Professional Documents
Culture Documents
Kaplan - Porter - 2011 9 - How To Solve The Cost Crisis in Health Care - HBR
Uploaded by
bayu prabuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kaplan - Porter - 2011 9 - How To Solve The Cost Crisis in Health Care - HBR
Uploaded by
bayu prabuCopyright:
Available Formats
HBR.
ORG
Robert S. Kaplan is a Baker Michael E. Porter is the
Foundation Professor at Bishop William Lawrence
Harvard Business School. University Professor at
Harvard. He is based at
Harvard Business School.
How to Solve
The Cost Crisis
In Health Care
The biggest problem with health care isn’t
with insurance or politics. It’s that we’re
measuring the wrong things the wrong way.
by Robert S. Kaplan and Michael E. Porter
PHOTOGRAPHY: MARK HOOPER
September 2011 Harvard Business Review 47
1271 Sep11 Kaplan layout.indd 47 7/27/11 6:08:04 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE
U.S. health care costs
currently exceed 17% of
GDP and continue to rise.
Other countries spend less of their GDP on health care they are unable to link cost to process improvements
but have the same increasing trend. Explanations are or outcomes, preventing them from making sys-
not hard to find. The aging of populations and the de- temic and sustainable cost reductions. Instead, pro-
velopment of new treatments are behind some of the viders (and payors) turn to simplistic actions such
increase. Perverse incentives also contribute: Third- as across-the-board cuts in expensive services, staff
party payors (insurance companies and governments) compensation, and head count. But imposing arbi-
reimburse for procedures performed rather than out- trary spending limits on discrete components of care,
comes achieved, and patients bear little responsibility or on specific line-item expense categories, achieves
for the cost of the health care services they demand. only marginal savings that often lead to higher total
But few acknowledge a more fundamental source systems costs and poorer outcomes. For example, as
of escalating costs: the system by which those costs payors introduce high copayments to limit the use of
are measured. To put it bluntly, there is an almost expensive drugs, costs may balloon elsewhere in the
complete lack of understanding of how much it costs system should patients’ overall health deteriorate
to deliver patient care, much less how those costs and they subsequently require more services.
compare with the outcomes achieved. Instead of Poor cost measurement has also led to huge
focusing on the costs of treating individual patients cross-subsidies across services. Providers are gener-
with specific medical conditions over their full cycle ously reimbursed for some services and incur losses
of care, providers aggregate and analyze costs at the on others. These cross-subsidies introduce major
specialty or service department level. distortions in the supply and efficiency of care. The
Making matters worse, participants in the health inability to properly measure cost and compare cost
care system do not even agree on what they mean by with outcomes is at the root of the incentive problem
costs. When politicians and policy makers talk about in health care and has severely retarded the shift to
cost reduction and “bending the cost curve,” they are more effective reimbursement approaches.
typically referring to how much the government or Finally, poor measurement of cost and outcomes
insurers pay to providers—not to the costs incurred also means that effective and efficient providers go
by providers to deliver health care services. Cutting unrewarded, while inefficient ones have little incen-
payor reimbursement does reduce the bill paid by tive to improve. Indeed, institutions may be penalized
insurers and lowers providers’ revenues, but it does when the improvements they make in treatments
nothing to reduce the actual costs of delivering care. and processes reduce the need for highly reimbursed
Providers share in this confusion. They often allocate services. Without proper measurement, the healthy
their costs to procedures, departments, and services dynamic of competition—in which the highest-value
based not on the actual resources used to deliver care providers expand and prosper—breaks down. In-
but on how much they are reimbursed. But reim- stead we have zero-sum competition in which health
bursement itself is based on arbitrary and inaccurate care providers destroy value by focusing on highly
assumptions about the intensity of care. reimbursed services, shifting costs to other entities,
Poor costing systems have disastrous conse- or pursuing piecemeal and ineffective line-item cost
quences. It is a well-known management axiom that reductions. Current health care reform initiatives will
what is not measured cannot be managed or im- exacerbate the situation by increasing access to an in-
proved. Since providers misunderstand their costs, efficient system without addressing the fundamental
48 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 48 7/27/11 6:08:11 PM
HBR.ORG
Idea in Brief
Much of the rapid escalation Pilot projects under way at As providers and payors
in health care costs can be hospital systems in the U.S. better understand costs,
attributed to the fact that and Europe demonstrate the they will be positioned to
providers have an almost transformative effect of a achieve a true “bending of
complete lack of understand- new approach that accu- the cost curve” from within
ing of how much it costs to rately measures costs—at the system, not based on
deliver patient care. Thus the level of the individual top-down mandates.
they lack the knowledge nec- patient with a given medical The sheer size of the op-
essary to improve resource condition over a full cycle of portunity to reduce health
utilization, reduce delays, care—and compares those care costs—with no sacrifice
and eliminate activities that costs to outcomes. in outcomes—is astounding.
don’t improve outcomes.
value problem: how to deliver improved outcomes at The remedy to that are best addressed in a coordinated way and
a lower total cost. the cost crisis should be broadly defined to include common com-
Fortunately, we can change this state of affairs. does not require plications and comorbidities. The cost of treating a
And the remedy does not require medical science medical science patient with diabetes, for example, must include not
breakthroughs or top-down governmental regula- breakthroughs or only the costs associated with endocrinological care
tion. It simply requires a new way to accurately mea- but also the costs of managing and treating associ-
new governmental
sure costs and compare them with outcomes. Our ated conditions such as vascular disease, retinal dis-
regulation. It simply
approach makes patients and their conditions—not ease, and renal disease. For primary and preventive
departmental units, procedures, or services—the
requires a new care, the unit of value measurement is a particular
fundamental unit of analysis for measuring costs and way to accurately patient population—that is, a group with similar pri-
outcomes. The experiences of several major institu- measure costs and mary care needs, such as healthy children or the frail
tions currently implementing the new approach—the compare them with and elderly with multiple chronic conditions.
Head and Neck Center at MD Anderson Cancer Cen- outcomes. Let’s explore the first component of the health
ter in Houston, the Cleft Lip and Palate Program at care value equation: health outcomes. Outcomes for
Children’s Hospital in Boston, and units performing any medical condition or patient population should
knee replacements at Schön Klinik in Germany and be measured along multiple dimensions, including
Brigham & Women’s Hospital in Boston—confirm our survival, ability to function, duration of care, dis-
belief that bringing accurate cost and value measure- comfort and complications, and the sustainability
ment practices into health care delivery can have a of recovery. Better measurement of outcomes will,
transformative impact. by itself, lead to significant improvements in the
value of health care delivered, as providers’ incen-
Understanding the tives shift away from performing highly reimbursed
Value of Health Care services and toward improving the health status of
The proper goal for any health care delivery system patients. Approaches for measuring health care out-
is to improve the value delivered to patients. Value comes have been described previously, notably in
in health care is measured in terms of the patient Michael Porter’s 2010 New England Journal of Medi-
outcomes achieved per dollar expended. It is not cine article, “What Is Value in Health Care?”
the number of different services provided or the vol- While measuring medical outcomes has received
ume of services delivered that matters but the value. growing attention, measuring the costs required to
More care and more expensive care is not necessarily deliver those outcomes, the second component of the
better care. value equation, has received far less attention. In the
To properly manage value, both outcomes and value framework, the relevant cost is the total cost of
cost must be measured at the patient level. Measured all resources—clinical and administrative personnel,
outcomes and cost must encompass the entire cycle drugs and other supplies, devices, space, and equip-
of care for the patient’s particular medical condition, ment—used during a patient’s full cycle of care for a
which often involves a team with multiple specialties specific medical condition, including the treatment
performing multiple interventions from diagnosis to of associated complications and common comorbidi-
treatment to ongoing management. A medical con- ties. We increase the value of health care delivered
dition is an interrelated set of patient circumstances to patients by improving outcomes at similar costs or
September 2011 Harvard Business Review 49
1271 Sep11 Kaplan layout.indd 49 7/27/11 6:08:11 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE
by reducing the total costs involved in patients’ care tools in place, health care providers can utilize medi-
while maintaining the quality of outcomes. cal staff, equipment, facilities, and administrative re-
A powerful driver of value in health care is that sources far more efficiently, streamline the path of
better outcomes often go hand in hand with lower to- patients through the system, and select treatment
tal care cycle costs. Spending more on early detection approaches that improve outcomes while eliminat-
and better diagnosis of disease, for example, spares ing services that do not.
patients suffering and often leads to less complex
and less expensive care later. Reducing diagnostic The Challenges of Health Care Costing
and treatment delays limits deterioration of health Accurate cost measurement in health care is chal-
and also lowers costs by reducing the resources re- lenging, first because of the complexity of health care
quired for care. Indeed, the potential to improve out- delivery itself. A patient’s treatment involves many
comes while driving down costs is greater in health different types of resources—personnel, equipment,
care than in any other field we have encountered. space, and supplies—each with different capabilities
The key to unlocking this potential is combining an and costs. These resources are used in processes that
accurate cost measurement system with the system- start with a patient’s first contact with the organiza-
atic measurement of outcomes. With these powerful tion and continue through a set of clinical consulta-
Myth #1
Charges are a good surrogate for provider costs.
