Professional Documents
Culture Documents
Aberegg 2020 Oi 200676 1603818809.24385
Aberegg 2020 Oi 200676 1603818809.24385
Uploaded by
rest_a2003Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aberegg 2020 Oi 200676 1603818809.24385
Aberegg 2020 Oi 200676 1603818809.24385
Uploaded by
rest_a2003Copyright:
Available Formats
Original Investigation | Pulmonary Medicine
Clinical, Bronchoscopic, and Imaging Findings of e-Cigarette, or Vaping,
Product Use–Associated Lung Injury Among Patients Treated
at an Academic Medical Center
Scott K. Aberegg, MD, MPH; Meghan M. Cirulis, MD; Sean D. Maddock, MD; Andrew Freeman, MD; Lynn M. Keenan, MD; Cheryl S. Pirozzi, MD, MS;
Sanjeev M. Raman, MBBS, MD; Joyce Schroeder, MD; Howard Mann, MBBCh; Sean J. Callahan, MD
Abstract Key Points
Question What are the typical clinical,
IMPORTANCE e-Cigarette, or vaping, product use–associated lung injury (EVALI) has caused more
radiographic, and bronchoscopic
than 2800 illnesses and 68 deaths in the United States. Better characterization of this novel illness is
findings and clinical outcomes of
needed to inform diagnosis and management.
e-cigarette, or vaping, product
use–associated lung injury (EVALI)?
OBJECTIVE To describe the clinical features, bronchoscopic findings, imaging patterns, and
outcomes of EVALI. Findings This case series of 31 patients
found that EVALI typically presented as
DESIGN, SETTING, AND PARTICIPANTS This case series of 31 adult patients diagnosed with EVALI a flu-like illness with elevated
between June 24 and December 10, 2019, took place at an academic medical center in Salt Lake inflammatory markers and an organizing
City, Utah. pneumonia pattern on computed
tomography imaging. Bronchoscopy
EXPOSURES e-Cigarette use, also known as vaping. showed lipid-laden macrophages and
had a high rate of false-positive results
MAIN OUTCOMES AND MEASURES Symptoms, laboratory findings, bronchoscopic results, for infection.
imaging patterns, and clinical outcomes.
Meaning The findings of this study
suggest that EVALI has a characteristic
RESULTS Data from 31 patients (median [interquartile range] age, 24 [21-31] years) were included in
clinical and radiographic presentation
the study. Patients were primarily men (24 [77%]) and White individuals (27 [87%]) who used
and that bronchoscopy has limited
e-cigarette products containing tetrahydrocannabinol (THC) (29 [94%]). Patients presented with
utility in its evaluation.
respiratory (30 [97%]), constitutional (28 [90%]), and gastrointestinal (28 [90%]) symptoms.
Serum inflammatory markers were elevated in all patients. Bronchoscopy was performed in 23 of 28
inpatients (82%) and bronchoalveolar lavage (BAL) revealed the presence of lipid-laden + Invited Commentary
macrophages (LLMs) in 22 of 24 cases (91%). BAL samples tested positive for Pneumocystis jirovecii
(3 patients [13%]), rhinovirus (2 patients [8%]), human metapneumovirus and Aspergillus (1 patient
+ Supplemental content
Author affiliations and article information are
each [4%]); all except human metapneumovirus were determined to be false-positives or clinically
listed at the end of this article.
inconsequential. The exclusive or dominant computed tomography (CT) pattern was organizing
pneumonia in 23 of 26 cases (89%). Patients received antibiotics (26 [84%]) and corticosteroids (24
[77%]), and all survived; 20 patients (65%) seen in follow-up showed marked improvement, but
residual symptoms (13 [65%]), radiographic opacities (8 [40%]), and abnormal pulmonary function
tests (8 of 18 [44%]) were common.
CONCLUSIONS AND RELEVANCE In this case series, patients with EVALI characteristically
presented with a flu-like illness with elevated inflammatory markers, LLMs on BAL samples, and an
organizing pneumonia pattern on CT imaging. Bronchoscopic testing for infection had a high
incidence of false-positive results. Patients had substantial residual abnormal results at early
(continued)
Open Access. This is an open access article distributed under the terms of the CC-BY License.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 1/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
Abstract (continued)
follow-up. These data suggest a limited role for bronchoscopy in typical presentations of EVALI
without risk factors for alternative diagnoses and the need for careful longitudinal follow-up.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176
Introduction
In early 2019, a flu-like illness associated with the use of e-cigarettes was identified in the United
States.1-5 Since that time, more than 2800 cases of e-cigarette, or vaping, product use–associated
lung injury (EVALI) have been reported to the US Centers for Disease Control and Prevention (CDC),
resulting in at least 68 deaths.6-11 Our understanding of this syndrome is based on 4 large patient
series, which together comprised approximately 315 patients, less detailed CDC data, and some
smaller case series.1,8,12-20 Despite these reports, numerous uncertainties remain, including
information on bronchoscopic findings, characteristic radiographic patterns, and longitudinal
outcomes.
Utah has experienced among the highest per capita EVALI rates in the United States.10,21 The
University of Utah Medical Center (UUMC) is a quaternary care academic medical center in Salt Lake
City, Utah, serving a large referral area. We identified a case of EVALI at UUMC during the final week
of June 2019. Bronchoalveolar lavage (BAL) specimens from this and subsequent patients revealed
the presence of lipid-laden microphages (LLMs), which led to suspicion the illness was a form of
exogenous lipoid pneumonia.2,22 We now know that this is probably inaccurate,13,23-25 but it
prompted a local practice of routine bronchoscopy for patients suspected of having EVALI. As a
result, most of the first 31 patients seen at UUMC underwent bronchoscopy with extensive molecular
and microbiological testing during the first 5 months of the outbreak.
In this article, we describe the presentation, evaluation, and clinical course of patients
diagnosed with EVALI at UUMC. A high rate of bronchoscopy, detailed characterization of imaging
findings by 2 thoracic radiologists, and follow-up data for most patients resolve some of the
remaining uncertainties regarding EVALI and provide a more complete picture of a typical case than
has, to our knowledge, been reported.
Methods
The initial 6 cases of EVALI identified at UUMC were cared for by 1 of the authors (S.K.A., M.M.C.,
S.D.M., L.M.K. C.S.P., S.M.R, or S.J.C.) between June 24 and August 16, 2019, and have been
previously reported2; they are included in this analysis as well. Thereafter, as the magnitude of the
outbreak became apparent, institutional emails and informal communications encouraged clinicians
to admit patients with suspected EVALI to a service staffed by the pulmonary faculty (pulmonary
inpatient or medical intensive care unit [ICU] services, as appropriate) or to contact the pulmonary
services for consultation and arranging outpatient follow-up. An ad hoc vaping clinic was created
within the general pulmonary clinic to facilitate follow-up after discharge and to accommodate
outpatient referrals. In addition, 2 of us (S.K.A. and S.J.C.) acted as liaisons between UUMC and the
Utah Department of Health to report cases and facilitate exchange of information. These processes
assured that few, if any, patients with EVALI were not identified for this report. Only cases reviewed
by 2 of us (S.K.A. and .S.J.C.) and determined to be a confirmed or probable diagnosis of EVALI based
on the CDC case definition (ie, e-cigarette use within 90 days of symptom onset, radiographic
infiltrates, a negative preliminary infectious workup, and no other plausible diagnoses) were
included.18 We stopped including patients when the current analysis was begun on December 10,
2019. Internal review board approval was granted for this case series, and informed consent was
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 2/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
waived because the data were deidentified. This study followed the the reporting guideline for
case series.
