Professional Documents
Culture Documents
Report
Uploaded by
pateldrash2498Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Report
Uploaded by
pateldrash2498Copyright:
Available Formats
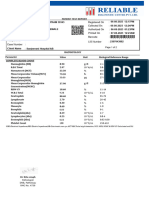
LABORATORY REPORT
Name : TRUPTI PATEL Sex/Age : Female / 47 Years Case ID : 20100197512
Ref. By : Dr. Mitul S Kotecha Dis. At : Pt. ID : 1831551
Bill. Loc. : Pt. Loc :
Reg Date and Time : 27-Jan-2022 11:54 Sample Type : Whole Blood EDTA Mobile No. : 8866460622
Sample Date and Time : 27-Jan-2022 11:21 Sample Coll. By : STMPL Ref Id1 :
Report Date and Time : 27-Jan-2022 13:16 Acc. Remarks Ref Id2 :
TEST RESULTS UNIT BIOLOGICAL REF. INTERVAL REMARKS
HAEMOGRAM REPORT
HB AND INDICES
Haemoglobin (Colorimetric) L 9.9 G% 12.00 - 15.00
RBC (Electrical Impedance) 4.37 millions/cumm 3.80 - 4.80
PCV(Calc) L 32.73 % 36.00 - 46.00
MCV (RBC histogram) L 74.9 fL 83.00 - 101.00
MCH (Calc) L 22.7 pg 27.00 - 32.00
MCHC (Calc) L 30.2 gm/dL 31.50 - 34.50
RDW (RBC histogram) 14.80 % 11.00 - 16.00
20100197512-TRUPTI PATEL-47 Years-Female
TOTAL AND DIFFERENTIAL WBC COUNT (Flowcytometry)
Total WBC Count 6550 /µL 4000.00 - 10000.00
[%] EXPECTED VALUES [ Abs ] EXPECTED VALUES
Neutrophil 54.8 % 40.00 - 70.00 3589 /ul 2000.00 - 7000.00
Lymphocyte 32.5 % 20.00 - 40.00 2129 /ul 1000.00 - 3000.00
Eosinophil 4.9 % 1.00 - 6.00 321 /ul 20.00 - 500.00
Monocytes 7.6 % 2.00 - 10.00 498 /ul 200.00 - 1000.00
Basophil 0.2 % 0.00 - 2.00 13 /ul 0.00 - 100.00
Neutrophil to Lymphocyte 1.69 0.78 - 3.53
Ratio (NLR)
PLATELET COUNT (Optical)
Platelet Count 368000 /µL 150000.00 - 410000.00
SMEAR STUDY
RBC Morphology Microcytosis, Hypochromia
WBC Morphology Total WBC count within normal limits.
Platelet Platelets are adequate in number.
Parasite Malarial Parasite not seen on smear.
Morphological Impression -
Note:(LL-VeryLow,L-Low,H-High,HH-VeryHigh ,A-Abnormal)
Page 1 of 5
Dr Vidhi Shah Dr. Sandip Shah Printed On : 27-Jan-2022 14:04
M.D. (Patho). M.D. (Path. & Bact.)
Consultant Pathologist
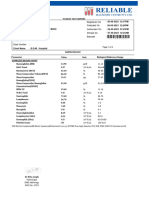
LABORATORY REPORT
Name : TRUPTI PATEL Sex/Age : Female / 47 Years Case ID : 20100197512
Ref. By : Dr. Mitul S Kotecha Dis. At : Pt. ID : 1831551
Bill. Loc. : Pt. Loc :
Reg Date and Time : 27-Jan-2022 11:54 Sample Type : Whole Blood EDTA Mobile No. : 8866460622
Sample Date and Time : 27-Jan-2022 11:21 Sample Coll. By : STMPL Ref Id1 :
Report Date and Time : 27-Jan-2022 13:59 Acc. Remarks Ref Id2 :
TEST RESULTS UNIT BIOLOGICAL REF RANGE REMARKS
HAEMATOLOGY INVESTIGATIONS
ESR H 106 mm after 1hr 3 - 20
Photometrical capillary stopped flow kinetic
analysis
20100197512-TRUPTI PATEL-47 Years-Female
Note:(LL-VeryLow,L-Low,H-High,HH-VeryHigh ,A-Abnormal)
Page 2 of 5
Dr. Pavan Dave Dr. Sandip Shah Printed On : 27-Jan-2022 14:04
DCP, DNB (PATH) M.D. (Path. & Bact.)
