Professional Documents
Culture Documents
Is Module 8
Uploaded by
gladyskheyagam0 ratings0% found this document useful (0 votes)
1 views26 pagesImmunology and Serology module 8
For medical laboratory science
Original Title
IS-MODULE-8
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentImmunology and Serology module 8
For medical laboratory science
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1 views26 pagesIs Module 8
Uploaded by
gladyskheyagamImmunology and Serology module 8
For medical laboratory science
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 26
› the study of the antigens associated with tumors, the immune
response to tumors, the tumor’s effect on the host’s immune status,
and the use of the immune system to help eradicate the tumor.
› Proto-oncogenes-genes that normally regulate the initiation and
execution of normal cells
› Oncogenes-the mutant forms of proto-oncogenes that contribute to
various tumor types or malignant transformation
› Tumor suppressor genes-removes growth-inhibitory signals that can
cause tumors
Tumors
are composed of cells that possess many of the attributes of the
normal cells from which they arose but have accelerated or
dysregulated growth
BENIGN TUMORS- not immortal and a tumor does not invade
surrounding tissue and normal body function is largely preserved
MALIGNANT TUMOR-immortal, progressively invasive,
CANCEROUS, can invade surrounding tissues and greatly disrupt
normal body function
METASTASIS-moves through the blood or lymph to new
sites, small clumps of cells that break off and spread where
they continue to grow
when the malignant cells travel through the body, causing
new foci of malignancy until body function is so disrupted
that death occurs.
Malignant cells typically differ visually from normal cells, are
metabolically more active to support their growth, and express
different genes or different levels of gene products as compared to
normal cells
arise from the endodermal
or ectodermal ephithelial
tissue
cancers or malignancies that
begin in the epithelial cells,
which are the cells that make
up the skin, and the tissues
that line various internal
organs and structures. Some
of the most common
carcinomas affect the breast,
lung, prostate, and colon.
a malignant tumor, a type of
cancer that arises from
transformed cells of
mesenchymal (connective
tissue) origin. Connective
tissue is a broad term that
includes bone, cartilage, fat,
vascular, or hematopoietic
tissues, and sarcomas can
arise in any of these types of
tissues.
malignant tumors of
hematopoietic cells of the
bone marrow
Leukemia-involves mainly
WBCs
Lymphoma-involves
lymphocytes
The conversion of a normal cell to a malignant cell is
typically a process, not an event.
1. Induction phase
cells are exposed to a variety of environmental insults, including
chemical carcinogens, oncogenic viruses, and radiation (ionizing
and ultraviolet). Cancer may only develop as the result of multiple
mutations caused by these insults, and it more readily develops in
cells genetically predisposed to these mutations.
take months to years, cells exhibit dysplasia or abnormal growth
that is not yet considered neoplasia, or consistent with a tumor.
2. In situ phase of cancer
when neoplastic cells have formed but are confined to the tissue of
origin
3. Invasion phase
cells are malignant and tries to invade normal tissues
4. Dissemination phase
tumor cells travel throughout the body, usually via the blood and
lymphatics
Tumors are also classified by the TNM system by the size of
the primary tumor (T), the involvement of adjacent lymph
nodes (N), and the detection of metastasis (M)
Immunosurveillance by the immune system to eradicate
cancer cells as they form has long been postulated. There
is increased incidence of tumors in those with deficient
immune systems such as the elderly and in
immunosuppressed individuals, but this is not proof of the
existence of immunosurveillance.
Tumor-specific antigens
not found on normal somatic cells (unique to tumor cells) but
result from mutations of genes
represent fragments of novel peptides (small proteins) that are
presented at the cell surface bound to the major histocompatibility
complex class I molecules. In that form they are recognized by T
lymphocytes (T cells) and eliminated.
Tumor-associated antigens (TAA)-antigens present in the
tumor tissue in higher amounts than in normal tissue
Oncofetal antigens
expressed on tumors and on normal fetal cells
Example: alpha - 1 - fetoprotein (AFP) and carcinoembryonic
antigen (CEA)
An ideal tumor marker has the following characteristics:
It must be produced by the tumor or as a result of the tumor and must be
secreted into some biological fluid that can be analyzed easily and
inexpensively for levels.