One of us (S.J.C.) reviewed each patient’s medical record and abstracted data for presented
variables. Other authors (M.M.C., S.D.M., L.M.K., S.M.R., A.F., and C.S.P.) reviewed data for each
patient to ensure accuracy. Bronchoscopic data were manually extracted for the following variables:
bronchoalveolar fluid cellular count and differential, respiratory virus polymerase chain reaction
(PCR), bacterial and fungal stains and cultures, Aspergillus galactomannan antigen, Legionella by
qualitative PCR, Chlamydia pneumoniae by PCR, and Pneumocystis jirovecii by PCR. Oil red-O stains
were performed on all but 1 BAL; results represent the cytopathologist’s quantification of the
percentage of LLMs observed in each sample according to established local laboratory practices.26
Two thoracic radiologists (H.M. and J.S.) jointly and retrospectively reviewed chest radiographs
and computed tomography (CT) images, classifying (by informal consensus) the latter into 1 or more
of the following previously reported patterns: organizing pneumonia (OP), diffuse alveolar
hemorrhage (DAH), acute lung injury (ALI), acute eosinophilic pneumonia (AEP), hypersensitivity
pneumonitis (HP), and exogenous lipoid pneumonia (ELP).3,26 When applicable, a dominant and
minor pattern were recorded. Images were also assessed for the presence of airway wall thickening
in relation to segmental bronchi.27
Statistical Analysis
Summary and descriptive statistics were calculated using Stata version 15.1 (StataCorp). No
prespecified level of statistical significance was set.
Results
Baseline Characteristics
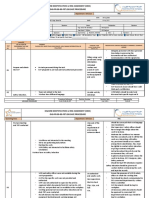
Table 1 shows the demographic characteristics, vaping exposures, and clinical characteristics of the
31 patients. Most were White individuals (27 [87%]) and men (24 [77%]), with a median
(interquartile range [IQR]) age of 24 (21-31) years. Most (29 [94%]) reported vaping
tetrahydrocannabinol (THC) either alone (12 [39%]) or in combination or alternation with nicotine (17
[55%]). Frequency of THC vaping was difficult to quantify due to a number of factors, including
variable qualities of vaping histories obtained, patients omitting or underreporting actual usage due
to the use of illicit substances, and a range of usage frequencies reported, such as a few times per day
to almost continuous use. Few patients reported changes in the frequency of their vaping temporally
related to their illness; however, many did report subjective changes they noticed in the quality of
the products they were using, be it taste or even visual assessment of the viscosity of the liquid. All
patients presented with at least 1 symptom from the following categories: respiratory (30 [97%]),
constitutional (28 [90%]), or gastrointestinal (28 [90%]); 24 (77%) had symptoms from all these
categories. The most common individual symptoms within each category were dyspnea (30 [97%])
and cough (25 [81%]); fever (28 [90%]) and chills (20 [65%]); and nausea (27 [87%]) and vomiting
(24 [77%]).
Laboratory Findings
Laboratory and bronchoscopic findings are summarized in Table 2. Most patients (28 [90%]) had a
mild peripheral leukocytosis with a median (IQR) white blood cell count of 15 300/μL (12 300/μL-
17 900/μL [to convert to ×109 per microliter, multiply by 0.001]) and a granulocyte predominance
(median [IQR] granulocyte percentage, 90.3% [88.0%-92.4%]). The erythrocyte sedimentation rate
and C-reactive protein levels were elevated in 25 of 26 patients (96%) and 31 patients (100%),
respectively, with median (IQR) values of 75 (42-100) mm/h and 25.8 (18.7-30.2) mg/dL (to convert
to milligrams per liter, multiply by 10), respectively. Overall, 7 of 26 patients (27%) had erythrocyte
sedimentation rate values of at least 100 mm/h. A minority had mild elevations in transaminases, and
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 3/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
hematuria was noted in 8 of 21 urinalysis samples (38%). HIV serologies were negative in all 19
patients for whom this was determined.
Bronchoscopic Features
Among all 31 patients, 24 (77%) underwent bronchoscopy with BAL. Three of the last 4 inpatients
(75%) in the series did not undergo bronchoscopy because by mid-November we had stopped
performing routine bronchoscopy; the final patient had bronchoscopy because of recurrent
symptoms resulting in readmission. The cytologic differential from BAL fluid showed a predominance
of macrophages (median [IQR], 53% [33%-79%]) followed by neutrophils (median [IQR], 28%
Table 1. Demographic Characteristics and Presenting Symptoms
Patients, No. (%)
Characteristic (N = 31)a
Age, median (IQR), y 24 (21-31)
Men 24 (77)
Ethnicity
Not Hispanic or Latino 24 (77)
Hispanic or Latino 7 (23)
Race
White 27 (87)
Native Hawaiian or other Pacific Islander 1 (3)
Unknown or not reported 3 (10)
Tobacco use
Current 8 (26)
Former 9 (29)
Never 14 (45)
Cigarette packs per day, median (IQR) 0.2 (0.1-1.0)
Years smoked, median (IQR)b 4 (2-15)
Type of e-cigarette
Nicotine 2 (7)
Marijuana or THC 12 (39)
THC and nicotine 17 (55)
No THC or nicotine 0
Time since starting vaping, median (IQR), mo 12 (3-24)
Presenting symptoms
Any constitutional, respiratory, or gastrointestinal 31 (100)
symptom
≥1 constitutional, respiratory, and gastrointestinal 24 (77)
symptom
Any constitutional symptom 28 (90)
Fever 28 (90)
Chills 20 (65)
Night sweats 13 (42)
Any respiratory symptom 30 (97)
Cough 25 (81)
Shortness of breath 30 (97)
Chest pain 17 (55)
Any gastrointestinal symptom 28 (90)
Nausea 27 (87)
Vomiting 24 (77)
Abdominal pain 10 (32)
Diarrhea 10 (32)
Abbreviations: IQR, interquartile range; THC, tetrahydrocannabinol.
a
Percentages may not sum to 100 due to rounding.
b
Data on years smoked available for 8 patients.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 4/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
[12%-48%]). Oil red-O staining was performed on 23 samples, and LLMs were present in 21 patients
(91%). The median (IQR) proportion of macrophages that stained positive with Oil red-O was 52%
(33%-76%).
Evaluation for Infection
Testing of BAL and noninvasively obtained samples for evidence of infection revealed 1 case (4%) of
human metapneumovirus, which was thought to be coincident with EVALI.28-30 This patient had a
Table 2. Laboratory Studies on Initial Presentation
Laboratory study Median (IQR)
White blood cell count, /μL 15 300 (12 300-17 900)
Differential, median (IQR), %
Granulocytes 90.3 (88.0-92.4)
Lymphocytes 5.7 (4.2-7.9)
Monocytes 2.4 (2-3.2)
Basophils 0.2 (0.1-0.3)
Eosinophils 0.3 (0.1-0.9)
ESR, mm/h 75 (42-100)
CRP, mg/dL 25.8 (18.7-30.2)
Elevated, No./total No. (%)
ESRa 25/26 (96)
CRPb 27/27 (100)
ESR or CRP 28/28 (100)
ESR >100 mm/h 7/26 (27)
Procalcitonin, ng/mL 0.3 (0.1-0.7)
Creatinine, mg/dL 0.85 (0.73-0.94)
Total bilirubin, mg/dL 1.0 (0.6-1.4)
AST, U/L 31 (25-37)
ALT, U/L 24 (18-39)
Elevated, No./total No. (%)
ASTc 6/30 (20)
ALTd 5/30 (17)
AST or ALT 7/30 (23)
Alkaline phosphatase, U/L 85 (72-114)
HIV 1, 2 antigen or antibody
Negative, No./total No. (%) 19/19 (100)
BAL performed, No./total No. (%) 24/31 (77)
Cytologic differential, % Abbreviations: ALT, alanine aminotransferase; AST,
Macrophages 53 (33-79) aspartate aminotransferase; BAL, bronchoalveolar
lavage; CRP, C-reactive protein; ESR, erythrocyte
Neutrophils 28 (12-48)
sedimentation rate; IQR, interquartile range; LLM,
Lymphocytes 6 (2-12)
lipid-laden microphage.