The widespread confusion between deeply flawed assumption that every estimates are not systematically mea-
what a provider charges, what it is billable event in a department has the sured or confirmed in practice settings.
actually reimbursed, and its costs is a same profit margin. Reimbursement- Reimbursing physicians on the basis of
major barrier to reducing the cost of based costing also buries the costs of highly aggregate and likely inaccurate
health care. Providers have aggravated valuable but nonbillable events, such estimates of their costs introduces
this problem by structuring impor- as patient consultations, in large over- major incentive problems into the
tant aspects of their costing systems head pools that are allocated arbitrarily health care system. But the problems
around the way they are reimbursed. and inaccurately to billable events. are compounded when the reimburse-
In the U.S., this is partly a histori- Although costing systems for physi- ment rates are also used to allocate
cal artifact of the Medicare cost-plus cian services differ from those used by physician costs to patients, a purpose
reimbursement system, which requires hospitals, they suffer from the same for which they were never intended.
hospital departments to prepare an problems. As is the case for hospitals, We need to abandon the idea that
annual Medicare Cost Report (MCR), U.S. physicians are reimbursed not on charges billed or reimbursements paid
detailing costs and charges by depart- the basis of an individual patient’s re- in any way reflect costs. In reality, the
ment. Rather than developing and source use but on average estimates of cost of using a resource—a physician,
maintaining accurate costing systems relative demands—relative value units, nurse, case manager, piece of equip-
that are based on actual resource or RVUs—on physician labor, practice ment, or square meter of space—is the
usage, separate from the regulatory expenses, and malpractice expenses same whether the resource is perform-
standard required for reimbursement, in performing billable activities. These ing a poorly or a highly reimbursed
hospitals defaulted to reimbursement- resource estimates are derived from service. Cost depends on how much of
driven systems. specialty panels and national surveys a resource’s available capacity (time)
Unfortunately, that approach was of physicians, who stand to gain from is used in the care for a particular pa-
flawed from the start because it was overestimating the time and complex- tient, not on the charge or reimburse-
based on the use of highly aggregate ity of their work. Despite the required ment for the service, or whether it is
data for estimating costs and the sign-off by government payors, the RVU reimbursed at all.
1271 Sep11 Kaplan layout.indd 50 7/27/11 6:08:12 PM
HBR.ORG
FURTHER READING
FROM THE AUTHORS
MEASURING VALUE
AND OUTCOMES
tions, treatments, and administrative processes until spends with each resource. (See Robert S. Kaplan
the patient’s care is completed. The path that the pa- and Steven R. Anderson’s “Time-Driven Activity- “What Is Value in
tient takes through the system depends on his or her Based Costing,” HBR 2004.) Health Care?”
by M.E. Porter
medical condition. In its initial implementation, such a costing sys- New England Journal of
The already complex path of care is further com- tem may appear complex. But the complexity arises Medicine, 2010
plicated by the highly fragmented way in which not from the methodology but from today’s idiosyn-
Redefining Health Care:
health care is delivered today. Numerous distinct and cratic delivery system, with its poorly documented Creating Value-Based
largely independent organizational units are involved processes for treating patients with particular condi- Competition on Results
in treating a patient’s condition. Care is also idiosyn- tions and its inability to map asset and expense cat- by M.E. Porter and
E.O. Teisberg
cratic; patients with the same condition often take egories to patient processes. As health care providers Harvard Business Review
different paths through the system. The lack of stan- begin to reorganize into units focused on conditions, Press, 2006
dardization stems to some extent from the artisanal standardize their protocols and treatment processes,
“A Strategy for Health
nature of medical practice—physicians in the same and improve their information systems, using the Care Reform: Towards a
organizational unit performing the same medical TDABC system will become much simpler. Value-Based System”
process (for instance, total knee replacement) often To see how TDABC works in the health care con- by M.E. Porter
New England Journal of
use different procedures, drugs, devices, tests, and text, we first explore a simplified example. Medicine, 2009
equipment. In operational terms, you might describe
health care today as a highly customized job shop. Costing the Patient: A Simple Example
TIME-DRIVEN
Existing costing systems, which measure the Consider Patient Jones, who makes an outpatient ACTIVITY-BASED
costs of individual departments, services, or sup- visit to a clinic. To estimate the total cost of Jones’s COSTING
port activities, often encourage the shifting of costs care, we first identify the processes he undergoes
Time-Driven Activity-
from one type of service or provider to another, or and the resources used in each process. Let’s assume Based Costing:
to the payor or consumer. The micromanagement of that Jones uses an administrative process for check- A Simpler and More
costs at the individual organizational unit level does in, registration, and obtaining documentation for Powerful Path to
Higher Profits
little to reduce total cost or improve value—and may third-party reimbursement; and a clinical process by R.S. Kaplan and
in fact destroy value by reducing the effectiveness of for treatment. Just three clinical resources are re- S.R. Anderson
care and driving up administrative costs. (For more quired: an administrator (Allen), a nurse (White), Harvard Business Review
Press, 2007
on the problems with current costing systems, see and a physician (Green).
the three Myth sidebars.) We begin by estimating the first of the two param- Cost and Effect: Using
Any accurate costing system must, at a fundamen- eters: the quantity of time (capacity) the patient uses Integrated Cost Systems
To Drive Profitability and
tal level, account for the total costs of all the resources of each resource at each process. From information Performance
used by a patient as she or he traverses the system. supplied by the three staffers, we learn that Jones by R.S. Kaplan and
That means tracking the sequence and duration of spent 18 minutes (0.3 hours) with Administrator R. Cooper
Harvard Business Review
clinical and administrative processes used by individ- Allen, 24 minutes (0.4 hours) with Nurse White for Press, 1998
ual patients—something that most hospital informa- a preliminary examination, and nine minutes (0.15
tion systems today are unable to do. This deficiency hours) with Physician Green for the direct examina-
can be addressed; technology advances will soon tion and consultation.
greatly improve providers’ ability to track the type Next, we calculate the capacity cost rate for each
and amount of resources used by individual patients. resource—that is, how much it costs, per hour or
In the meantime, it is possible to determine the pre- per minute, for a resource to be available for patient-
dominant paths followed by patients with a particular related work—using the following equation:
medical condition, as our pilot sites have done.
With good estimates of the typical path an indi- Capacity Cost Expenses Attributable to Resourcei
Rate for Resourcei = Available Capacity of Resource
vidual patient takes for a medical condition, provid- i
ers can use the time-driven activity-based costing The numerator aggregates all the costs associated
(TDABC) system to assign costs accurately and rela- with supplying a health care resource, such as Allen,
tively easily to each process step along the path. This White, or Green. It starts with the full compensation
improved version of activity-based costing requires of each person, including salary, payroll taxes, and
that providers estimate only two parameters at each fringe benefits such as health insurance and pen-
process step: the cost of each of the resources used sions. To that we add the costs of all other associated
in the process and the quantity of time the patient resources that enable Allen, White, and Green to be
September 2011 Harvard Business Review 51
1271 Sep11 Kaplan layout.indd 51 7/27/11 6:08:27 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE HBR.ORG
available for patient care. These typically include a Let’s assume that similar calculations yield
pro rata share of costs related to employee supervi- capacity cost rates for Administrator Allen and
sion, space (the offices each staffer uses), and the Physician Green of $45 per hour and $300 per hour,
equipment, information technology, and telecom- respectively.
munications each uses in the normal course of work. We calculate the total cost of Jones’s visit to the fa-
In this way, the cost of many of the organization’s cility by simply multiplying the capacity cost rate of
shared or support resources can be assigned to the each resource by the time (in hours) Jones spent using
resources that directly interact with the patient. the resource, and then adding up the components:
Supervision cost, for example, can be calculated As this example
on the basis of how many people a manager super- demonstrates, ac- (0.3 hours × $45)
(0.4 hours × $65)
vises. Space costs are a function of occupancy area curately calculating + (0.15 hours × $300)
and rental rates; IT costs are based on an individual’s the cost of delivering Total cost of visit: $84.50
use of computers and communications products and health care is quite
services. Assume that we find Nurse White’s total straightforward under the TDABC system. Although
cost to be as follows: the example is admittedly simplified, it captures al-
most all the fundamental concepts any health care
Annual compensation provider needs to apply to estimate the cost of treat-
(including fringe benefits) $65,000 ing patients over their full cycles of care.
