-
genotype. ber of plan enrollees, divided by 12 months.
Intervention Mix and Time Horizon Input Data
The intervention was a theoretical, one-time gene therapy The proportion of patients with SCD and a severe phenotype
based on betibeglogene autotemcel (HGB-206 trial). All indi- was 25% in the base case and varied from 10% to 40% in the
viduals entered the model in the standard of care state— sensitivity analysis. These parameters were determined via
representing routine preventive and acute SCD care, in aggre- opinion as no data were available to inform the estimate.
gate. Allogenic HSCT was not considered a competing therapy The annual market diffusion rate of the gene therapy was
under the assumption that an efficacious autologous gene 7% in the base case across all 5 years. There were no data to
therapy would be preferred (and the 7% diffusion rate leaves inform this estimate given the novelty of this drug class; there-
adequate market share for transplantation among those with fore, we aimed for a conservative estimate. A range of the an-
severe disease). Other noncurative therapies were not in- nual market diffusion rate from 2% to 15% was considered in
cluded as competing treatments. A 5-year time horizon was the sensitivity analysis.
used to allow for modeling of a 5-year annuity payment. The baseline SCD-related health expenditure was $42 200
per year in the base case. There is significant variation among
Analytic Framework Description published data for annual SCD-related expenditures. The base
A static cohort entered the model receiving standard of care case was calculated as the mean of 2 prior studies represent-
(eFigure 1 in the Supplement). Each year, a subset of this co- ing low and high ends of the expenditure range: the low esti-
hort (defined via the market diffusion rate) received the gene mate ($17 100) came from a study of Florida Medicaid pa-
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2021 Volume 175, Number 6 619
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
Research Original Investigation A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease
Figure 1. Standard vs Annuity Payment Model: Mean Per-Member
Per-Month Budget Impact of Gene Therapy for 10-State Sample Results
2.50 An estimated 5464 Medicaid enrollees with SCD would be eli-
Standard repayment Annuity payment gible for the therapy nationally, with 2315 individuals in the
10 state Medicaid programs of interest (16 per 100 000 enroll-
Per-member per-month cost, $
2.00
ees). The model projected a mean 1-year budget impact of
$29.96 million per state Medicaid program (Table 2) with a
1.50
mean of $1.91 PMPM (0.31% of program budget). Florida dem-
onstrated the highest absolute 1-year cost among the states
1.00
evaluated, at $67.43 million ($1.48 PMPM), whereas Washing-
ton, DC, had the lowest, at $5.71 million ($1.81 PMPM). Rela-
0.50 tive to each program’s total budget, Mississippi’s spending was
the highest and represented 0.45% of the budget with $3.07
0 PMPM in year 1.
1 2 3 4 5
Over time, savings accrued and fewer individuals re-
Year
mained eligible for the therapy. An annual decrease in budget
impact occurred across the 5-year time horizon. For Missis-
tients with SCD13 and the high estimate ($67 250) came from sippi, the annual cost for years 1 through 5 was $23.8, $21.6,
a study of costs in the year preceding HSCT.17 These esti- $19.5, $17.6, and $15.8 million (PMPM decreasing from $3.07
mates provided the upper and lower bounds for the sensitiv- in year 1 to $2.04 in year 5). The mean budget impact across
ity analysis. All costs are updated to 2019 US dollars using the the 10 state perspectives decreased from $1.91 PMPM in year 1
Consumer Price Index. to $1.27 in year 5.
The cost of the gene therapy was $1.85 million in 2019
US dollars for the single administration in the base case— Annuity Payment Model
derived from initial pricing ($1.78 million) of betibeglogene Compared with the standard payment scenario, the 5-year an-
autotemcel in the European Union for β-thalassemia plus nuity payment decreased the short-term budget impact dur-
$70 000 for 1 admission for myeloablative conditioning fol- ing the first 4 years by deferring some spending beyond the
lowed by gene therapy infusion.18,22 The cost of incident 5-year horizon (Figure 1). By year 5, the annual budget impact
admission for autologous stem cell transplantation in the annuity model exceeded that of the standard repay-
($120 000) was derived from commercial payer data and ment. The same number of patients received the therapy in
adjusted to $70 000 in the assumption that Medicaid pays both scenarios. eFigures 2 to 12 in the Supplement demon-
57% of the commercial rate for inpatient care.23,24 The range strate the PMPM cost for the standard vs annuity payment for
considered for sensitivity analysis ($1.44 million-$2.17 mil- each of the 10 states and for all US Medicaid programs in jag-
lion) represents a 23% discount from the base c ase gregate.