Eosinophils 0 (0-2)
SI conversion factors: To convert AST, ALT, and alkaline
Presence of LLMs, No./total No. (%)e 21/23 (91) phosphatase to microkatals per liter, multiply by
LLMs, median (IQR), % 52 (33-76) 0.0167; creatinine to micromoles per liter, multiply by
Urine drug screen, No./total No. (%) 76.25; CRP to milligrams per liter, multiply by 10; total
bilirubin to micromoles per liter, multiply by 17.104;
Marijuana 11/11 (100)
and white blood cell count to ×109/μL, multiply
Cocaine 0/11
by 0.001.
Heroin 0/1 a
Greater than upper reference limit (20 mm/h).
Methamphetamine 1/11 (9) b
Greater than upper reference limit (0.8 mg/dL).
Narcotics 2/11 (18) c
Greater than upper reference limit (40 U/L).
Benzodiazepine 0/11 d
Greater than upper reference limit (60 U/L).
Methadone 0/11
e
One patient who underwent BAL did not have LLM
Buprenorphine 0/11
testing performed.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 5/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
prolonged course, with a hospital stay of 21 days, including 14 days in the ICU receiving oxygen via
high flow nasal cannula. Two patients (8%) had rhinovirus on PCR testing of BAL fluid.28,29,31 Three
samples (13%) had positive PCR assays for Pneumocystis jirovecii that were considered false-positives
because Pneumocystis direct fluorescence antibodies were negative and the patients recovered
without treatment for Pneumocystis. One BAL culture (4%) had growth of Aspergillus nidulans,
which was deemed a commensal organism or contaminant and not treated; this patient also
recovered. Finally, 1 patient (4%) had intermediate positive acute serologies (immunoglobin M) for
Mycoplasma pneumoniae. In addition to corticosteroids, he was treated with ceftriaxone and
azithromycin, but they were discontinued after 2 days when the diagnosis of EVALI was made, and
he recovered.
Imaging
Chest radiography revealed multifocal, multilobar opacities, variable in extent and distribution,
consistent with foci of alveolar consolidation. Twenty-six patients (84%) underwent CT scanning
(Table 3). eFigure 1 in the Supplement shows examples of the major patterns seen on CT imaging.
The OP pattern was the sole pattern in 18 examinations (69%) and the dominant pattern in 5 (19%).
The HP pattern was the dominant pattern in 2 examinations (8%). The AEP pattern was dominant
in 1 examination (4%). The ELP pattern was nondominant in 1 examination (4%), and the ALI pattern
was nondominant in 1 examination (4%). No examinations manifested the DAH pattern. Table 4
summarizes major characteristics of each pattern. Subpleural sparing was present in 15 examinations
(58%). Airway wall thickening (eFigure 2 in the Supplement) was present in 21 patients (81%).
Table 3. Computed Tomography Findings
Patients, No. (%)
Pattern (n = 26)a
b
Organizing pneumonia 26 (100)
Pneumonitis
Hypersensitivityc 5 (19)
Acute
Eosinophilicd 1 (4)
Lung injurye 1 (4)
Exogenous lipoid pneumoniae 1 (4)
Diffuse alveolar hemorrhage 0
Subpleural sparing
Yes 10 (39)
Some 5 (19)
Anyf 15 (58)
No 11 (42)
Airway wall thickening
Yes 21 (81)
No 5 (19)
a
Percentages may not sum to 100 due to rounding. Totals and percentages for
all patterns sum to greater than 26 and 100%, respectively, because some
examinations were classified as having more than 1 pattern.
b
Organizing pneumonia was the sole pattern in 18 examinations and the
dominant pattern in 5 examinations.
c
Hypersensitivity pneumonitis was the dominant pattern in 2 examinations.
d
Dominant pattern.
e
Nondominant pattern.
f
Any subpleural sparing includes patients in the yes and some categories.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 6/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
Management
Most patients (28 [90%]) were admitted to the hospital, and 8 (268%) were treated in the ICU
(Table 5). The median (IQR) hospital stay was 4 (3-7) days, with a range of 1 to 21 days, highlighting
the variability in illness severity and response to treatment. Most patients (27 [87%]) required
supplemental oxygen: 5 patients (16%) required supplemental oxygen delivered by high flow nasal
cannula, 3 (10%) required mechanical ventilation, and 1 (3%) was supported with venovenous
extracorporeal membrane oxygenation. Most were treated with antibiotics (26 [84%]) and
Table 4. Computed Tomography Classification Scheme Used to Establish Joint Consensus by the 2 Radiologists
Patterna Method of classification
Organizing pneumonia Peripheral or perilobular patchy bilateral GGOs or consolidation; reverse halo sign;
atoll sign
Hypersensitivity pneumonitis Upper-lung or midlung predominant GGOs; centrilobular nodules; air trapping
Acute eosinophilic pneumonia Bilateral and symmetric GGOs or consolidation; pleural effusions; septal thickening
Acute lung injury Acute phase: heterogenous consolidation; GGOs; crazy-paving dependent
distribution; organizing phase: development of reticulation and traction
bronchiectasis
Diffuse alveolar hemorrhage Centrilobular nodules; GGOs; consolidation; subpleural sparing
Exogenous lipoid pneumonia Dependent distribution; GGOs; consolidation; crazy-paving; macroscopic fat
attenuation, ≤30 HU
Abbreviations: GGOs, ground glass opacities; HU,
Giant cell interstitial pneumonia GGOs; architectural distortion; peribronchiolar linear opacities
Hounsfield units.
Airway wall thickening Qualitative visual analysis a
Adapted from Henry TS et al, 2019.26
Table 5. Treatment and Outcomes
Patients, No. (%)
Treatment or outcome (N = 31)a
Admitted
Hospital 28 (90)
ICU 8 (26)
Hospital length of stay, median (IQR), d 4 (3-7)
Highest respiratory support
Room air 4 (13)
Nasal cannula 19 (61)
High flow nasal cannula 5 (16)
Noninvasive positive pressure ventilation 0
Mechanical ventilation 2 (7)
Extracorporeal membranous oxygenationb 1 (3)
Treatment
Steroids 24 (77)
IV methylprednisolone 16 (52)
Starting daily dose, median (IQR), mgc 60 (60-156)
Planned duration, median (IQR), d 7 (1-15)
Antibiotics 26 (84)
Pulmonary function tests at follow-up, median (IQR)
Predicted FEV1, % 92 (83-104)
Predicted FVC, % 99 (93-107)
FEV1/FVC 84 (75-86)
Predicted DLCO, % 76 (64-83)
Abbreviations: DLCO, diffusing capacity for carbon monoxide; FEV1, forced
expiratory volume in 1 second; FVC, forced vital capacity; ICU, intensive care
unit; IQR, interquartile range; IV, intravenous.
a
Percentages may not sum to 100 due to rounding.
b
One patient was supported with venovenous extracorporeal membranous
oxygenation.
c
Doses expressed in milligram equivalents of prednisone.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 7/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
corticosteroids (24 [77%]). Corticosteroid regimens were variable but tended to consist of 40 to 60
mg of prednisone daily with a duration ranging from a few days to 2 weeks. Slightly more than
one-third of patients (11 [36%]) were discharged while still receiving supplemental oxygen.
Readmissions
Two patients (6%) were rehospitalized after discharge. One (3%) was not initially treated with
corticosteroids after a single dose of prednisone induced a manic reaction. After discharge, he
resumed vaping THC and was readmitted with new lung opacities, a new subpleural cystic space in
the right middle lobe, a contiguous pneumothorax, and pneumomediastinum, the last attributed to
the Macklin phenomenon. He improved with chest tube drainage and reinstitution of corticosteroids.