Consultant Pathologist
LABORATORY REPORT
Name : TRUPTI PATEL Sex/Age : Female / 47 Years Case ID : 20100197512
Ref. By : Dr. Mitul S Kotecha Dis. At : Pt. ID : 1831551
Bill. Loc. : Pt. Loc :
Reg Date and Time : 27-Jan-2022 11:54 Sample Type : Serum Mobile No. : 8866460622
Sample Date and Time : 27-Jan-2022 11:21 Sample Coll. By : STMPL Ref Id1 :
Report Date and Time : 27-Jan-2022 12:59 Acc. Remarks Ref Id2 :
TEST RESULTS UNIT BIOLOGICAL REF RANGE REMARKS
BIOCHEMICAL INVESTIGATIONS
S.G.P.T. 12.00 U/L 0.0 - 59
NADH (Without P-5-P)
C- Reactive Protein H 10.90 mg/L 0 - 5.0
Immunotubidometric assay
.
INTERPRETATIONS:
Detecting systemic inflammatory processes. Detecting infection and assessing response to antibiotic treatment of bacterial infections Differentiating
between active and inactive disease forms with concurrent infection CRP levels can increase dramatically (100-fold or more) after severe trauma, bacterial
infection, inflammation, surgery, or neoplastic proliferation. CRP has been used to assess activity of inflammatory disease, to detect infections after surgery,
to detect transplant rejection, and to monitor these inflammatory processes. Elevated values are consistent with an acute inflammatory process.
CAUTIONS :
Elevated C-reactive protein (CRP) values are nonspecific and should not be interpreted without a complete clinical history. Oral contraceptives may
20100197512-TRUPTI PATEL-47 Years-Female
increase CRP levels. HSCRP/C-Reactive Protein, High Sensitivity, Serum is the appropriate CRP test to order to assess risk of cardiovascular disease or
events.
Creatinine 0.57 mg/dL 0.55 - 1.02
Kinetic Alkaline Picrate
Note:(LL-VeryLow,L-Low,H-High,HH-VeryHigh ,A-Abnormal)
Page 3 of 5
Dr Sandip Shah Dr. Sandip Shah Printed On : 27-Jan-2022 14:04
M.D. (Path. & Bact.) M.D. (Path. & Bact.)
Consultant Pathologist Consultant Pathologist
LABORATORY REPORT
Name : TRUPTI PATEL Sex/Age : Female / 47 Years Case ID : 20100197512
Ref. By : Dr. Mitul S Kotecha Dis. At : Pt. ID : 1831551
Bill. Loc. : Pt. Loc :
Reg Date and Time : 27-Jan-2022 11:54 Sample Type : Serum Mobile No. : 8866460622
Sample Date and Time : 27-Jan-2022 11:21 Sample Coll. By : STMPL Ref Id1 :
Report Date and Time : 27-Jan-2022 13:28 Acc. Remarks Ref Id2 :
TEST RESULTS UNIT BIOLOGICAL REF RANGE REMARKS
BIOCHEMICAL INVESTIGATIONS
25 OH Cholecalciferol (D2+D3) L 26.1 ng/mL Adult:
CMIA 30 - 100 Normal Level
20 - <30 Insufficiency
< 20 Deficiency
> 150 Toxicity
Pediatric
20 - 100 Normal Level
15 - <20 Insufficiency
< 15 Deficiency
25-OH-VitD plays a primary role in the maintenance of calcium homeostasis. It promotes intestinal calcium absorption and, in concert with PTH, skeletal
calcium deposition, or less commonly, calcium mobilization. Modest 25-OH-VitD deficiency is common; in institutionalised elderly, its prevalence may be
20100197512-TRUPTI PATEL-47 Years-Female
>50%. Although much less common, severe deficiency is not rare either. Reasons for suboptimal 25-OH-VitD levels include lack of sunshine exposure, a
particular problem in Northern latitudes during winter; inadequate intake; malabsorption (e.g, due to Celiac disease); depressed hepatic vitamin D 25-
hydroxylase activity, secondary to advanced liver disease; and enzyme-inducing drugs, in particular many antiepileptic drugs, including phenytoin,
phenobarbital, and carbamazepine, that increase 25-OH-VitD metabolism. Hypervitaminosis D is rare, and is only seen after prolonged exposure to
extremely high doses of vitamin D. When it occurs, it can result in severe hypercalcemia and hyperphosphatemia.