Its circulating half-life must be long enough to permit its concentration to
rise with increasing tumor load.
It must increase to clinically significant levels (above background control
levels) while the disease is still treatable and with few false negatives
(sufficient sensitivity).
The antigen must be absent from or at background levels in all
individuals without the malignant disease in question to minimize false-
positive test results (sufficient specificity).
can provide important adjunct information to patient histories
and physical exams
tests include stool occult blood and colonoscopy for
colorectal carcinoma, Papanicolaou smear for cervical
cancer, self-exams for breast and testicular cancer, x-ray
mammography for breast cancer, and digital rectal exam for
prostate cancer
three types of laboratory methods for cancer screening and
diagnosis are gross and microscopic morphology of tumors,
detection of antigen/protein tumor markers, and DNA/RNA
molecular diagnostics
the choice of method often depends on convenience, cost,
sensitivity, and specificity
Some of the molecular diagnostic techniques that have
become increasingly routine include the following:
1. Cytogenetic studies:
Many cancers are associated with particular karyotypes. However,
as more precise knowledge of the exact gene defects present in
various cancers is gained, testing for the aberrant genes is
becoming more prevalent.
2. Nucleic acid amplification techniques:
Polymerase chain reaction (PCR) and its variants increase
the inherent level of DNA or RNA, allowing the detection of
small populations of cancer cells (including circulating cells in
metastasis) and the detection of mutations, deletions, and
gene rearrangements/translocations
3. Fluorescent in situ hybridization (FISH)
Nucleic acid probes capable of binding to sequences of
interest are tagged with fluorophors and applied to cells.
Cells containing the sequence of interest can be visualized
with fluorescent microscopes. Similar techniques using
nonfluorescent labels such as enzymes and silver stains are
also becoming available.
Proteomics
new field that employs mass spectrometry (MS) to identify and quantify
an array of proteins simultaneously present in a sample. This has given
birth to a new field called oncopeptidomics (defined as application of
peptidomics technologies to the field of oncology)
Protein profiling in cancer patients will aid in the discovery of new tumor
markers or patterns of protein expression that are consistent with cancer.
Oncopeptidomics may allow more subtle increases of tumor markers to
have diagnostic significance, since multiple markers can be measured
and the overall pattern assessed, but this is currently only at the research
stage
final aspect of tumor immunology
1. Passive immunotherapy-involves transfer of antibody,
cytokines, or cells to patients who may not be able to mount
an immune response.
-many barriers because of possible recipient rejection of foreign cells,
graft-versus host disease (GVHD), and the fragility of live cells.
2. Active immunotherapy- patients are treated in a manner that
stimulates them to mount immune responses to their
tumors.