The other patient was discharged with a 5-day course of prednisone but did not complete it. He was
rehospitalized 3 days later with worsening hypoxemia and progressive pulmonary opacities.
Corticosteroids were reinstituted, and he improved with continued supportive care.
Follow-up
All patients survived, and 20 patients (65%) were seen in follow-up. Median (IQR) time to follow-up
after hospital discharge was 16 (11-28) days, and at the time of follow-up, no patients required
supplemental oxygen. Ten patients (50%) had follow-up chest radiographs, which were either
normal or demonstrated near complete resolution of opacities. Pulmonary function tests were
performed in 18 patients (85%) and demonstrated normal spirometry (median [IQR] percentage of
forced vital capacity exhaled in first second [FEV1/FVC], 83.5% [75.3%-86.0%], median [IQR]
predicted FVC, 99.0% [93.3%-106.5%], and median [IQR] predicted FEV1, 92.0% [82.8%-103.8%])
but mildly reduced predicted diffusion capacity (median [IQR], 76% [64%-83%]). All patients
improved, but residual symptoms were common, with 13 (65%) reporting shortness of breath, 9
(45%) reporting cough, and 2 (10%) reporting chest pain. Small numbers of patients continued to
report nausea and vomiting (2 [10%]), fatigue (2 [10%]), night sweats (1 [5%]), and weight loss (1
[5%]). Seven patients (35%) had no residual symptoms at the time of follow-up.
Discussion
We report a retrospective series of cases of EVALI, an emergent flu-like respiratory illness with the
potential for high morbidity and mortality,11 seen at the University of Utah during the height of the
epidemic in 2019. Our patients were evaluated and managed at an academic medical center using a
relatively uniform and comprehensive diagnostic strategy with high rates of bronchoscopy and chest
CT imaging as well as a substantial early follow-up rate. Thus, this series complements but extends
data from previous reports and enhances our understanding of this novel disease.
Our findings confirm those of previous series by showing that EVALI presents as a flu-like illness
with respiratory, constitutional, and gastrointestinal symptoms as well as elevated serum
inflammatory markers. However, more patients in previous series were treated in an ICU and fewer
underwent bronchoscopy. In the seminal series by Layden et al,1 52 of 98 patients (53%) were cared
for in an ICU, and 43 patients (44%) underwent bronchoscopy. In the series by Blagev et al,12 33 of
60 patients (55%) were admitted to an ICU, and 19 patients (32%) underwent bronchoscopy. More
recent additions to the literature, including those by Zou et al,20 Henzerling et al,14 and MacMurdo
et al,16 demonstrated similar ICU admission rates (range, 46%-47%) and bronchoscopy rates (range,
19%-47%). By comparison, only 8 (26%) of our patients were treated in an ICU, and a much larger
proportion of all patients (22 [77%]) underwent bronchoscopy. The reason for the lower rate of ICU
admission in our series is not readily apparent but may reflect a lower severity of illness or different
thresholds for ICU utilization. Of note, the demographic characteristics of our cohort are comparable
to other series1,12,14-16,20 in that they are comprised largely of young, White men who frequently use
THC products, with substantial psychiatric comorbidity rates. This argues against underlying
demographic dissimilarities as the cause of lower ICU admissions.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 8/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
There are several reasons for the high rate of bronchoscopy in our series. First, before EVALI
became a well-recognized clinical entity, bronchoscopy was performed as part of a general diagnostic
survey for infection, diffuse alveolar hemorrhage, acute eosinophilic pneumonia, and so on.32-35
Second, the consistent identification of LLMs in BAL specimens reinforced this practice. Finally, we
used bronchoscopy as the most sensitive means of excluding alternative diagnoses and reducing
diagnostic uncertainty given that EVALI was considered a diagnosis of exclusion.33,36
Similar to previous series and case reports, we found LLMs in most cytological samples from
BAL fluid.1,4,12,13,17 LLMs are a nonspecific cytopathological finding that are observed in a raft of
diseases including lipoid pneumonia, amiodarone toxicity, and aspiration.22,25,37 It is unknown
whether LLMs are a marker of EVALI, a marker of vaping, or a marker of vaping products that contain
the causative agent of EVALI.13,17,23,24 Future studies are needed to determine whether LLMs are
useful in the diagnosis of EVALI. Our data show only that they are typically present.
Current clinical guidance is undecided regarding the role of bronchoscopy in the evaluation of
patients with suspected or possible EVALI and emphasizes the role of clinical discretion in individual
cases.1,12,38,39 Our data show that in suspected cases of EVALI during the apogee of the epidemic,
bronchoscopy rarely contributed meaningfully to diagnosis. This suggests that in the absence of risk
factors for or symptoms of a specific infectious or other alternative diagnosis, bronchoscopy is not
routinely necessary, as has been argued by other authors.16 There were no complications of
bronchoscopy in our patients, but a recent article reported a high rate of adverse events among
younger patients, further arguing for limiting the use of bronchoscopy in typical cases of EVALI.40
Our finding of 3 false-positive PCR results for Pneumocystis jirovecii may be surprising to some
readers. The most stringent, criterion standard for a diagnosis of Pneumocystis pneumonia
incorporates longitudinal evaluation of clinical and radiographic data as well as response to treatment
or lack thereof. Using that standard, the specificity of PCR testing for Pneumocystis is on the order of
80% to 90%,41,42 meaning that in persons without clinical Pneumocystis disease, 10% to 20% will
have the organism detected by PCR due to colonization rather than infection. When a test with this
level of specificity is used in a low prevalence population (such as ours, lacking risk factors for
Pneumocystis pneumonia), most positive tests will be false-positives, as dictated by Bayes theorem.
Failure to incorporate information regarding disease prevalence into diagnostic estimates has been
termed base rate neglect,43 and it may go undetected in clinical practice if all positive PCR results are
presumed to represent clinical illness and are treated for Pneumocystis pneumonia.44 Our series, by
happenstance alone, buttresses these general principles of diagnostic reasoning because our
patients were not treated and all improved, confirming that the PCR results were false-positives.
A wide array of patterns of injury on CT imaging have been reported in EVALI.3,26,37,45,46 Our
series is among the first to document the variability of imaging patterns within a cohort. Most
patients had the OP pattern as the exclusive finding, a feature witnessed to a high degree in other
studies.16 The prototypical OP pattern comprises multifocal, multilobar, ground glass opacities, often
contiguous with uninvolved pulmonary lobules, and sometimes with sparing of the peripheral,
subpleural lung. We caution that this very prevalent imaging pattern does not predict pathologic
findings in the lung. None of our patients had biopsies, but 1 report of 8 patients with EVALI showed
OP on histopathological examination of biopsy specimens in just 4 cases (50%).17
All patients in our series had good outcomes, although nearly two-thirds had residual symptoms
at follow-up. These symptoms as well as normal spirometry and abnormal diffusion capacity testing
align with the findings in previous series.12,15,20 Because EVALI has substantial overlap with other
causes of acute lung injury, it may have a similar natural history and result in residual respiratory
morbidity on long-term follow-up.47,48 Follow-up CT imaging may be useful for reticular changes as
well as quantitative evaluation of potential airway disease in patients with normal spirometry, as
demonstrated in a large research study in obstructive lung disease.27 Longitudinal evaluation of
symptoms and pulmonary function are also needed to better understand the natural history and
long-term prognosis of EVALI.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 9/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
Limitations
This retrospective case series has all the limitations inherent in uncontrolled, observational data. Not
all variables were present for every patient due to variations in care between clinicians. We may have
missed cases of EVALI that were not brought to our attention or where the diagnosis of EVALI was
missed. Some of our patients may have had pneumonia with negative diagnostic testing and
improved with antibiotics and corticosteroids, so they were falsely identified as cases of EVALI. Our
assessment of LLMs relied on a semiquantitative and nonstandardized assessment by the examining
cytopathologist, intended for clinical use, not research. Our radiologists were not masked to the
presumed diagnosis of EVALI when they jointly arrived at an informal consensus regarding
radiographic patterns. Vaping histories were variable and difficult to quantify, as was administration
of corticosteroids. Follow-up data were incomplete. In spite of these unavoidable limitations of
observational research, this series adds meaningful data to the growing body of evidence
regarding EVALI.
