Professional Documents
Culture Documents
33 Jan2013 006 240425 090126
Uploaded by
drsjkianiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
33 Jan2013 006 240425 090126
Uploaded by
drsjkianiCopyright:
Available Formats
J. Kiani, A. Moghimbeigi, H. Azizkhani, et al.
Original Article
The Prevalence and Associated Risk Factors of Peripheral Diabet-
ic Neuropathy in Hamedan, Iran
Javad Kiani MD•1, Abbas Moghimbeigi PhD2, Homeyra Azizkhani MD3, Soghra Kosarifard4
Abstract
Background: Diabetic neuropathy is one of the most common complications of diabetes mellitus, of which it’s most prevalent form is
chronic sensorimotor neuropathy. The aim of this study is to assess the prevalence of diabetic peripheral neuropathy (DPN) and its associ-
ated risk factors among diabetic patients who reside in Hamedan, Iran.
Methods: A cross-sectional study of 600 types 1 and 2 diabetic patients was performed using the standard Neuropathy Symptom Score
(NSS) and Neuropathy Disability Score (NDS) criteria for the diagnosis of diabetic neuropathy.
Results: Overall prevalence of DPN in this population was 45.7% (95% CI: 42.6%-48.8%). The prevalence of DPN in type 1 diabetic
patients was 21.5%, whereas in type 2 diabetic patients it was 49.3% (P<0.001). Duration of diabetes and education level were signi¿cantly
associated with DPN in type 1 diabetic patients and a history of foot ulcer, age, duration of diabetes, weight, education level, and sex had a
signi¿cant association with DPN in type 2 diabetic patients according to multiple logistic regression analysis.
Conclusion: The results of our study showed a relatively high prevalence of DPN in our diabetic population. A signi¿cant difference ex-
isted in the prevalence of DPN between types 1 and 2 diabetic patients.
Keywords: Diabetes, neuropathy, prevalence, risk factors
Cite this article as: Kiani J, Moghimbeigi A, Azizkhani H, Kosarifard S. The prevalence and associated risk factors of peripheral diabetic neuropathy in Hamedan,
Iran. Arch Iran Med. 2013; 16(1): 17 – 19.
Introduction Patients and Methods
iabetic neuropathy is one of the most common complica- This cross-sectional study was conducted at the Diabetes Center
D tions of diabetes mellitus, and its morbidity and mortality
is a large part of the cost of diabetes care.1 The most com-
of Hamedan, Western Iran. Convenience sampling was used to
enroll patients. Patients who matched the ADA criteria10 for dia-
mon form of diabetic neuropathy is chronic sensorimotor neu- betes (types 1 and 2) were asked to participate in this project by
ropathy. Several mechanisms are involved in pathogenesis of dia- invitation. We recruited 600 patients from April 18 to Septem-
betic neuropathy, such as hyperglycemia, the polyol pathway, ber 4, 2011. After obtaining written informed consent, a ques-
glycation, and oxidative stress, among others.2 tionnaire that included general information, height and weight,
Earlier studies have reported a worldwide prevalence of 22.7% smoking status, duration of diabetes, type of medication, history
to 54% for diabetic peripheral neuropathy (DPN).3 Estimates of of foot ulcer, and laser photocoagulation was completed. Then
the prevalence of diabetic neuropathy vary to a large extent, due height, weight and blood pressure were recorded. Patients were
to the differences in the type of patients, the neurological effects considered hypertensive if on medication or if they had a systolic
of ageing and diagnostic methods and criteria.4–6 blood pressure 140 mmHg and/or diastolic blood pressure 80
A few studies have evaluated the prevalence of DPN in different mmHg. An endocrinologist examined the patients for the pres-
regions of Iran, with a reported prevalence from 32% to 75.1%.7–9 ence of DPN. We used the standard Neuropathy Symptom Score
The aim of this study was to estimate the prevalence of DPN (NSS) and Neuropathy Disability Score (NDS) criteria for the di-
and its associated risk factors in a population of diabetic patients agnosis of diabetic neuropathy.11,12 First, the NSS questionnaire
in Hamedan, a province in Western Iran. that included questions regarding the type of sensation, location
and time of symptoms, waking up from sleep, and factors that
relieved symptoms were asked and recorded. Then, the NDS data
sheet was completed. This data sheet contained neurologic ex-
Authors’ Af¿liations: 1Department of Endocrinology, Department of Inter-
nal Medicine, Faculty of Medicine, Hamedan University of Medical Sciences, amination parameters such as the ankle reÀex and perceptions of