(Medicaid best-price guarantee for drug) with the upper
bound as the “intrinsic value” of the treatment as proposed Sensitivity Analysis
by the manufacturer.18 The list price often overestimates Figure 2 demonstrates the result of the sensitivity analysis at
true cost but is widely used for similar purposes. No costs years 1 and 5 for the mean PMPM cost across the sample. Base-
associated with prehospitalization or posthospitalization line SCD-related expenditures had no association with year 1
care or adverse effects were included. The model was PMPM spending (no savings from averted expenditures in the
intended to provide a conservative estimate of the cost of first year), so this parameter is only in Figure 2B. The budget
the therapy. impact was most sensitive to changes in the rate of market dif-
In addition to full upfront payment, a 5-year 20% annuity fusion. Conversely, list price of the therapy and baseline SCD-
payment was evaluated (20% of price paid annually). The related expenditures had a more modest impact. For the gene
manufacturer of betibeglogene autotemcel established an out- therapy price range considered ($1.44 million to $2.17 mil-
come-based annuity in Germany and suggests this as an op- lion), the year 1 mean PMPM cost was $1.49 to $2.24.
tion in other markets.25 Our model used a 5-year annuity with
no outcome-based component given assumed 100% effective-
ness and durability.
Discussion
Sensitivity Analyses and Uncertainty Our results indicate that a commercially available gene therapy
The uncertainty of model inputs was evaluated using 1-way for severe SCD will likely generate a considerable short-term
sensitivity analysis for the following parameters: proportion budget impact and potentially present affordability chal-
with a severe phenotype, market diffusion rate, price of the lenges for many Medicaid programs. For the 10 states with the
gene therapy, and annual costs of standard of care. We report highest prevalence of SCD, our results suggest a 1-year bud-
mean PMPM cost as the outcome of interest across the 10- get impact of nearly $2 PMPM. These findings demonstrate
state sample. how, even under ideal circumstances (fully curative therapy
620 JAMA Pediatrics June 2021 Volume 175, Number 6 (Reprinted) jamapediatrics.com
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease Original Investigation Research
Figure 2. Univariate Sensitivity Analysis: Mean Per-Member Per-Month Budget Impact for 10-State Sample
A Year 1
Rate market diffusion (2%-15%)
Percentage with severe phenotype (10%-40%)
Price of gene therapy ($1.44 million to $2.17 million)
0 1.00 2.00 3.00 4.00
Per-member per-month cost, $
B Year 5
Rate market diffusion (2%-15%)
Percentage with severe phenotype (10%-40%)
Price of gene therapy ($1.44 million to $2.17 million)
Baseline annual SCD expenditures ($17 100-$67 250)
0 0.50 1.00 1.50 2.00
Blue line indicates mean cost per
Per-member per-month cost, $ member per month. SCD indicates
sickle cell disease.
with minimal associated costs of administration), this emerg- medical benefits. Because SCD will likely present the first of
ing class of durable one-time therapies may create unique fi- many affordability challenges in this emerging drug class, more
nancial challenges. We sought to focus on states with the high- research is needed evaluating potential reimbursement
est prevalence of SCD, but from a national perspective, the strategies.
budget impact is not trivial, at $0.80 PMPM for all US Medic- These findings represent a theoretical 5-year period in
aid programs in aggregate. which access to gene therapy for SCD is unencumbered by mar-
Although there is no threshold for budgetary signifi- ket entry delays owing to manufacturing or coverage negotia-
cance for Medicaid plans, any new technology adding $1 to tions, both of which have occurred in Europe with this therapy
$3 PMPM is noteworthy, especially when applyed to few for β-thalassemia.29,30 The uptake in the first year after ap-
enrollees. No existing therapies are suitable for direct com- proval may be more limited than our 7% rate owing to new
parison, although gene therapy for spinal muscular atrophy regulatory and manufacturing challenges. In addition, SCD af-
provides context. One recent budget impact analysis esti- fects racial/ethnic groups experiencing barriers to accessing
mated a PMPM cost of less than $0.10 for a US payer includ- care, systemic racism, and a history of exploitation within the
ing the gene therapy onasemnogene abeparvovec-xioi on US health care system. Even if the initial years after approval
the formulary. 26 Alternatively, we considered Medicaid demonstrate limited diffusion, it is possible that annual de-
spending on the DAA sofosbuvir in 2014. We estimated an mand may exceed the 166 individuals treated in year 1 of our
average PMPM cost of $1.54 in the 10 Medicaid programs model.
