Professional Documents
Culture Documents
Hyperkalaemia in Adults JCG0020 v5
Uploaded by
io0oiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyperkalaemia in Adults JCG0020 v5
Uploaded by
io0oiCopyright:
Available Formats
A Clinical Guideline for the Management of Hyperkalaemia in Adults
For Use in: Emergency departments and all adult wards
By: Clinicians
For: Adult patients with hyperkalaemia
Division responsible for document:
Medical Division (including Emergency)
Key words: Hyperkalaemia, AKI, acute kidney injury
Name of document author: Dr Ravi Varma, Dr Jean Patrick, Nicola Korn
Consultant – Renal Medicine, Consultant -
Job title of document author: Renal Medicine, Specialist Pharmacist – Renal
Medicine
Name of document author’s Line Dr Mohammed Mahdi Althaf
Manager: Helen Willimott
Consultant/ Service Director – Renal Medicine,
Job title of author’s Line Manager:
Pharmacy Team Leader - Medicine
Supported by: Dr Mahzuz Karim – Consultant – Renal
Clinical Guidelines Assessment Panel
Assessed and approved by the:
If approved by committee or Governance
Lead Chair’s Action; tick here
Date of approval: 2nd August 2023
Ratified by or reported as approved Clinical Standards Group and Effectiveness Sub-
to (if applicable): Board
To be reviewed before:
This document remains current after this 2nd August 2024
date but will be under review
To be reviewed by: Authors
Reference and / or Trust Docs ID No: 9078
Version No: 5
Compliance links: (is there any NICE
None
related to guidance)
If Yes - does the strategy/policy
deviate from the recommendations of N/A
NICE? If so why?
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 1 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Version and Document Control:
Version Date of
Change Description Author
No. Update
JCG0020 31 July Change of header and reference to joint THCGAP
v1 2014 hospital version
JCG0020 03 March Addition of an alternative insulin / Dr C Ross,
v2 2017 glucose treatment option (8 units Mr N Weavers
actrapid in 100mL 20% glucose)
JCG0020 01 Change in dose of Calcium Gluconate. Dr C Ross
v3 October Advice on (K+) and (Glucose) monitoring.
2018
Change of trust template to newest
version, change from joint clinical
guideline to NNUHFT trust guideline
CG9078 30 June Change in insulin/glucose treatment Dr R Varma
v4 2022 option based on renal association Miss N Korn
hyperkalaemia guideline
Addition of sodium zirconium
cyclosilicate
Change in administration rate for
calcium gluconate Dr R Varma
25 July
CG9078v5 Change in monitoring frequency for Dr J Patrick
2023
potassium in moderate or severe Miss N Korn
hyperkalaemia
This is a Controlled Document
Printed copies of this document may not be up to date. Please check the hospital
intranet for the latest version and destroy all previous versions.
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 2 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Contents page
1. Quick Reference Guide Emergency Management of Hyperkalaemia in Adults..4
2. Objective/s..................................................................................................................5
3. Scope..........................................................................................................................5
4. Rationale.....................................................................................................................5
5. Causes of hyperkalaemia.........................................................................................5
5.1 Pseudohyperkalaemia.........................................................................................5
5.2 Excessive potassium intake...............................................................................5
5.3 Re-distribution.....................................................................................................6
5.4 Impaired renal potassium excretion..................................................................6
6. Processes to be followed.........................................................................................7
6.1 Broad recommendations....................................................................................7
6.2 STEP 1: Antagonism of cardiac effects:...........................................................8
6.2.1 Calcium............................................................................................................8
6.3 STEP 2: Redistribution of potassium into cells...............................................8
6.3.1 Insulin and Glucose (off label use)..................................................................8
6.3.2 ß2-Adrenergic Agonists (Salbutamol) (off label use).....................................10
6.3.3 Sodium bicarbonate.......................................................................................10
6.4 STEP 3: Removal of potassium from the body..............................................10
6.4.1 Intravenous fluids..........................................................................................10
6.4.2 Diuretics.........................................................................................................11
6.4.2.1 Sodium zirconium cyclosilicate.............................................................11
6.4.3 Cation-exchange resins.................................................................................11
6.4.4 Extracorporeal potassium wasting – dialysis................................................12
6.4.5 Other measures.............................................................................................12
7. Clinical audit standards..........................................................................................13
8. Summary of development and consultation process undertaken before
registration and dissemination..............................................................................13
9. References................................................................................................................13
10. Equality Impact Assessment (EIA)........................................................................14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 3 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
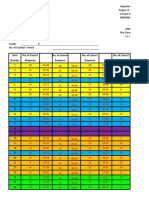
1. Quick Reference Guide Emergency Management of Hyperkalaemia in Adults
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 4 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
2. Objective/s
To improve the management of hyperkalaemia in adult patients (18 years or over) in the
Trust.
3. Scope
Treatment of hyperkalaemic cardiac arrest is outside the scope of this guideline, the
relevant algorithms and guidelines should be followed.
4. Rationale
Hyperkalaemia is a life-threatening condition, primarily due to its effect on the heart. It is
defined as a serum potassium level higher than 5.5 mmol/L. It is seen in 1.1% to 10% of
all hospitalised patients, with approximately 1% having significant hyperkalaemia of
greater than 6.0 mmol/L and is associated with a high mortality rate (14.3% to 41%).
