Professional Documents
Culture Documents
381 Full
Uploaded by
waciy70505Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
381 Full
Uploaded by
waciy70505Copyright:
Available Formats
Canadian Experience with the Pipeline
Embolization Device for Repair of
Unruptured Intracranial Aneurysms
C.J. O'Kelly, J. Spears, M. Chow, J. Wong, M. Boulton, A.
Weill, R.A. Willinsky, M. Kelly and T.R. Marotta
This information is current as AJNR Am J Neuroradiol 2013, 34 (2) 381-387
of April 25, 2024. doi: https://doi.org/10.3174/ajnr.A3224
http://www.ajnr.org/content/34/2/381
ORIGINAL RESEARCH
INTERVENTIONAL
Canadian Experience with the Pipeline Embolization Device for
Repair of Unruptured Intracranial Aneurysms
C.J. O’Kelly, J. Spears, M. Chow, J. Wong, M. Boulton, A. Weill, R.A. Willinsky, M. Kelly, and T.R. Marotta
ABSTRACT
BACKGROUND AND PURPOSE: Flow-diverting stents, such as the PED, have emerged as a novel means of treating complex intracranial
aneurysms. This retrospective analysis of the initial Canadian experience provides insight into technical challenges, clinical and radiographic
outcomes, and complication rates after the use of flow-diverting stents for unruptured aneurysms.
MATERIALS AND METHODS: Cases were compiled from 7 Canadian centers between July 2008 and December 2010. Each center pro-
spectively tracked their initial experience; these data were retrospectively updated and pooled for analysis.
RESULTS: During the defined study period, 97 cases of unruptured aneurysm were treated with the PED, with successful stent deployment
in 94 cases. The overall complete or near-complete occlusion rate was 83%, with a median follow-up at 1.25 years (range 0.25–2.5 years).
Progressive occlusion was witnessed over time, with complete or near-complete occlusion in 65% of aneurysms followed through 6
months, and 90% of aneurysms followed through 1 year. Multivariate analysis found previous aneurysm treatment and female sex
predictive of persistent aneurysm filling. Most patients were stable or improved (88%), with the most favorable outcomes observed in
patients with cavernous carotid aneurysms. The overall mortality rate was 6%. Postprocedural aneurysm hemorrhage occurred in 3
patients (3%), while ipsilateral distal territory hemorrhage was observed in 4 patients (3.4%).
CONCLUSIONS: Flow-diverting stents represent an important tool in the treatment of complex intracranial aneurysms. The relative
efficacy and morbidity of this treatment must be considered in the context of available alternate interventions.
ABBREVIATIONS: ICH ⫽ intracerebral hemorrhage; PED ⫽ Pipeline embolization device
limited morbidity.2,3 Flow-diverting stents have been used to suc-
F low-diverting stents have emerged as a treatment option for
complex intracranial aneurysms. These flexible, low-porosity
stents limit flow into and out of intracranial aneurysms, resulting
cessfully treat complex aneurysms with limited therapeutic alter-
natives, yet their role in general aneurysm management remains
in thrombosis of the aneurysms over time.1 Early experience with to be defined. Rare but significant complications, such as delayed
these devices has suggested a high rate of aneurysm closure with aneurysm rupture and distal ICH, have tempered enthusiasm for
widespread use. Questions remain regarding the overall efficacy
Received March 19, 2012; accepted after revision May 21. of the devices, the morbidity of treatment, long-term outcomes,
From the Division of Neurosurgery (C.J.O., M.C.), Department of Surgery, University and the cost-effectiveness of these expensive devices.
of Alberta, Edmonton, Alberta, Canada; Division of Neurosurgery, Department of We present the initial Canadian experience with 1 flow-divert-
Surgery (J.S.), and Department of Radiology (R.A.W., T.R.M.), University of Toronto,
Toronto, Ontario, Canada; Division of Neurosurgery (J.W.), Department of Clinical ing stent, the PED (ev3; Plymouth, Minnesota). This retrospective
Neurosciences, University of Calgary, Calgary, Alberta, Canada; Division of Neuro-
surgery (M.B.), Department of Surgery, University of Western Ontario, London,
analysis provides a real-world sense of the efficacy, limitations,
Ontario, Canada; Department of Radiology (A.W.), University of Montreal, Mon- and complications associated with the PED. In many cases the
treal, Quebec, Canada; and Division of Neurosurgery, Department of Surgery
(M.K.), University of Saskatchewan, Saskatoon, Saskatchewan, Canada. results are positive, but important complications require circum-
Previously presented in abstract form at: Canadian Congress of Neurological Sci- spect incorporation of these devices into cerebrovascular practice.
ences, Vancouver, British Columbia, Canada, June 17, 2011; World Fedaration of In-
terventional and Therapeutic Neuroradiology, Capetown, South Africa, November
9, 2011. MATERIALS AND METHODS
Please address correspondence to Dr. Cian J. O’Kelly, 2D1.02 Mackenzie Centre, This is a retrospective cohort study of all unruptured aneurysm
8440-112 St, Edmonton, Alberta, Canada, T6G 2B7; e-mail: cian.okelly@alberta-
healthservices.ca cases treated with the PED in Canada between July 2008 and De-
Indicates article with supplemental on-line table. cember 2010. Case data were prospectively gathered at each of the
http://dx.doi.org/10.3174/ajnr.A3224 7 participating centers. Local research ethics board approval was
AJNR Am J Neuroradiol 34:381– 87 Feb 2013 www.ajnr.org 381
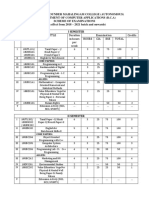
obtained at the University of Alberta. For the purpose of this Table 1: Clinical presentations
study, the data were anonymized and pooled for retrospective Number of Patients
analysis. During the initial portion of this study, the PED was only Clinical Presentation (%)
available through a Health Canada compassionate-use program. Visual complaints 36 (37.1%)
Diplopia (cranial nerve palsy) 24 (24.7%)
The initial cases at each site were proctored by expert users. The
Visual loss 12 (12.4%)
PED was considered primarily for cases where the alternative— Headaches 14 (14.4%)
either surgery or conventional coiling—was felt to carry either Incidental 25 (25.8%)
excessive procedural risk or a high likelihood of failure to durably Recanalization of previously treated aneurysm 17 (17.5%)
occlude the aneurysm. The PED was also considered as an alter- Neurological deficit 4 (4.12%)
Other 1 (1.0%)
native to vessel sacrifice for the treatment of large, complex ante-
rior circulation aneurysms.
Stent placement and periprocedural management were not
tic regression or Cox proportional hazards modeling, where
standardized but were generally uniform as a result of the guid-
appropriate.
ance of a relatively small core group of proctors. Patients were
preloaded with dual antiplatelet medication, mainly acetylsali-
RESULTS
cylic acid and clopidogrel, continued for an additional 6 months.