included in our analysis (in 2019 dollars).27 Our results indi- Upfront and 5-year annuity payment models were ex-
cate that gene therapy for SCD could present an affordability plored given uncertainty regarding the payment model to be
challenge comparable with that presented by the DAAs for used in the US. As seen in Figure 1, the annuity payment de-
some Medicaid plans. creases the short-term budget impact, partly by moving some
It is unclear if this sizable budget impact would force Med- expense beyond the 5-year horizon. Such an approach may be
icaid plans to implement strategies to limit access. As a soci- desirable for payers looking to minimize short-term uncer-
ety, we would need to consider the lack of alternative thera- tainty and risk, but it provides no inherent savings or benefit
pies and inequity in research funding for SCD compared with when assuming a societal perspective. In Germany, a 5-year
other diseases.28 Furthermore, the population with SCD may installment plan has been offered, with payment being con-
be especially marginalized and lacking the degree of orga- tingent on patients with β-thalassemia remaining transfu-
nized advocacy seen in other disease areas such as cystic fi- sion independent.31
brosis. Several Medicaid programs have faced litigation in re- For US payers, outcome-based contracting may be appeal-
sponse to access restrictions for the cost-effective DAAs for ing for mitigating risk, although experience implementing such
hepatitis C.3 Extrapolating from the DAA experience would be contracting is limited. Moreover, health system incentives and
tenuous, as the financing of prescription benefits differs from infrastructure may impede large-scale implementation of out-
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2021 Volume 175, Number 6 621
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
Research Original Investigation A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease
come-based reimbursements. Although there is uncertainty The therapy’s price was extrapolated from European pric-
regarding alternative financing methods in the US, many agree ing for a different indication. We presumably underesti-
that a nonstandard approach is needed.32,33 As evidenced by mated the true cost of the therapy by omitting ancillary costs
the controversy surrounding volume-based managed entry of associated with preparation, administration, and follow-up.15
the DAAs to the market for hepatitis C, such an approach for a We assumed that the therapy cured all recipients and pre-
curative therapy for SCD is unlikely to be accepted. vented any SCD-related costs in subsequent years. Even if the
One-way sensitivity analysis demonstrated that the rate therapy proves to be this effective, organ damage from SCD may
of market diffusion and the percentage of patients meeting eli- require ongoing care. Future analyses need to consider such
gibility criteria were both highly associated with the budget health care use as clinical trial data mature. We intended to
impact (Figure 2). Although the potential price of the therapy demonstrate how even an ideal therapy may still present short-
has received much attention, the price has a relatively mod- term fiscal challenges when limited to those with severe dis-
est impact when much uncertainty exists regarding the size ease. Last, our study does not consider potential improve-
of target population and market diffusion. ments in quality of life or other meaningful outcomes—here
Our analyses synthesize available data and are not meant we encourage future inquiry, including cost-effectiveness
to suggest coverage decisions for Medicaid programs. Rather, analysis.
they are meant to inform preexisting methods guiding cover- Our findings cannot be generalized to other payer per-
age decisions based on states’ unique context. Payers will need spectives given the variable prevalence of SCD. In addition,
to make decisions in the context of the disease burden among variation in payer contracting and financing will influence af-
enrollees, as well as availability of alternative treatments (ie, fordability.
comprehensive care and allogeneic HSCT).
Limitations
This study has some limitations. As with any theoretical analy-
Conclusions
sis, the validity of the model inputs determines the validity of A gene therapy for severe SCD is likely to produce a consider-
the findings. For example, our estimation of the proportion of able budget impact for many Medicaid plans while early clini-
patients with the severe phenotype meeting eligibility crite- cal trial data suggest that this therapeutic class may consid-
ria was imprecise, with no data available to inform the param- erably improve the lives of patients. With payers needing to
eter. The market diffusion rate was also a challenging param- balance short-term budgets, we expect some action will need
eter given the paucity of data for this drug class. Patients with to be taken to ensure affordability. This may prompt Medic-
SCD may be reluctant to be early adopters or early commer- aid plans to increase revenue, restrict access, or establish al-
cial success may increase demand. In addition, the eligibility ternative reimbursement methods. Gene therapy for SCD is
criteria used may differ from the eventual product label as one likely to provide an early demonstration of the unique finan-
trial plans to enroll children aged 2 to 14 years.25 cial challenges associated with this emerging drug class.
ARTICLE INFORMATION REFERENCES 5. Seeley E, Chimonas S, Kesselheim AS. Can
Accepted for Publication: December 2, 2020. 1. Quinn C, Young C, Thomas J, Trusheim M; MIT outcomes-based pharmaceutical contracts reduce
NEWDIGS FoCUS Writing Group. Estimating the drug prices in the US? a mixed methods
Published Online: March 22, 2021. assessment. J Law Med Ethics. 2018;46(4):952-963.
doi:10.1001/jamapediatrics.2020.7140 clinical pipeline of cell and gene therapies and their
potential economic impact on the US healthcare doi:10.1177/1073110518821995
Correction: This article was corrected on June 7, system. Value Health. 2019;22(6):621-626. doi:10. 6. Centers for Disease Control and Prevention.