INTERPRETATION
• Levels <10 ng/mL may be associated with more severe abnormalities and can lead to inadequate mineralization of newly formed osteoid, resulting
in rickets in children and osteomalacia in adults. In these individuals, serum calcium levels may be marginally low, and parathyroid hormone (PTH)
and serum alkaline phosphatase are usually elevated. Definitive diagnosis rests on the typical radiographic findings or bone
biopsy/histomorphometry.
• Patients who present with hypercalcemia, hyperphosphatemia, and low PTH may suffer either from ectopic, unregulated conversion of 25-OH-VitD
to 1,25 (OH)2-VitD, as can occur in granulomatous diseases, particularly sarcoidosis, or from nutritionally-induced hypervitaminosis D. Serum 1,25
(OH)2-VitD levels will be high in both groups, but only patients with hypervitaminosis D will have serum 25-OH-VitD concentrations of >80 ng/mL,
typically >150 ng/mL.
• Patients with CKD have an exceptionally high rate of severe vitamin D deficiency that is further exacerbated by the reduced ability to convert 25-
OH- VitD into the active form, 1,25 (OH)2-VitD. Emerging evidence also suggests that the progression of CKD & many of the cardiovascular
complications may be linked to hypovitaminosis D.
• Approximately half of Stage 2 and 3 CKD patients are nutritional vitamin D deficient (25-OH-VitD, less than 30 ng/mL), and this deficiency is more
common among stage 4 CKD patients. Additionally, calcitriol (1,25 (OH)2-VitD) levels are also overtly low (less than 22 pg/mL) in CKD patients.
Similarly, vast majority of dialysis patients are found to be deficient in nutritional vitamin D and have low calcitriol levels. Recent data suggest an
elevated PTH is a poor indicator of deficiencies of nutritional vitamin D and calcitriol in CKD patients.CAUTIONS Long term use of anticonvulsant
medications may result in vitamin D deficiency that could lead to bone disease; the anticonvulsants most implicated are phenytoin, phenobarbital,
carbamazepine, and valproic acid.
------------------ End Of Report ------------------
Note:(LL-VeryLow,L-Low,H-High,HH-VeryHigh ,A-Abnormal)
Page 4 of 5
Dr Sandip Shah Dr. Sandip Shah Printed On : 27-Jan-2022 14:04
M.D. (Path. & Bact.) M.D. (Path. & Bact.)
Consultant Pathologist Consultant Pathologist
LABORATORY REPORT
Name : TRUPTI PATEL Sex/Age : Female / 47 Years Case ID : 20100197512
Ref. By : Dr. Mitul S Kotecha Dis. At : Pt. ID : 1831551
Bill. Loc. : Pt. Loc :
Reg Date and Time : 27-Jan-2022 11:54 Sample Type : Serum Mobile No. : 8866460622
Sample Date and Time : 27-Jan-2022 11:21 Sample Coll. By : STMPL Ref Id1 :
Report Date and Time : 27-Jan-2022 13:28 Acc. Remarks Ref Id2 :
# For test performed on specimens received or collected from non-NSRL locations, it is presumed that the specimen belongs to the patient named or
identified as labeled on the container/test request and such verification has been carried out at the point generation of the said specimen by the sender.
NSRL will be responsible Only for the analytical part of test carried out. All other responsibility will be of referring Laboratory.