Baseline Characteristics
Dual antiplatelet treatment was extended in cases of in-stent ste-
A total of 109 PED cases were performed at the participating cen-
nosis. Where possible, stents were deployed by using a tri-axial
ters between June 2008 and December 2010, including 97 patients
catheter system consisting of a larger shuttle-type guide catheter
with unruptured aneurysms (12 patients with ruptured aneu-
(Cook Vascular, Vandergrift, Pennsylvania), a flexible distal ac-
rysms were excluded from this analysis). The mean age at the time
cess guide catheter (Neuron; Penumbra, Alameda, California),
of treatment was 56.5 years. Most patients were female (82.5%).
and a microcatheter (Marksman, ev3, Irvine, California; or Ren-
Visual complaints (diplopia, visual field changes, and visual acu-
egade Hi-Flo, Boston Scientific, Natick, Massachusetts). Full hep- ity changes) were the most common mode of presentation
arinization was initiated before establishing the triaxial catheter (37.1%); other presentations are summarized in Table 1. Patients
system, aiming for 2–2.5 times the activated coagulation time. presenting with other neurologic deficits were generally with mass
The number of stents deployed and the use of adjuvant coils was at effect, secondary to large partially thrombosed aneurysms, while 1
the discretion of the treating physicians. Postdeployment angio- patient presented with emboli from a similar aneurysm. One pa-
plasty, generally using a 4 ⫻ 10 mm to 4 ⫻ 20 mm HyperGlide tient (other) presented with middle ear effusion, secondary to a
balloon (ev3), was occasionally required to address problems with petrosal segment carotid artery aneurysm.4
stent kinking and inadequate vessel wall apposition. Most aneurysms in this series were large and wide-neck aneu-
Baseline characteristics were recorded, including patient de- rysms. The mean aneurysm diameter was 19 mm (range 2– 60
mographics, mode of presentation, and aneurysm specifics such mm), while the mean neck width was 8 mm (range 2–25 mm).
as location, largest diameter (mm), neck width (mm), and mor- The average neck-to-dome ratio was 0.48. Eight percent of the
phology. Periprocedural morbidity and mortality events were re- aneurysms had a fusiform morphology. Partial thrombosis of the
corded, as were any significant clinical events through follow-up. aneurysm sac was observed in 25.7% of cases. A detailed summary
The patients’ clinical status was recorded at planned follow-up of aneurysm location is shown in Fig 1. Aneurysms were predom-
assessments. Standardized outcome assessments were not rou- inantly located in the anterior circulation (81.4%), with 34% of
tinely performed at each institution and therefore could not be these in the cavernous segment and 58% in the supraclinoid
included in our analysis. Radiographic follow-up consisted of a segment.
combination of CTA, MRA, and DSA. Follow-up paradigms—in
particular, technique and timing—varied between centers. Aneu- Procedural Specifics
rysm closure was judged using all available radiographic modali- The PED was successfully deployed in 94 of 97 cases (96.9%). In 2
ties. Aneurysm filling was categorized as no significant change cases, the PED could not be deployed due to an inability to gain
(95%–100% of baseline contrast filling), residual aneurysm (5%– stable catheter access across the neck of a giant aneurysm. In 1 of
95% residual filling), near-complete occlusion (entry remnant, these cases, the parent vessel was ultimately sacrificed while con-
⬍5% residual filling), and complete occlusion (no filling). Stan- servative management was opted for in the other case. In the third
dardized assessment of contrast stasis was not available for anal- case, the PED retracted into the aneurysm, necessitating parent
ysis. In-stent stenosis was recorded for patients undergoing DSA, vessel occlusion. The patient had previously passed a test occlu-
whereas the residual aneurysm mass was estimated from the sion and tolerated the permanent vessel occlusion.
cross-sectional imaging (CTA and MRA). Residual aneurysm Of cases where device deployment was achieved, the mean
mass was noted as increased, not significantly changed (75%– number of PEDs used was 1.8 (range 1–13). In over half of the
100% of baseline), reduced (25%–75% of baseline), or signifi- cases (53.2%), a single PED was deployed, while 2 or 3 stents were
cantly reduced (⬍25% of baseline). used in 31.9% and 9.6% of cases, respectively. Five or more stents
All data were analyzed using SAS statistical software (version (range 5–13) were used in the remaining 5% of cases. Multiple
9.2; SAS, Cary, North Carolina). Kaplan-Meier methodology was PEDs were used more frequently in fusiform aneurysms (mean
followed for generation of time-to-event curves. Univariate and 4.1 PEDs, P ⬍ .001). Additional coils were placed in the aneurysm
multivariate analyses of outcomes were conducted by using logis- sac in 5.1% of cases. In most cases, partial coiling of the aneurysm
382 O’Kelly Feb 2013 www.ajnr.org
Table 2: Predictors of aneurysm closure over time: univariate
survival analysis
Covariate Hazard Ratio P Value
PED number 1.05 .36
Age 0.99 .69
Female gender 0.52 .03
Coil use 0.99 .69
Posterior circulation 0.57 .07
Aneurysm diameter 0.99 .52
Aneurysm neck 1.01 .55
Associated thrombus 1.05 .82
Recanalized 0.36 .002
Note:—PED number refers to number of Pipeline stents used to treat the aneurysm.
Coil use refers to the use of additional coils at the time of PED treatment. Recanalized
refers to a recurrence of a previously treated aneurysm.
FIG 1. Aneurysm location for cases in the Canadian experience. Sev-
enty-nine (81.4%) cases were located in the anterior circulation, with
18 (18.6%) located in the posterior circulation.
was undertaken to disrupt entry flow into the aneurysm sac. In 1
vertebrobasilar junction aneurysm, the nonstented vertebral ar-
tery was occluded with coils at its distal V4 segment. As expected,
most aneurysms continued to fill on the postdeployment control
angiogram, with only 2% of cases showing complete or near-com-
plete closure at this stage.
FIG 2. Kaplan-Meier survival plot demonstrating the rate of aneu-
rysm closure over time. Shaded circles indicate censored
Radiographic Outcomes observations.