2021, to fix an error in the text. 1016/j.jval.2019.03.014 Data & statistics on sickle cell disease. Updated
Author Contributions: Dr DeMartino had full 2. The FoCUS Project. Survey results: Payer October 21, 2019. Accessed April 1, 2020. https://
access to all the data in the study and takes perspectives on financing and reimbursement of www.cdc.gov/ncbddd/sicklecell/data.html
responsibility for the integrity of the data and the one-time high-cost durable treatments. 7. Panepinto JA, Bonner M. Health-related quality
accuracy of the data analysis. Massachusetts Institute of Technology Center for of life in sickle cell disease: past, present, and
Concept and design: All authors. Biomedical Innovation. Published October 11, 2019. future. Pediatr Blood Cancer. 2012;59(2):377-385.
Acquisition, analysis, or interpretation of data: Accessed January 20, 2020. https://newdigs.mit. doi:10.1002/pbc.24176
DeMartino, Haag, Hersh, Caughey. edu/sites/default/files/MIT FoCUS Payer Perspectives
Drafting of the manuscript: DeMartino, Haag, Roth. 8. Ballas SK, Barton FB, Waclawiw MA, et al.
2019F210v044.pdf Hydroxyurea and sickle cell anemia: effect on
Critical revision of the manuscript for important
intellectual content: DeMartino, Hersh, 3. Wyden R, Grassley C. The price of Sovaldi and its quality of life. Health Qual Life Outcomes. 2006;4:
Caughey, Roth. impact on the U.S. health care system. Committee 59. doi:10.1186/1477-7525-4-59
Statistical analysis: DeMartino, Haag, Hersh, Roth. on Finance, United States Senate. Published 9. DeBaun MR, Ghafuri DL, Rodeghier M, et al.
Administrative, technical, or material support: December 2015. Accessed January 20, 2020. Decreased median survival of adults with sickle cell
DeMartino. https://www.finance.senate.gov/imo/media/doc/1 disease after adjusting for left truncation bias:
Supervision: DeMartino, Roth. %20The%20Price%20of%20Sovaldi%20and% a pooled analysis. Blood. 2019;133(6):615-617.
20Its%20Impact%20on%20the%20U.S.% doi:10.1182/blood-2018-10-880575
Conflict of Interest Disclosures: Dr Roth reported 20Health%20Care%20System%20(Full%
receiving personal fees from Genentech, Bristol 20Report).pdf 10. Niihara Y, Miller ST, Kanter J, et al; Investigators
Myers Squibb, and personal fees from Bayer of the Phase 3 Trial of L-Glutamine in Sickle Cell
outside the submitted work. No other disclosures 4. Trusheim MR, Cassidy WM, Bach PB. Alternative Disease. A phase 3 trial of L-glutamine in sickle cell
were reported. state-level financing for hepatitis C treatment—the disease. N Engl J Med. 2018;379(3):226-235. doi:10.
“Netflix model”. JAMA. 2018;320(19):1977-1978. 1056/NEJMoa1715971
doi:10.1001/jama.2018.15782
622 JAMA Pediatrics June 2021 Volume 175, Number 6 (Reprinted) jamapediatrics.com
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease Original Investigation Research
11. Vichinsky E, Hoppe CC, Ataga KI, et al; HOPE 19. The Kaiser Family Foundation. State health N Engl J Med. 2015;373(13):1279-1281. doi:10.1056/
Trial Investigators. A phase 3 randomized trial of facts: total Medicaid spending FY 2018. Updated NEJMc1506108
voxelotor in sickle cell disease. N Engl J Med. 2019; August 2019. Accessed November 1, 2019. https:// 28. Farooq F, Mogayzel PJ, Lanzkron S, Haywood C,
381(6):509-519. doi:10.1056/NEJMoa1903212 www.kff.org/medicaid/state-indicator/total- Strouse JJ. Comparison of US federal and
12. Ataga KI, Kutlar A, Kanter J, et al. Crizanlizumab medicaid-spending/?currentTimeframe=0& foundation funding of research for sickle cell
for the prevention of pain crises in sickle cell sortModel=%7B%22colId%22:%22Location%22, disease and cystic fibrosis and factors associated
disease. N Engl J Med. 2017;376(5):429-439. doi:10. %22sort%22:%22asc%22%7D with research productivity. JAMA Netw Open.
1056/NEJMoa1611770 20. Sullivan SD, Mauskopf JA, Augustovski F, et al. 2020;3(3):e201737-e201737. doi:10.1001/
13. Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Budget impact analysis—principles of good jamanetworkopen.2020.1737
Hartzema AG. The cost of health care for children practice: report of the ISPOR 2012 Budget Impact 29. bluebird bio. bluebird bio Reports third quarter
and adults with sickle cell disease. Am J Hematol. Analysis Good Practice II Task Force. Value Health. 2019 financial results and highlights operational
2009;84(6):323-327. doi:10.1002/ajh.21408 2014;17(1):5-14. doi:10.1016/j.jval.2013.08.2291 progress. Published October 31, 2019. Accessed
14. Kanter J, Tisdale JF, Mapara MY, et al. 21. Clinicaltrials.gov. A study evaluating the safety April 6, 2020. https://investor.bluebirdbio.com/
Resolution of sickle cell disease manifestations in and efficacy of bb1111 in severe sickle cell disease. news-releases/news-release-details/bluebird-bio-
patients treated with lentiglobin gene therapy: Published May 16, 2014. Accessed November 10, reports-third-quarter-2019-financial-results-and
updated results from the phase 1/2 Hgb-206 group 2019. https://clinicaltrials.gov/ct2/show/ 30. National Institute for Health and Care
C study. Blood. 2019;134(suppl_1):990. doi:10. NCT02140554 Excellence. Betibeglogene autotemcel for treating
1182/blood-2019-128894 22. Leschly N. In pricing our gene therapy, Bluebird transfusion-dependent beta-thalassemia [ID968].