In most patients, the pathophysiology of hyperkalaemia is multifactorial, with reduced
renal function, medications, acidosis, and hyperglycaemia being the most common
contributing factors.
5. Causes of hyperkalaemia
5.1 Pseudohyperkalaemia
This is an artefactual increase in serum K+ due to its release from cells during or after
venepuncture. Potential causes include:
Increased K+ efflux from local muscle due to fist clenching or prolonged
tourniquet time.
Thrombocytosis, leucocytosis and/or erythrocytosis
Delay in processing of sample leading to cell lysis
5.2 Excessive potassium intake
This is usually only a problem if potassium excretion is impaired, e.g. in patients with
renal failure, those with a type IV renal tubular acidosis (e.g. diabetic nephropathy), or
patients on drugs such as potassium-sparing diuretics, ACE inhibitors, or angiotensin
receptor blockers, renin inhibitors.
Red cell transfusion is a well-described cause of hyperkalaemia, typically seen in
children or in massive transfusions, but also in patients with significant renal
dysfunction. Risk factors for transfusion-related hyperkalaemia include the rate and
volume of transfusion, the use of central venous infusion and/or pressure pumping, the
use of irradiated blood, and the age of the blood infused.
It is worth noting that some commonly used laxatives contain potassium – Movicol ®,
Laxido®, Klean-Prep® and Fybogel®.
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 5 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Lo-Salt is a commercial preparation containing 66% potassium chloride (KCl) . Patients
with or at risk of hyperkalaemia should be advised not to use this as a salt substitute.
Some herbal medicines (e.g. alfalfa, dandelion, horsetail, milk weed, nettle and others)
also contain potassium and should be avoided in patients with or at risk of
hyperkalaemia.
5.3 Re-distribution
Several different mechanisms can result in an efflux of intracellular potassium, resulting
in hyperkalaemia:
Increased serum osmolarity as in people with diabetes with severe
hyperglycaemia or as a result of hypertonic mannitol.
Rhabdomyolysis may cause hyperkalaemia.
Metabolic acidosis associated with inorganic ions is associated with
hyperkalaemia. Acidosis causes extracellular movement of K +: this is more
profound with ‘fixed’ rather than organic acidosis.
Digoxin inhibits Na+/K+-ATPase and therefore impairs uptake of potassium by
skeletal muscle; thus digoxin overdose can result in hyperkalaemia.
Non-selective ß-blockers can cause hyperkalaemia in part by inhibiting cellular
uptake (but also through effects on renin-aldosterone system)
Agents that depolarise skeletal muscle, such as succinylcholine, or that activate
potassium-dependent amino acid exchangers, such as lysine or arginine, can
also lead to hyperkalaemia.
5.4 Impaired renal potassium excretion
Renal failure of any cause will usually lead to impaired potassium excretion.
Hypoaldosteronsim will result in hyperkalaemia. Aldosterone promotes both kaliuresis
and proton excretion in the cortical and medullary collecting ducts by a variety of
mechanisms. Aldosterone deficiency or resistance (e.g. Addison’s disease,
pseudohypoaldosteronism, type IV renal tubular acidosis) will therefore result in
hyperkalaemia.
Several drugs cause impaired renal potassium excretion.
Class Examples Mechanism
Inhibit conversion of angiotensin I to
ACE inhibitors Lisinopril, ramipril, perindopril
angiotensin II
Angiotensin
Losartan, candesartan, Inhibit activation of angiotensin
receptor
irbesartan receptor by angiotensin II
blockers
Aldosterone
Spironolactone, eplerenone, Block aldosterone receptor
receptor
drospirenone activation
antagonists
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 6 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Amiloride, triamterene
(trimethoprim, co-trimoxazole Block/inhibit collecting duct apical
Potassium-
and pentamidine are Na+-Cl- symport channels,
sparing
structurally similar to amiloride decreasing gradient for potassium
diuretics
and can have similar effect) secretion
Inhibit prostaglandin stimulation of
collecting duct potassium secretion,
NSAIDs Ibuprofen, diclofenac
inhibit renin release, can cause
renal failure
Inhibit basolateral Na+/K+-ATPase in
Calcineurin
Cyclosporin, tacrolimus collecting duct; also inhibit apical
inhibitors
secretory potassium channels
Inhibit aldosterone synthase, rate-
Heparin and Heparin sodium, dalteparin,
limiting enzyme for aldosterone
LMWH enoxaparin
synthesis
6. Processes to be followed
6.1 Broad recommendations
Management of hyperkalaemia is dictated by the potassium level and the severity of
ECG changes. There is an overlap between conservative (see later) and emergency
treatment of hyperkalaemia. For patients presenting with cardiac arrest – please
follow ALS algorithm and relevant guidelines, medical treatment for
hyperkalaemia should be given as per hyperkalaemic cardiac arrest algorithm.
Emergency treatment is indicated if:
There is severe hyperkalaemia (K+ > 6.5 mmol/L)
There are hyperkalaemic ECG changes – loss of P waves, prolonged PR
interval, peaked T waves, widened QRS complexes, and sine wave development
(hyperkalaemia may also be associated with bradycardia or complete heart block
– in this situation, a temporary pacing wire and urgent dialysis is often necessary)
In situations where artefactual hyperkalaemia is a possibility, repeat U&Es should be
taken, but do not delay treatment whilst waiting for result if any of the above are
present.