Ex. Adjuvants such as BCG
You might also like
- Cancer ImmunologyDocument37 pagesCancer ImmunologyBeenish SarfrazNo ratings yet
- 9.lecturer 18 Biochemistry Effect On Tumor and Tumor MarkersDocument19 pages9.lecturer 18 Biochemistry Effect On Tumor and Tumor MarkersAbdulRahman MuthannaNo ratings yet
- Biology Investigatory Project: Study On CancerDocument24 pagesBiology Investigatory Project: Study On CancerAthiya Zainab100% (1)
- Blood Vessels Vasculogenesis Endothelial Mesoderm Embryo: Angiogenesis Is The Physiological Process Through Which NewDocument23 pagesBlood Vessels Vasculogenesis Endothelial Mesoderm Embryo: Angiogenesis Is The Physiological Process Through Which NewDaniel SutantoNo ratings yet
- Name: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of Submission: TopicDocument8 pagesName: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of Submission: TopicAnoosha FarooquiNo ratings yet
- Neoplasia S. M Jawwad AliDocument25 pagesNeoplasia S. M Jawwad AliAnt EverafterNo ratings yet
- An Introduction To Cancer Biology: When Good Cells Go BadDocument68 pagesAn Introduction To Cancer Biology: When Good Cells Go BadSavitaNo ratings yet
- Introduction To OncologyDocument58 pagesIntroduction To OncologyserviceNo ratings yet
- Name: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of Submission: TopicDocument8 pagesName: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of Submission: TopicAnoosha FarooquiNo ratings yet
- Conchem q4 Module 3 Week 5-6Document8 pagesConchem q4 Module 3 Week 5-6Tiffany Moore100% (2)
- Cancer and Malignant GrowthDocument3 pagesCancer and Malignant GrowthTapan Kumar PalNo ratings yet
- Cancer (Medical Term:Malignant NeoplasmDocument7 pagesCancer (Medical Term:Malignant NeoplasmolussojiNo ratings yet
- Cancer CareDocument84 pagesCancer Careakoeljames8543No ratings yet
- Chapter 16-JnuCancer - 複本Document42 pagesChapter 16-JnuCancer - 複本Wai Kwong ChiuNo ratings yet
- Investigatory Project On CANCERDocument15 pagesInvestigatory Project On CANCERSreeja SwainNo ratings yet
- Prepared By: Anna Marie M. Montalban, RN, Us-RnDocument71 pagesPrepared By: Anna Marie M. Montalban, RN, Us-RnPrecai Permangil100% (2)
- Cellular AberrationDocument71 pagesCellular AberrationKris TejereroNo ratings yet
- 13 ChemoDocument40 pages13 ChemoSweet SunNo ratings yet
- Jurnal NeoplasmaDocument10 pagesJurnal NeoplasmaFadhilah Asyifa DewantiNo ratings yet
- Neoplastic DisordersDocument36 pagesNeoplastic DisordersJSeasharkNo ratings yet
- L11, Pathophysiology ManualDocument11 pagesL11, Pathophysiology Manualph.mt.pharmaNo ratings yet
- 3 CancerDocument47 pages3 Cancerkirubel getyeNo ratings yet
- Cc2 - MidtermDocument3 pagesCc2 - MidtermMika SusadaNo ratings yet
- Cancer DevelopmentDocument4 pagesCancer DevelopmenterinNo ratings yet
- Cellular AberrationDocument58 pagesCellular AberrationTauqeer AhmedNo ratings yet
- Unco Ntrolled Proliferation: Distinguishing Property of Malignant Cells. Without Intervention, Cancerous Tissues Grow inDocument7 pagesUnco Ntrolled Proliferation: Distinguishing Property of Malignant Cells. Without Intervention, Cancerous Tissues Grow inYukiNo ratings yet
- G Path-NeoplasiaDocument60 pagesG Path-Neoplasiachouchou124No ratings yet
- Oncology NursingDocument7 pagesOncology NursingDiana Laura Lei100% (1)
- CancerDocument19 pagesCancerparabharshita2709No ratings yet
- Cancer: Large Group of DiseasesDocument141 pagesCancer: Large Group of Diseasesmynoidanh19No ratings yet