Supervision cost By capturing all the costs over the complete cycle
(10% of nursing supervisor’s full cost) $9,000 of care for an individual patient’s medical condition,
Occupancy (9 sq. meters of space we allow providers and payors to address virtually
@ $1,200/sq. meter/year) $10,800 any costing question. Providers can aggregate and
Technology and support $2,560 analyze patients’ cost of care by age, gender, and
Annual total cost of Nurse White $87,360 comorbidity, or by treatment facility, physician, em-
Monthly total cost of Nurse White $7,280 ployer, and payor. They can calculate total and aver-
age costs for any category or subcategory of patients
We next calculate Nurse White’s availability for while still capturing the detailed data on individual
patient care—the denominator of our capacity cost patients needed to understand the sources of cost
rate equation. This calculation starts with 365 days variation within each category.
per year and subtracts all the time that the employee
is not available for work. The calculation for Nurse The Cost Measurement Process
White is as follows: Moving beyond the simplified example, let’s now
look at the seven steps our pilot sites are using to
Start with 365 days per year estimate the total costs of treating their patient
less weekend days 104 populations.
less vacation days 20 1. Select the medical condition. We begin by
less holidays 12 specifying the medical condition (or patient popula-
less sick days 5 tion) to be costed, including the associated compli-
224 available days per year cations and comorbidities that affect processes and
18.7 days per month resources used during the patient’s care. For each
condition, we define the beginning and end of the
Start with 7.5 hours per available day patient care cycle. For chronic conditions, we choose
less scheduled breaks (hours) 0.5 a care cycle for a period of time, such as a year.
less meetings, training, education 1.0 2. Define the care delivery value chain. Next,
Available clinical hours 6 hours per day we specify the care delivery value chain (CDVC),
which charts the principal activities involved in a
Nurse White is therefore available for patient patient’s care for a medical condition along with
work 112 hours per month (6 hours a day for 18.7 their locations. The CDVC focuses providers on
days). Dividing the monthly cost of the resource the full care cycle rather than on individual pro-
($7,280) by monthly capacity (112 hours) gives us cesses, the typical unit of analysis for most process
Nurse White’s capacity cost rate: $65 per hour. improvements and lean initiatives in health care.
52 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 52 7/27/11 6:08:28 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE HBR.ORG
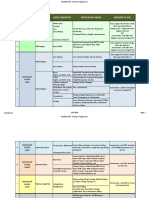
CREATING A COST
MEASUREMENT
SYSTEM
1Select the medical
condition and/or (The exhibit “The Care Delivery Value Chain” shows who needs a laryngoscopy as part of her clinical visit
patient population the CDVC developed with the Brigham & Women’s requires an additional process step. The time esti-
to be examined pilot site for patients with severe knee osteo- mate and associated incremental resources required
arthritis.) This overall view of the patient care cycle can be easily added to the overall time equation for
2Define the care
helps to identify the relevant dimensions along
which to measure outcomes and is also the start-
ing point for mapping the processes that make up
that patient. (See again the process map exhibit.)
To estimate standard times and time equations,
our pilot sites have found it useful to bring together
delivery value chain each activity. all the people involved in a set of processes for fo-
3. Develop process maps of each activity in cused discussion. In the future, we expect providers
3Develop process
patient care delivery. Next we prepare detailed
process maps for each activity in the care delivery
will use electronic handheld, bar-code, and RFID
devices to capture actual times, especially if TDABC
value chain. Process maps encompass the paths becomes the generally accepted standard for mea-
maps of each activ-
patients may follow as they move through their suring the cost of patient care.
ity in patient care
care cycle. They include all the capacity-supplying 5. Estimate the cost of supplying patient
delivery; identify the
resources (personnel, facilities, and equipment) in- care resources. In this step, we estimate the direct
resources involved
volved at each process along the path, both those costs of each resource involved in caring for patients.
and any supplies
directly used by the patient and those required to The direct costs include compensation for employ-
used for the patient
make the primary resources available. (The exhibit ees, depreciation or leasing of equipment, supplies,
at each process
“New-Patient Process Map” shows a process map for or other operating expenses. These data, gathered
one segment of the patient care cycle at the MD An- from the general ledger, the budgeting system, and
4Obtain time
derson Head and Neck Center.) In addition to identi-
fying the capacity-supplying resources used in each
other IT systems, become the numerator for calcu-
lating each resource’s capacity cost rate.
estimates for each process, we identify the consumable supplies (such We must also account for the time that many
process step as medications, syringes, catheters, and bandages) physicians, particularly in academic medical centers,
used directly in the process. These do not have to be spend teaching and doing research in addition to their
5Estimate the cost
shown on the process maps.
Our pilot sites used several approaches for creat-
ing process maps. Some project teams interviewed
clinical responsibilities. We recommend estimating
the percentage of time that a physician spends on
clinical activities and then multiplying the physi-
of supplying each clinicians individually to learn about patient flow, cian’s compensation by this percentage to obtain the
patient care while others organized “power meetings” in which amount of pay accounted for by the physician’s clini-
resource people from multiple disciplines and levels of man- cal work. The remaining compensation should be
agement discussed the process together. Even at this assigned to teaching and research activities.
6Estimate the practi-
early stage in the project, the sessions occasionally
identified immediate opportunities for process and
Next, we identify the support resources neces-
sary to supply the primary resources providing pa-
cost improvement. tient care. For personnel resources, as illustrated in
cal capacity of each
4. Obtain time estimates for each process. the Patient Jones example, these include supervising
resource provider,
We also estimate how much time each provider or employees, space and furnishings (office and patient
and calculate the
other resource spends with a patient at each step in treatment areas), and corporate functions that sup-
capacity cost rate
the process. When a process requires multiple re- port patient-facing employees. When calculating the
sources, we estimate the time required by each one. cost of supplies, we include the cost of the resources
7Compute the total
For short-duration, inexpensive processes that
vary little across patients, we recommend using stan-
used to acquire them and make them available for
patient use during the treatment process (for in-
costs over each pa- dard times (rather than investing resources to record stance, purchasing, receiving, storage, sterilization,
tient’s cycle of care actual ones). Actual duration should be calculated and delivery).
for time-consuming, less predictable processes, es- Finally, we need to allocate the costs of depart-
pecially those that involve multiple physicians and ments and activities that support the patient-facing
nurses performing complex care activities such as work. We map those processes as we did in step 3
major surgery or examination of patients with com- and then calculate and assign costs to patient-facing
plicated medical circumstances. resources on the basis of their demands for the ser-
TDABC is also well suited to capture the effect vices of these departments, using the process that
of process variation on cost. For example, a patient will be described in step 6.
54 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 54 7/27/11 6:08:28 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE
CASE STUDY: THE CARE DELIVERY VALUE CHAIN
Severe Knee Osteoarthritis Requiring Replacement
The care delivery value chain is both a descriptive and prescriptive tool. By systematically mapping the full set
of activities delivered over the cycle of care for a medical condition, spanning multiple providers and nonclinical
care settings, the CDVC enables analysis of how the set of activities together generates patient value and offers
providers a systematic approach to analyze, improve, and integrate the configuration of care delivery.
INFORMING • Importance of • Meaning of diagnosis • Setting expectations • Expectations for • Importance of rehab • Importance of
AND exercise, weight recovery adherence exercise, maintaining
ENGAGING • Prognosis (short- • Importance of
reduction, proper and long-term nutrition, weight loss, • Importance of rehab • Longitudinal care healthy weight
What do nutrition outcomes) vaccinations plan
patients • Post-surgery risk
need to be • Drawbacks and • Home preparation factors
educated benefits of surgery
about?