Urgent management of hyperkalaemia is considered in three steps:
STEP 1: Antagonism of the cardiac effects of hyperkalaemia
STEP 2: Rapid reduction in serum potassium by redistribution into cells
STEP 3: Removal of potassium from the body
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 7 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Note 1: It is mandatory that all patients with hyperkalaemia (K level ≥6.0 mmol/L) should
have an urgent 12-lead ECG performed and, if there are any hyperkalaemic changes or
if K level ≥ 6.5 mmol/L, should be on a cardiac monitor (minimum 3-lead continuous
ECG monitoring).
Note 2: It is recommended that serum potassium is assessed at least 1, 2, 4, 6 and 24
hours after identification and treatment of moderate or severe hyperkalaemia..
Note 3: The following therapies are listed to explain the physiology and posology. A
recommendation for a hierarchy of use is as per the attached algorithm.
Note 4: Some therapies are essentially holding-manoeuvres (Calcium, glucose/insulin,
and salbutamol). In the absence of another treatable pathology (e.g. overt dehydration),
definitive therapy – dialysis – will be necessary.
6.2 STEP 1: Antagonism of cardiac effects:
6.2.1 Calcium
Calcium reduces myocardial excitability in the face of hyperkalaemia. It is available as
10% calcium gluconate. The dose is 30 mL of 10% of calcium gluconate,
administered intravenously over 10 minutes via large IV access with continuous
cardiac monitoring. The effect is seen within 3 minutes and lasts 30-60 minutes. The
dose may be repeated – after 5 to 10 minutes – if no effect is seen or if ECG changes
recur after initial improvement. It MUST NOT be administered via a line containing
bicarbonate as it will precipitate as calcium carbonate.
As an alternative to 10% calcium gluconate, 10% calcium chloride may be administered.
The dose of 10% calcium chloride is 10 mL as it contains 3 times more calcium than
calcium gluconate. Calcium chloride has been recommended in the setting of
haemodynamic instability, including cardiac arrest.
Calcium should be used cautiously in patients taking digoxin as hypercalcaemia
potentiates the action of digoxin and may precipitate myocardial toxicity. In this case, it
is necessary to infuse it more slowly (over 30 min in 100 mL of 5% glucose) to allow for
an even distribution of calcium in the extracellular compartment.
6.3 STEP 2: Redistribution of potassium into cells
6.3.1 Insulin and Glucose (off label use)
Insulin lowers serum potassium by stimulation of the Na +/K+-ATPase. This effect is
reliable, reproducible, dose-dependent and effective.
In recent years, there have been multiple published reports on a high incidence of
iatrogenic hypoglycaemia after administration of insulin and glucose. The most
consistent risk factor for iatrogenic hypoglycaemia is a low pre-treatment blood glucose.
Reducing the dose of insulin alone did not consistently reduce hypoglycaemic episodes,
there is more evidence to support increasing the total glucose load to 50g. The lowest
risk of severe hypoglycaemia was associated with continuous delivery of glucose. The
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 8 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
treatment regimen has been altered to reduce the incidence of iatrogenic
hypoglycaemia.
The recommended treatment regimen is:
Check pre-treatment blood glucose level prior to insulin and glucose
administration
Administer 10 units of actrapid insulin (using an insulin syringe) with 50 mL
of 50% glucose (25 g of glucose). This should be administered intravenously
via a central venous access device/large vein via a syringe pump over 15-30
minutes. Monitor for phlebitis if 50% glucose is administered via a large
peripheral vein.
(NB-for alternative glucose regimens see box below)
If pre-treatment blood glucose < 7.0 mmol/L administer 10% glucose at 50
mL/hour for 5 hours (25 g)
o target blood glucose 4.0 – 7.0 mmol/L
o titrate rate of infusion if required
Monitor blood glucose as per advice below
Anticipate and treat hypoglycaemia promptly
Alternative Glucose regimens providing 25 g of glucose include 125 mL of 20%
glucose or 250 mL of 10% glucose. The 10 units of soluble insulin should be added to
the total volume of glucose required and drawn up into 50 mL intravenous syringes
(syringe pump maximum volume is 50 mL). If alternative glucose regimens are used
the syringe pump will need to be changed promptly several times through treatment.
The effect on serum potassium begins in 10-20 minutes, peaks at 30-60 min, and lasts
for 4-6 hours. In most patients, the serum potassium drops by 0.5-1.2 mmol/L with this
treatment. The dose may be repeated if necessary.
Close monitoring of capillary blood glucose levels, for a minimum of 12 hours after
administration of the insulin-glucose infusion, should be done at 0, 30, 60, 90, 120, 180,
240, 300, and 360, 480 and 720 minutes. If the patient has been started on a
continuous glucose infusion titrate rate of infusion according to blood glucose levels.
Seek advice from senior medical doctor if patient becomes hypoglycaemic (capillary
blood glucose < 4 mmoL/L). If patient becomes hyperglycaemic whilst on 10% glucose
infusion stop infusion and contact senior medical doctor for advice.