15. Walters M, Locatelli F, Thrasher A, et al. Safety weighed value, shared risk, and a lifetime cap. STAT. Updated April 6, 2020. Accessed April 6, 2020.
of autologous hematopoietic stem cell Published November 26, 2019. Accessed February https://www.nice.org.uk/guidance/indevelopment/
transplantation with gene addition therapy for 1, 2020. https://www.statnews.com/2019/11/26/ gid-ta10334
transfusion dependent beta-thalassemia, sickle cell gene-therapy-pricing-bluebird-value-shared-risk- 31. bluebird bio. bluebird bio Announces launch in
disease and cerebral adrenoleukodystrophy. lifetime-cap/ Germany of Zynteglo (autologous CD34+ cells
Presented at: Transplantation and Cellular Therapy 23. Broder MS, Quock TP, Chang E, et al. The cost encoding βA-T87Q-globin gene) gene therapy for
Meeting, American Society for Transplantation and of hematopoietic stem-cell transplantation in the patients 12 years and older with transfusion-
Cellular Therapy; February 5, 2020; United States. Am Health Drug Benefits. 2017;10(7): dependent β-thalassemia who do not have β0/β0
Orlando, Florida. 366-374. genotype. Published January 13, 2020. Accessed
16. Wilson-Frederick SH, Hulihan M, Anderson KK. 24. Selden TM, Karaca Z, Keenan P, White C, April 6, 2020. https://investor.bluebirdbio.com/
Prevalence of sickle cell disease among Medicaid Kronick R. The growing difference between public news-releases/news-release-details/bluebird-bio-
beneficiaries in 2012. Centers for Medicare & and private payment rates for inpatient hospital announces-launch-germany-zynteglotm-
Medicaid Services Office of Minority Health. care. Health Aff (Millwood). 2015;34(12):2147-2150. autologous-cd34
Published June 2019. Accessed November 10, 2019. doi:10.1377/hlthaff.2015.0706 32. The FoCUS Project. Precision financing
https://www.cms.gov/About-CMS/Agency- 25. bluebird bio. bluebird bio Reports fourth solutions for durable/potentially curative therapies.
Information/OMH/Downloads/Data-Highlight-16- quarter and full year 2019 financial results and Massachusetts Institute of Technology Center for
Sickle-Cell-Disease.pdf highlights operational progress. Published February Biomedical Innovation website. Published January
17. Arnold SD, Brazauskas R, He N, et al. Clinical 18, 2020. Accessed April 1, 2020. https://investor. 24, 2019. Accessed November 10, 2020. https://
risks and healthcare utilization of hematopoietic bluebirdbio.com/news-releases/news-release- newdigs.mit.edu/sites/default/files/MIT%
cell transplantation for sickle cell disease in the USA details/bluebird-bio-reports-fourth-quarter-and- 20FoCUS%20Precision%20Financing%
using merged databases. Haematologica. 2017;102 full-year-2019-financial 202019F201v023.pdf
(11):1823-1832. doi:10.3324/haematol.2017.169581 26. Malone D, Miller B, Dean R, et al. Use of single 33. Basu A. Financing cures in the United States.
18. Beasley DM, Mathias T. Bluebird prices gene dose gene-replacement therapy for the treatment Expert Rev Pharmacoecon Outcomes Res. 2015;15
therapy at 1.58 million euros over 5 years. Reuters of spinal muscular atrophy type 1: a United States (1):1-4. doi:10.1586/14737167.2015.990887
Health News. Published June 14, 2019. Accessed payer budget impact analysis. Value Health. 2019;
November 10, 2019. https://www.reuters.com/ 22:S336-S337. doi:10.1016/j.jval.2019.04.1644
article/us-bluebird-bio-gene-therapy-price/ 27. Liao JM, Fischer MA. Early patterns of
bluebird-prices-gene-therapy-at-1-575-million- sofosbuvir utilization by state Medicaid programs.