20100197512-TRUPTI PATEL-47 Years-Female
Note:(LL-VeryLow,L-Low,H-High,HH-VeryHigh ,A-Abnormal)
Page 5 of 5
Dr Sandip Shah Dr. Sandip Shah Printed On : 27-Jan-2022 14:04
M.D. (Path. & Bact.) M.D. (Path. & Bact.)
Consultant Pathologist Consultant Pathologist
You might also like
- Laboratory Report: M.D. (Path. & Bact.)Document13 pagesLaboratory Report: M.D. (Path. & Bact.)pateldrash2498No ratings yet
- Laboratory Report: Consultant PathologistDocument2 pagesLaboratory Report: Consultant Pathologisttafiki4253No ratings yet
- 3upneaa5qdckn2nonvdn0vouDocument7 pages3upneaa5qdckn2nonvdn0vouNitinNo ratings yet
- LPL - Pasricha Diagnostics & Ultrasound ClinicDocument4 pagesLPL - Pasricha Diagnostics & Ultrasound ClinicJohnnieNo ratings yet
- Department of Laboratory MedicineDocument2 pagesDepartment of Laboratory MedicineShreenath KNNo ratings yet
- Q2ohrv4w3sib2vnjaa2m4iebDocument10 pagesQ2ohrv4w3sib2vnjaa2m4iebShalu SaharanNo ratings yet
- Indian EconomyDocument10 pagesIndian Economyrajputdhruv100No ratings yet
- 463938838Document8 pages463938838sumitthardak34No ratings yet
- LPL - PSC Rohini (DC Chowk) Shop No. 27, Ground Floor, SG Mall, Sect or - 9, DC Chowk, Rohini New Delhi - 110 DelhiDocument2 pagesLPL - PSC Rohini (DC Chowk) Shop No. 27, Ground Floor, SG Mall, Sect or - 9, DC Chowk, Rohini New Delhi - 110 DelhiSaurabh GuptaNo ratings yet
- AiimsDocument7 pagesAiimsYOGENDRANo ratings yet
- dfee0562-f38e-4bbe-b0fa-7eb727ea32eaDocument4 pagesdfee0562-f38e-4bbe-b0fa-7eb727ea32eaNirmal RajoriaNo ratings yet
- Medical ReportsDocument5 pagesMedical Reportsritikapagraj01No ratings yet
- 99f5fd85-4ee0-4756-afcf-49c54943d6afDocument12 pages99f5fd85-4ee0-4756-afcf-49c54943d6afprint emitraNo ratings yet
- Test Report: Complete Blood Count (CBC)Document1 pageTest Report: Complete Blood Count (CBC)WSC ALMANo ratings yet
- MedicalDocument1 pageMedicalyashrrajsinha31No ratings yet
- Sohp230300015306 15654625Document4 pagesSohp230300015306 15654625Rohit KumarNo ratings yet
- Gpbxa1l2sjwh0xeblfzsz3zxDocument8 pagesGpbxa1l2sjwh0xeblfzsz3zxmani bhushan sharmaNo ratings yet
- Kvo2rd2iirnhll0zct4myobjDocument10 pagesKvo2rd2iirnhll0zct4myobjmani bhushan sharmaNo ratings yet
- HC20297293 PDFDocument20 pagesHC20297293 PDFGhanshyamPatankarNo ratings yet
- LPLT12448 : LPL - Lpl-Rohini (National Reference Lab) Sector - 18, Block - E Rohini DELHI 110085Document6 pagesLPLT12448 : LPL - Lpl-Rohini (National Reference Lab) Sector - 18, Block - E Rohini DELHI 110085Kumar ManglamNo ratings yet
- Laboratory Report: M.D. (Patho) M.D. (Patho) M.D. (Patho)Document2 pagesLaboratory Report: M.D. (Patho) M.D. (Patho) M.D. (Patho)Parth KaravadraNo ratings yet
- Amarjeet KaurDocument7 pagesAmarjeet Kauralansari shopNo ratings yet
- Report YashwaniDocument9 pagesReport Yashwaniv.verma7290No ratings yet
- Test Report: Complete Blood Count (CBC)Document3 pagesTest Report: Complete Blood Count (CBC)WSC ALMANo ratings yet