In hyperglycaemic patients with hyperkalaemia, insulin may be administered without
glucose (in the case of diabetic ketoacidosis as a fixed rate insulin infusion) with close
monitoring of serum glucose levels. Discuss with SpR or Consultant. For patients with
diabetic ketoacidosis follow the national guideline for the management of adult patients
with diabetic ketoacidosis. (Trust document ID: 1140)
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 9 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
6.3.2 ß2-Adrenergic Agonists (Salbutamol) (off label use)
Salbutamol exerts its effects via activation of Na +/K+-ATPase.
The recommended dose is 10- 20 mg of nebulised salbutamol. Its effects are seen
at about 30 minutes and peak at 90 minutes, lasting for 2-6 hours. It reduces serum
potassium levels by 0.5-1.0 mmol/L. However, several studies have shown that a
subset of patients is not responsive to the potassium-lowering effects of salbutamol, and
as such it should not be used as a single agent in the management of hyperkalaemia.
The effects of salbutamol are also attenuated in patients on ß-blockers and digoxin. It is
unclear whether treatment with salbutamol has a significant additive effect to insulin on
its own.
Treatment with salbutamol may cause a significant tachycardia and should be used in
caution in those with ischaemic heart disease.
6.3.3 Sodium bicarbonate
Previously used routinely in the treatment of hyperkalaemia, sodium bicarbonate is now
reserved for hyperkalaemia associated with renal failure and acidosis.
The recommended dose is 1.26% sodium bicarbonate infused intravenously at a
rate determined by the patient’s fluid status and degree of acidosis.
Hyperkalaemia and metabolic acidosis with cardiac arrest should be treated with
50 mL of 8.4% sodium bicarbonate (which is available on the arrest trolley).
Sodium bicarbonate should be used with extreme caution in the following situations:
In anuric or hypervolaemic patients – the significant sodium load may result in
symptomatic fluid overload
Hypocalcaemia – bicarbonate causes precipitation of calcium; the resultant fall in
ionised calcium may result in tetany or fits
Patients with type 2 respiratory failure – potential for paradoxical acidosis within
the central nervous system
6.4 STEP 3: Removal of potassium from the body
6.4.1 Intravenous fluids
Most cases of acute (or acute on chronic) kidney injury in hospital are a result of
intravascular volume depletion (i.e. pre-renal). In these situations, correction of volume
status with intravenous fluids may be sufficient to restore renal function and promote a
kaliuresis.
Compound sodium lactate (Hartmann’s solution) should not be used when
hyperkalaemia is present as it contains 5 mmol/Litre of potassium).
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 10 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
6.4.2 Diuretics
In certain cases, increasing renal potassium elimination with diuretics may be adequate
to lower total body potassium. However, in the setting of renal insufficiency (chronic or
acute) the effectiveness of diuretic therapy may be limited. The use of diuretics is
only indicated for those patients who are fluid replete.
In the acute setting, the diuretic most often used is intravenous furosemide. The
dose will vary depending on renal function, but in those with significant renal
impairment, up to 250 mg may be used to try and promote a kaliuresis: the effect
is mild.
6.4.2.1 Sodium zirconium cyclosilicate
Sodium Zirconium Cyclosilicate (SZC) is a non-absorbed potassium binder that
preferentially exchanges H+ and Na+ for K+ and ammonium ions throughout the entire
gastrointestinal tract. The K+-binding capacity of SZC is up to 9 times greater than that
of sodium polystyrenesulfonate. NICE has approved SZC as an option in the treatment
of acute life-threatening hyperkalaemia alongside standard care in hospitalised patients
Correction phase: the recommended dose is 10 g orally three times a day until
normokalaemia (serum K 4.0-5.0 mmol/L) is achieved. Usual treatment duration is 24-
48 hours, maximum duration is 72 hours. Sodium Zirconium Cyclosilicate should be
discontinued after 72 hours if normokalaemia not achieved.
Maintenance phase: a dose of 5 g daily can be prescribed once normokalaemia is
achieved, this can be titratred up to 10 g per day or down to 5 g alternate days
depending on serum K levels. The maintenance dose should be discontinued once
hypokalaemia develops (serum K level < 4.0 mmol/L)
The contents of the sachet should be emptied into a glass containing approximately 45
mL of water and stirred well. The powder will not dissolve. Advise the patient to drink
the tasteless liquid while still cloudy, if the suspension settles it should be stirred again.
6.4.3 Cation-exchange resins
Ion-exchange resins are cross-linked polymers containing acidic or basic structural units
that can exchange either anions or cations on contact with a solution. The most
commonly used cation-exchange resin used is Calcium Resonium ®. The onset of action
is slow (> 4 hours) and efficacy is unpredictable therefore it should only be used in
conjunction with other measures in the management of acute hyperkalaemia. It is also
poorly tolerated due to taste and constipation. Cation exchange resins have been
associated with colonic necrosis (most commonly seen with sodium polystyrene
sulfonate used in conjunction with sorbitol). Therefore, they should not be used in those
with bowel obstruction or an ileus.
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 11 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
The recommended dose is 15 g orally three times a day; each dose should be
given with 15 mL of lactulose to prevent constipation and to facilitate passage of
the resin through the gut.