euros-over-five-years-idUSKCN1TF1HP
jamapediatrics.com (Reprinted) JAMA Pediatrics June 2021 Volume 175, Number 6 623
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/25/2023
You might also like
- Acctg 201 Midterm Quiz 3Document10 pagesAcctg 201 Midterm Quiz 3Minie KimNo ratings yet
- CM1 Assignment Y1 Solutions 2019 (FINAL)Document8 pagesCM1 Assignment Y1 Solutions 2019 (FINAL)Swapnil SinghNo ratings yet
- Acturarial Mathematics - BowersDocument780 pagesActurarial Mathematics - BowersEstefanía Luna Flores100% (1)
- Accounting and The Time Value of Money: Learning ObjectivesDocument83 pagesAccounting and The Time Value of Money: Learning ObjectivesedrianclydeNo ratings yet
- Classifi Cation of Treatment-Related Mortality in Children WithDocument7 pagesClassifi Cation of Treatment-Related Mortality in Children WithIgnatia Rosalia KiranaNo ratings yet
- SDOM Promising TherapiesDocument16 pagesSDOM Promising TherapiesdarlingcarvajalduqueNo ratings yet
- Relevance of Genomics To Healthcare and Nursing Practice: Guest EditorialDocument2 pagesRelevance of Genomics To Healthcare and Nursing Practice: Guest Editorialicha_mustika09No ratings yet
- Study 3Document10 pagesStudy 3Bernadett FarkasNo ratings yet
- The Babyseq Project: Implementing Genomic Sequencing in NewbornsDocument10 pagesThe Babyseq Project: Implementing Genomic Sequencing in NewbornsCristhian Rodriges AntonNo ratings yet
- Healthcare SpendingDocument20 pagesHealthcare Spendingmikeb92556No ratings yet
- Developing A Balanced Business Model For Gene TherapyDocument4 pagesDeveloping A Balanced Business Model For Gene TherapySupriya KapasNo ratings yet
- Draft For Gene TherapyDocument10 pagesDraft For Gene Therapychristian fabrosNo ratings yet
- Differences Between Children and Adults With Hidradenitis SuppurativaDocument7 pagesDifferences Between Children and Adults With Hidradenitis SuppurativaDermatología 2025No ratings yet
- Fphar 13 946415Document11 pagesFphar 13 946415Yulian 53No ratings yet
- 11 Emerging Technology in Medicine PDFDocument8 pages11 Emerging Technology in Medicine PDFArj NaingueNo ratings yet
- Ph-Based-And-10-Essentials (Updated)Document14 pagesPh-Based-And-10-Essentials (Updated)Beverly DatuNo ratings yet
- Precision Medicine in Pediatric Oncology: ReviewDocument8 pagesPrecision Medicine in Pediatric Oncology: ReviewCiocan AlexandraNo ratings yet
- 2020 Vegan Diet CVDDocument12 pages2020 Vegan Diet CVDMariNo ratings yet
- Retrospective Evaluation of Single Patient InvestiDocument9 pagesRetrospective Evaluation of Single Patient InvestiDawit BirhanuNo ratings yet
- Hemepath 2895 ZhaoDocument5 pagesHemepath 2895 ZhaoleartaNo ratings yet
- Articulo MamaDocument12 pagesArticulo MamaILIANA PINEDA RODRIGUEZNo ratings yet
- Potential Medication Dosing Errors in Outpatient Pediatrics: See Editorial, P 727Document7 pagesPotential Medication Dosing Errors in Outpatient Pediatrics: See Editorial, P 727Tammy Utami DewiNo ratings yet
- Pellegrin Morgan ProspectusDocument15 pagesPellegrin Morgan ProspectusKeyzia Galatia ManusNo ratings yet
- Meta-Análise 2021 - ItáliaDocument9 pagesMeta-Análise 2021 - ItáliaLeonardo Müller RodriguesNo ratings yet
- Role of Pharmacogenomics in Drug DevelopmentDocument11 pagesRole of Pharmacogenomics in Drug DevelopmentVeronica BalanNo ratings yet
- 11 ArticuloDocument9 pages11 ArticuloNia MoonNo ratings yet
- Jamapediatrics Wu 2020 VP 200014 1598544896.56465Document2 pagesJamapediatrics Wu 2020 VP 200014 1598544896.56465apeachNo ratings yet
- Jamaoncology Wang 2021 Oi 200103 1615397490.23946Document9 pagesJamaoncology Wang 2021 Oi 200103 1615397490.23946Oncologia Puerta del MarNo ratings yet
- JAMA Pediatrics - Lead StudyDocument9 pagesJAMA Pediatrics - Lead StudyWXYZ-TV Channel 7 DetroitNo ratings yet
- Nihms 741059Document16 pagesNihms 741059Panagiotis MisthosNo ratings yet
- Karla, Articulo 2-2Document13 pagesKarla, Articulo 2-2Richard Alejandro OrellanaNo ratings yet
- Personalized MedicineFinalDocument11 pagesPersonalized MedicineFinalJHNo ratings yet