Median follow-up for the entire cohort was 1.25 years (range
0.25–2.5 years). At the most recent radiographic follow-up, 68.4%
of aneurysms were completely occluded, with near-occlusion (en- residual aneurysm size (75%–100% of baseline). Reduced (25%–
try remnant) noted in an additional 15.8% of aneurysms. As such, 75% of baseline) or significantly reduced (⬍25% of baseline) size
complete or near-complete occlusion was noted in 84.2% of cases. was observed in 27 (33%) and 21 (26%) cases, respectively. As
Reduced aneurysm filling (5%–95% residual) was observed in indicated in Fig 2, the proportion of cases showing reduction in
4.2% of cases, while 11.6% of cases showed persistent filling size increases through long-term follow-up. Aneurysm growth
(⬎95% residual). The progressive closure of aneurysms over time occurred in 3 cases and was associated with adverse neurologic
is demonstrated in Fig 2. Persistent filling of the aneurysm was outcomes (described below).
observed infrequently beyond 1 year of follow-up. Predictors of DSA follow-up was available for analysis of in-stent stenosis
aneurysm closure were assessed in a univariate proportional haz- and vessel occlusion in 58 (61%) cases. Of the patients undergoing
ards model (Table 2). Recurrence of a previously treated aneu- angiography, most (90%) showed no evidence of in-stent steno-
rysm was associated with decreased aneurysm closure. Similarly, sis. There were 2 cases (3%) of mild in-stent stenosis, which re-
location in the posterior circulation demonstrated a trend for re- solved spontaneously in subsequent follow-up. Two cases (3%)
duced aneurysm closure over time. Multivariate analysis was per- demonstrated significant, but stable, stenosis of 50% and 70%.
formed for statistically significant univariate predictors (P ⬍ .10), There were 2 cases of delayed vessel occlusion (3%) occurring 7
with sex and previous treatment independently associated with and 12 months after the stent placement procedure. Neither of
reduced rates of aneurysm closure (Table 2). these cases was associated with permanent neurologic deficit,
Data on residual aneurysm mass were available for 82 of though 1 patient had a small area of diffusion restriction noted on
94 cases (87%). Overall, 31 cases (38%) showed no change in MR imaging.
AJNR Am J Neuroradiol 34:381– 87 Feb 2013 www.ajnr.org 383
Table 3: Predictors of mortality: univariate logistic regression
analysis
Covariate Odds Ratio P Value
Age 0.970 .27
Female gender 5.77 .04
Mode of presentation N/Aa .99
Posterior circulation 10.57 .01
Aneurysm diameter 0.97 .43
Aneurysm neck 1.04 .73
Associated thrombus 1.60 .60
a
Mode of presentation was analyzed as a global model categorizing presentations as
cranial nerve deficit, headache, incidental, neurologic deficit (noncranial nerve), re-
canalization of previously treated aneurysm, or other. Global model not significant;
individual predictors also not significant (odds ratios and P values not shown).
Clinical Outcomes and Complications
At most recent follow-up, 89.3% of patients are well, with either
no deficit or a stable or improved pre-existing deficit (84 of 94
patients). Four patients (4.3%) have new, persistent neurologic
deficits, all of which are improving at last follow-up. Overall mor-
tality in the series is 6.4% (6 cases), as summarized in the On-line
Table. In univariate analyses (Table 3), only aneurysm location in FIG 3. Kaplan-Meier survival plot comparing the rate of aneurysm
closure for cavernous segment aneurysms versus other locations.
the posterior circulation was associated with increased odds of Shaded circles indicate censored observations.
mortality. There was a trend toward increased mortality among
females. Of the 10 patients presenting with visual loss, 1 died Cavernous Segment Aneurysms
(Patient 4, On-line Table) and 9 were available for follow-up. Of Cavernous segment aneurysms represent a unique subset of the
these, 4 remained stable, 4 have significantly improved vision, and overall cohort. A total of 26 cavernous segment aneurysms were
1 had complete resolution of visual deficit. Of the 5 patients pre- treated, 70% presenting with cranial neuropathy. This subset
senting with a neurologic deficit, 1 died (Patient 6, On-line Ta- tended to be larger in size (mean diameter 21.4 mm versus 17.6
ble), 2 are stable, 1 has improved, and 1 deficit has resolved. The mm, P ⫽ .05). There was also a trend toward increased partial
outcomes for oculomotor cranial neuropathies are reviewed with thrombosis of the aneurysm fundus, observed in 38% of cavern-
the cavernous aneurysms below. ous aneurysms versus 20% for all other aneurysms (P ⫽ .07).
Hemorrhage from the treated aneurysm was documented in 3 Aneurysm closure is probably superior in this category. Although
cases (3.2%). One case (previously reported5) resulted in brain survival analysis does not indicate any increased rate of closure
stem hemorrhage and death (Patient 1, On-line Table). In an- over time (P ⫽ .90; Fig 3), the proportion of aneurysms going on
other case, there was a trace of subarachnoid blood noted on to complete or near-complete occlusion is higher. All cavernous
imaging, but death was attributed to acute aneurysm thrombosis aneurysms (100%) achieved complete or near-complete occlu-
and hydrocephalus (Patient 5, On-line Table). The third case oc- sion through follow-up compared with 78% of noncavernous ca-
curred over 1 year after aneurysm treatment. This patient had a rotid locations (P ⫽ .005).
Serious neurologic complications did not occur in this cohort,
complex previously ruptured and coiled carotid termination an-
with no incidence of distal ICH or aneurysmal hemorrhage. There
eurysm. The aneurysm continued to fill after treatment with a
were no deaths (0% mortality) in this subset, compared with 6
single Pipeline stent into the middle cerebral artery. An attempt
deaths in noncavernous locations (8.5%). New or worsened cra-
was made to coil the residual aneurysm and anterior cerebral ar-
nial nerve deficits occurred in 3 patients (11.5%) after treatment
tery outlet from the contralateral side. This failed and the patient
with the PED. In 2 cases, the cranial nerve deficit has resolved,
declined further treatment. She then presented with hemorrhage
whereas 1 of the patients has persistent though improved diplo-
from the index aneurysm. This was managed with surgical occlu-
pia. There were 2 periprocedural minor embolic strokes related to
sion of the A1 segment of the anterior cerebral artery, followed by
tortuous access to the aneurysm. In both cases, the associated
placement of second Pipeline stent. neurologic deficit—mild hemiparesis—resolved in follow-up.
Distal ipsilateral parenchymal hemorrhage occurred in 4 cases For patients presenting with cranial nerve deficit (18/26 cavern-
(4.3%). One patient died (Patient 2, On-line Table). One patient ous aneurysms), 11 have complete resolution (61%), with subto-
remained well without intervention. Two patients have persistent tal improvement noted in an additional 2 cases (11%) and no
but improving neurologic deficits, 1 required surgical evacuation significant change in the remaining 5 cases (28%).