Calcium Resonium® may also be administered rectally in those unable to take or
tolerate it orally. The recommended dose is 30 g as an enema retained for 9 hours
and followed by irrigation. (NB: For rectal administration please refer to summary of
product characteristics, it can be administered rectally as a suspension of 30 g resin in
150 ml of water or 10% dextrose, as a daily retention enema .)
6.4.4 Extracorporeal potassium wasting – dialysis
All modes of renal replacement therapy are effective in removing potassium, with
haemodialysis being the most rapid. Haemodialysis is indicated when hyperkalaemia is
refractory to medical management.
If haemodialysis is likely to be necessary, it is important to enlist the help of the
renal team at an early stage.
In patients who are haemodynamically unstable, haemodialysis may not be appropriate,
and they may instead need haemofiltration – early consultation with the ITU team will be
necessary.
6.4.5 Other measures
If a rapidly reversible cause of renal failure is identified, such as obstructive uropathy,
then treatment of the underlying cause with close observation may be adequate to treat
the hyperkalaemia.
All potentially offending drugs should be stopped immediately.
Although not indicated for acute hyperkalaemia, mineralocorticoid therapy (e.g.
fludrocortisone starting at 50 microgram daily) may be indicated as chronic
management of hyperkalaemia in patients with type IV renal tubular acidosis (e.g.
diabetic nephropathy, sickle cell disease).
Patients with chronic renal failure and a chronic metabolic acidosis may benefit from
long-term oral sodium bicarbonate (usually started at 500mg TDS) for chronic
management of hyperkalaemia.
All patients should be placed on a low potassium diet. Patients have a sign "low
potassium diet" added to beds/handover for catering to be alerted, not all patients
remain on a low potassium diet once hyperkalaemia resolved hence it is not appropriate
to give a leaflet to all patients. If renal fct doesn't improve and the patient remains under
care of nephrology most patient will be seen by a renal dietician at some point (in
particular if commencing renal replacement therapy); the available leaflets:
Kidney Disease: Controlling your Potassium if you have Diabetes – Trust Doc ID
14863.
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 12 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
Kidney Disease - Controlling Your Potassium (Trust Doc ID: 107) will be handed
out to relevant patients in a clinic environment/ by dieticians if appropriate
7. Clinical audit standards
This guideline is applicable across the Trust.
The renal clinical governance lead should coordinate a 3-yearly audit regarding the
management of hyperkalaemia in (non-dialysis) patients with a [K+] >6.5 (identified via
ICE). The audit will determine whether the management of patients with severe
hyperkalaemia is in line with the treatment algorithm proposed in this guideline.
The audit results will be sent to the Clinical Standards Group and Effectiveness Sub-
Board who will ensure that these are discussed at relevant governance meetings to
review the results and make recommendations for further action.
8. Summary of development and consultation process undertaken before
registration and dissemination
The authors listed above drafted this document, during its development it has been
circulated for comment to: Dr M Karim, Dr M Mahdi Althaf Dr M Andrews, Dr A Friedla,
Dr M Todd, Dr T Marshall, Ms H Willimott, Ms B Tedder.
This version has been endorsed by the Clinical Guidelines Assessment Panel.
9. References
1. Moore, M. L. & Bailey, R. R. Hyperkalaemia in patients in hospital. The New
Zealand medical journal 102, 557-558 (1989).
2 Paice, B., Gray, J. M., McBride, D., Donnelly, T. & Lawson, D. H. Hyperkalaemia in
patients in hospital. Br Med J (Clin Res Ed) 286, 1189-1192 (1983).
3 Stevens, M. S. & Dunlay, R. W. Hyperkalemia in hospitalized patients. Int Urol
Nephrol 32, 177-180 (2000).
4 Acker, C. G., Johnson, J. P., Palevsky, P. M. & Greenberg, A. Hyperkalemia in
hospitalized patients: causes, adequacy of treatment, and results of an attempt to
improve physician compliance with published therapy guidelines. Arch Intern Med
158, 917-924 (1998).
5 Mount, D. & Zandi-Nejad, K. in Brenner and Rector's The Kidney (ed BM Brenner)
997-1040 (WB Saunders, 2004).
6 Hirota, K. et al. Two cases of hyperkalemia after administration of hypertonic
mannitol during craniotomy. Journal of anesthesia 19, 75-77, doi:10.1007/s00540-
004-0270-4 (2005).
7. Baines R, Chu A, Mann S, MacRury M. Renal association clinical practice
guidelines treatment of acute hyperkalaemia in adults, 1-161 (2020)
8. Lindner G, Burdmann EA, Clase CM, Hemmelgarn BR, Herzog CA, Malyszko J,
Nagahama M, Pecoits-Filho R, Rafique Z,Rossignol P, Singer AJ. Acute
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 13 of 14
Clinical Guideline for the Management of Hyperkalaemia in Adults
hyperkalemia in the emergency department: a summary from a Kidney Disease:
Improving Global Outcomes conference. European Journal of Emergency Medicine
27(5), 329-337(2020).