MEASURING • Joint-specific • Loss of cartilage • Baseline health • Blood loss • Infections • Joint-specific
What measures symptoms and • Change in status • Operative time • Joint-specific symptoms and
need to be function (e.g., subchondral bone • Fitness for surgery symptoms and function
collected? WOMAC scale) • Complications
• Joint-specific (e.g., ASA score) function • Weight gain or loss
• Overall health (e.g.,
SF-12 scale) symptoms and • Inpatient length • Missed work
function of stay • Overall health
• Overall health • Ability to return to
normal activities
ACCESSING • PCP office • Specialty office • Specialty office • Operating room • Nursing facility • Specialty office
Where do
patient care • Health club • Imaging facility • Pre-op evaluation • Recovery room • Rehab facility • Primary care office
activities take • Physical therapy clinic center • Orthopedic floor at • Physical therapy • Health club
place? hospital or specialty clinic
surgery center • Home
TYPICAL PATH OF PATIENT CARE
MONITORING/ DIAGNOSING PREPARING INTERVENING RECOVERING/ MONITORING/
PREVENTING REHABBING MANAGING
CARE MONITOR IMAGING Overall prep ANESTHESIA SURGICAL MONITOR
DELIVERY • Conduct PCP exam • Perform and evaluate • Conduct home • Administer • Immediate return to • Consult regularly
What activities • Refer to specialists, MRI and x-ray assessment anesthesia (general, OR for manipulation, with patient
are performed if necessary –Assess cartilage loss • Monitor weight loss epidural, or if necessary
at each stage? –Assess bone regional) MANAGE
alterations MEDICAL
PREVENT SURGICAL PREP • Prescribe
SURGICAL • Monitor coagulation prophylactic
• Prescribe anti- CLINICAL EVALUATION • Perform cardiology, PROCEDURE
inflammatory pulmonary LIVING antibiotics when
medicines • Review history and evaluations • Determine approach needed
imaging (e.g., minimally • Provide daily living
• Recommend exercise • Run blood labs invasive) support (showering, • Set long-term
regimen • Perform physical dressing) exercise plan
exam • Conduct pre-op • Insert device
• Set weight loss targets physical exam • Track risk indicators • Revise joint, if
• Recommend • Cement joint necessary
treatment plan (fever, swelling,
(surgery or other PAIN MANAGEMENT other)
options) • Prescribe preemp- PHYSICAL THERAPY
tive multimodal pain
ORTHOPEDIC meds • Daily or twice daily
SURGEON PT sessions
For more on the CDVC, see Redefining Health Care: Creating Value-Based Competition on Results, by M.E. Porter and E.O. Teisberg (Harvard Business Review Press, 2006).
This approach to allocating support costs repre- When costing support departments, a good
sents a major shift from current practice. To illustrate, guideline is the “rule of 1.” Support functions that
let’s compare the allocation of the resources required have only one employee can be treated as a fixed
in a centralized department to sterilize two kinds of cost; they can be either not allocated at all or allo-
surgical tool kits, those used for total knee replace- cated using a simplistic method, as is currently done.
ment and those used for cardiac bypass. Existing But departments that have more than one person or
cost systems tend to allocate higher sterilization more than one unit of any resource represent vari-
costs to cardiac bypass cases than to knee replace- able costs. The workload of these departments has
ment cases because the charges (or direct costs) are expanded because of increased demand for the ser-
higher for a cardiac bypass than for a knee replace- vices and outputs they provide. Their costs should
ment. Under TDABC, however, we have learned that and can be assigned on the basis of the patient pro-
more time and expense are required to sterilize the cesses that create demand for their services.
typically more complex knee surgery tools, so rela- Project teams tasked with estimating the cost to
tively higher sterilization costs should be assigned to supply resources—the numerator of the capacity
knee replacements. cost rate—should have expertise in finance, human
56 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 56 7/27/11 6:08:28 PM
Myth #2
resources, and information systems. They can do Hospital overhead costs
this work in parallel with the process mapping and
time estimation (steps 3 and 4) performed by clini-
are too complex to allocate
cians and team members with expertise in quality accurately.
management and process improvement.
6. Estimate the capacity of each resource, Most health care leaders will eventually accept the idea that
and calculate the capacity cost rate. Deter- the direct costs of patient care, such as nurses, physicians, and
mining the practical capacity for employees—the consumable supplies (drugs, bandages, and syringes), ought to
denominator in the capacity cost rate equation—re- be assigned more accurately to individual patients. But many
quires three time estimates, which are gathered from leaders believe that allocating the costs of indirect and support
HR records and other sources: units cannot be done except with crude, arbitrary methods,
a. The total number of days that each employee often dressed up to look sophisticated. Typically, they use a
actually works each year. “peanut butter” method, which spreads overhead and sup-
b. The total number of hours per day that the em- port costs across each department’s billable activities (see
ployee is available for work. Myth #1) using metrics such as the size of direct costs, head
c. The average number of hours per workday used count, length of stay, assigned physical space, number of
for nonpatient-related work, such as breaks, training, patients, number of procedures, RVUs supplied, or costs-
education, and administrative meetings. to-charge ratios (Myth #1 again).
The effect of such arbitrary support-department al-
Monthly Practical a × (b c)
= 12 ⁻
Capacity of Resource locations on the measured cost of services can be pro-
found. In the past, Schön Klinik, like other hospitals in
For physicians who divide their time among clinical, Germany, had reduced the capacity of its total knee
research, and education activities, we subtract time replacement rehabilitation units in part because the
spent on research and education activities to obtain existing cost system portrayed them as less profit-
the number of hours per month that they are avail- able than acute-care units. During Schön Klinik’s cost
able for clinical work. pilot, the project team discovered that the existing
For equipment resources, we measure capacity cost system allocated support-department costs
by estimating the number of days per month and the largely on the basis of length of patient stay, not on
number of hours per day that each piece of equip- the patient’s use of support resources. Since Schön
ment can be used. This represents the upper limit on total knee replacement patients spent 75% of their
the capacity of the equipment. The actual capacity stay in the rehab facility, rehab had been allocated
utilization of much health care equipment is some- about 75% of support department costs.
times lower because equipment capacity is sup- The TDABC analysis showed, however, that the de-
plied in large lumps. For instance, suppose a piece mand for many support-unit services, such as medi-
of equipment can do 10,000 blood tests a month. A cal billing, is far higher during the days a patient
hospital decides to buy the equipment knowing that spends in the acute-care facility than during rehab
it needs to process only 6,000 tests per month. In days. With support costs properly assigned, the rehab
this case, we make an adjustment: The costing sys- facility showed improved profitability. Schön Klinik be-
tem should use the time required to perform 6,000 gan to contemplate the expansion of its rehabilitation
tests as the capacity of the resource. Otherwise, the capacity—a complete reversal of its previous decision—
tests actually performed on the equipment will, at and shifted its focus more intensively on reducing sup-
best, cover only 60% of its cost. If the provider sub- port costs incurred during the acute-care stay.
sequently ends up using the equipment for a higher Once indirect costs have been accurately assigned,
number of tests, it can adjust the capacity rate managers and physicians can look for ways to reduce
accordingly. demand for support-department services and improve
This treatment of capacity follows the rule of 1 and the efficiency with which they are delivered. That, in turn,
should be applied when the organization has only will enable organizations to lower their spending on these
one unit of the equipment. Now suppose a provider resources.
has 12 facilities that each use equipment capable of
performing 10,000 blood tests per month—but each
facility performs only 6,000 tests per month. In that
1271 Sep11 Kaplan layout.indd 57 8/9/11 9:17:22 AM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE
New-Patient
Process Map
This process map
describes a seg-
ment of the patient
case, the capacity of each resource unit should be set processes and restructure care delivery. Capitalizing care cycle at MD
at the full 10,000 tests per month, not its expected on these value-creating opportunities—previously
Anderson Head
number. We want the system to signal the cost of hidden by inadequate and siloed costing systems—
and Neck Center.
unused capacity when a provider chooses to supply is the key to solving the health care cost problem.
capacity at multiple locations or facilities rather than Let’s examine some of the most promising opportu-
Process maps
consolidating its use of expensive equipment. nities that proper costing reveals. show the resources
In addition to the lumpiness with which capac- Eliminate unnecessary process variations required for each
ity gets acquired, factors such as peak load demands, and processes that don’t add value. In our pilots, activity and often
surge capacity, and capacity acquired for future we have documented significant variation in the reveal immediate
growth should be accounted for. This applies to both processes, tools, equipment, and materials used by opportunities for
equipment and personnel. (Those factors can be in- physicians performing the same service within the process improve-
corporated, but the treatment is beyond the scope same unit in the same facility. For example, in total ment and cost
of this article.) knee replacement, surgeons use different implants, reduction.