Hamedan, Iran, 2Department of Biostatistics and Epidemiology, School of Public pinprick, cold, and vibration. A score of 0 to 2 was assigned for
Health and Center of Health Research, Hamedan University of Medical Sci- each parameter. Total NSS and NDS scores were the sum of these
ences, Hamedan, Iran, 3Faculty of Medicine, Hamedan University of Medical
Sciences, Hamedan, Iran, 4Hamedan Diabetes Center, Hamedan University of scores. The criteria for diagnosis of DPN was an NDS score of
Medical Sciences, Hamedan, Iran. at least 6, irrespective of NSS score, or an NDS score of 3 – 5 in
•Corresponding author and reprints: Javad Kiani MD, Department of En- combination with an NSS score of at least 5.5 We used the t-test
docrinology, Department of Internal Medicine, College of Medical Sciences,
Hamedan University of Medical Sciences, Hamedan, Iran. Tel: +98 811 838 for data analysis to compare quantitative variables; and qualita-
0155, Fax: +98 811 838 1035, E-mail: javadkiani@umsha.ac.ir. tive variables were compared with the chi-square or Fisher’s
Accepted for publication: 11 July 2012 exact tests. P-values less than 0.05 were considered statistically
Archives of Iranian Medicine, Volume 16, Number 1, January 2013 17
The prevalence and associated risk factors of peripheral diabetic neuropathy
signi¿cant. Because of the numerous risk factors involved in the DPN, who were 48.16 ± 14.6 years old (P < 0.001). Those with
occurrence of DPN, we have used multiple logistic regression DPN had a longer duration of diabetes (11.4 ± 8 years) compared
models to identify those risk factors associated with DPN. In the with those without DPN (7.3 ± 6.3 years; P < 0.001).
backward method, we used the Wald test to evaluate the signi¿- Multiple logistic regression analysis was used to evaluate the
cance of the variables. The Wald test is equal to beta divided by correlation between DPN and multiple factors such as age, sex,
the standard error of beta, where the obtained value (± 1.96) is not weight, height, hypertension, systolic and diastolic blood pres-
statistically signi¿cant. The exit and entrance of the variables into sure, smoking, duration of diabetes, type of diabetes, type of med-
the model were at the level of Į = 0.05. All statistical analyses ication (insulin or oral agent), history of foot ulcer and education
were performed using SPSS for Windows. level separately for type 1 and type 2 diabetes. Factors that have
a signi¿cant association are shown in Table 2. In this model, the
Results duration of diabetes and education level were signi¿cantly associ-
ated with DPN in type 1 diabetic patients and history of foot ulcer,
General characteristics of the study population are shown in age, duration of diabetes, weight, education level and sex had a
Table 1. A total of 600 diabetic patients (79 type 1 and 521 type signi¿cant association with DPN in type 2 diabetic patients.
2) were included in this study. The mean age of the patients was
53.26 ± 14.46 years and the mean duration of diabetes was 9.26 Discussion
± 7.44 years. Overall prevalence of DPN was 45.7% (95% CI:
42.6% – 48.8%). Prevalence of DPN in type 1 diabetic patients was In general, the prevalence of DPN in our studied population was
21.5% and the prevalence in type 2 diabetic patients was 49.3% 45.7% and history of foot ulcer, age, duration of diabetes, weight,
(P < 0.001). We observed that the prevalence of DPN was higher diastolic blood pressure, education level and sex were associated
among men (51.5%) than women (42.8%; P = 0.045). In terms of with DPN. Previous studies of the prevalence of neuropathy in
diabetes duration, there was no signi¿cant difference between men diabetic patients have reported different results. In one Portuguese
(9.5 ± 7.1 years) and women (9.1 ± 7.5 years; P = 0.569). study, the prevalence of clinical DPN was reported to be 32.2%,
Of the patients with DPN, 36.9% were male whereas 29.1% of however DPN was de¿ned as the presence of altered sensitivities
the patients without DPN were male (P = 0.045). Patients with and reÀexes, regardless of symptoms.13 In two studies conducted
DPN were 59.3 ± 11.6 years old compared to patients without in Spain, Cabezas-Cerrato and colleagues6 reported a prevalence
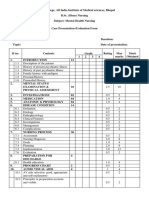
Table 1. Baseline characteristics of the study population and prevalence of diabetic peripheral neuropathy (DPN) in types 1 and 2 diabetic patients.