Conclusions
EVALI is a serious flu-like respiratory syndrome that mimics infectious pneumonia. In this study,
patients presented with a characteristic but nonspecific constellation of respiratory, constitutional,
and gastrointestinal symptoms as well as elevated serum inflammatory markers. CT imaging typically
revealed an organizing pneumonia pattern. Bronchoscopy typically revealed LLMs but had an
unacceptably high rate of results that were not indicative of true infection. These observations may
help physicians recognize prototypical cases of EVALI, make a provisional clinical diagnosis without
invasive testing, and then assess response to abstinence from vaping with or without corticosteroid
administration. Most patients improve with these measures; however, residual symptoms and
abnormalities on pulmonary imaging and function are present in a significant proportion of patients
at early follow-up. Additional work is needed to determine the long-term prognosis of this novel and
potentially deadly syndrome.
ARTICLE INFORMATION
Accepted for Publication: July 22, 2020.
Published: November 6, 2020. doi:10.1001/jamanetworkopen.2020.19176
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2020 Aberegg SK
et al. JAMA Network Open.
Corresponding Author: Scott K. Aberegg, MD, MPH, Division of Respiratory, Critical Care, and Occupational
Pulmonary Medicine, University of Utah School of Medicine, 26 N 1900 E, Salt Lake City, UT 84112 (scottaberegg@
gmail.com).
Author Affiliations: Division of Pulmonary and Critical Care Medicine, University of Utah Health, Salt Lake City
(Aberegg, Cirulis, Maddock, Freeman, Keenan, Pirozzi, Raman, Callahan); Division of Respiratory, Critical Care, and
Occupational Pulmonary Medicine, University of Utah School of Medicine, Salt Lake City (Aberegg); George E.
Wahlen Department of Veterans Affairs Medical Center, Salt Lake City, Utah (Keenan, Callahan); Department of
Radiology and Imaging Sciences, University of Utah, Salt Lake City (Schroeder, Mann).
Author Contributions: Drs Aberegg and Callahan had full access to all of the data in the study and take
responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Aberegg, Cirulis, Maddock, Keenan, Pirozzi, Raman, Callahan.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Aberegg, Cirulis, Maddock, Freeman, Keenan, Mann, Callahan.
Critical revision of the manuscript for important intellectual content: Aberegg, Cirulis, Maddock, Freeman, Pirozzi,
Raman, Schroeder, Mann, Callahan.
Statistical analysis: Cirulis, Maddock, Callahan.
Administrative, technical, or material support: Schroeder, Callahan.
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 10/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
Supervision: Aberegg, Raman, Callahan.
Conflict of Interest Disclosures: None reported.
REFERENCES:
1. Layden JE, Ghinai I, Pray I, et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin—final
report. N Engl J Med. 2020;382(10):903-916. doi:10.1056/NEJMoa1911614
2. Maddock SD, Cirulis MM, Callahan SJ, et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med.
2019;381(15):1488-1489. doi:10.1056/NEJMc1912038
3. Henry TS, Kanne JP, Kligerman SJ. Imaging of vaping-associated lung disease. N Engl J Med. 2019;381(15):
1486-1487. doi:10.1056/NEJMc1911995
4. Davidson K, Brancato A, Heetderks P, et al. Outbreak of electronic-cigarette-associated acute lipoid
pneumonia—North Carolina, July-August 2019. MMWR Morb Mortal Wkly Rep. 2019;68(36):784-786. doi:10.
15585/mmwr.mm6836e1
5. Schier JG, Meiman JG, Layden J, et al; CDC 2019 Lung Injury Response Group. Severe pulmonary disease
associated with electronic-cigarette-product use—interim guidance. MMWR Morb Mortal Wkly Rep. 2019;68(36):
787-790. doi:10.15585/mmwr.mm6836e2
6. Blount BC, Karwowski MP, Shields PG, et al. Vitamin E acetate in bronchoalveolar-lavage fluid associated with
EVALI. N Engl J Med. 2020. 382(8):697-705. doi:10.1056/NEJMoa1916433
7. Chatham-Stephens K, Roguski K, Jang Y, et al; Lung Injury Response Epidemiology/Surveillance Task Force;
Lung Injury Response Clinical Task Force. Characteristics of hospitalized and nonhospitalized patients in a
nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury—United States, November 2019.
MMWR Morb Mortal Wkly Rep. 2019;68(46):1076-1080. doi:10.15585/mmwr.mm6846e1
8. Evans METE, Twentyman E, Click ES, et al; Lung Injury Response Clinical Task Force; Lung Injury Response
Clinical Working Group. Update: interim guidance for health care professionals evaluating and caring for patients
with suspected e-cigarette, or vaping, product use–associated lung injury and for reducing the risk for
rehospitalization and death following hospital discharge—United States, December 2019. MMWR Morb Mortal
Wkly Rep. 2020;68(5152):1189-1194. doi:10.15585/mmwr.mm685152e2
9. Gaub KL, Hallyburton S, Samanic C, et al. Patient characteristics and product use behaviors among persons with
e-cigarette, or vaping, product use-associated lung injury—Indiana, June-October 2019. MMWR Morb Mortal Wkly
Rep. 2019;68(49):1139-1141. doi:10.15585/mmwr.mm6849a3
10. Hswen Y, Brownstein JS. Real-time digital surveillance of vaping-induced pulmonary disease. N Engl J Med.
2019;381(18):1778-1780. doi:10.1056/NEJMc1912818
11. Werner AK, Koumans EH, Chatham-Stephens K, et al; Lung Injury Response Mortality Working Group.
Hospitalizations and deaths associated with EVALI. N Engl J Med. 2020;382(17):1589-1598. doi:10.1056/
NEJMoa1915314
12. Blagev DP, Harris D, Dunn AC, Guidry DW, Grissom CK, Lanspa MJ. Clinical presentation, treatment, and short-
term outcomes of lung injury associated with e-cigarettes or vaping: a prospective observational cohort study.
Lancet. 2019;394(10214):2073-2083. doi:10.1016/S0140-6736(19)32679-0
13. Butt YM, Smith ML, Tazelaar HD, et al. Pathology of vaping-associated lung injury. N Engl J Med. 2019;381(18):
1780-1781. doi:10.1056/NEJMc1913069
14. Heinzerling A, Armatas C, Karmarkar E, et al. Severe lung injury associated with use of e-cigarette, or vaping,
products—California, 2019. JAMA Intern Med. 2020;180(6):1-9. doi:10.1001/jamainternmed.2020.0664
15. Kalininskiy A, Bach CT, Nacca NE, et al. e-Cigarette, or vaping, product use associated lung injury (EVALI): case
series and diagnostic approach. Lancet Respir Med. 2019;7(12):1017-1026. doi:10.1016/S2213-2600(19)30415-1
16. MacMurdo M, Lin C, Saeedan MB, et al. e-Cigarette or vaping product use-associated lung injury: clinical,
radiologic, and pathologic findings of 15 cases. Chest. 2020;157(6):e181-e187. doi:10.1016/j.chest.2020.01.030
17. Mukhopadhyay S, Mehrad M, Dammert P, et al. Lung biopsy findings in severe pulmonary illness associated
with e-cigarette use (vaping). Am J Clin Pathol. 2020;153(1):30-39.