- Anti Neoplastic AgentsDocument116 pagesAnti Neoplastic AgentsAbii KetiNo ratings yet
- 4th Lecture (NCM106 CA I) Care of Clients in Cellular Aberrations, ABC, Emergency and Disaster NursingDocument14 pages4th Lecture (NCM106 CA I) Care of Clients in Cellular Aberrations, ABC, Emergency and Disaster NursingKamx Mohammed100% (3)
- Mohammad Altamimi, MD, PHD Jordan UniversityDocument16 pagesMohammad Altamimi, MD, PHD Jordan UniversityDaniel AtiehNo ratings yet
- Mohammad Altamimi, MD, PHD Jordan UniversityDocument16 pagesMohammad Altamimi, MD, PHD Jordan UniversityDaniel AtiehNo ratings yet
- CANCERDocument84 pagesCANCERhydrocodoonieNo ratings yet
- Nursing Care of The Client With CancerDocument15 pagesNursing Care of The Client With CancerAlvin M Alcayno0% (1)
- Topics: Nasopharyngeal CarcinomaDocument21 pagesTopics: Nasopharyngeal CarcinomaShruthi Y nursingNo ratings yet
- Lewis: Medical-Surgical Nursing, 9 Edition: CancerDocument8 pagesLewis: Medical-Surgical Nursing, 9 Edition: CancerPrincess AgarwalNo ratings yet
- Thursday, 3 November 2022 10:14 PMDocument5 pagesThursday, 3 November 2022 10:14 PMAdiel CalsaNo ratings yet
- Cancer" Is The Latin Word For Crab.: Normal Mechanism of Body GrowthDocument9 pagesCancer" Is The Latin Word For Crab.: Normal Mechanism of Body Growthanupriya mittalhy6No ratings yet
- Immuno TherapyDocument20 pagesImmuno TherapyAttis PhrygiaNo ratings yet
- Tumour Immunology: Von Ryan F. Lingcallo, RMTDocument20 pagesTumour Immunology: Von Ryan F. Lingcallo, RMTJuan SalenNo ratings yet
- Neoplasia Summer 2020Document38 pagesNeoplasia Summer 2020Sharif HossainNo ratings yet
- Neoplasia Stom Eng 2011Document58 pagesNeoplasia Stom Eng 2011Artem GrigoryanNo ratings yet
- Oncologic Nursing: Oncology: OverviewDocument156 pagesOncologic Nursing: Oncology: OverviewNathalie KerrNo ratings yet
- MR 28 Agustus-1Document7 pagesMR 28 Agustus-1BramaNo ratings yet
- Invasion of ECM Degradation of ECMDocument8 pagesInvasion of ECM Degradation of ECMJezreel NicolasNo ratings yet
- Ursing Care of Client With CancerDocument51 pagesUrsing Care of Client With CancerJimmelyn PalosNo ratings yet
- Oncology: Ivano-Frankivsk National Medical University Department of OncologyDocument41 pagesOncology: Ivano-Frankivsk National Medical University Department of OncologyAli Baker AlgelaneNo ratings yet
- Module 3.1. Intro To Cellular Aberration and PathophysiologyDocument15 pagesModule 3.1. Intro To Cellular Aberration and PathophysiologyShiena Mae PelagioNo ratings yet
- FranciscoDocument4 pagesFranciscoFrances FranciscoNo ratings yet
- Management of Patient With CancerDocument47 pagesManagement of Patient With Canceruuuhbnb lplhghNo ratings yet
- Cancer OverviewDocument13 pagesCancer OverviewDevansh MoyalNo ratings yet
- JSCR 18 013Document7 pagesJSCR 18 013Mary ChikamaraNo ratings yet
- Tumor Immunology: ObjectivesDocument20 pagesTumor Immunology: ObjectivesMarl EstradaNo ratings yet
- CancerBooklest FinalDocument15 pagesCancerBooklest Finalrafael alvarizNo ratings yet
- NE0PLASIADocument28 pagesNE0PLASIADaniel SutantoNo ratings yet
- Cancer ResearchDocument5 pagesCancer ResearchmelanieNo ratings yet
- Tumor Immunology: M. Nagarkatti Teaching ObjectivesDocument4 pagesTumor Immunology: M. Nagarkatti Teaching Objectives99manu99No ratings yet
- Forefoot Myopericytoma: A Case Reportand Review of The LiteratureDocument4 pagesForefoot Myopericytoma: A Case Reportand Review of The LiteratureIJAR JOURNALNo ratings yet