Type 1 Type 2 P-value
Number (%) 79 (13.1) 521 (86.8) <0.001
Age (years) 28.2±10.6 57.0±10.6 <0.001
Duration (years) 9.5±7.2 9.2±7.4 0.703
Education level (%) <0.001
Illiterate 4 (5) 185 (35.5)
Elementary 12 (15.1) 118 (22.6)
< High school 46 (58.2) 176 (33.7)
High school 17 (21.5) 42 (8)
Height (cm) 164.0±9.8 158.8±8.5 < 0.001
Weight (kg) 64.0±12.4 71.5±11.9 < 0.001
BMI (kg/cm2) 23.7±4.3 28.3±4.3 < 0.001
Systolic blood pressure (mmHg) 110.8±15.2 125.6±19.6 <0.001
Diastolic blood pressure (mmHg) 62.8±8.6 70.7±11.8 <0.001
Hx of hypertension (%) <0.001
No 75 (94.9) 285 (54.7)
Yes 4 (5.1) 236 (45.3)
Smoking (%) 0.148
No 71 (89.9) 490 (94.1)
Yes 8 (10.1) 31 (5.9)
Medications (%) <0.001
Oral agent 4 (5.1) 313 (60.1)
Insulin 72 (91.1) 119 (22.8)
Oral agent + insulin 3 (3.8) 89 (17.1)
Hx of foot ulcer (%) 0.821
No 70 (88.6) 457 (87.7)
Yes 9 (11.3) 64 (12.2)
Hx of laser photocoagulation (%) 0.004
No 77 (97.4) 448 (85.9)
Yes 2 (2.5) 73 (14)
DPN (%) <0.001
No 62 (78.5) 264 (50.7)
Yes 17 (21.5) 257 (49.3)
hx: History, DPN: Diabetic peripheral neuropathy
18 Archives of Iranian Medicine, Volume 16, Number 1, January 2013
J. Kiani, A. Moghimbeigi, H. Azizkhani, et al.
Table 2. Multiple logistic regression analysis of associated risk factors with diabetic peripheral neuropathy (DPN) in types 1 and 2 diabetes.
Type 1 diabetes
Variable Wald P-value Adj. OR (95% CI)*
Duration 5.85 0.016 1.16 (1.03–1.32)
Education level 9.43 0.002 0.17 (0.05–0.53)
Type 2 diabetes
Variable Wald P-value Adj. OR (95% CI)*
Hx of foot ulcer 8.76 0.003 2.73 (1.40–5.31)
Age 28.60 <0.001 1.06 (1.03–1.08)
Duration 13.81 <0.001 1.05 (1.02–1.08)
Weight 4.06 0.044 1.01 (1.00–1.03)
Education level 9.53 0.002 0.72 (0.58–0.88)
Sex 7.63 0.006 0.51 (0.32–0.82)
hx: History, Adj. OR (95% CI) *: Adjusted odds ratio (95% CI)
of 22.7% and Garcia and colleagues3 reported a prevalence of References
39.6% for diabetic polyneuropathy. Also, another study in Can-
ada reported a prevalence of 15% for neuropathy in established 1. Vinik AI, Mitchell BD, Leichter SB, Wagner AL, Brian JT, Georges
diabetic patients.14 However, these studies all used different diag- LP. Epidemiology of the complications of Diabetes. In: Leslie RDG,
Robbins DC (eds) Diabetes: Clinical science in Practice. Cambridge
nostic methods to diagnose neuropathy. Some studies have evalu- University Press, Cambridge. 1195; 221 – 287.
ated the prevalence of diabetic neuropathy in Iran. According to 2. Boulton Ajm, Malik Ra, Arezz Jc, Sosenko JM. Diabetic somatic neu-
a study in Tehran, the prevalence of DPN was reported at 31.9% ropatheis. Diabetes Care. 2004; 27: 1458 – 1486.