In practice, we have found that underutilization surgical kits, surgeons’ hoods, and supplies, thereby
of expensive equipment capacity is often not a con- introducing substantial cost variation in treating pa-
scious decision but a failure of the costing system tients with the same condition at the same site. The
to provide visibility into resource utilization. That surgical unit now measures the costs and outcomes
problem is corrected by the TDABC approach. We that each surgeon produces. As a result, clinical
describe opportunities to improve resource capacity practice leaders are able to have more constructive
utilization later in the article. and better informed discussions about how best to
To calculate the resource capacity cost rate, we standardize care and treatment processes to reduce
simply divide the resource’s total cost (step 5) by its the costs of variability and limit the use of expensive
practical capacity (step 6) to obtain a rate, measured approaches and materials that do not demonstrably
in dollars or euros per unit of time, typically an hour lead to improved outcomes.
or a minute. In addition to reducing process variations, our
7. Calculate the total cost of patient care. pilot sites have eliminated steps or entire processes
Steps 3 through 6 establish the structure and data that did not improve outcomes. Schön Klinik, for
components of the TDABC system. In the final step, example, lowered costs by reducing the breadth of
the project team estimates the total cost of treating a tests included in its common laboratory panel after
patient by simply multiplying the capacity cost rates learning that many of the tests did not provide new
(including associated support costs) for each re- information that would lead to improvement in
source used in each patient process by the amounts outcomes.
of time the patient spent with the resource (step 4). Comparing practices across different countries
Sum up all the costs across all the processes used for the same condition also reveals major opportuni-
during the patient’s complete cycle of care to pro- ties for improvement. The reimbursement for a total
duce the total cost of care for the patient. joint replacement care cycle in Germany and Swe-
den is approximately $8,500, including all physician
Opportunities to Improve Value and technical services and excluding only outpatient
Our new approach actively engages physicians, clini- rehabilitation. The comparable figure in U.S. medi-
cal teams, administrative staff, and finance profes- cal centers is $30,000 or more. Since providers in all
sionals in creating the process maps and estimating three countries report, in aggregate, similar margins
the resource costs involved in treating patients over on joint replacement care, U.S. providers’ costs are
their care cycle. This bridges the historical divide be- likely two to three times as high as those of their
tween managers and clinical teams that has often led European counterparts. By comparing process maps
to tensions and stalemates over cost-cutting steps. and resource costs for the same medical condition
TDABC builds a common information platform that across multiple sites, we can determine how much of
will unleash innovation based on a shared under- the cost difference is attributable to variations in pro-
standing of the actual processes of care. Even at our cesses, protocols, and productivity and how much is
pilot site Schön Klinik, which already had an excel- attributable to differences in resource or supply costs
lent departmental cost-control system, introducing such as wages and implant prices. Our initial research
TDABC revealed powerful new ways to improve its suggests that although inputs are more expensive in
58 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 58 7/27/11 6:08:38 PM
HBR.ORG
Registration and Plan of Care Plan of Care
Verification Intake Clinician Visit Discussion Scheduling
Resources: Receptionist, patient access Nurse, receptionist MD, mid-level Registered nurse, medical doctor, Patient service
specialist, interpreter provider, medical patient service coordinator coordinator
assistant, patient
service coordina-
Patient arrives tor, RN
Check in patient; Verify patient Assess patient; Initiate patient Discuss plan Review plan of Schedule tests
communicate information; assemble paper- workup; review of care care; introduce and consults;
arrival complete con- work; place patient history; MD team; review communicate
RCPT, PAS patient in room conduct physi- schedule for schedule to
sent forms patient
2 PAS RN cal exam
MLP
return visit
RN PSC
MIN
40 20 45 30 15 5
MIN MIN MIN MIN MIN MIN
Clean room;
Patient
complete paper-
Laryngoscopy NO work; check
Receptionist needed? e-mail and voice- Scheduled
90%
mail for updates for same day?
Interpreter
or changes to
RN Registered Nurse plan of care
YES RN
MLP Mid-Level Provider 10%
10 YES
90%
MA Medical Assistant MIN
MD Medical Doctor Perform
laryngoscopy
PAS Patient Access Specialist
MD, MA, PSC
Enter next
process
PSC Patient Service Coordinator
10 Changes to
MIN plan of care? NO
90%
NO
10%
YES
10%
Patient
Notify patient departs
of changes
RN
30
MIN
the United States, the higher cost in U.S. facilities is nation and delays when a patient is handed off from
mainly due to lower resource productivity. one specialty or service to the next. Another cause of
Improve resource capacity utilization. The low resource utilization is having specialized equip-
TDABC approach identifies how much of each re- ment available just in case the need arises. Some
source’s capacity is actually used to perform pro- facilities that serve patients with unpredictable and
cesses and treat patients versus how much is unused rare medical needs make a deliberate decision to
and idle. Managers can clearly see the quantity and carry extra capacity. In such cases, an understanding
cost of unused resource capacity at the level of in- of the actual cost of excess capacity should trigger a
dividual physicians, nurses, technicians, pieces of discussion on how best to consolidate the treatment
equipment, administrators, or organizational units. of such patients. Much excess resource capacity,
Resource utilization data also reveal where increas- however, is due not to rare conditions or poor hand-
ing the supply of certain resources to ease bottle- offs but to the prevailing tendency of many hospi-
necked processes would enable more timely care tals and clinics to provide care for almost every type
and serve more patients with only modestly higher of medical problem. Such fragmentation of service
expenditures. lines introduces costly redundancy throughout the
When managers have greater visibility into areas health care system. It can also lead to inferior out-
where substantial and expensive unused capacity comes when providers handle a low volume of cases
exists, they can identify the root causes. For ex- of each type. Accurate costing gives managers a
ample, some underutilization of expensive space, valuable tool for consolidating patient care for low-
equipment, and personnel is caused by poor coordi- volume procedures in fewer institutions, which
September 2011 Harvard Business Review 59
1271 Sep11 Kaplan layout.indd 59 7/27/11 6:08:38 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE
would both reduce the high costs of unused capacity physicians and other skilled staff members require
and improve outcomes. their level of expertise and training. The process
Deliver the right processes at the right lo- maps developed for TDABC often reveal opportuni-
cations. Many services today are delivered in over- ties for appropriately skilled but lower-cost health
resourced facilities or facilities designed for the most care professionals to perform some of the processes
complex patient rather than the typical patient. By currently performed by physicians without adversely
accurately measuring the cost of delivering the affecting outcomes. Such substitutions would free
same services at different facilities, rather than us- up physicians and nurses to focus on their highest-
ing figures based on averaged direct costs and inac- value-added roles. (For an example from one of our
curate overhead allocations, providers are able to pilot sites, see the sidebar “A Cancer Center Puts the
see opportunities to perform particular services at New Approach to Work.”)
properly resourced and lower-cost locations. Such Speed up cycle time. Health care providers
realignment of care delivery, already under way at have multiple opportunities to reduce cycle times for
Children’s Hospital Boston, improves the value and treating patients, which in turn will reduce demand
convenience of more routine services for both pa- for resource capacity. For example, reducing the
tients and caregivers while allowing tertiary facilities time that patients have to wait will reduce demand
to concentrate their specialized resources on truly for patient supervision and space. Speeding up cycle
complex care. time also improves outcomes, both by minimizing
Match clinical skills to the process. Re- the duration of patient uncertainty and discomfort
source utilization can also be improved by examin- and by reducing the risk of complications and mini-
ing whether all the processes currently performed by mizing disease progression. As providers improve
Myth #3
Most health care costs are fixed.