10. Equality Impact Assessment (EIA)
Not applicable
Clinical Guideline for the Management of Hyperkalaemia in Adults
Author/s: Dr R Varma, Nicola Korn Author/s title: Specialist Register, Specialist Pharmacist
Approved by: Chair of CGAP Date approved: 02/08/2023 Review date: 02/08/2024
Available via Trust Docs Version: 5 Trust Docs ID: 9078 Page 14 of 14
You might also like
- Hyperkalaemia in Adults JCG0020 v4Document14 pagesHyperkalaemia in Adults JCG0020 v4TNo ratings yet
- Transfusion Reaction Guideline CA4029 v4Document17 pagesTransfusion Reaction Guideline CA4029 v4Rija KhanNo ratings yet
- Hyponatremia Inpatient Management of JCG0342 V6Document12 pagesHyponatremia Inpatient Management of JCG0342 V6Rivulet1No ratings yet
- Kawasaki Disease in Children V6.2Document16 pagesKawasaki Disease in Children V6.2Nurhasna Sushmita SariNo ratings yet
- Hyponatremia Inpatient Management of JCG0342 V3Document12 pagesHyponatremia Inpatient Management of JCG0342 V3zikryauliaNo ratings yet
- Diagnosis and Management of Complete Kawasaki Disease in ChildrenDocument13 pagesDiagnosis and Management of Complete Kawasaki Disease in ChildrenJ SNo ratings yet
- Acute Haemodialysis PrescriptionDocument24 pagesAcute Haemodialysis PrescriptionSurya Abadi KristyoadiNo ratings yet
- Albumin Guideline Approved June 2022Document13 pagesAlbumin Guideline Approved June 2022dermato pharmacyNo ratings yet
- FINAL KDIGO CKD MBD Commentary Final For PublicationDocument26 pagesFINAL KDIGO CKD MBD Commentary Final For PublicationSan DeutschNo ratings yet
- Intravenous Magnesium Sulphate in Acute Severe Asthma in Children Clinical Guideline 1.1Document7 pagesIntravenous Magnesium Sulphate in Acute Severe Asthma in Children Clinical Guideline 1.1Shyam DhokiaNo ratings yet
- Suspected Thyroid Emergencies Management of CA5060 v3.2Document12 pagesSuspected Thyroid Emergencies Management of CA5060 v3.2Jonathan jamir FarahNo ratings yet
- Blood Products in Newborn Infants v7ffDocument22 pagesBlood Products in Newborn Infants v7ffmaxlpz07No ratings yet
- Renal Function Based Dose Adjustments Adult Inpatient - Ambulatory 17.06.27Document89 pagesRenal Function Based Dose Adjustments Adult Inpatient - Ambulatory 17.06.27benny christantoNo ratings yet
- Vascular Access Procedure and Practice GuidelinesDocument25 pagesVascular Access Procedure and Practice GuidelinesBruno Miguel MagalhãesNo ratings yet
- KDIGO 2024 ANCA Vasculitis Guideline Executive Sum - 240226 - 085441Document3 pagesKDIGO 2024 ANCA Vasculitis Guideline Executive Sum - 240226 - 085441Rossio Ortuño LoboNo ratings yet
- Guiding Weight and Blood Pressure Management On Dialysis PatientDocument6 pagesGuiding Weight and Blood Pressure Management On Dialysis PatientSavita HanamsagarNo ratings yet
- Epidural Analgesia in Labour CA4054 v4.1Document8 pagesEpidural Analgesia in Labour CA4054 v4.1sand52525No ratings yet
- Protocolo Manejo de Alteraciones de La Presion en El EmbarazoDocument36 pagesProtocolo Manejo de Alteraciones de La Presion en El EmbarazoBernardita O'Brien de VanderbiltNo ratings yet
- Management of AKIDocument20 pagesManagement of AKIChris SngNo ratings yet
- Practical Transfusion Medicine for the Small Animal PractitionerFrom EverandPractical Transfusion Medicine for the Small Animal PractitionerNo ratings yet
- Clinical Guideline For Anticoagulant Use in AdultsDocument108 pagesClinical Guideline For Anticoagulant Use in Adultsmonday125No ratings yet
- Patient Blood Management Guideline For Adults With Critical BleedingDocument170 pagesPatient Blood Management Guideline For Adults With Critical BleedingAbril BernalNo ratings yet
- Management of Hemostasis and Coagulopathies for Surgical and Critically Ill Patients: An Evidence-Based ApproachFrom EverandManagement of Hemostasis and Coagulopathies for Surgical and Critically Ill Patients: An Evidence-Based ApproachRating: 5 out of 5 stars5/5 (1)
- Antifungal Clinical Guideline CA4006 v3.2Document18 pagesAntifungal Clinical Guideline CA4006 v3.2Adrian Pardo VillegasNo ratings yet
- Tim Gilbert and Nicola Rudge Chief of Medicine 1 Service and Chief PharmacistDocument39 pagesTim Gilbert and Nicola Rudge Chief of Medicine 1 Service and Chief PharmacistjellyjohnNo ratings yet
- Blood Transfusion Policy 6.3Document90 pagesBlood Transfusion Policy 6.3raNo ratings yet