amongst 124 diabetic patients as determined by the Michigan cri- 3. Garcia JM, Velasco PP, Cabrerizo L, Pe´rez M, Go´mez VL. Preva-
lence of distal diabetic polyneuropathy using quantitative sensory
teria.7 A study in Isfahan on 810 diabetic patients reported a DPN methods in a population with diabetes of more than 10 years’ disease
prevalence of 75.1%, as diagnosed by symptoms, signs and nerve duration. Endocrinol Nutr. 2010; 57(9): 414 – 420.
conduction velocity studies.9 Another study in Yazd Province, 4. Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A
Iran reported a prevalence of 51.7% for diabetic sensory neuropa- multicentre study of the prevalence of diabetic peripheral neuropa-
thy in the United Kingdom hospital clinic population. Diabetologia.
thy in 2350 patients by considering physical signs for diagnosis.8 1993; 36: 1 – 5.
Various factors are associated with neuropathy such as age, male 5. Dyck PJ, Kratz KM, Karnes JL, Litchy WJ, Klein R, Pach JM, et al.
sex, duration of diabetes and glycemic control. In the present The prevalence by staged severity of various types of diabetic neu-
study, neuropathy was associated with duration of diabetes in type ropathy, retinopathy, and nephropathy in a population-based cohort:
The Rochester Diabetic Neuropathy Study. Neurology. 1993; 43: 817
1 diabetics. In type 2 diabetic patients, neuropathy was associated – 824.
with history of foot ulcer, age, duration of diabetes, weight and 6. Cabezas-Cerrato J; for the Neuropathy Spanish Study Group of the
sex. Neuropathy was inversely associated with patient’s education Spanish Diabetes Society (SDS): The prevalence of clinical diabetic
polyneuropathy in Spain: a study in primary care and hospital clinic
level in both types 1 and 2 diabetes. The association of neuropa-
groups. Diabetologia. 1998; 41: 1263 – 1269.
thy with duration of diabetes and age noted in the current study 7. Tabatabaei O, Mohajeri MR, Madani SP, Heshmat R, Larijani B. The
were similar to other studies. We observed no association between prevalence of diabetic peripheral neuropathy and related factors. Ira-
neuropathy and height or BMI, which supported results of some nian J Publ Health. 2011; 40(3): 55 – 62.
8. Rahimdel A, Afkhami M, Souzani A, Modaresi M, Mashahiri MR.
studies,10 however contrasted other studies’ ¿ndings.15 Our study Prevalence of sensory neuropathy in type 2 diabetic patients in Iranian
did not show any correlation between smoking and neuropathy, population (Yazd province). Iranian Journal of Diabetes and Obesity.
unlike some previous studies.14 2009; 1(1): 30 – 35.
The current study had some limitations. First, it was possible 9. Janghorbani M, Rezvanian H, Kachooei A, Ghorbani A, Chitsaz A,
Izadi F, Amini M. Peripheral neuropathy in type 2 diabetes mellitus in
that our patients were not representative of all diabetic patients Isfahan, Iran: prevalence and risk factors. Int J Diabetes & Metabo-
since this study was performed in one center. A multicenteric lism. 2006; 14: 126 – 133.
study could better estimate the true prevalence of DPN. Patients’ 10. American Diabetes Association. Standards of medical care in diabe-
glycemic control was not clear; it might have been better to de- tes-2010. Diabetes Care. 2010; 29: 11 – 61.
11. Dyck PJ, Litchy WJ, Lehman KA, Hokanson JL, Low PA, O’Brien
termine HA1C levels of the patients. Finally, we did not evaluate PC. Variables inÀuencing neuropathic endpoints: The Rochester Dia-
other causes of neuropathy. betic Neuropathy Study of Healthy Subjects. Neurology. 1995; 45:
The results of our study showed a relatively high prevalence 1115 – 1121.
(45.7%) of DPN that was associated with a history of foot ulcer, 12. Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH.
A multicentre study of the prevalence of diabetic peripheral neu-
age, duration of diabetes, weight, diastolic blood pressure, educa- ropathy in the United Kingdom hospital clinic population. Diabeto-
tion level and sex. logia. 1993; 36: 1 – 5.
13. Barbosa AP, Medina JL, Ramos EP, Barros HP, and the DPN in Porto
study group. Prevalence and risk factors of clinical diabetic polyneu-
Acknowledgment ropathy in a Portuguese primary health care population. Diabetes
Metab. 2001; 27: 496 – 502.