Many health care system participants, If most costs were fixed, growth in ment inattention, not of the nature
including economists and accoun- demand for health care would increase of those costs.
tants, believe that most costs in only that small fraction of costs that Space costs are also not fixed.
health care are fixed because so much are variable, leading to lower average Space is perhaps an organization’s
care is delivered using shared staff, costs in the system, not the dramati- most fungible resource. If demand for
space, and equipment. The result of cally higher share of GDP now being space is reduced, units can be consoli-
this misguided thinking is that cost devoted to health care. dated into smaller space, and excess
reduction efforts tend to focus on only To understand why most health space can be repurposed, sold, or sub-
the small fraction of costs seen as care costs are not fixed, start with leased. Similarly, equipment costs can
variable, such as drugs and supplies, personnel costs, which are gener- be avoided if changes in processes,
which are sometimes referred to as ally at least 50% of the total costs treatment protocols, or patient mix
marginal or incremental costs. This of health care providers, according eliminate the demand for the re-
myth also motivates some health care to American Hospital Association sources. Equipment no longer needed
organizations to expand through merg- statistics. Hint: Personnel costs are can be retired or sold to other health
ers, acquisitions, and organic growth not fixed. Hospital executives can set care institutions that are expanding
in order to reap economies of scale the quantity, mix, and compensation their capacity.
by spreading their fixed costs over an of their personnel each year, or even All told, we estimate that upwards
increased volume of business. more frequently. Personnel costs are of 95% of what health care manag-
But if most health care costs were fixed only when executives allow them ers think of as fixed costs are actually
truly fixed, we would not have the to be. The claim that personnel costs under their control and therefore not
health care cost problem we do today. are fixed is a reflection of manage- really fixed.
60 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 60 7/27/11 6:08:39 PM
HBR.ORG
their process flows and reduce redundancy, their PILOT
patients will no longer have to be so “patient” as they
receive a complete cycle of care.
Optimize over the full cycle of care. Health
care providers today are typically organized around
A Cancer
Center Puts
specialties and services, which complicates coordi-
nation, interrupts the seamless, integrated flow of
patients from one process to the next, and leads to
the duplication of many processes. In the typical
care delivery process, for example, patients see mul-
tiple providers in multiple locations and undergo
a separate scheduling interaction, check-in, medi-
cal consultation, and diagnostic workup for each
one. This wastes resources and creates delays. The
The New
TDABC model makes visible the high costs of these
redundant administrative and clinical processes,
motivating professionals from different depart-
ments to work together to integrate care across de-
Approach
partments and specialties. Eliminating unnecessary
administrative and clinical processes represents one
of the biggest opportunities for lowering costs.
With a complete picture of the time and resources
involved, providers can optimize across the entire
To Work
care cycle, not just the parts. Physicians and staff by Heidi W. Albright, MHA, and Thomas W. Feeley, MD
may shift more of their time and resources to the
front end of the care cycle—to activities such as pa-
tient education and clinical team consultations—to
reduce the likelihood of patients experiencing far
more costly complications and readmissions later in
T
the cycle.
Additionally, this resource- and process-based ap- he University of Texas MD Anderson Cancer Center
proach gives providers visibility into valuable non- is a National Cancer Institute–designated Compre-
billed events in the cycle of care. These activities— hensive Cancer Center, located in Houston, Texas.
such as nurse counseling time, physician phone Seeing more than 30,000 new patients every year,
calls to patients, and multidisciplinary care team MD Anderson accounts for approximately 20% of
meetings—can often make major contributions to cancer care within the Houston region and 1% of
efficiency and favorable outcomes. Because existing cancer care nationally. MD Anderson is a medical
systems hide these costs in overhead (see Myth #1), condition–focused center that provides integrated,
such important elements of care are prone to be min- interdisciplinary care across the care cycle.
imized or left unmanaged. In collaboration with Michael Porter, we em-
barked on a major effort to expand clinical outcome measurement, begin-
Capturing the Payoffs ning with a study of 2,468 patients in the Head and Neck Center, in 2008.
“Calculating the return on investment of perfor- We created the Institute for Cancer Care Excellence in December 2008 to
mance improvement has been missing from most of support this effort. In 2010, with Robert Kaplan, we launched a pilot project,
the quality improvement discussions in health care,” also within the Head and Neck Center, to assess the feasibility of applying
Dr. Thomas Feeley at MD Anderson told us. “When modern cost accounting to health care delivery.
measurement does occur, the assumptions are usu- Traditionally, at MD Anderson, we used a charge-based cost accounting
ally gross, inaccurate, and sometimes overstated,” system. However, we realized that its cost allocations were problematic at
he added. “TDABC gave us a powerful tool to actu- several levels. For a start, the drivers of cost in health care had changed
ally model the effect an improvement will have on but the allocation methodology had not, with the result that our costing no
costs.” Accurate costing allows the impact of process CONTINUED ON NEXT PAGE
September 2011 Harvard Business Review 61
1271 Sep11 Kaplan layout.indd 61 7/27/11 6:08:52 PM
HBR.ORG
improvements to be readily calculated, validated, lead to reduced spending on resources that are no
and compared. longer needed. Managers also have the informa-
The big payoff occurs when providers use accu- tion they need to redeploy resources freed up as a
rate costing to translate the various value-creating result of process improvements. Leaders gain a tool
opportunities into actual spending reductions. A they never had before: a way to link decisions about
cruel fact of life is that total costs will not actually fall patient needs and treatment processes directly to
unless providers issue fewer and smaller paychecks, resource spending.
consume less (and less expensive) space, buy fewer
supplies, and retire or dispose of excess equipment. Reinventing Reimbursement
Facing revenue pressure due to lower reimburse- If we are to stop the escalation of total health care
ments—particularly from government programs costs, the level of reimbursement must be reduced.
such as Medicare and Medicaid—providers today But how this is done will have profound implications
use a hatchet approach to cost reduction by mandat- for the quality and supply of health care. Across-the-
ing arbitrary cuts across departments. That approach board cuts in reimbursement will jeopardize the
jeopardizes both the quality and the supply of care. quality of care and likely lead to severe rationing.
With accurate costing, providers can target their Reductions that enable the quality of care to be main-
cost reductions in areas where real improvements in tained or improved need to be informed by accurate
When providers understand the total costs of treating
patients over their complete cycle of care, they can
contemplate innovative reimbursement approaches without
fear of sacrificing their financial sustainability.
resource utilization and process efficiencies enable knowledge of the total costs required to achieve the
providers to spend less without having to ration care desired outcomes when treating individual patients
or compromise its quality. with a given medical condition.
Health care organizations today, like all other The current system of reimbursement is discon-
firms, conduct arduous and time-consuming budget- nected from actual costs and outcomes and discour-
ing and capacity planning processes, often accompa- ages providers and payors from introducing more
nied by heated arguments, power negotiations, and cost-effective processes for treating patients. With
frustration. Such difficulties are symptomatic of in- today’s inadequate costing systems, reimbursement
adequate costing systems and can be avoided. rates have often been based on historical charges.
A TDABC budgeting process starts by predict- That approach has introduced massive cross subsi-
ing the volume and types of patients the provider dies that reimburse some services generously and
expects. Using these forecasts combined with the pay far below costs for others, leading to excess
process maps for treating each patient condition, supply for well-reimbursed services and inadequate
providers can predict the quantity of resource hours delivery and innovation for poorly reimbursed ones.
required. This can then be divided by the practical Adjusting only the level of reimbursement, how-
capacity of each resource type to obtain accurate es- ever, will not be enough. Any true health care reform
timates of the quantity of each resource needed to will require abandoning the current complex fee-for-
meet the forecasted demand. Estimated monthly service payment schedule altogether. Instead, pay-
expense budgets for future periods can be easily ors should introduce value-based reimbursement,
obtained by multiplying the quantity of each re- such as bundled payments, that covers the full care
source category required by the monthly cost of each cycle and includes care for complications and com-
resource. mon comorbidities. Value-based reimbursement
In this way, managers can make virtually all rewards providers who deliver the best overall care
their costs “variable.” They can readily see how ef- at the lowest cost and who minimize complications
ficiency improvements and process innovations rather than create them. The lack of accurate cost
September 2011 Harvard Business Review 63
1271 Sep11 Kaplan layout.indd 63 7/27/11 6:09:12 PM
THE BIG IDEA HOW TO SOLVE THE COST CRISIS IN HEALTH CARE HBR.ORG
Accurate costing allows the impact of
process improvements to be readily
calculated, validated, and compared.