of the hematoma, while the other was managed conservatively. In
addition to the case mentioned above (Patient 5, On-line Table), DISCUSSION
1 other patient developed acute hydrocephalus secondary to Review of the initial Canadian experience with the PED demon-
thrombosis of a vertebrobasilar junction aneurysm. This was suc- strates effective angiographic closure of the treated aneurysms,
cessfully managed with endoscopic third ventriculostomy. with 84.2% complete or near-complete occlusion through an av-
384 O’Kelly Feb 2013 www.ajnr.org
erage of 1.25 years follow-up. Survival analysis indicates progres- potential risk. In our series, symptomatic periprocedural ischemic
sive aneurysm closure over time. These results are comparable stroke was relatively rare, occurring in 4% of cases, with persis-
with other studies in the literature reporting angiographic aneu- tent, but improving, deficit in 2%. This study did not consider
rysm occlusion rates in between 74% and 94% of cases.2,3,6-11 In new silent ischemic events, as postprocedural MR imaging scans
the current study, multivariate analysis suggested female sex and were not available for all patients. Embolic events may occur at
previous aneurysm treatment as predictors of persistent aneu- increased frequency, given the size of the delivery devices and the
rysm filling. Many studies do not comment on predictors of an- complexity of cranial vascular access seen in typical flow-diver-
eurysm occlusion after flow-diverting stent placement. Although sion cases. On the other hand, dual antiplatelet therapy has been
small numbers precluded statistical analysis, McAuliffe et al8 associated with a reduction in thromboembolic events in series
identified fusiform aneurysms, smaller aneurysm size, and previ- using conventional coiling15,16 and with stent-assisted coiling
ous aneurysm treatment as predictors of persistent angiographic techniques.17 Distal ipsilateral hemorrhage has emerged as a more
filling in follow-up. Further study is required to better predict specific complication related to flow diversion. In our Canadian
successful aneurysm occlusion with flow-diverting stents. The experience, distal hemorrhage occurred in 4% of cases, resulting
most favorable results in this initial Canadian experience came in significant morbidity and mortality. The incidence of these
from the subset of cavernous segment aneurysms, with all cavern- hemorrhages varies in the literature, with no occurrences in most
ous aneurysms closed by 1 year. There were no deaths and signif- series.3,6,8,9,11 Fischer et al2 reported 3 cases in their experience
icant morbidity was uncommon. Most patients presenting with (101 cases) with the PED. The putative mechanism is unknown,
cranial nerve deficits were resolved or improved in follow-up. but hemorrhagic conversion of ischemic embolic events, due to
Flow-diverting stents may represent an important treatment op- antiplatelet medication, combined with altered pressure dynam-
tion for patients with large cavernous aneurysms; however, one ics, due to redirected flow, have been postulated.18 Although the
must consider that proximal occlusion is a safe and effective treat- phenomenon appears to be relatively specific to flow diversion, it
ment in appropriately selected patients.12 has been described with conventional stent-assisted coiling pro-
There were 2 general sources of morbidity after PED treatment cedures.19 Finally, aneurysms may undergo an increase in size
of the aneurysms in this series: failure to alter the natural history after treatment due to acute thrombosis and perianeurysmal
or complications related to placement of the device. The natural edema. In cavernous aneurysms, this manifested as new cranial
history of unruptured aneurysms has never been clearly defined. neuropathy. Most of these resolved over time; however, certain
Nevertheless, most studies have shown that large aneurysms, such patients had persistent deficits. This acute increase in aneurysm
as those treated in this study, have a high risk of rupture and mass effect also resulted in hydrocephalus, necessitating a surgical
neurologic morbidity due to progressive growth.13 In many cases, intervention (third ventriculostomy). If hydrocephalus is a po-
the PED appears to avert this natural history by leading to aneu- tential concern on the basis of the preoperative imaging, prophy-
rysm occlusion and even regression of the aneurysm mass. How- lactic intervention before initiation of antiplatelet medication
ever, there are important exceptions. Despite successful PED may be beneficial.
placement, aneurysm rupture occurred in 3.2% of cases in this Allowing for overlap of specific complications, the overall
series. One of the cases occurred over 1 year after the initial treat- morbidity and mortality rate in this series is 10.7% (6.3% mortal-
ment in an aneurysm that demonstrated persistent filling despite ity, 4.4% morbidity). The observed morbidity in this series must
the successful PED placement. Before presenting with rehemor- be considered in the context of the existing therapeutic alterna-
rhage, the patient had declined further intervention. The other tives. Effective surgical treatment of large aneurysms can fre-
cases bled relatively early after partial thrombosis of the treated quently be achieved, with acceptable morbidity and mortality.
aneurysms. This pattern is similar to other reports in the literature More elaborate surgical procedures, such as high-flow bypass and
and has been postulated by others to relate to thrombus-mediated circulatory arrest, have elevated procedural risk. In a recent report
weakening of the aneurysm wall.5,14 In this manner, it is possible from a high-volume center, surgery for giant aneurysms using
that the flow diversion may actually increase the risk of rupture bypass and proximal occlusion techniques has a reported mortal-
after treatment. The true incidence of aneurysm rupture after ity of 13% and permanent neurologic morbidity of 9%.20 Simi-
flow-diverting stent placement remains unknown. Kulcsár et al14 larly, in a series of 105 patients with hypothermic circulatory ar-
reported a series of 13 similar cases pooled from multiple institu- rest at the Barrow Neurological Institute, the combined
tions; however, the appropriate denominator could not be estab- procedure-related morbidity and mortality was 32%.21 Conven-
lished. In other series, this delayed aneurysm rupture is a relatively tional endovascular approaches such as coiling with balloon or
rare occurrence, observed in 0%,3,9 1%,6 and 1.4%6 of cases de- stent assistance may have relatively lower procedural risk; how-
pending on the report. In the absence of aneurysm rupture, failure ever, these interventions have been shown to have diminished
to alter the natural history can manifest as progressive aneurysm efficacy for large, complex aneurysms leading to an increased risk
growth. In the Canadian experience, there were 3 cases of progres- of recurrence and retreatment. In a systematic review of giant
sive aneurysm enlargement despite the flow-diverting stent. Im- aneurysms treated with conventional endovascular approaches,
portantly, this progression in size corresponded to adverse neu- the complete occlusion rate was 57%, with recanalization in
rologic outcomes. 27%.22 The rates of morbidity and mortality were 17% and 8%,
The second source of morbidity after placement of a flow- respectively.22
diverting stent is procedure-related complication. As with any Given that flow-diverting stents are a relatively recent innova-
endovascular procedure, periprocedural stroke is an important tion, their performance through long-term follow-up remains to
AJNR Am J Neuroradiol 34:381– 87 Feb 2013 www.ajnr.org 385
be evaluated. Imaging protocols varied significantly between and tives. Ongoing analysis of flow-diverting stents for radiographic
within the participating centers. In our experience, CTA is pre- and clinical performance is required.