- Koagulasi Intravaskuler Diseminata Pada Kanker: January 2015Document13 pagesKoagulasi Intravaskuler Diseminata Pada Kanker: January 2015Zinnan Al-FaqihNo ratings yet
- Cancer Cell and Cell CycleDocument10 pagesCancer Cell and Cell CycleRouie AzucenaNo ratings yet
- Radiation Dose and Image Quality BT DBT and FFDMDocument6 pagesRadiation Dose and Image Quality BT DBT and FFDMRenadNo ratings yet
- 1 Introduction To Economic EvaluationDocument31 pages1 Introduction To Economic EvaluationSwayam MohapatraNo ratings yet
- Diet and CancerDocument7 pagesDiet and CanceraibutyNo ratings yet
- BreastQ-bank Full - 2Document44 pagesBreastQ-bank Full - 2Helene AlawamiNo ratings yet
- Female Genital Tract Cytopathology: PracticalDocument26 pagesFemale Genital Tract Cytopathology: PracticalNgotelo FunwiNo ratings yet
- CT Simulation MethodologyDocument41 pagesCT Simulation MethodologyRohla habibiNo ratings yet
- Bernhardt 2020Document6 pagesBernhardt 2020ghanaNo ratings yet
- Lymph Nodes Normal and MalignantDocument12 pagesLymph Nodes Normal and MalignantMagzNo ratings yet
- Face Tanner: HB179, HB175, HB172Document76 pagesFace Tanner: HB179, HB175, HB172gheorghe_georgelNo ratings yet
- Asian Hps ReportDocument145 pagesAsian Hps ReportUMRATUN HAYATINo ratings yet
- Carcinoma of Prostate: Patho Ogy - Chapter &Document29 pagesCarcinoma of Prostate: Patho Ogy - Chapter &HAMIDNo ratings yet
- Cell Line Profile MDA-MB-231 (ECACC Catalogue No.)Document3 pagesCell Line Profile MDA-MB-231 (ECACC Catalogue No.)Manikanta Sai KumarNo ratings yet
- Communique of The 5TH National Conference On Environment and HealthDocument8 pagesCommunique of The 5TH National Conference On Environment and HealthJoshuaNo ratings yet
- Summary of BASICS OF DIFFUSION MRI PDFDocument13 pagesSummary of BASICS OF DIFFUSION MRI PDFParamitha AdriyatiNo ratings yet
- DIANDRA PARIKESIT Thrombus-Like - Tumor - of - Renal - Cell - Carcinoma - MimickDocument4 pagesDIANDRA PARIKESIT Thrombus-Like - Tumor - of - Renal - Cell - Carcinoma - MimickYulia DjatiwardaniNo ratings yet
- 02 Breast PDFDocument15 pages02 Breast PDFANAS ALINo ratings yet
- Standardization of The Definition and Surgical.9Document11 pagesStandardization of The Definition and Surgical.9JobelleNo ratings yet
- Instructor's Presentation-Tumor MarkersDocument57 pagesInstructor's Presentation-Tumor MarkersMACOB, ETHELHYN JHANENo ratings yet
- Family Support and Self-Esteem of Patient With Breast CancerDocument5 pagesFamily Support and Self-Esteem of Patient With Breast CancerDean Rex Azriel TelaumbanuaNo ratings yet
- ProstateDocument204 pagesProstatevonicaNo ratings yet
- 17, Feb, FDocument13 pages17, Feb, FMohsin AliNo ratings yet
- Elsevier HPV 16-18Document8 pagesElsevier HPV 16-18Kevin SNo ratings yet
- Malignant Proliferating Trichilemmal Tumor One Case and Literature ReviewDocument4 pagesMalignant Proliferating Trichilemmal Tumor One Case and Literature ReviewIJAR JOURNALNo ratings yet
- Liposarcoma Cyto PDFDocument10 pagesLiposarcoma Cyto PDFHerdyastuti NurwestriNo ratings yet
- Comparing Breast-Conserving Surgery With Radical MastectomyDocument6 pagesComparing Breast-Conserving Surgery With Radical MastectomyRonald Cariaco FlamesNo ratings yet
- Melanoma 2016Document413 pagesMelanoma 2016Anca-Raluca Pascu100% (2)
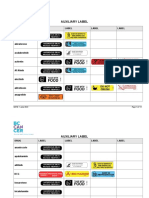
- Auxiliary Label LISTDocument14 pagesAuxiliary Label LISTAbdur RachmanNo ratings yet