18. Perrine CG, Pickens CM, Boehmer TK, et al; Lung Injury Response Epidemiology/Surveillance Group.
Characteristics of a multistate outbreak of lung injury associated with e-cigarette use, or vaping—United States,
2019. MMWR Morb Mortal Wkly Rep. 2019;68(39):860-864. doi:10.15585/mmwr.mm6839e1
19. Triantafyllou GA, Tiberio PJ, Zou RH, et al. Vaping-associated acute lung injury: a case series. Am J Respir Crit
Care Med. 2019;200(11):1430-1431. doi:10.1164/rccm.201909-1809LE
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 11/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
20. Zou RH, Tiberio PJ, Triantafyllou GA, et al. Clinical characterization of e-cigarette, or vaping, product
use-associated lung injury in 36 patients in Pittsburgh, Pennsylvania. Am J Respir Crit Care Med. 2020;201(10):
1303-1306. doi:10.1164/rccm.202001-0079LE
21. Lewis N, McCaffrey K, Sage K, et al. e-Cigarette use, or vaping, practices and characteristics among persons
with associated lung injury—Utah, April-October 2019. MMWR Morb Mortal Wkly Rep. 2019;68(42):953-956. doi:
10.15585/mmwr.mm6842e1
22. Gondouin A, Manzoni P, Ranfaing E, et al. Exogenous lipid pneumonia: a retrospective multicentre study of 44
cases in France. Eur Respir J. 1996;9(7):1463-1469. doi:10.1183/09031936.96.09071463
23. Gotts JE, Jordt SE, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ. 2019;
366:l5275. doi:10.1136/bmj.l5275
24. Madison MC, Landers CT, Gu BH, et al. Electronic cigarettes disrupt lung lipid homeostasis and innate
immunity independent of nicotine. J Clin Invest. 2019;129(10):4290-4304. doi:10.1172/JCI128531
25. Pambuccian SE. Testing for lipid-laden macrophages in bronchoalveolar lavage fluid to diagnose vaping-
associated pulmonary injury: are we there yet? J Am Soc Cytopathol. 2020;9(1):1-8. doi:10.1016/j.jasc.2019.10.002
26. Henry TS, Kligerman SJ, Raptis CA, Mann H, Sechrist JW, Kanne JP. Imaging findings of vaping-associated lung
injury. AJR Am J Roentgenol. 2020;214(3):498-505. doi:10.2214/AJR.19.22251
27. Woodruff PG, Barr RG, Bleecker E, et al; SPIROMICS Research Group. Clinical significance of symptoms in
smokers with preserved pulmonary function. N Engl J Med. 2016;374(19):1811-1821. doi:10.1056/NEJMoa1505971
28. Jain S, Self WH, Wunderink RG, et al; CDC EPIC Study Team. Community-acquired pneumonia requiring
hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415-427. doi:10.1056/NEJMoa1500245
29. Jennings LC, Anderson TP, Beynon KA, et al. Incidence and characteristics of viral community-acquired
pneumonia in adults. Thorax. 2008;63(1):42-48. doi:10.1136/thx.2006.075077
30. Vidaur L, Totorika I, Montes M, Vicente D, Rello J, Cilla G. Human metapneumovirus as cause of severe
community-acquired pneumonia in adults: insights from a ten-year molecular and epidemiological analysis. Ann
Intensive Care. 2019;9(1):86. doi:10.1186/s13613-019-0559-y
31. Wang K, Xi W, Yang D, et al. Rhinovirus is associated with severe adult community-acquired pneumonia in
China. J Thorac Dis. 2017;9(11):4502-4511. doi:10.21037/jtd.2017.10.107
32. Du Rand IA, Blaikley J, Booton R, et al; British Thoracic Society Bronchoscopy Guideline Group. British Thoracic
Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax. 2013;68(suppl 1):
i1-i44. doi:10.1136/thoraxjnl-2013-203618
33. Meyer KC, Raghu G, Baughman RP, et al; American Thoracic Society Committee on BAL in Interstitial Lung
Disease. An official American Thoracic Society clinical practice guideline: the clinical utility of bronchoalveolar
lavage cellular analysis in interstitial lung disease. Am J Respir Crit Care Med. 2012;185(9):1004-1014. doi:10.1164/
rccm.201202-0320ST
34. Musher DM, Thorner AR. Community-acquired pneumonia. N Engl J Med. 2014;371(17):1619-1628. doi:10.
1056/NEJMra1312885
35. Orlowski HLP, McWilliams S, Mellnick VM, et al. Imaging spectrum of invasive fungal and fungal-like infections.
Radiographics. 2017;37(4):1119-1134. doi:10.1148/rg.2017160110
36. Feinsilver SH, Fein AM, Niederman MS, Schultz DE, Faegenburg DH. Utility of fiberoptic bronchoscopy in
nonresolving pneumonia. Chest. 1990;98(6):1322-1326. doi:10.1378/chest.98.6.1322
37. McCauley L, Markin C, Hosmer D. An unexpected consequence of electronic cigarette use. Chest. 2012;141(4):
1110-1113. doi:10.1378/chest.11-1334
38. Jatlaoui TC, Wiltz JL, Kabbani S, et al; Lung Injury Response Clinical Working Group. Update: interim guidance
for health care providers for managing patients with suspected e-cigarette, or vaping, product use-associated lung
injury—United States, November 2019. MMWR Morb Mortal Wkly Rep. 2019;68(46):1081-1086. doi:10.15585/
mmwr.mm6846e2
39. Siegel DA, Jatlaoui TC, Koumans EH, et al; Lung Injury Response Clinical Working Group; Lung Injury Response
Epidemiology/Surveillance Group. Update: interim guidance for health care providers evaluating and caring for
patients with suspected e-cigarette, or vaping, product use associated lung injury—United States, October 2019.
MMWR Morb Mortal Wkly Rep. 2019;68(41):919-927. doi:10.15585/mmwr.mm6841e3
40. Diaz CD, Carroll BJ, Hemyari A. Pulmonary illness related to e-cigarette Use. N Engl J Med. 2020;382(4):
384-385. doi:10.1056/NEJMc1915111
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 12/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
JAMA Network Open | Pulmonary Medicine Clinical, Bronchoscopic, and Imaging Findings of EVALI
41. Fauchier T, Hasseine L, Gari-Toussaint M, Casanova V, Marty PM, Pomares C. Detection of Pneumocystis
jirovecii by quantitative PCR to differentiate colonization and pneumonia in immunocompromised HIV-positive
and HIV-negative patients. J Clin Microbiol. 2016;54(6):1487-1495. doi:10.1128/JCM.03174-15
42. Perret T, Kritikos A, Hauser PM, et al. Ability of quantitative PCR to discriminate Pneumocystis jirovecii
pneumonia from colonization. J Med Microbiol. 2020;69(5):705-711. doi:10.1099/jmm.0.001190
43. Bar-Hillel M. The base rate fallacy in probability judgments. Acta Psychologica. 1980;44(3):211-233. doi:10.1016/
0001-6918(80)90046-3
44. Bushyhead JB, Christensen-Szalanski JJ. Feedback and the illusion of validity in a medical clinic. Med Decis
Making. 1981;1(2):115-123. doi:10.1177/0272989X8100100203
45. Khan MS, Khateeb F, Akhtar J, et al. Organizing pneumonia related to electronic cigarette use: a case report
and review of literature. Clin Respir J. 2018;12(3):1295-1299. doi:10.1111/crj.12775
46. Sommerfeld CG, Weiner DJ, Nowalk A, Larkin A. Hypersensitivity pneumonitis and acute respiratory distress
syndrome from e-cigarette use. Pediatrics. 2018;141(6):e20163927. doi:10.1542/peds.2016-3927
47. Herridge MS, Tansey CM, Matté A, et al; Canadian Critical Care Trials Group. Functional disability 5 years after
acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293-1304. doi:10.1056/NEJMoa1011802
48. Orme J Jr, Romney JS, Hopkins RO, et al. Pulmonary function and health-related quality of life in survivors of
acute respiratory distress syndrome. Am J Respir Crit Care Med. 2003;167(5):690-694. doi:10.1164/rccm.