ferred over MRA in cases where there are not additional coils or
clips causing artifacts. Contrast-enhanced CTA and MRA appear Disclosures: Michael Kelly—RELATED: Support for Travel to Meetings for the Study
to be sufficient to evaluate for residual aneurysm filling as well as or Other Purposes: Covidien-ev3, Comments: Pipeline proctors course in Anakara,
Turkey, April 2011, and Pipeline Users Meeting, Calgary, AB, January 2012—reimburse-
the residual aneurysm mass. Neither technique is suited to evalu- ment for travel expenses only; OTHER RELATIONSHIPS: The 2 meetings were about
ating in-stent stenosis. DSA can be used at 6 months to screen for the Pipeline embolization device, which is one of the devices reported in the man-
in-stent stenosis, thereby allowing a decision to be made regard- uscript. Thomas R. Marotta—RELATED: Consulting Fee or Honorarium: Proctoring
for PED from ev3, Covidien; Support for Travel to Meetings for the Study or Other
ing continuation of dual antiplatelet therapy. The optimal use and
Purposes: Proctoring for PED from ev3, Covidien; UNRELATED: Consultancy: Proc-
need for DSA in long-term follow-up requires further analysis. toring for PED from ev3, Covidien; Patents (planned, pending, or issued): EVASC
Significant in-stent stenosis is relatively rare, occurring in 2 medical: eclips – endovascular clip system. Drs. Marotta, Kelly, and O’Kelly have
cases in this series, with both patients remaining relatively stable served as proctors for ev3 Endovascular on Pipeline deployment cases.
or improving over time. Of greater concern are our 2 cases of
delayed vessel occlusion. Fortunately, neither patient suffered
lasting neurologic consequences because of aneurysm locations in REFERENCES
the anterior circulation with intact collateral circulation. Fiorella 1. Bendok BR, Parkinson RJ, Hage ZA, et al. The effect of vascular
reconstruction device-assisted coiling on packing density, effective
et al23 reported a case with delayed stent thrombosis in the poste-
neck coverage, and angiographic outcome: an in vitro study. Neu-
rior circulation, with significant morbidity. The timeframe for rosurgery 2007;61:835– 40; discussion 840 – 41
most studies in the literature precludes effective analysis of this 2. Fischer S, Vajda Z, Aguilar Perez M, et al. Pipeline embolization
phenomenon. As such, the relative uncertainty in long-term per- device (PED) for neurovascular reconstruction: initial experience
formance should be factored into clinical decision-making sur- in the treatment of 101 intracranial aneurysms and dissections.
rounding potential flow-diversion interventions. Neuroradiology 2012;54:369 – 82
This study suffers from a number of limitations, given its ret- 3. Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular recon-
struction of cerebral aneurysms with the Pipeline embolization
rospective and nonrandomized nature. Outcomes were self-re-
device: the Buenos Aires experience. Neurosurgery 2009;64:632– 42;
ported by the treating interventionalist, introducing potential discussion 642– 43; quiz N6
measurement bias. Standardized outcome measures such as an- 4. Fuller E, Marotta TR, Chen JM, et al. Middle ear aneurysm treated
giographic grading scales and clinical outcome scales were not with an innovative, vessel-preserving, aneurysm-occluding stent.
uniformly applied and were not available for complete analysis. Laryngoscope 2010;120:796 –99
Due to the proctoring requirements, case selection and stent de- 5. Chow M, McDougall C, O’Kelly C, et al. Delayed spontaneous rup-
ture of a posterior inferior cerebellar artery aneurysm following
ployment were subject to expert supervision, limiting generaliz-
treatment with flow diversion: a clinicopathologic study. AJNR
ability of the data. This study was not, however, intended to pro- Am J Neuroradiol 2012;33:E46 –51
vide definitive answers. Rather, this study reports a nascent 6. Byrne JV, Beltechi R, Yarnold JA, et al. Early experience in the treat-
experience with a novel technology used to treat challenging in- ment of intra-cranial aneurysms by endovascular flow diversion: a
tracranial aneurysms. The purpose of this review is to highlight multicentre prospective study. PLoS One 2010;5
areas for further research and study. Focused randomized trials 7. Lubicz B, Collignon L, Raphaeli G, et al. Flow-diverter stent for the
endovascular treatment of intracranial aneurysms: a prospective
are needed determine the relative efficacy of flow-diverting stents
study in 29 patients with 34 aneurysms. Stroke 2010;41:2247–53
compared with standard aneurysm treatment. Further data are 8. McAuliffe W, Wycoco V, Rice H, et al. Immediate and midterm
needed on long-term outcomes as well as predictors of aneurysm results following treatment of unruptured intracranial aneurysms
closure and procedural complications. Finally, even if flow-di- with the Pipeline embolization device. AJNR Am J Neuroradiol
verting stents can be established as a safe and effective treatment 2012;33:164 –70
for intracranial aneurysms, it must be determined whether these 9. Nelson PK, Lylyk P, Szikora I, et al. The Pipeline embolization device
for the intracranial treatment of aneurysms trial. AJNR Am J Neu-
expensive devices are cost-effective for health care systems. Of
roradiol 2011;32:34 – 40
note, the cost of a single PED approaches 3– 4 times that of a
10. Szikora I, Berentei Z, Kulcsar Z, et al. Treatment of intracranial an-
conventional intracranial stent. As a result, a case using a single eurysms by functional reconstruction of the parent artery: the Bu-
PED may have a similar cost to stent-assisted coiling; however, the dapest experience with the Pipeline embolization device. AJNR
costs rise exponentially with multiple PED use. Whether cost sav- Am J Neuroradiol 2010;31:1139 – 47
ings are realized in prevention of recurrence or complications 11. Wagner A, Cortsen M, Hauerberg J, et al. Treatment of intracranial
requires further analysis. aneurysms. Reconstruction of the parent artery with flow-diverting
(Silk) stent. Neuroradiology 2012;54:709 –18