- H5zx4fklv4ovtl2lopumlbu3Document9 pagesH5zx4fklv4ovtl2lopumlbu3roypalNo ratings yet
- Oxy Patho Sample ReportDocument12 pagesOxy Patho Sample ReportWycliffe AnshulNo ratings yet
- SL Report PDFDocument2 pagesSL Report PDFAnonymous JEqeJdhw2No ratings yet
- Abhishek 001045Document5 pagesAbhishek 001045abhidomadiya2121No ratings yet
- Hemogram Test Name Units Results Bio. Ref. Interval: Page 1 of 6Document6 pagesHemogram Test Name Units Results Bio. Ref. Interval: Page 1 of 6Anmol SabharwalNo ratings yet
- WM17SDocument10 pagesWM17Ssheshu MNo ratings yet
- Test Report: Hemogram Test Name Units Results Bio. Ref. IntervalDocument19 pagesTest Report: Hemogram Test Name Units Results Bio. Ref. Intervalcs2015ok77No ratings yet
- SVLT Lab Report DetailsDocument1 pageSVLT Lab Report Detailspancard1098No ratings yet
- Complete Blood Count (CBC) Test Name Units Results Bio. Ref. IntervalDocument6 pagesComplete Blood Count (CBC) Test Name Units Results Bio. Ref. IntervalAnmol SabharwalNo ratings yet
- Ck4tzxj55reuochnn2p5ecwaDocument6 pagesCk4tzxj55reuochnn2p5ecwaMuscle Arora0% (1)
- Aeftih00xz45wh31kru1fekbDocument6 pagesAeftih00xz45wh31kru1fekbAvantika BirwalNo ratings yet
- RADHEDocument4 pagesRADHENeeraj KumarNo ratings yet
- Blood Report Yatendra 08112022Document4 pagesBlood Report Yatendra 08112022mped 6100% (1)
- SHANTIDocument4 pagesSHANTINeeraj KumarNo ratings yet
- L89 - Ypl Diagnostics Ypl Diagnosticssamrat Hopping Mall, Garh Road, Pin Code No: 252002meerut Uttar MeerutDocument3 pagesL89 - Ypl Diagnostics Ypl Diagnosticssamrat Hopping Mall, Garh Road, Pin Code No: 252002meerut Uttar MeerutAyush Kumar GuptaNo ratings yet
- Mrs BIMLA W O JAYRAM 30343 06 08 2023 06 54 42 PMDocument2 pagesMrs BIMLA W O JAYRAM 30343 06 08 2023 06 54 42 PMfadikex618No ratings yet
- Zoheir Aissaoui Rals03 10016 1Document5 pagesZoheir Aissaoui Rals03 10016 1babelfirdaousNo ratings yet
- Test Report: Pass. No.Document2 pagesTest Report: Pass. No.Hasmukh patelNo ratings yet
- WP02Document9 pagesWP02lucky jainNo ratings yet
- S50 - Rauta Chauraha-CCDocument11 pagesS50 - Rauta Chauraha-CCRohit Kumar SinghNo ratings yet
- D Seshagiri Rao-08Nov2023-Health CheDocument7 pagesD Seshagiri Rao-08Nov2023-Health CheSUNSHINE DIAGNOSTICSNo ratings yet
- L96 - Patna Lab 2 (Home Visit) : Patientreportscsuperpanel - SP - General - Template01 - SC (Version: 7)Document3 pagesL96 - Patna Lab 2 (Home Visit) : Patientreportscsuperpanel - SP - General - Template01 - SC (Version: 7)Rohit Gautam DwivediNo ratings yet
- H5zx4fklv4ovtl2lopumlbu3Document9 pagesH5zx4fklv4ovtl2lopumlbu3roypalNo ratings yet
- Lal Path Labreport PDFDocument10 pagesLal Path Labreport PDFIpad AppleNo ratings yet
- Thyrocare Processed atDocument3 pagesThyrocare Processed atKarim SirNo ratings yet
- Hdkgzt2ylj5kruld3lxjt3uuDocument10 pagesHdkgzt2ylj5kruld3lxjt3uuPRIYANSHU NAMANNo ratings yet