This study was supported by Hamedan University of Medical 14. Bruce SG, Young TK. Prevalence and risk factors for neuropathy in
Sciences. The authors are indebted to the patients that partici- a Canadian ¿rst nation community. Diabetes Care. 2008; 31: 1837 –
1841.
pated in this project. We gratefully acknowledge Dr. Atefeh Ta- 15. Mold JW, Vesely SK, Keyl BA, Schenk JB, Roberts M. The preva-
vana and Akram Bathaie, staff of the Hamedan Diabetes Center lence, predictors, and consequences of peripheral sensory neuropathy
for data collection, Elaheh Talebi for data entry, and Jalal Kiani, in older patients. J Am Board Fam Pract. 2004; 17: 309 – 318.
PhD for editing the article.
Archives of Iranian Medicine, Volume 16, Number 1, January 2013 19
You might also like
- First Motion For Declaratory JudgmentDocument15 pagesFirst Motion For Declaratory JudgmentRobert Davidson, M.D., Ph.D.100% (2)
- Heartasia 2016 010847Document7 pagesHeartasia 2016 010847Neneng HumairohNo ratings yet
- Ultimate Guide To Content Marketing PDFDocument25 pagesUltimate Guide To Content Marketing PDFMd.Muzibur RahmanNo ratings yet
- Metrology - Book - Hari PDFDocument212 pagesMetrology - Book - Hari PDFKallol ChakrabortyNo ratings yet
- Rotating Machinery 3d TutorialDocument14 pagesRotating Machinery 3d Tutorialأسامةبوعزيز100% (1)
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- MPS and Item AnalysisDocument177 pagesMPS and Item AnalysisMary Ann Palima80% (5)
- Cancer HandbookDocument15 pagesCancer Handbookdaddytrill777No ratings yet
- Labyrinth Weir DesignDocument15 pagesLabyrinth Weir Designchutton681No ratings yet
- Prevalence and Major Risk Factors of Diabetic Retinopathy: A Cross-Sectional Study in EcuadorDocument5 pagesPrevalence and Major Risk Factors of Diabetic Retinopathy: A Cross-Sectional Study in EcuadorJorge Andres Talledo DelgadoNo ratings yet
- Frequency of Peripheral Neuropathy Among Patients of Type 2 Diabetes Mellitus by Using The Michigan Neuropathy Screening InstrumentDocument5 pagesFrequency of Peripheral Neuropathy Among Patients of Type 2 Diabetes Mellitus by Using The Michigan Neuropathy Screening InstrumentMedERA JCMHLMCNo ratings yet
- Prevalence and Its Associated Determinants of Diabetic Peripheral Neuropathy (DPN) in Individuals Having Type-2 Diabetes Mellitus in Rural South India _[PAUTHORS], Indian Journal of Community Medicine (IJCM)Document3 pagesPrevalence and Its Associated Determinants of Diabetic Peripheral Neuropathy (DPN) in Individuals Having Type-2 Diabetes Mellitus in Rural South India _[PAUTHORS], Indian Journal of Community Medicine (IJCM)Michael SelvarajNo ratings yet
- 1 s2.0 S1658361211701731 Main PDFDocument11 pages1 s2.0 S1658361211701731 Main PDFMakmur SejatiNo ratings yet
- Migraine and Type 2 Diabetes Is There Any Association - Art-3A10.1186-2Fs40200-016-0241-yDocument7 pagesMigraine and Type 2 Diabetes Is There Any Association - Art-3A10.1186-2Fs40200-016-0241-ySlamet PamujiNo ratings yet
- Effect of Variability of Hemoglobin Value On Type and Severity of Diabetic Retinopathy in Adult Type II Diabetes Mellitus PatientsDocument11 pagesEffect of Variability of Hemoglobin Value On Type and Severity of Diabetic Retinopathy in Adult Type II Diabetes Mellitus PatientsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Diabetic Foot Risk Factors in Type 2 Diabetes Patients: A Cross-Sectional Case Control StudyDocument5 pagesDiabetic Foot Risk Factors in Type 2 Diabetes Patients: A Cross-Sectional Case Control Studychintya claraNo ratings yet