200206-542OC
SUPPLEMENT.
eFigure 1. CT Imaging in 5 EVALI Cases
eFigure 2. Airway Wall Thickening in Right Upper Lobe in 2 Patients
JAMA Network Open. 2020;3(11):e2019176. doi:10.1001/jamanetworkopen.2020.19176 (Reprinted) November 6, 2020 13/13
Downloaded From: https://jamanetwork.com/ on 11/08/2021
You might also like
- Nurse's Role and Responsibilities in Administration of MedicationDocument88 pagesNurse's Role and Responsibilities in Administration of MedicationSonia Singh88% (34)
- List of Orthopedic BooksDocument16 pagesList of Orthopedic BooksAmit Maurya100% (1)
- Community-Acquired Pneumonia in The Emergency DepartmentDocument7 pagesCommunity-Acquired Pneumonia in The Emergency DepartmentpachomdNo ratings yet
- 1 s2.0 S1198743X18308565 MainDocument6 pages1 s2.0 S1198743X18308565 MainYulia Niswatul FauziyahNo ratings yet
- Clinicopathological Characteristics of 8697 Patients With COVID-19 in China A Meta-AnalysisDocument11 pagesClinicopathological Characteristics of 8697 Patients With COVID-19 in China A Meta-AnalysisBenaya PhNo ratings yet
- Film Array PDFDocument10 pagesFilm Array PDFW Antonio Rivera MartínezNo ratings yet
- Validacion CPISDocument5 pagesValidacion CPISXavier AbrilNo ratings yet
- Bronchoscopic Procedures During COVID-19 PandemicDocument8 pagesBronchoscopic Procedures During COVID-19 PandemicwantoNo ratings yet
- 2021 Nac EscmiDocument10 pages2021 Nac EscmiJesus PlanellesNo ratings yet
- 209 Full PDFDocument8 pages209 Full PDFAngga PratamaNo ratings yet
- Pi Is 0954611123001932Document5 pagesPi Is 0954611123001932Angela Fonseca LatinoNo ratings yet
- PIIS2214109X23001353Document14 pagesPIIS2214109X23001353Joaquin OlivaresNo ratings yet
- Neumonia Asociado A Servicios de La SaludDocument7 pagesNeumonia Asociado A Servicios de La SaludOscarNo ratings yet
- The Pulmonary Sequalae in Discharged Patients With COVID-19: A Short-Term Observational StudyDocument7 pagesThe Pulmonary Sequalae in Discharged Patients With COVID-19: A Short-Term Observational StudyCloud NeilalungNo ratings yet
- Tracheotomy in COVID-19 Patients: A Systematic Review and Meta-Analysis of Weaning, Decannulation, and SurvivalDocument8 pagesTracheotomy in COVID-19 Patients: A Systematic Review and Meta-Analysis of Weaning, Decannulation, and SurvivalSebastián Contreras CubillosNo ratings yet
- Jurnal 2Document10 pagesJurnal 2GFORCE .ID.No ratings yet
- Clinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency DepartmentDocument5 pagesClinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency Departmentnavali rahmaNo ratings yet
- Biomarkers and Outcomes of COVID-19 Hospitalisations: Systematic Review and Meta-AnalysisDocument12 pagesBiomarkers and Outcomes of COVID-19 Hospitalisations: Systematic Review and Meta-AnalysisPedro Luz da RosaNo ratings yet
- Chest X Ray in CAPDocument7 pagesChest X Ray in CAPsahatmanurungNo ratings yet
- The Role of Physical Examination in Establishing The Diagnosis of PneumoniaDocument4 pagesThe Role of Physical Examination in Establishing The Diagnosis of PneumoniaCarlos GuiterizNo ratings yet
- Telehealth Model in Improving Health Service During COVID-19 PandemicDocument8 pagesTelehealth Model in Improving Health Service During COVID-19 Pandemicnur arifahNo ratings yet
- 1 s2.0 S1743919115013953 MainDocument11 pages1 s2.0 S1743919115013953 MainMita AdrianiNo ratings yet
- Ficha 5Document12 pagesFicha 5mariaNo ratings yet
- Clinical Microbiology and Infection: Research NoteDocument4 pagesClinical Microbiology and Infection: Research NoteNoorNo ratings yet
- PAVM em Terapia IntensivaDocument10 pagesPAVM em Terapia IntensivaVictor Hugo SilveiraNo ratings yet
- Global Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19Document14 pagesGlobal Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19Tao ShenNo ratings yet
- 2007 Diagnostic Strategies in Nosocomial PneumoniaDocument6 pages2007 Diagnostic Strategies in Nosocomial PneumoniaIvana Daniela BelloNo ratings yet
- 1 s2.0 S0954611123003153 MainDocument8 pages1 s2.0 S0954611123003153 MainEducation serviceNo ratings yet
- Evaluation of The Biofire Filmarray Pneumonia Panel Plus For Lower Respiratory Tract InfectionsDocument11 pagesEvaluation of The Biofire Filmarray Pneumonia Panel Plus For Lower Respiratory Tract InfectionsrachelNo ratings yet
- Machine Learning Automatically Detects Covid-19 Using Chest Cts in A Large Multicenter CohortDocument27 pagesMachine Learning Automatically Detects Covid-19 Using Chest Cts in A Large Multicenter CohortballechaseNo ratings yet
- Epistimologi B.inggrisDocument3 pagesEpistimologi B.inggrisbudiNo ratings yet
- Performance of Radiologists in Differentiating COVID-19 From Non-COVID-19 Viral Pneumonia at Chest CTDocument9 pagesPerformance of Radiologists in Differentiating COVID-19 From Non-COVID-19 Viral Pneumonia at Chest CTrishaNo ratings yet
- COVID-19 Infection in Octagenarian Patients: Imaging Aspects and Clinical CorrelationsDocument11 pagesCOVID-19 Infection in Octagenarian Patients: Imaging Aspects and Clinical CorrelationsRila RivandaNo ratings yet
- Procalcitoninandcap PDFDocument10 pagesProcalcitoninandcap PDFmohd zonNo ratings yet
- Cpis - IdsaDocument5 pagesCpis - IdsaChristian Rodriguez BermudezNo ratings yet
- Factors Predicting Mortality in Pulmonary TuberculosisDocument6 pagesFactors Predicting Mortality in Pulmonary TuberculosisCentral Asian StudiesNo ratings yet
- Covid CT Chest Scan Score & SeverityDocument7 pagesCovid CT Chest Scan Score & SeverityMohan DesaiNo ratings yet
- Medical ScienceDocument14 pagesMedical Sciencerppawar_321203003No ratings yet
- Expanded CURB-65: A New Score System Predicts Severity of Community-Acquired Pneumonia With Superior EfficiencyDocument8 pagesExpanded CURB-65: A New Score System Predicts Severity of Community-Acquired Pneumonia With Superior EfficiencyWilliamRayCassidyNo ratings yet
- Comparison of Clinical Characteristics and Performance of Pneumonia Severity Score and CURB-65 Among Younger Adults, Elderly and Very Old SubjectsDocument8 pagesComparison of Clinical Characteristics and Performance of Pneumonia Severity Score and CURB-65 Among Younger Adults, Elderly and Very Old SubjectsUnomoshNo ratings yet
- Diagnosis and Testing in Bronchiolitis: A Systematic ReviewDocument8 pagesDiagnosis and Testing in Bronchiolitis: A Systematic ReviewDaniel IrrazabalNo ratings yet
- GulhanDocument9 pagesGulhanYezekael Sebastian QuintinusNo ratings yet
- Abx Empirica de NacDocument9 pagesAbx Empirica de NacMarcelo Jimenez CruzNo ratings yet