- Life Healthcare - CC Gram-Ijarata Thana-Paliganj Paipura KAL Patna Lab II R K ESTATE Opposite IGIMS Raja Bazar Bailey Road Patna-800014Document5 pagesLife Healthcare - CC Gram-Ijarata Thana-Paliganj Paipura KAL Patna Lab II R K ESTATE Opposite IGIMS Raja Bazar Bailey Road Patna-800014Parth From class 7 ANo ratings yet
- Test Results Units Biological Reference Interval: Haematology Kushal Pro-1 (KP-1) CBC-Comprehensive (20 Paramaters)Document6 pagesTest Results Units Biological Reference Interval: Haematology Kushal Pro-1 (KP-1) CBC-Comprehensive (20 Paramaters)Ravindranatha AnNo ratings yet
- Sdv2a1qefsqvd2aj3ybfov5eDocument3 pagesSdv2a1qefsqvd2aj3ybfov5eAshish RanaNo ratings yet
- Complete Blood Count (CBC With E.S.R) .: Investigation Units Result Biological Reference IntervalDocument4 pagesComplete Blood Count (CBC With E.S.R) .: Investigation Units Result Biological Reference Intervalmaryam.ksohrabNo ratings yet
- Saifee, 24.02.2024 - Darji - UnlockedDocument1 pageSaifee, 24.02.2024 - Darji - Unlockedritikdarji2106No ratings yet
- Abhishek 001560Document2 pagesAbhishek 001560abhidomadiya2121No ratings yet
- GOURAB SAHOO-Male21 Years-77852Document2 pagesGOURAB SAHOO-Male21 Years-77852J. K. MuduliNo ratings yet
- Lab ResultDocument1 pageLab ResultrabeeiNo ratings yet
- Dinesh SainiDocument2 pagesDinesh Sainifadikex618No ratings yet
- Ce3 F8e8 425e 9d25 93b8a2b717c0Document6 pagesCe3 F8e8 425e 9d25 93b8a2b717c0pateldrash2498No ratings yet
- Derivative Analyst JDDocument2 pagesDerivative Analyst JDpateldrash2498No ratings yet
- Vp°Ffiv 'Phf Lh° Hpμvπka°' 'F: Your DetailsDocument2 pagesVp°Ffiv 'Phf Lh° Hpμvπka°' 'F: Your Detailspateldrash2498No ratings yet
- 100 % Result of Std.10 - Best Score Holders of The Year 2021-22Document1 page100 % Result of Std.10 - Best Score Holders of The Year 2021-22pateldrash2498No ratings yet
- 2024-03-28-22-32-17fy 22-23 - 380015Document12 pages2024-03-28-22-32-17fy 22-23 - 380015pateldrash2498No ratings yet
- Unit-1 Concept of International MarketingDocument34 pagesUnit-1 Concept of International Marketingpateldrash2498No ratings yet
- Kiani v. Bureau of Immigration and Deportation, GR No. 160922, 27 ESCRADocument19 pagesKiani v. Bureau of Immigration and Deportation, GR No. 160922, 27 ESCRAmheritzlynNo ratings yet
- DS - LWT300 - SF - A4 EN Rev BDocument4 pagesDS - LWT300 - SF - A4 EN Rev BZts MksNo ratings yet
- Harmony Radio, R2.8: Order Codes ReferenceDocument51 pagesHarmony Radio, R2.8: Order Codes ReferenceRalaivao Solofohery Dieu-donnéNo ratings yet
- Metrologic Colombia S.A.S. Medellín Medellín Colombia: Oferta Economica CO20233ADocument3 pagesMetrologic Colombia S.A.S. Medellín Medellín Colombia: Oferta Economica CO20233AJulian MoraNo ratings yet
- Simple Usecases of PI B2B - SFTP and PGPDocument35 pagesSimple Usecases of PI B2B - SFTP and PGPPiedone640% (1)
- BioEdit Version 7.0.0 PDFDocument192 pagesBioEdit Version 7.0.0 PDFJovanderson JacksonNo ratings yet