- E2 Journal of Hypertension Vol 35, E-Supplement 3, November 2017Document1 pageE2 Journal of Hypertension Vol 35, E-Supplement 3, November 2017Sadam_fasterNo ratings yet
- DM 2Document3 pagesDM 2Clararida RiawanNo ratings yet
- Observations: Relationship Between Periodontal Disease and Diabetic RetinopathyDocument24 pagesObservations: Relationship Between Periodontal Disease and Diabetic RetinopathyPaulo AuadNo ratings yet
- Reconfirmation of Newly Discovered Risk Factors of Diabetic Peripheral Neuropathy in Patients With Type 2 Diabetes: A Case-Control StudyDocument10 pagesReconfirmation of Newly Discovered Risk Factors of Diabetic Peripheral Neuropathy in Patients With Type 2 Diabetes: A Case-Control Studychrisna dewiNo ratings yet
- Egyptian Pediatric Association Gazette: M.H. Elsamahy, Y.I. Elhenawy, N. AltayebDocument5 pagesEgyptian Pediatric Association Gazette: M.H. Elsamahy, Y.I. Elhenawy, N. Altayebida ayu agung WijayantiNo ratings yet
- Development and Validation of A Risk Prediction Model For End-Stage Renal Disease in Patients With Type 2 DiabetesDocument13 pagesDevelopment and Validation of A Risk Prediction Model For End-Stage Renal Disease in Patients With Type 2 DiabetesMarta CarolNo ratings yet
- Editorial: Complications of Diabetes 2017Document5 pagesEditorial: Complications of Diabetes 2017landoo oooNo ratings yet
- Komplikasi DiabetesDocument4 pagesKomplikasi DiabetesFrans SaputraNo ratings yet
- Presentation 3Document14 pagesPresentation 3api-285634882No ratings yet
- Do Not Copy: Dementia Is Associated With Chronic Rhinosinusitis: A Population-Based Case-Controlled StudyDocument5 pagesDo Not Copy: Dementia Is Associated With Chronic Rhinosinusitis: A Population-Based Case-Controlled StudyDominique MendozaNo ratings yet
- Journal of Clinical & Translational Endocrinology: Original ResearchDocument11 pagesJournal of Clinical & Translational Endocrinology: Original ResearchAmparito SanchezNo ratings yet
- Копия Towards prevention of diabetic peripheral neuropathy clinical presentation, pathogenesis, and new treatmentsDocument15 pagesКопия Towards prevention of diabetic peripheral neuropathy clinical presentation, pathogenesis, and new treatmentsn01zelolNo ratings yet
- Journal Pone 0171987Document9 pagesJournal Pone 0171987Maulida HalimahNo ratings yet
- Kepustakaan 2.1Document5 pagesKepustakaan 2.1Ikhsan FebriansyahNo ratings yet
- Analysis of Balance Dysfuntion and Fall PDFDocument6 pagesAnalysis of Balance Dysfuntion and Fall PDFJulenda CintarinovaNo ratings yet
- Association of Proteinuria and Incident Atrial Fibrillation in Patients With Diabetes Mellitus: A Population Based Senior Cohort StudyDocument10 pagesAssociation of Proteinuria and Incident Atrial Fibrillation in Patients With Diabetes Mellitus: A Population Based Senior Cohort StudydrkhengkiNo ratings yet
- Original Research PaperDocument4 pagesOriginal Research PaperFernando SilalahiNo ratings yet
- Nursing Diagnosis Risk For Unstable Blood Glucose Level in Patients With Diabetes MellitusDocument6 pagesNursing Diagnosis Risk For Unstable Blood Glucose Level in Patients With Diabetes MellitusJulio ArgañarazNo ratings yet
- Review Article: Aristidis Veves, MD, Miroslav Backonja, MD, and Rayaz A. Malik, MB, PHDDocument15 pagesReview Article: Aristidis Veves, MD, Miroslav Backonja, MD, and Rayaz A. Malik, MB, PHDsrinivasNo ratings yet
- Anemia and The Risk of ProgressionDocument8 pagesAnemia and The Risk of ProgressionArriza MaulanaNo ratings yet
- ID None PDFDocument16 pagesID None PDFrioNo ratings yet