- Albumin - Adult - Inpatient Clinical Practice GuidelineDocument17 pagesAlbumin - Adult - Inpatient Clinical Practice Guidelineanisa rachmitaNo ratings yet
- Arterial Blood Gases by Direct Arterial PunctureDocument15 pagesArterial Blood Gases by Direct Arterial PunctureRaden Dicky Wirawan ListiandokoNo ratings yet
- Renal Association Hyperkalaemia Guideline 2020Document161 pagesRenal Association Hyperkalaemia Guideline 2020Rudeus GreyratNo ratings yet
- Guia OxigenoterapiaDocument10 pagesGuia OxigenoterapiaJonathan AlvaradoNo ratings yet
- Guideline For The Use of Continuous Renal Replacment Therapy in ICUDocument37 pagesGuideline For The Use of Continuous Renal Replacment Therapy in ICUAron PaivaNo ratings yet
- PBM Guidelines Obstetrics and MaternityDocument139 pagesPBM Guidelines Obstetrics and MaternityQ.C. Karla MargallesNo ratings yet
- Dapagliflozin For Treating Chronic Kidney Disease PDF 82611498049477Document27 pagesDapagliflozin For Treating Chronic Kidney Disease PDF 82611498049477A9 El-EbidiNo ratings yet
- Xodo Document - Periprocedural - Anticoagulation - GuidelineDocument16 pagesXodo Document - Periprocedural - Anticoagulation - Guidelinebrigde_xNo ratings yet
- 1 s2.0 S0016508521033825 MainDocument14 pages1 s2.0 S0016508521033825 MainElizabeth Mercadillo RealNo ratings yet
- Guide MedRPDocument20 pagesGuide MedRPMohammed HaiderNo ratings yet
- Renal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysFrom EverandRenal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysNo ratings yet
- AttbDocument6 pagesAttbmuiz_travxNo ratings yet
- Equine Clinical PathologyFrom EverandEquine Clinical PathologyRaquel M. WaltonNo ratings yet
- Jurnal 3Document35 pagesJurnal 3tikaNo ratings yet
- Steroid Injections in Adult Patients With Joint and Soft Tissue Conditions JCG0055v3 PDFDocument18 pagesSteroid Injections in Adult Patients With Joint and Soft Tissue Conditions JCG0055v3 PDFSarath KumarNo ratings yet
- PIIS0828282X21001653Document22 pagesPIIS0828282X21001653Mohamed RawyNo ratings yet
- Emergency Treatment of Anaphylaxis Policy and GuidelinesDocument14 pagesEmergency Treatment of Anaphylaxis Policy and GuidelinesWaqasAhmadNo ratings yet
- S PpromDocument16 pagesS PpromthtjnhyukmNo ratings yet
- Acute Haemodialysis Clinical GuidelinesDocument16 pagesAcute Haemodialysis Clinical GuidelinesAron PaivaNo ratings yet
- Pre Operative Assessment Tests CA5130 v5Document5 pagesPre Operative Assessment Tests CA5130 v5corredorcarlos101No ratings yet
- Anafilaktik ShockDocument14 pagesAnafilaktik ShockFattan GemsNo ratings yet
- Fluid Balance and Renal Replacement Therapy Initiation Strategy: A Secondary Analysis of The STARRT-AKI TrialDocument11 pagesFluid Balance and Renal Replacement Therapy Initiation Strategy: A Secondary Analysis of The STARRT-AKI Trialnina2911No ratings yet
- Electrolyte DisturbanceDocument21 pagesElectrolyte DisturbanceLuke TosingaNo ratings yet
- Massive Blood Loss in AdultsDocument16 pagesMassive Blood Loss in AdultsPurwadi SujalmoNo ratings yet
- Joint Guideline For The Management of Respiratory Distress Syndrome of The NewbornDocument17 pagesJoint Guideline For The Management of Respiratory Distress Syndrome of The Newbornmoy9616No ratings yet
- J of Bone Mineral Res - 2022 - Bilezikian - Evaluation and Management of Primary Hyperparathyroidism Summary StatementDocument22 pagesJ of Bone Mineral Res - 2022 - Bilezikian - Evaluation and Management of Primary Hyperparathyroidism Summary StatementElena Borş MorariNo ratings yet
- Pharmacotherapy - 2022 - Skersick - Evaluating The Evidence For Sacubitril Valsartan Across The Continuum of Heart FailureDocument12 pagesPharmacotherapy - 2022 - Skersick - Evaluating The Evidence For Sacubitril Valsartan Across The Continuum of Heart FailureJ MrNo ratings yet
- Endometrial Hyperplasia Management G40 v4Document12 pagesEndometrial Hyperplasia Management G40 v4sulaimanakramzai123No ratings yet
- American Society of Hematology 2018 Guidelines For Management of Venous Thromboembolism Optimal Management of Anticoagulation TherapyDocument35 pagesAmerican Society of Hematology 2018 Guidelines For Management of Venous Thromboembolism Optimal Management of Anticoagulation TherapyBladimir CentenoNo ratings yet