data covering the full cycle of care for a patient has numbers, they can make bold and politically difficult
been the major barrier to adopting alternative reim- decisions to lower costs while sustaining or improv-
bursement approaches, such as bundled reimburse- ing outcomes. Dr. Jens Deerberg-Wittram, a senior
ment, that are more aligned with value. executive at Schön Klinik, told us, “A good costing
We believe that our proposed improvements in system tells you which areas are worth addressing
cost measurement, coupled with better outcome and gives you confidence to have the difficult discus-
measurement, will give third-party payors the con- sions with medical professionals.” As providers and
fidence to introduce reimbursement methods that payors better understand costs, they will see numer-
better reward value, reduce perverse incentives, and ous opportunities to achieve a true “bending of the
encourage provider innovation. As providers start to cost curve” from within the system, not in response
understand the total costs of treating patients over to top-down mandates. Accurate costing also un-
their complete cycle of care, they will also be able to locks a whole cascade of opportunities, such as pro-
contemplate innovative reimbursement approaches cess improvement, better organization of care, and
without fear of sacrificing their financial sustainabil- new reimbursement approaches that will accelerate
ity. Those that deliver desired health outcomes faster the pace of innovation and value creation. We are
and more efficiently, without unnecessary services, struck by the sheer size of the opportunity to reduce
and with proven, simpler treatment models will not the cost of health care delivery with no sacrifice in
be penalized by lower revenues. outcomes. Accurate measurement of costs and out-
comes is the previously hidden secret for solving the
ACCURATELY MEASURING costs and outcomes is the health care cost crisis. HBR Reprint R1109B
single most powerful lever we have today for trans-
The authors would like to acknowledge the extensive and
forming the economics of health care. As health care invaluable assistance of Mary Witkowski, Dr. Caleb Stowell,
leaders obtain more accurate and appropriate costing and Craig Szela in the preparation of this article.
CARTOON: CHRIS WILDT
“Actually, I don’t know who these people are. They came with the frame.”
64 Harvard Business Review September 2011
1271 Sep11 Kaplan layout.indd 64 7/27/11 6:09:13 PM
You might also like
- Answers To Competency Assessment SectionDocument16 pagesAnswers To Competency Assessment Sectionapi-209542414100% (1)
- Healthcare White PaperDocument4 pagesHealthcare White Paperramakanta_sahu100% (1)
- Harvard Business Review on Fixing Healthcare from Inside & OutFrom EverandHarvard Business Review on Fixing Healthcare from Inside & OutNo ratings yet
- Taurian Curriculum Framework Grade 12 BIODocument8 pagesTaurian Curriculum Framework Grade 12 BIOpummyg100% (1)
- Classroom Readiness ChecklistDocument2 pagesClassroom Readiness ChecklistRoseman Tumaliuan100% (1)
- Nursing Care of A Family With An InfantDocument26 pagesNursing Care of A Family With An InfantJc GarciaNo ratings yet
- Porter y Kapplan (2011)Document18 pagesPorter y Kapplan (2011)ANA MARIA RIOSNo ratings yet
- HPN6Document50 pagesHPN6Joy MichaelNo ratings yet
- Cleveland HelpingDocument33 pagesCleveland HelpingHyma SandraNo ratings yet
- Will Increasing Primary Care Spending Alone Save Money?Document2 pagesWill Increasing Primary Care Spending Alone Save Money?anonNo ratings yet
- What Does The RAND Health Insurance ExperimentDocument3 pagesWhat Does The RAND Health Insurance ExperimentsunnyNo ratings yet
- 5 Quality Measures That Matter For Value-Based CareDocument8 pages5 Quality Measures That Matter For Value-Based CareTuan Nguyen DangNo ratings yet
- Value and Payment in Sleep Medicine JCSM 2018Document4 pagesValue and Payment in Sleep Medicine JCSM 2018cjbae22No ratings yet
- Comprehensive Health Care Reform and Biomedical InnovationDocument21 pagesComprehensive Health Care Reform and Biomedical InnovationcashelNo ratings yet
- Reducing Healthcare Costs: The Physician Perspective OnDocument7 pagesReducing Healthcare Costs: The Physician Perspective OnJeddy Zawadi GeeNo ratings yet
- Defining and Implementing Value-Based Health Care - A Strategic FrameworkDocument4 pagesDefining and Implementing Value-Based Health Care - A Strategic FrameworkQuang Danh PhạmNo ratings yet
- How Would Medicare For All Affect Health System Capacity? Evidence From Medicare For SomeDocument2 pagesHow Would Medicare For All Affect Health System Capacity? Evidence From Medicare For SomeCato InstituteNo ratings yet
- Defensiva - 3Document14 pagesDefensiva - 3Alexandra MateiNo ratings yet
- Better Ways To Pay For Health Care FOCUSDocument8 pagesBetter Ways To Pay For Health Care FOCUSCristhian LarrahondoNo ratings yet
- What Is Value-Based Healthcare - NEJM CatalystDocument3 pagesWhat Is Value-Based Healthcare - NEJM CatalystRémi DANHOUNDONo ratings yet
- An RX For Health Care Woes - CPAs and Firms Can Manage Health Care Costs NowDocument4 pagesAn RX For Health Care Woes - CPAs and Firms Can Manage Health Care Costs NowJill Edmonds, Communications DirectorNo ratings yet
- Reducing Administrative Costs and Improving The Health Care SystemDocument4 pagesReducing Administrative Costs and Improving The Health Care Systemrongse@gmail.comNo ratings yet
- Future Healthcare Value Based Healthcare Is It The Way Forward 002Document5 pagesFuture Healthcare Value Based Healthcare Is It The Way Forward 002amiraNo ratings yet
- 2013 Current Challenges To Academic Health CentersDocument2 pages2013 Current Challenges To Academic Health CentersIkramIzatNo ratings yet
- Ctu Medication ManagementnovoiceDocument12 pagesCtu Medication Managementnovoiceapi-240028260No ratings yet
- Who Is Driving The Interest in OualityDocument10 pagesWho Is Driving The Interest in Oualitymzahid7823No ratings yet
- 40 A National Strategy Pp982 990Document9 pages40 A National Strategy Pp982 990cma909No ratings yet
- Making Health Reform WorkDocument26 pagesMaking Health Reform WorkCenter for American ProgressNo ratings yet
- EpisodeBasedPayment PerspectivesforConsiderationDocument24 pagesEpisodeBasedPayment PerspectivesforConsiderationHazelnutNo ratings yet
- Approaches To Physician Payment The Deconstruction Primary CareDocument6 pagesApproaches To Physician Payment The Deconstruction Primary CarerianberlianproductiveNo ratings yet
- Driving GrowthDocument6 pagesDriving GrowthsolomonNo ratings yet
- Appropriate Use of Reference Pricing CanDocument5 pagesAppropriate Use of Reference Pricing CansunnyNo ratings yet
- Value-Based Insurance Design Landscape DigestDocument35 pagesValue-Based Insurance Design Landscape DigestNational Pharmaceutical CouncilNo ratings yet
- Health Delivery ch2Document20 pagesHealth Delivery ch2JeffersonNo ratings yet
- HealthcareTransformers ValueBasedHealthcareDocument30 pagesHealthcareTransformers ValueBasedHealthcareamiraNo ratings yet
- Controlling Health Care CostsDocument3 pagesControlling Health Care CostsAthanassios VozikisNo ratings yet
- Consumer Driven Health CareDocument9 pagesConsumer Driven Health CareKevin VarnerNo ratings yet