- Dibetes Risk Score - Findrisc - Jaana Lindstrom - ArticleDocument7 pagesDibetes Risk Score - Findrisc - Jaana Lindstrom - ArticleShayekh M ArifNo ratings yet
- Diabetic Neuropathy in ChildrenDocument14 pagesDiabetic Neuropathy in Childrensucca07No ratings yet
- Prevalence of Peripheral Diabetic Neuropathy and Its Association With Patients Related FactorsDocument3 pagesPrevalence of Peripheral Diabetic Neuropathy and Its Association With Patients Related FactorsNawish SohailNo ratings yet
- Retinopathy DiabeticDocument5 pagesRetinopathy DiabeticMagnaNo ratings yet
- Depresi CKD 2Document4 pagesDepresi CKD 2sufaNo ratings yet
- Prospective Cohort Study of Type 2 Diabetes and The Risk of Parkinson's DiseaseDocument3 pagesProspective Cohort Study of Type 2 Diabetes and The Risk of Parkinson's DiseasesastiraNo ratings yet
- 887 4212 1 PBDocument6 pages887 4212 1 PBMaxine TaeyeonNo ratings yet
- IMJM Vol 16 p053 066Document14 pagesIMJM Vol 16 p053 066rosmyNo ratings yet
- 3358 2 Full PDFDocument15 pages3358 2 Full PDFFira KhasanahNo ratings yet
- Undiangnose DMDocument8 pagesUndiangnose DMTri YuliasihNo ratings yet
- Schizophrenia Research: ArticleinfoDocument5 pagesSchizophrenia Research: ArticleinfojhuNo ratings yet
- Righi (2016)Document6 pagesRighi (2016)PelagyalNo ratings yet
- Diabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDocument12 pagesDiabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDwitari Novalia HaraziNo ratings yet
- The Emergence of Non-Communicable Disease in Indonesia: Dyah PurnamasariDocument2 pagesThe Emergence of Non-Communicable Disease in Indonesia: Dyah Purnamasarinene_luciaNo ratings yet
- Predictors For Diabetic Retinopathy in Normoalbuminuric People With Type 2 Diabetes MellitusDocument6 pagesPredictors For Diabetic Retinopathy in Normoalbuminuric People With Type 2 Diabetes MellitusdrheriNo ratings yet
- Complicaciones y Mortalidad en Pacientes Con Ezq y DBTDocument11 pagesComplicaciones y Mortalidad en Pacientes Con Ezq y DBTDanitza YhovannaNo ratings yet
- Psychiatric and Medical Conditions in Transition-Aged Individuals With ASDDocument13 pagesPsychiatric and Medical Conditions in Transition-Aged Individuals With ASDLAURA CAMILA CACERES DELGADONo ratings yet
- Clinical Study: Steroid-Induced Diabetes: Is It Just Unmasking of Type 2 Diabetes?Document6 pagesClinical Study: Steroid-Induced Diabetes: Is It Just Unmasking of Type 2 Diabetes?inaagustinpNo ratings yet
- Skiripsi Melda Yanti (1411216086)Document5 pagesSkiripsi Melda Yanti (1411216086)intan purnamaNo ratings yet
- Effect of BmiDocument5 pagesEffect of BmiSyaiful Putra RanaNo ratings yet
- Coffee and Tea Consumption and The Risk of Parkinson's DiseaseDocument7 pagesCoffee and Tea Consumption and The Risk of Parkinson's DiseaseJenivia LulileloNo ratings yet
- Bidirectional AssociationDocument10 pagesBidirectional AssociationAndrea MorenoNo ratings yet
- Diabetic Neuropathy CLINTHERDocument22 pagesDiabetic Neuropathy CLINTHERValerie hongNo ratings yet
- Frequency, Clinical Characteristics and Predictors of KetoacidosisDocument9 pagesFrequency, Clinical Characteristics and Predictors of KetoacidosisYogiPrimaZulkifliNo ratings yet
- Evaluation of Pre-Hypertension, Hypertension and Its Associated Factors Among I Year Medical StudentsDocument4 pagesEvaluation of Pre-Hypertension, Hypertension and Its Associated Factors Among I Year Medical StudentsutarinuNo ratings yet
- Compliance With Treatment of Patients With Hypertension in Almadinah Almunawwarah: A Community-Based StudyDocument7 pagesCompliance With Treatment of Patients With Hypertension in Almadinah Almunawwarah: A Community-Based StudyAjikNo ratings yet