- 2021.4 LG Therapeutics and COVID 19 2021 12 07 ENDocument81 pages2021.4 LG Therapeutics and COVID 19 2021 12 07 ENNining SagitaNo ratings yet
- Guidelines For Patients On Chronic Haemodialysis Programme QehbDocument33 pagesGuidelines For Patients On Chronic Haemodialysis Programme QehbRhys Espinosa100% (2)
- PCR Weak Results GuidanceDocument9 pagesPCR Weak Results GuidanceKwan Ga HouNo ratings yet
- JCS 2020 Update Guidelines PDFDocument35 pagesJCS 2020 Update Guidelines PDFdongerinbros dongerinbrosNo ratings yet
- Kipor Diesel Generator KDE23SS3 CatalogueDocument32 pagesKipor Diesel Generator KDE23SS3 CatalogueAbbasNo ratings yet
- A - Persuasive TextDocument15 pagesA - Persuasive TextMA. MERCELITA LABUYONo ratings yet
- ENTRAPRENEURSHIPDocument29 pagesENTRAPRENEURSHIPTanmay Mukherjee100% (1)
- DH 0507Document12 pagesDH 0507The Delphos HeraldNo ratings yet
- 2 Lista Total de Soportados 14-12-2022Document758 pages2 Lista Total de Soportados 14-12-2022Emanuel EspindolaNo ratings yet
- Panlilio vs. Regional Trial Court, Branch 51, City of ManilaDocument10 pagesPanlilio vs. Regional Trial Court, Branch 51, City of ManilaMaria Nicole VaneeteeNo ratings yet
- Death and The King's Horseman AnalysisDocument2 pagesDeath and The King's Horseman AnalysisCelinaNo ratings yet
- E Tech SLHT QTR 2 Week 1Document11 pagesE Tech SLHT QTR 2 Week 1Vie Boldios Roche100% (1)
- Name: Nur Hashikin Binti Ramly (2019170773) Course Code: Udm713 - Decision Making Methods and Analysis Assignment Title: Need Gap AnalysisDocument2 pagesName: Nur Hashikin Binti Ramly (2019170773) Course Code: Udm713 - Decision Making Methods and Analysis Assignment Title: Need Gap AnalysisAhmad HafizNo ratings yet
- 1-Gaikindo Category Data Jandec2020Document2 pages1-Gaikindo Category Data Jandec2020Tanjung YanugrohoNo ratings yet
- Item AnalysisDocument7 pagesItem AnalysisJeff LestinoNo ratings yet
- Spice Processing UnitDocument3 pagesSpice Processing UnitKSHETRIMAYUM MONIKA DEVINo ratings yet
- HDFC Bank-Centurion Bank of Punjab: Presented By: Sachi Bani Perhar Mba-Ib 2010-2012Document40 pagesHDFC Bank-Centurion Bank of Punjab: Presented By: Sachi Bani Perhar Mba-Ib 2010-2012Sumit MalikNo ratings yet
- GooseberriesDocument10 pagesGooseberriesmoobin.jolfaNo ratings yet
- ANNAPURNA Sanitary Work 3 FinalDocument34 pagesANNAPURNA Sanitary Work 3 FinalLaxu KhanalNo ratings yet
- Kolehiyo NG Lungsod NG Lipa: College of Teacher EducationDocument3 pagesKolehiyo NG Lungsod NG Lipa: College of Teacher EducationPrincess LopezNo ratings yet
- Pigeon Racing PigeonDocument7 pagesPigeon Racing Pigeonsundarhicet83No ratings yet
- Final Test General English TM 2021Document2 pagesFinal Test General English TM 2021Nenden FernandesNo ratings yet
- Land Building and MachineryDocument26 pagesLand Building and MachineryNathalie Getino100% (1)
- TNEA Participating College - Cut Out 2017Document18 pagesTNEA Participating College - Cut Out 2017Ajith KumarNo ratings yet
- Placement TestDocument6 pagesPlacement TestNovia YunitazamiNo ratings yet
- Eradication, Control and Monitoring Programmes To Contain Animal DiseasesDocument52 pagesEradication, Control and Monitoring Programmes To Contain Animal DiseasesMegersaNo ratings yet
- Responsive Docs - CREW Versus Department of Justice (DOJ) : Regarding Investigation Records of Magliocchetti: 11/12/13 - Part 3Document172 pagesResponsive Docs - CREW Versus Department of Justice (DOJ) : Regarding Investigation Records of Magliocchetti: 11/12/13 - Part 3CREWNo ratings yet
- PSIG EscalatorDocument31 pagesPSIG EscalatorNaseer KhanNo ratings yet
- UXBenchmarking 101Document42 pagesUXBenchmarking 101Rodrigo BucketbranchNo ratings yet
- Lower Gastrointestinal BleedingDocument1 pageLower Gastrointestinal Bleedingmango91286No ratings yet
- Wastewater Treatment: Sudha Goel, Ph.D. Department of Civil Engineering, IIT KharagpurDocument33 pagesWastewater Treatment: Sudha Goel, Ph.D. Department of Civil Engineering, IIT KharagpurSubhajit BagNo ratings yet
- English HL P1 Nov 2019Document12 pagesEnglish HL P1 Nov 2019Khathutshelo KharivheNo ratings yet
- Java Magazine JanuaryFebruary 2013Document93 pagesJava Magazine JanuaryFebruary 2013rubensaNo ratings yet
- Annals of The B Hand 014369 MBPDocument326 pagesAnnals of The B Hand 014369 MBPPmsakda HemthepNo ratings yet