12. Niiro M, Shimozuru T, Nakamura K, et al. Long-term follow-up
CONCLUSIONS study of patients with cavernous sinus aneurysm treated by proxi-
Flow-diverting stents such as the PED represent an important tool mal occlusion. Neurol Med Chir (Tokyo) 2000;40:88 –96; discussion
in the treatment of complex intracranial aneurysms. These stents 96 –97
have the potential to achieve dramatic results in difficult aneu- 13. Wiebers DO, Whisnant JP, Huston J 3rd, et al. Unruptured intracra-
nial aneurysms: natural history, clinical outcome, and risks of sur-
rysms, but complications and treatment failure can occur. Our
gical and endovascular treatment. Lancet 2003;362:103–10
results suggest that enthusiasm for this technology should be tem- 14. Kulcsár Z, Wetzel SG, Augsburger L, et al. Effect of flow diversion
pered by a careful consideration of the efficacy and morbidity of treatment on very small ruptured aneurysms. Neurosurgery
these devices compared with more standard treatment alterna- 2010;67:789 –93
386 O’Kelly Feb 2013 www.ajnr.org
15. Hwang G, Jung C, Park SQ, et al. Thromboembolic complications of to the stent-remodeled coil embolization of intracranial aneu-
elective coil embolization of unruptured aneurysms: the effect of rysms. Neurosurgery 2010;67:73–78; discussion 78 –79
oral antiplatelet preparation on periprocedural thromboembolic 20. Sughrue ME, Saloner D, Rayz VL, et al. Giant intracranial
complication. Neurosurgery 2010;67:743– 48; discussion 748 aneurysms: evolution of management in a contemporary surgical
16. Yamada NK, Cross DT 3rd, Pilgram TK, et al. Effect of antiplatelet series. Neurosurgery 2011;69:1261–70; discussion 1270 –71
therapy on thromboembolic complications of elective coil emboli- 21. Ponce FA, Spetzler RF, Han PP, et al. Cardiac standstill for cerebral
zation of cerebral aneurysms. AJNR Am J Neuroradiol 2007;28:1778 – 82 aneurysms in 103 patients: an update on the experience at the Barrow
17. Brooks NP, Turk AS, Niemann DB, et al. Frequency of thromboem- Neurological Institute. Clinical article. J Neurosurg 2011;114:877– 84
bolic events associated with endovascular aneurysm treatment: ret- 22. Parkinson RJ, Eddleman CS, Batjer HH, et al. Giant intracranial
rospective case series. J Neurosurg 2008;108:1095–100 aneurysms: endovascular challenges. Neurosurgery 2006;59:S103–
18. Cruz JP, Chow MC, O’Kelly CJ, et al. Delayed ipsilateral parenchy- 12; discussion S3–13
mal hemorrhage following flow diversion for the treatment of an- 23. Fiorella D, Hsu D, Woo HH, et al. Very late thrombosis of a Pipeline
terior circulation aneurysms. AJNR Am J Neuroradiol 2012;33:603– 08 embolization device construct: case report. Neurosurgery 2010;67:
19. Kim DJ, Suh SH, Kim BM, et al. Hemorrhagic complications related E313–14; discussion E314
AJNR Am J Neuroradiol 34:381– 87 Feb 2013 www.ajnr.org 387
You might also like
- Microbiology With Diseases by Body System 4th Edition Bauman Solutions ManualDocument6 pagesMicrobiology With Diseases by Body System 4th Edition Bauman Solutions Manuala507104630No ratings yet
- Stellite 6 Datasheet PDFDocument2 pagesStellite 6 Datasheet PDFEswaran100% (1)
- Short - and Long-Term Outcomes at A Single InstitutionDocument7 pagesShort - and Long-Term Outcomes at A Single InstitutionJonathan Frimpong AnsahNo ratings yet
- International Journal of Gerontology: Hung-Bun Lam, Li-Fen ChaoDocument4 pagesInternational Journal of Gerontology: Hung-Bun Lam, Li-Fen ChaoKoesoema WijayaNo ratings yet
- Cerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDocument11 pagesCerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDaniel EllerNo ratings yet
- 82 cases-Tub-multicenter-2018-ChanghaiDocument10 pages82 cases-Tub-multicenter-2018-Changhaiying huangNo ratings yet
- 10 3174@ajnr A6814Document7 pages10 3174@ajnr A6814Stefano BruniNo ratings yet
- Metaanalisis FD en Agudo Ajnr 223 Pacientes CagnazoDocument7 pagesMetaanalisis FD en Agudo Ajnr 223 Pacientes CagnazoangelNo ratings yet
- Interdisciplinary Neurosurgery: Advanced Techniques and Case ManagementDocument16 pagesInterdisciplinary Neurosurgery: Advanced Techniques and Case ManagementEvelyn JudithNo ratings yet
- Medip, IJRMS-7729 ODocument7 pagesMedip, IJRMS-7729 ORagupathi MNo ratings yet
- Lee, Et Al. 2018 - JACCDocument8 pagesLee, Et Al. 2018 - JACCCARLOS SANTIAGO PEREZ RODRIGUEZNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofNatalia ArizaNo ratings yet
- 62 2020 Article 898Document7 pages62 2020 Article 898sinamirjaniNo ratings yet
- Trial of Endovasculr Treatment of Acute Basilar Artery OcclusionDocument12 pagesTrial of Endovasculr Treatment of Acute Basilar Artery OcclusionVictorNo ratings yet
- TurkeyGMJ 62 200 enDocument6 pagesTurkeyGMJ 62 200 enCocoNo ratings yet
- Tomasello ContourDocument11 pagesTomasello ContourangelNo ratings yet
- 1 s2.0 S0929664617300487 MainDocument8 pages1 s2.0 S0929664617300487 MainSuryati HusinNo ratings yet
- Salvage of Malfunction DPDocument5 pagesSalvage of Malfunction DPBandac AlexandraNo ratings yet
- PCA Cierre Por Cateterismo en Prematutos ExtremosDocument9 pagesPCA Cierre Por Cateterismo en Prematutos Extremosannie.estdiNo ratings yet
- Endovascular Stentgraft Placement in Aortic Dissection A MetaanalysisDocument10 pagesEndovascular Stentgraft Placement in Aortic Dissection A MetaanalysisCiubuc AndrianNo ratings yet
- 2022 Perioperative Complications of Transvenous Embolization of Ruptured Intracranial Arteriovenous MalformationsDocument7 pages2022 Perioperative Complications of Transvenous Embolization of Ruptured Intracranial Arteriovenous MalformationsstaseaditNo ratings yet
- The Management of Severe Aortoiliac Occlusive Disease: Endovascular Therapy Rivals Open ReconstructionDocument10 pagesThe Management of Severe Aortoiliac Occlusive Disease: Endovascular Therapy Rivals Open ReconstructionRobert ChristevenNo ratings yet
- Ejemplo1 Tabla1Document12 pagesEjemplo1 Tabla1Isabel MartNo ratings yet
- The Cleveland Clinic Experience From 89 To 98Document10 pagesThe Cleveland Clinic Experience From 89 To 98Vlad NeagoeNo ratings yet
- 1638 FullDocument8 pages1638 Fulldps_1976No ratings yet