- Association of Diabetic Retinopathy in Type II Diabetes Mellitus With Hba1c Levels: A StudyDocument6 pagesAssociation of Diabetic Retinopathy in Type II Diabetes Mellitus With Hba1c Levels: A StudyYoga TDNo ratings yet
- Quality of Life of Children With Type 1 Diabetes: A Systematic ReviewDocument12 pagesQuality of Life of Children With Type 1 Diabetes: A Systematic ReviewNila Sari ChandraNo ratings yet
- The Prevalence of Diabetic Retinopathy and Associated Risk Factors Among Sioux IndiansDocument3 pagesThe Prevalence of Diabetic Retinopathy and Associated Risk Factors Among Sioux IndiansTrx AntraxNo ratings yet
- The Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianFrom EverandThe Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianNo ratings yet
- Metrology Lab Report 1Document4 pagesMetrology Lab Report 1Wan FaiznurNo ratings yet
- Role-Play #1: Saving Energy: WellDocument4 pagesRole-Play #1: Saving Energy: WellDaniel VasquezNo ratings yet
- CinderellaDocument6 pagesCinderellaainiNo ratings yet
- BKM CH 01 AnswersDocument4 pagesBKM CH 01 AnswersDeepak OswalNo ratings yet
- School Form 1 (SF 1)Document6 pagesSchool Form 1 (SF 1)Precilla ZoletaNo ratings yet
- Ref DerbyDocument455 pagesRef DerbyjmaasoftNo ratings yet
- Art 2 SyllabusDocument2 pagesArt 2 Syllabusapi-260266731No ratings yet
- Chichewa Kalata Ndi Chimangirizo 1Document15 pagesChichewa Kalata Ndi Chimangirizo 1dysonjonas269No ratings yet
- f2f MUSICDocument44 pagesf2f MUSICRio CostalesNo ratings yet
- 2016 GP Y5 Infopack - Media + Social Issues - FINAL PDFDocument104 pages2016 GP Y5 Infopack - Media + Social Issues - FINAL PDFMelissaNo ratings yet
- Komposisi Jenis Tumbuhan Bawah Di Lahan Revegetasi Pasca Tambang BatubaraDocument14 pagesKomposisi Jenis Tumbuhan Bawah Di Lahan Revegetasi Pasca Tambang BatubaraRizka Putri SelinaNo ratings yet
- Evaluation Form MSCDocument5 pagesEvaluation Form MSCvikash kumarNo ratings yet
- Marketing Strategy of Pepsi AssaignmentDocument48 pagesMarketing Strategy of Pepsi AssaignmentZekria Noori AfghanNo ratings yet
- Breaking Down The Barriers: The Gut Microbiome, Intestinal Permeability and Stress-Related Psychiatric DisordersDocument20 pagesBreaking Down The Barriers: The Gut Microbiome, Intestinal Permeability and Stress-Related Psychiatric DisordersCSilva16No ratings yet
- Cadbury Beverages, Inc V3a RaeDocument49 pagesCadbury Beverages, Inc V3a RaeRaeleen St PierreNo ratings yet
- The Drum Magazine 23 OctoberDocument40 pagesThe Drum Magazine 23 OctoberFa BaNo ratings yet
- The Trophy Wife Mills Boon Comics by Rosalie Ash b0188d5pq4 PDFDocument5 pagesThe Trophy Wife Mills Boon Comics by Rosalie Ash b0188d5pq4 PDFmeenusshellNo ratings yet
- Technical Analysis of Sun PharmaDocument7 pagesTechnical Analysis of Sun PharmaAshutosh TulsyanNo ratings yet
- CFA Career Guide 2014 PDFDocument121 pagesCFA Career Guide 2014 PDFAlex CNo ratings yet
- Chapter 1 To 3Document26 pagesChapter 1 To 3Hyman Jay Blanco100% (1)
- 6QQMN969 Module OutlineDocument4 pages6QQMN969 Module OutlineyuvrajwilsonNo ratings yet
- 2G Feature ListDocument135 pages2G Feature ListPraveen DubeyNo ratings yet
- Crimes Case ListDocument53 pagesCrimes Case ListDaksh AnujNo ratings yet











![Prevalence and Its Associated Determinants of Diabetic Peripheral Neuropathy (DPN) in Individuals Having Type-2 Diabetes Mellitus in Rural South India _[PAUTHORS], Indian Journal of Community Medicine (IJCM)](https://imgv2-2-f.scribdassets.com/img/document/527040009/149x198/b045f9b0ff/1632384843?v=1)