- 1 s2.0 S0959652618323667 MainDocument12 pages1 s2.0 S0959652618323667 MaintaliagcNo ratings yet
- Technical Schedule World BankDocument249 pagesTechnical Schedule World BankPramod ShastryNo ratings yet
- Westermo MRD 330-3xx & GreenBow IPSec VPN Client Software ConfigurationDocument12 pagesWestermo MRD 330-3xx & GreenBow IPSec VPN Client Software ConfigurationgreenbowNo ratings yet
- PDF Applied Failure Analysis 1 NSW - CompressDocument2 pagesPDF Applied Failure Analysis 1 NSW - CompressAgungNo ratings yet
- Eco SPARDocument3 pagesEco SPARMohammad LabinNo ratings yet
- Business and Finance TerminologyDocument15 pagesBusiness and Finance TerminologyKat KatNo ratings yet
- PCIB Vs Escolin DigestDocument3 pagesPCIB Vs Escolin DigestsamontedianneNo ratings yet
- Etpm Mód 3 Assignment 2.1 Grammar and Use of English SkillsDocument3 pagesEtpm Mód 3 Assignment 2.1 Grammar and Use of English SkillsLourdes LimaNo ratings yet
- The Cycle of Leadership Through Transformational, Eccles - (Leadership) PDFDocument16 pagesThe Cycle of Leadership Through Transformational, Eccles - (Leadership) PDFEliana LopezNo ratings yet
- Conext Battery Monitor Quick Start Guide 975 0690-03-01 Rev B SPA1Document2 pagesConext Battery Monitor Quick Start Guide 975 0690-03-01 Rev B SPA1xray123zzzNo ratings yet
- Pecson Vs CADocument3 pagesPecson Vs CASophiaFrancescaEspinosaNo ratings yet
- AMEM211 Lab2 PotentiometerDocument10 pagesAMEM211 Lab2 PotentiometerB.s. BhosleNo ratings yet
- Robert Plank's Super SixDocument35 pagesRobert Plank's Super SixkoyworkzNo ratings yet
- CM760 E-Brochure HemobasculaDocument6 pagesCM760 E-Brochure Hemobasculajordigs50No ratings yet
- Compt I A Network Plus 008Document902 pagesCompt I A Network Plus 008trainmNo ratings yet
- Sub Clause 1.15 Limitation of Liability PDFDocument4 pagesSub Clause 1.15 Limitation of Liability PDFBogdanNo ratings yet
- United States Court of Appeals, Third CircuitDocument18 pagesUnited States Court of Appeals, Third CircuitScribd Government DocsNo ratings yet
- Single Line DiagramDocument1 pageSingle Line DiagramGhanshyam Singh100% (2)
- QUIZ - PFRS 1 - FIRST TIME ADOPTION OF PFRSsDocument2 pagesQUIZ - PFRS 1 - FIRST TIME ADOPTION OF PFRSsGonzalo Jr. Ruales86% (7)
- How To Apply For The UpcatDocument3 pagesHow To Apply For The UpcatAaron ReyesNo ratings yet
- Allama Iqbal Open University, Islamabad Warning: (Department of Secondary Teacher Education)Document2 pagesAllama Iqbal Open University, Islamabad Warning: (Department of Secondary Teacher Education)Tehmina HanifNo ratings yet
- Pas 38 Pas 41 Pas 40Document12 pagesPas 38 Pas 41 Pas 40Leddie Bergs Villanueva VelascoNo ratings yet
- Assignment On Industrial Relation of BDDocument12 pagesAssignment On Industrial Relation of BDKh Fahad Koushik50% (6)
- The US Navy - Fact File - MQ-8C Fire ScoutDocument2 pagesThe US Navy - Fact File - MQ-8C Fire ScoutAleksei KarpaevNo ratings yet