- Cardiac Interventions in Neonates WiDocument11 pagesCardiac Interventions in Neonates WiimNo ratings yet
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552No ratings yet
- ACO Peripro 2016Document10 pagesACO Peripro 2016Philippe Bocanegra FernándezNo ratings yet
- Artigo HGF Neorologia Maio 2021Document11 pagesArtigo HGF Neorologia Maio 2021Daniela MarinhoNo ratings yet
- Epistksis AnteriorDocument5 pagesEpistksis AnterioradyNo ratings yet
- An Outcomes Analysis of Anterior Epistaxis Management in The Emergency DepartmentDocument5 pagesAn Outcomes Analysis of Anterior Epistaxis Management in The Emergency DepartmentadyNo ratings yet
- 8cases - Complex MCA-Tub-2020-ChanghaiDocument8 pages8cases - Complex MCA-Tub-2020-Changhaiying huangNo ratings yet
- Laringo y BroncoespasmoDocument4 pagesLaringo y BroncoespasmoLUIS FERNANDO GOMEZ CANONo ratings yet
- Ultrasound-Guided Subclavian Vein Catheterization. A Systematic Review and Meta-Analysis. Crit Care Med 2015Document10 pagesUltrasound-Guided Subclavian Vein Catheterization. A Systematic Review and Meta-Analysis. Crit Care Med 2015angelama1783riosNo ratings yet
- ATTENTION TrialDocument12 pagesATTENTION TrialmrabhilekhNo ratings yet
- The Management and Outcome For Patients With Chronic Subdural Hematoma: A Prospective, Multicenter, Observational Cohort Study in The United KingdomDocument8 pagesThe Management and Outcome For Patients With Chronic Subdural Hematoma: A Prospective, Multicenter, Observational Cohort Study in The United KingdomRosario RosarioNo ratings yet
- Chronic SDHDocument8 pagesChronic SDHAnonymous A9R0aLsNo ratings yet
- Bomba de Flujo Microaxial en El Shock Cardiogénico Relacionado ConDocument12 pagesBomba de Flujo Microaxial en El Shock Cardiogénico Relacionado ConAdrianaIDCNo ratings yet
- Lemus Rangel 2010Document2 pagesLemus Rangel 2010audiNo ratings yet
- [19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedDocument7 pages[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedBruno MañonNo ratings yet
- Follow-Up Transcatheter Closure of Atrial Septal Defect in Young Children: Results andDocument7 pagesFollow-Up Transcatheter Closure of Atrial Septal Defect in Young Children: Results andKholid KuNo ratings yet
- Intubasi SulitDocument11 pagesIntubasi Sulitpcyjx6s2qjNo ratings yet
- Jurnal THTDocument3 pagesJurnal THTValentina AdindaNo ratings yet
- Endovascular Management of Acute Epidural Hematomas: Clinical Experience With 80 CasesDocument7 pagesEndovascular Management of Acute Epidural Hematomas: Clinical Experience With 80 CasesDeby AnditaNo ratings yet
- Percutaneous Implantation of An Entirely Intracardiac Leadless PacemakerDocument11 pagesPercutaneous Implantation of An Entirely Intracardiac Leadless PacemakerRaul OrtegaNo ratings yet
- Jagsi 2014Document9 pagesJagsi 2014Arlette M.No ratings yet
- STITCH Protocol 2011Document9 pagesSTITCH Protocol 2011Crhistian GarcíaNo ratings yet
- 803 FullDocument8 pages803 FullYud yaoNo ratings yet
- Septic ShockDocument12 pagesSeptic ShockPatrick CommettantNo ratings yet
- ArticolsssaDocument11 pagesArticolsssaCosmin GabrielNo ratings yet
- Eufred Study Results: Progressive Occlusion Increases Over Time Ive Occlusion Increases ODocument20 pagesEufred Study Results: Progressive Occlusion Increases Over Time Ive Occlusion Increases OUssiy RachmanNo ratings yet
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaNo ratings yet
- Single-Visit Endovenous Laser Treatment and Tributary Procedures For Symptomatic Great Saphenous Varicose VeinsDocument5 pagesSingle-Visit Endovenous Laser Treatment and Tributary Procedures For Symptomatic Great Saphenous Varicose VeinsValeriaNo ratings yet
- Proceedings of The 2014 Spring Meeting of The Society of British 2014Document40 pagesProceedings of The 2014 Spring Meeting of The Society of British 2014rabiatul adawiyahNo ratings yet
- (19330693 - Journal of Neurosurgery) Neuroendoscopic Stent Placement For Cerebrospinal Fluid Pathway Obstructions in AdultsDocument9 pages(19330693 - Journal of Neurosurgery) Neuroendoscopic Stent Placement For Cerebrospinal Fluid Pathway Obstructions in AdultsVlad VPNo ratings yet
- 6 Antithrombotic Therapy in Patients With Infective EndocarditisDocument12 pages6 Antithrombotic Therapy in Patients With Infective Endocarditisabdeali hazariNo ratings yet
- Endovascular Embolization in The Treatment of EpistaxisDocument7 pagesEndovascular Embolization in The Treatment of Epistaxisjasa ebook18No ratings yet
- Nerjm SesionDocument12 pagesNerjm SesionjorgeNo ratings yet
- Bess Is Sow 2014Document2 pagesBess Is Sow 2014Alfredo ChoquetNo ratings yet
- Bernard D. Prendergast and Pilar Tornos: Surgery For Infective Endocarditis: Who and When?Document26 pagesBernard D. Prendergast and Pilar Tornos: Surgery For Infective Endocarditis: Who and When?om mkNo ratings yet
- Current Endovascular Strategies For Cerebral Venous Thrombosis: Report of The SNIS Standards and Guidelines CommitteeDocument8 pagesCurrent Endovascular Strategies For Cerebral Venous Thrombosis: Report of The SNIS Standards and Guidelines CommitteeRafika Ayu NadiaNo ratings yet
- State of the Art Techniques in Critical Care Echocardiography: 3D, Tissue, ContrastFrom EverandState of the Art Techniques in Critical Care Echocardiography: 3D, Tissue, ContrastKonstantin YastrebovNo ratings yet
- kij5Document10 pageskij5waciy70505No ratings yet
- kij4Document10 pageskij4waciy70505No ratings yet
- 1 s2.0 S1877050917327254 MainDocument8 pages1 s2.0 S1877050917327254 Mainwaciy70505No ratings yet
- 1 s2.0 S1474667017328033 MainDocument6 pages1 s2.0 S1474667017328033 Mainwaciy70505No ratings yet
- 1 s2.0 S0042698900002595 MainDocument12 pages1 s2.0 S0042698900002595 Mainwaciy70505No ratings yet
- 1 s2.0 S1474667017331336 MainDocument6 pages1 s2.0 S1474667017331336 Mainwaciy70505No ratings yet
- Resehk Aplle JuiceDocument6 pagesResehk Aplle Juicewaciy70505No ratings yet
- SIPRIPP21Document64 pagesSIPRIPP21waciy70505No ratings yet
- 1 s2.0 S1474667017341010 MainDocument5 pages1 s2.0 S1474667017341010 Mainwaciy70505No ratings yet