- Evidence 1 STDocument7 pagesEvidence 1 STTania FigueroaNo ratings yet
- Poi 150091Document7 pagesPoi 150091Subekti MPNo ratings yet
- Prehospital Airway Management: A Systematic ReviewDocument13 pagesPrehospital Airway Management: A Systematic ReviewmirzaNo ratings yet
- For The ReportersDocument11 pagesFor The ReportersBeverly DatuNo ratings yet
- Decision Making in Differences of Sex DevelopmentDocument3 pagesDecision Making in Differences of Sex DevelopmentHamad ShahNo ratings yet
- 9424-Article Text-69428-1-10-20200725Document10 pages9424-Article Text-69428-1-10-20200725KELLY ALEJANDRA CAICEDO DIAZNo ratings yet
- Comparision of 2 Techniques of TCF Closure Analysis of Outcomes and Health Care UseDocument6 pagesComparision of 2 Techniques of TCF Closure Analysis of Outcomes and Health Care Usehai1No ratings yet
- PIIS0140673616309461Document9 pagesPIIS0140673616309461Jose Angel BarreraNo ratings yet
- Sociology Health Illness - 2023 - Ross - Unsettling The Treatment Imperative Chemotherapy Decision Making in The Wake Of-14Document19 pagesSociology Health Illness - 2023 - Ross - Unsettling The Treatment Imperative Chemotherapy Decision Making in The Wake Of-14ayu decontryNo ratings yet
- Djaa 048Document17 pagesDjaa 048Satra Azmia HerlandaNo ratings yet
- Multi Stakeholder Consensus On A Target Product Profile For - 2021 - The LancetDocument9 pagesMulti Stakeholder Consensus On A Target Product Profile For - 2021 - The LancetRachelNo ratings yet
- PrEP ChouDocument18 pagesPrEP ChouSeptian 99No ratings yet
- Cost Analysis of Emergency Department Criteria For Evaluation of Febrile Infants Ages 29 To 90 DaysDocument10 pagesCost Analysis of Emergency Department Criteria For Evaluation of Febrile Infants Ages 29 To 90 DaysSuwandi ChangNo ratings yet
- Malnutricion en Pacientes PolitraumatizadosDocument11 pagesMalnutricion en Pacientes PolitraumatizadosYolis MirandaNo ratings yet
- Clortalidona Vs HCLDocument10 pagesClortalidona Vs HCLdiana stefhany marin ramirezNo ratings yet
- Association of Emotional Intelligence With Malpractice ClaimsDocument7 pagesAssociation of Emotional Intelligence With Malpractice ClaimsAndreu GatuellasNo ratings yet
- Direct-to-Consumer Genetic Testing: User Motivations, Decision Making, and Perceived Utility of ResultsDocument10 pagesDirect-to-Consumer Genetic Testing: User Motivations, Decision Making, and Perceived Utility of ResultsJiaxin ZhengNo ratings yet
- The Science of Clinical Practice - Disease Diagnosis or Patient Prognosis - Croft Et Al 2015Document8 pagesThe Science of Clinical Practice - Disease Diagnosis or Patient Prognosis - Croft Et Al 2015Bipul RajbhandariNo ratings yet
- Supportive Care in Pediatric Oncology: A Practical Evidence-Based ApproachFrom EverandSupportive Care in Pediatric Oncology: A Practical Evidence-Based ApproachJames H. FeusnerNo ratings yet
- Serial Procalcitonin Predicts Mortality in Severe Sepsis Patients Results From The Multicenter Procalcitonin MOnitoring SEpsis (MOSES) StudyDocument9 pagesSerial Procalcitonin Predicts Mortality in Severe Sepsis Patients Results From The Multicenter Procalcitonin MOnitoring SEpsis (MOSES) StudyNestor AmaroNo ratings yet
- Fertility Preservation in Pediatric Leukemia and LymphomaDocument11 pagesFertility Preservation in Pediatric Leukemia and LymphomaElianaNo ratings yet
- Compet. de SaúdeDocument11 pagesCompet. de SaúdeLuciana OliveiraNo ratings yet
- Association of Race/Ethnicity and Sex With Differences in Health Care Use and Treatment For AcneDocument8 pagesAssociation of Race/Ethnicity and Sex With Differences in Health Care Use and Treatment For AcnebellaNo ratings yet
- HC Personalised Medicine Paper FinalDocument10 pagesHC Personalised Medicine Paper Finalnely coniNo ratings yet
- Breast Cancer and Biomedical Informatics: The Prognochip ProjectDocument6 pagesBreast Cancer and Biomedical Informatics: The Prognochip ProjectRuanita VeigaNo ratings yet
- AI Toward Personalized MedicineDocument8 pagesAI Toward Personalized Medicinepog3nderNo ratings yet