- The Effect of Pay-For-Performance in Hospitals: Lessons For Quality ImprovementDocument9 pagesThe Effect of Pay-For-Performance in Hospitals: Lessons For Quality ImprovementMasrun FatanahNo ratings yet
- Comprehensive Care PhysicianDocument9 pagesComprehensive Care PhysiciannurNo ratings yet
- How Much The Quality of Healthcare Costs? A Challenging Question!Document2 pagesHow Much The Quality of Healthcare Costs? A Challenging Question!Mehak KhannaNo ratings yet
- 305T Paper 4Document8 pages305T Paper 4Emery SteeleNo ratings yet
- BCG Next Generation Medical Management - v3Document14 pagesBCG Next Generation Medical Management - v3Sumit Kumar AwkashNo ratings yet
- "Indumbent" Healthcare Thinking: Prices Don't MatterDocument5 pages"Indumbent" Healthcare Thinking: Prices Don't MatterDavid W. JohnsonNo ratings yet
- Kelompok 3Document9 pagesKelompok 3Yunny FaustineNo ratings yet
- Actuarial Value: A Method For Comparing Health Plan BenefitsDocument12 pagesActuarial Value: A Method For Comparing Health Plan BenefitsParakh AhoojaNo ratings yet
- Cost Accounting in Healthcare PDFDocument8 pagesCost Accounting in Healthcare PDFfilosofal62100% (2)
- How To Make Market Competition Work in Healthcare: Kerianne H. Holman, MD, and Rodney A. Hayward, MDDocument5 pagesHow To Make Market Competition Work in Healthcare: Kerianne H. Holman, MD, and Rodney A. Hayward, MDMichael RandolphNo ratings yet
- Allen - Impacts of Pay For Performance On The Quality of Primary CareDocument9 pagesAllen - Impacts of Pay For Performance On The Quality of Primary Carekevinbgt99No ratings yet
- Home Care Position Paper 4 5 111 PDFDocument20 pagesHome Care Position Paper 4 5 111 PDFRichard HutasoitNo ratings yet
- Nihms 1032116Document12 pagesNihms 1032116TeresaSM19No ratings yet
- BCG Paying For Value in Health Care September 2019 - tcm9 227552Document32 pagesBCG Paying For Value in Health Care September 2019 - tcm9 227552Anand KumarNo ratings yet
- Decision-Making in Healthcare As A Complex Adaptive System: Craig KuziemskyDocument4 pagesDecision-Making in Healthcare As A Complex Adaptive System: Craig KuziemskyChofi SaezNo ratings yet
- Jama 2019 14603Document2 pagesJama 2019 14603Craig WangNo ratings yet
- Thinking Outside The Box Moving The Respiratory Care ProfessionDocument9 pagesThinking Outside The Box Moving The Respiratory Care Professionnicomat85No ratings yet
- KH AHA Benefits of Hospital Mergers Acquisitions 2021 10 08Document20 pagesKH AHA Benefits of Hospital Mergers Acquisitions 2021 10 08Amr AhmedNo ratings yet
- The Beginner's Guide To New Health Care Payment Models - BrookingsDocument7 pagesThe Beginner's Guide To New Health Care Payment Models - BrookingsMaca Vera RiveroNo ratings yet
- Delivery System WhitepaperDocument12 pagesDelivery System Whitepapernchc-scribdNo ratings yet
- Aligning Reimbursement With Value - Institute For Strategy and Competitiveness - Harvard Business SchoolDocument1 pageAligning Reimbursement With Value - Institute For Strategy and Competitiveness - Harvard Business SchoolTuan Nguyen DangNo ratings yet
- Does The Doctor Need A Boss?, Cato Briefing Paper No. 111Document12 pagesDoes The Doctor Need A Boss?, Cato Briefing Paper No. 111Cato InstituteNo ratings yet
- Identifying and Resolving Disputes in New Accountable Care SettingsDocument10 pagesIdentifying and Resolving Disputes in New Accountable Care SettingsRothHealthLawNo ratings yet
- Chapter 5 - Provider Reimbursement MethodsDocument18 pagesChapter 5 - Provider Reimbursement MethodsAdityaNo ratings yet
- Health Affairs Blog Appropriate Use of Reference Pricing Can Increase Value PrintDocument5 pagesHealth Affairs Blog Appropriate Use of Reference Pricing Can Increase Value PrintBrett BernsteinNo ratings yet
- Value Based Pricing 2Document6 pagesValue Based Pricing 2Kavita SubramaniamNo ratings yet
- Textbook of Urgent Care Management: Chapter 22, Health Plan ContractingFrom EverandTextbook of Urgent Care Management: Chapter 22, Health Plan ContractingNo ratings yet
- Daftar Pustaka DiserasiDocument297 pagesDaftar Pustaka Diserasibayu prabuNo ratings yet
- 1 PBDocument8 pages1 PBbayu prabuNo ratings yet
- Dampak Psikologis Tenaga Kesehatan Selama Pandemi COVID-19: Brian Pinggian, Hendri Opod, Lydia DavidDocument8 pagesDampak Psikologis Tenaga Kesehatan Selama Pandemi COVID-19: Brian Pinggian, Hendri Opod, Lydia DavidM. Arif ArrahmanNo ratings yet
- Call For Abstract TF6 T20Document3 pagesCall For Abstract TF6 T20bayu prabuNo ratings yet
- Penentuan Kelayakan Finansial Usaha Produksi Pupuk Abc Pada CV - Xyz Dusun Sebotu Kabupaten SanggauDocument8 pagesPenentuan Kelayakan Finansial Usaha Produksi Pupuk Abc Pada CV - Xyz Dusun Sebotu Kabupaten SanggauArif SetiajayaNo ratings yet
- 3 Ways To Move Like A NinjaDocument4 pages3 Ways To Move Like A NinjaWisnu Wicaksono100% (1)
- PFA Vs PTFE in InstrumentationDocument5 pagesPFA Vs PTFE in InstrumentationArif HakimNo ratings yet
- Government of Canada Gouvernement Du CanadaDocument17 pagesGovernment of Canada Gouvernement Du CanadaSaman BetkariNo ratings yet
- Manual GISDocument36 pagesManual GISDanil Pangestu ChandraNo ratings yet
- Web Aggregator SyllabusDocument5 pagesWeb Aggregator Syllabussam franklinNo ratings yet
- Cubal Cargo Manual Draft 2 November 2011Document384 pagesCubal Cargo Manual Draft 2 November 2011toma cristian100% (2)
- Rubric On Baking CakesDocument3 pagesRubric On Baking CakesshraddhaNo ratings yet
- Notes About BurnsDocument11 pagesNotes About BurnsMichelle Ann GacudNo ratings yet
- Activity 2: College of EngineeringDocument3 pagesActivity 2: College of EngineeringMa.Elizabeth HernandezNo ratings yet
- 3 Composites PDFDocument14 pages3 Composites PDFKavya ulliNo ratings yet
- FT8 - Air System - Maintenance - P&W FT8 - Solar Turbines Technical BLOGDocument3 pagesFT8 - Air System - Maintenance - P&W FT8 - Solar Turbines Technical BLOGLibyanManNo ratings yet
- ms1471pt5-99 - Vocabulary Smoke ControlDocument8 pagesms1471pt5-99 - Vocabulary Smoke ControlBryan Ng Horng HengNo ratings yet
- FCE Writing 14 - ArticleDocument4 pagesFCE Writing 14 - Articlepingu70No ratings yet
- Genomics and Crop ImprovementDocument56 pagesGenomics and Crop Improvementsenguvelan100% (6)
- NANOGUARD - Products and ApplicationsDocument2 pagesNANOGUARD - Products and ApplicationsSunrise VenturesNo ratings yet
- Perdev - Module 9Document9 pagesPerdev - Module 9April Rose CortesNo ratings yet
- Knopp2017 Article OnceACheaterAlwaysACheaterSeriDocument11 pagesKnopp2017 Article OnceACheaterAlwaysACheaterSeriAnda F. CotoarăNo ratings yet
- Gec 014 Prelim ExaminationDocument2 pagesGec 014 Prelim ExaminationcykablyatNo ratings yet
- 13 ECCMinorAmendReqDocument2 pages13 ECCMinorAmendReqal bentulanNo ratings yet
- Assessment in The Affective DomainDocument19 pagesAssessment in The Affective DomainChano MorenoNo ratings yet
- HooksDocument7 pagesHooksapi-233765416No ratings yet
- What Is Aerobic Exercise?Document27 pagesWhat Is Aerobic Exercise?Zedy GullesNo ratings yet
- PU-133AB - 規格GMXa spc 2022Document5 pagesPU-133AB - 規格GMXa spc 2022Ý TrầnNo ratings yet
- Solid Dosage Form Part 1Document48 pagesSolid Dosage Form Part 1Claire Marie AlvaranNo ratings yet
- Pia AlgebraDocument12 pagesPia AlgebraCarvajal EdithNo ratings yet
- 4Dx - Series B Capital Raising IMDocument42 pages4Dx - Series B Capital Raising IMsamNo ratings yet