- 1 s2.0 S0898122100003400 MainDocument14 pages1 s2.0 S0898122100003400 Mainwaciy70505No ratings yet
- S On The Yield of AppDocument8 pagesS On The Yield of Appwaciy70505No ratings yet
- 1 s2.0 S0927776512003426 MainDocument10 pages1 s2.0 S0927776512003426 Mainwaciy70505No ratings yet
- Paster Barkai Golan 2008 Mouldy Fruits and Vegetables As A Source of Mycotoxins Part 2Document12 pagesPaster Barkai Golan 2008 Mouldy Fruits and Vegetables As A Source of Mycotoxins Part 2waciy70505No ratings yet
- Canadian Experience Discourse and Anti-Racialism in A Post-Racial SocietyDocument21 pagesCanadian Experience Discourse and Anti-Racialism in A Post-Racial Societywaciy70505No ratings yet
- 1 s2.0 S0163725899000480 MainDocument18 pages1 s2.0 S0163725899000480 Mainwaciy70505No ratings yet
- Walitt Et Al-2015-Cochrane Database of Systematic ReviewsDocument54 pagesWalitt Et Al-2015-Cochrane Database of Systematic Reviewswaciy70505No ratings yet
- Capital Mobilization of Skilled Migrants - A Relational Perspective - Al Ariss - 2011 - British Journal of Management - Wiley Online LibraryDocument51 pagesCapital Mobilization of Skilled Migrants - A Relational Perspective - Al Ariss - 2011 - British Journal of Management - Wiley Online Librarywaciy70505No ratings yet
- Immigrant CredentialsDocument10 pagesImmigrant Credentialswaciy70505No ratings yet
- Rearranging The Deck Chairs? A Critical Examination of Canada'S Shifting (Im) Migration PoliciesDocument1 pageRearranging The Deck Chairs? A Critical Examination of Canada'S Shifting (Im) Migration Policieswaciy70505No ratings yet
- Ucalgary 2021 Marulanda DavidDocument167 pagesUcalgary 2021 Marulanda Davidwaciy70505No ratings yet
- Labour Market Experiences of Recent DependeDocument115 pagesLabour Market Experiences of Recent Dependewaciy70505No ratings yet
- Immigrant Skills and Immigrant Outcomes Under A SeDocument61 pagesImmigrant Skills and Immigrant Outcomes Under A Sewaciy70505No ratings yet
- Settlement of Newcomers To Canada Fall 2010Document224 pagesSettlement of Newcomers To Canada Fall 2010waciy70505No ratings yet
- The Relationship Between Students Course Perception and Their Approaches To Studying in Undergraduate Science Courses A Canadian ExperienceDocument21 pagesThe Relationship Between Students Course Perception and Their Approaches To Studying in Undergraduate Science Courses A Canadian Experiencewaciy70505No ratings yet
- An Overview of Discourses of Skilled ImmDocument35 pagesAn Overview of Discourses of Skilled Immwaciy70505No ratings yet
- Admin,+cws19n3 MojabDocument6 pagesAdmin,+cws19n3 Mojabwaciy70505No ratings yet
- Immigration Policy, National Origin, and Immigrant Skills: A Comparison of Canada and The United StatesDocument46 pagesImmigration Policy, National Origin, and Immigrant Skills: A Comparison of Canada and The United Stateswaciy70505No ratings yet
- Chapter4 OF mATERIAL ENGINEERINGDocument6 pagesChapter4 OF mATERIAL ENGINEERINGaljhun fujitsuNo ratings yet
- Pipelife Long Length PE Pipe SystemsDocument28 pagesPipelife Long Length PE Pipe SystemsAhceneNo ratings yet
- MATH 415 (Operational Research II)Document2 pagesMATH 415 (Operational Research II)saeedNo ratings yet
- Revit To Design Builder PDFDocument4 pagesRevit To Design Builder PDFMayNo ratings yet
- Seminar in Seminar in Translation Informatics. InformaticsDocument3 pagesSeminar in Seminar in Translation Informatics. InformaticsMohammed Sabri BatainehNo ratings yet
- Fluke199XRAY: Users ManualDocument22 pagesFluke199XRAY: Users ManualAndres CañaveralNo ratings yet
- Workplace Injuries - Kind of Accident (LFSINJKND)Document22 pagesWorkplace Injuries - Kind of Accident (LFSINJKND)Osman KantheNo ratings yet
- Be Summer 2012Document2 pagesBe Summer 2012babaf79912No ratings yet
- Certification of Engineering Calculation 2: I-FormDocument69 pagesCertification of Engineering Calculation 2: I-FormParantap RahaNo ratings yet
- Cost-Volume-Profit Relationships: Mcgraw-Hill /irwinDocument82 pagesCost-Volume-Profit Relationships: Mcgraw-Hill /irwinXu FengNo ratings yet
- Math 115 Uiuc Written Homework 6 SolutionsDocument4 pagesMath 115 Uiuc Written Homework 6 Solutionsafmspqvdy100% (1)
- Bca 2018 2021 PDFDocument94 pagesBca 2018 2021 PDFBala SivaramNo ratings yet
- Manual Ricoh Aficio SG3110SFNwDocument128 pagesManual Ricoh Aficio SG3110SFNwvalentindanielNo ratings yet
- Electrochemistry Short Answers Type Questions PDFDocument7 pagesElectrochemistry Short Answers Type Questions PDFAKSHAT KUMARNo ratings yet
- Business Research Methods: Session 6 To 7Document109 pagesBusiness Research Methods: Session 6 To 7Contact InfoNo ratings yet
- Interrupts and Traps in Oberon-ARMDocument3 pagesInterrupts and Traps in Oberon-ARMmqt99311zwoho.comNo ratings yet
- Datasheet c5271Document1 pageDatasheet c5271Abel RodriguezNo ratings yet
- MM 1Document6 pagesMM 1Rana Naveed0% (1)
- FreeNAS 11.2Document370 pagesFreeNAS 11.2phong nguyen huuNo ratings yet
- MU 4080 English Version 1.0.0Document43 pagesMU 4080 English Version 1.0.0Matz100% (1)
- The Last ProblemsDocument4 pagesThe Last ProblemsAnirban SahaNo ratings yet
- Spatial vs. Frequency DomainDocument6 pagesSpatial vs. Frequency DomainakhorshidinetNo ratings yet
- CATALOGO PRODOTTI 2013 Per Sito WEB TEDDocument52 pagesCATALOGO PRODOTTI 2013 Per Sito WEB TEDmuhammad abidin100% (1)
- Electric Power Systems. Vol. I. Electric NetworksDocument843 pagesElectric Power Systems. Vol. I. Electric Networksluciantoma75% (4)
- Lm2596-Xxe5/F5: Cystech Electronics CorpDocument12 pagesLm2596-Xxe5/F5: Cystech Electronics Corpfabian orozNo ratings yet
- 9 - ATPL Questions MeteorologyDocument99 pages9 - ATPL Questions MeteorologyRitwik Chowdhury100% (1)
- Notes On Sandwich MaterialsDocument57 pagesNotes On Sandwich Materialsarcadio_buendiaNo ratings yet
- Description: 2009 Dodge Journey SE 2009 Dodge Journey SEDocument312 pagesDescription: 2009 Dodge Journey SE 2009 Dodge Journey SEChristian Martinez100% (1)







































![[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matched](https://imgv2-2-f.scribdassets.com/img/document/722525723/149x198/0c84be9862/1712965550?v=1)