- qt5j15k0nf NosplashDocument2 pagesqt5j15k0nf NosplashsinayaphetNo ratings yet
- Science, Technology & Society Module 11Document8 pagesScience, Technology & Society Module 11Earl Daniel PulpulaanNo ratings yet
- Module 011 - Emerging Technology in Medicine: Genomic SequencingDocument27 pagesModule 011 - Emerging Technology in Medicine: Genomic SequencingAxie InfiNo ratings yet
- Accelerating Pediatric Cancer Drug Development: Challenges and Opportunities For Pediatric Master ProtocolsDocument9 pagesAccelerating Pediatric Cancer Drug Development: Challenges and Opportunities For Pediatric Master ProtocolsRaodatul IstiharohNo ratings yet
- Predictors For Single Agent Resistance in FIGO Score 5 or 6 Gestational Trophoblastic NeoplasiaDocument11 pagesPredictors For Single Agent Resistance in FIGO Score 5 or 6 Gestational Trophoblastic NeoplasiaKim RamirezNo ratings yet
- Pediatric Pulmonology - 2023 - Roddy - Dexamethasone Versus Methylprednisolone For Critical Asthma A Single CenterDocument9 pagesPediatric Pulmonology - 2023 - Roddy - Dexamethasone Versus Methylprednisolone For Critical Asthma A Single CenterKlinikdr RIDHANo ratings yet
- Drill 3 AK FSUU AccountingDocument15 pagesDrill 3 AK FSUU AccountingRobert CastilloNo ratings yet
- Cost Accounting Guerrero Franchises Chap06Document17 pagesCost Accounting Guerrero Franchises Chap06AlexanNo ratings yet
- Ma m1 Modelling Financial SituationsDocument15 pagesMa m1 Modelling Financial SituationsAyellah Marie VedoralNo ratings yet
- FM MidtermDocument392 pagesFM MidtermSatya SinghNo ratings yet
- Time Value of MoneyDocument18 pagesTime Value of MoneyJunaid SubhaniNo ratings yet
- Aims of Finance FunctionDocument56 pagesAims of Finance FunctionBV3S100% (1)
- FinanceDocument26 pagesFinanceBhargav D.S.No ratings yet
- EconomicsDocument13 pagesEconomicsmarkanthonycorpinNo ratings yet
- Q4-PT1Document4 pagesQ4-PT1Sam Lanver James A GuevarraNo ratings yet
- FN 202 Chapter 4Document38 pagesFN 202 Chapter 4BablooNo ratings yet
- Métodos Cuantitativos: Alex Contreras MirandaDocument23 pagesMétodos Cuantitativos: Alex Contreras MirandaRafael BustamanteNo ratings yet
- Determinants of Interest RatesDocument27 pagesDeterminants of Interest RatesraviNo ratings yet
- Exam FM Practice Exam 3Document71 pagesExam FM Practice Exam 3nad_nattNo ratings yet
- Annuity Calculator: Withdrawal PlanDocument2 pagesAnnuity Calculator: Withdrawal Plansaurabhm590No ratings yet
- Name: Date: Instructor: INSTRUCTIONS: Encircle The Correct AnswerDocument14 pagesName: Date: Instructor: INSTRUCTIONS: Encircle The Correct AnswerJasNo ratings yet
- ch10 - LiabilitiesDocument89 pagesch10 - LiabilitiessherlyneNo ratings yet
- BFIN300 Full Hands OutDocument46 pagesBFIN300 Full Hands OutGauray LionNo ratings yet
- Acc 501 Midterm Preparation FileDocument22 pagesAcc 501 Midterm Preparation FilesephienoorNo ratings yet
- General AnnuityDocument21 pagesGeneral AnnuityMark Alconaba GeronimoNo ratings yet
- Business Math A Step by Step Handbook 1622204522Document1,111 pagesBusiness Math A Step by Step Handbook 1622204522subhadramajumder11_7No ratings yet
- Activity Sheets: Quarter 2 - MELC 5Document8 pagesActivity Sheets: Quarter 2 - MELC 5MARIBETH BABANo ratings yet
- ChEg 5193 Lecture 7 Interest and InvestmentDocument28 pagesChEg 5193 Lecture 7 Interest and InvestmentGammachisNo ratings yet
- Module 5 Topic 1 Annuity Due - Paid at The Beginning of The Payment Interval. House Rent Is An Example ofDocument3 pagesModule 5 Topic 1 Annuity Due - Paid at The Beginning of The Payment Interval. House Rent Is An Example ofGian Luigi KatigbakNo ratings yet
- Advanced Zimbabwe Tax Module 2011 PDFDocument125 pagesAdvanced Zimbabwe Tax Module 2011 PDFCosmas Takawira88% (24)
- NPV Practice and Valuation Questions From Harvard CasesDocument18 pagesNPV Practice and Valuation Questions From Harvard Casesshahin selkarNo ratings yet
- Financial Accounting 2 Chapter 4Document27 pagesFinancial Accounting 2 Chapter 4Elijah Lou ViloriaNo ratings yet