- Prevalence of Clinical Signs Within Reference Ranges Among Hospitalized Patients Prescribed Antibiotics For PneumoniaDocument12 pagesPrevalence of Clinical Signs Within Reference Ranges Among Hospitalized Patients Prescribed Antibiotics For PneumoniaAndres PoloNo ratings yet
- Academic Emergency Medicine - 2020 - Ebell - Accuracy of Signs and Symptoms For The Diagnosis of Community AcquiredDocument14 pagesAcademic Emergency Medicine - 2020 - Ebell - Accuracy of Signs and Symptoms For The Diagnosis of Community AcquiredOnilis RiveraNo ratings yet
- Qin 2010Document8 pagesQin 2010jajajaneinNo ratings yet
- Peerj 1374Document12 pagesPeerj 1374David Restu Prasetia ManikNo ratings yet
- Association Between Smoking Habit and Pulmonary Tuberculosis at Dr. Soetomo General Academic HospitalDocument5 pagesAssociation Between Smoking Habit and Pulmonary Tuberculosis at Dr. Soetomo General Academic HospitalairwanNo ratings yet
- En 13Document8 pagesEn 13Bruna CarvalhoNo ratings yet
- Research Article Review On Diagnosis of COVID-19 From Chest CT Images Using Artificial IntelligenceDocument10 pagesResearch Article Review On Diagnosis of COVID-19 From Chest CT Images Using Artificial IntelligenceKurama Nine TailsNo ratings yet
- 2021 Article 6994Document13 pages2021 Article 6994Syrine BoughzalaNo ratings yet
- Liberation and Mortality Outcomes in Pediatric Long Term Ventilation: A Qualitative Systematic ReviewDocument10 pagesLiberation and Mortality Outcomes in Pediatric Long Term Ventilation: A Qualitative Systematic ReviewmarleeramirezNo ratings yet
- Cytological Analysis of Bronchial Washings in RSUD Pasar MingguDocument8 pagesCytological Analysis of Bronchial Washings in RSUD Pasar MingguReza DigambiroNo ratings yet
- A Prospective, Randomized Study of Ventilator-Associated Pneumonia in Patients Using A Closed vs. Open Suction SystemDocument7 pagesA Prospective, Randomized Study of Ventilator-Associated Pneumonia in Patients Using A Closed vs. Open Suction SystemFebri Nick Daniel SihombingNo ratings yet
- Jurnal 5Document6 pagesJurnal 5Arswendo ValentinoNo ratings yet
- The Accuracy of Ultrasound-Guided Lung Biopsy Pathology andDocument8 pagesThe Accuracy of Ultrasound-Guided Lung Biopsy Pathology andHeru SigitNo ratings yet
- Pooled Analysis of 163 Published Tuberculous Peritonitis Cases From TurkeyDocument7 pagesPooled Analysis of 163 Published Tuberculous Peritonitis Cases From TurkeyDumitru RadulescuNo ratings yet
- Ventilator-Associated Pneumonia in Adults in Developing Countries: A Systematic ReviewDocument8 pagesVentilator-Associated Pneumonia in Adults in Developing Countries: A Systematic Reviewfrisca susdiNo ratings yet
- Neumonia AspirativaDocument9 pagesNeumonia AspirativaMileth GonzalezNo ratings yet
- MKV 046Document5 pagesMKV 046ardhenaNo ratings yet
- Clinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareFrom EverandClinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareNo ratings yet
- Ijerph 19 01164Document15 pagesIjerph 19 01164rest_a2003No ratings yet
- Main 1Document4 pagesMain 1rest_a2003No ratings yet
- 7 Bo I21 y UKi 1 B FVGZ Fvqo 1596767887Document27 pages7 Bo I21 y UKi 1 B FVGZ Fvqo 1596767887rest_a2003No ratings yet
- APSR Newsletter Vol 31-1Document23 pagesAPSR Newsletter Vol 31-1rest_a2003No ratings yet
- 2.prevalence and Impact of - Myocardial InjuryDocument14 pages2.prevalence and Impact of - Myocardial Injuryrest_a2003No ratings yet
- Imunologi ASMA FannieDocument9 pagesImunologi ASMA Fannierest_a2003No ratings yet
- Centers For Disease Control and Prevention's Sexually Transmitted Diseases Infection GuidelinesDocument6 pagesCenters For Disease Control and Prevention's Sexually Transmitted Diseases Infection GuidelinesabhinavrautNo ratings yet
- Community Based Health CareDocument24 pagesCommunity Based Health CarePrashant S Bhosale100% (2)
- Practical Information For Foreign Students: PrefaceDocument36 pagesPractical Information For Foreign Students: PrefacedanielNo ratings yet
- Altered Body TemperatureDocument27 pagesAltered Body TemperatureAnusikta PandaNo ratings yet
- Healthpoint SeptemberDocument4 pagesHealthpoint SeptemberngochasfNo ratings yet
- Module 3 AsepsisDocument14 pagesModule 3 Asepsisjhoyjhoy779No ratings yet
- Beat COVID-19 Situationer #004 (May 1)Document9 pagesBeat COVID-19 Situationer #004 (May 1)Glomarie Alyssa RacelisNo ratings yet
- Evms Critical Care Covid-19 Management ProtocolDocument39 pagesEvms Critical Care Covid-19 Management ProtocolUzletiszemNo ratings yet
- OHS-PR-09-03-F07 JOB SAFE PROCEDURE (01) OHTL Route SurveyDocument13 pagesOHS-PR-09-03-F07 JOB SAFE PROCEDURE (01) OHTL Route Surveymohammed tofiqNo ratings yet
- Dr. Ika Prasetya WijayaDocument31 pagesDr. Ika Prasetya Wijayabidang keperawatanNo ratings yet
- The Hidden Cause of Rhematic ArthiritisDocument12 pagesThe Hidden Cause of Rhematic ArthiritisLeslin BruttusNo ratings yet
- Night Slim Pro Sirath82Document8 pagesNight Slim Pro Sirath82Sirath RazaNo ratings yet
- NURSING CARE PLAN FOR CROHN'sDocument2 pagesNURSING CARE PLAN FOR CROHN'sMuhyeeSalaIdjadNo ratings yet
- Need For Clinical Microbiologists by Dr.T.V.Rao MDDocument2 pagesNeed For Clinical Microbiologists by Dr.T.V.Rao MDtummalapalli venkateswara rao100% (1)
- Case Study PCAPDocument32 pagesCase Study PCAPJohn Paul Andrade100% (1)
- Dengue Fever: Centre For Health Protection, Department of Health July 2019Document17 pagesDengue Fever: Centre For Health Protection, Department of Health July 2019Melissa Marie CustodioNo ratings yet
- Pe 11 Diagnostic Test With Answer KeyDocument7 pagesPe 11 Diagnostic Test With Answer KeyJames LopezNo ratings yet
- Fauci Dossier Valentine S Day Document 2022 (1) SummaryDocument5 pagesFauci Dossier Valentine S Day Document 2022 (1) SummarySherri StreightNo ratings yet
- List of Health Care AcronymsDocument9 pagesList of Health Care AcronymsAsalah AlabedNo ratings yet
- Drug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeDocument5 pagesDrug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeCia TriiNo ratings yet
- Cytotec Drug CardDocument1 pageCytotec Drug CardBenNo ratings yet
- Telemedicine For Healthcare CapabilitiesDocument12 pagesTelemedicine For Healthcare CapabilitiesSandiNo ratings yet
- TuberculosisDocument9 pagesTuberculosissarguss14100% (4)
- Reishimax GLP Us PipDocument3 pagesReishimax GLP Us PipKeith KingNo ratings yet
- Commercial Essential Oils As Potential Antimicrobials To Treat Skin DiseasesDocument92 pagesCommercial Essential Oils As Potential Antimicrobials To Treat Skin DiseasesxiuhtlaltzinNo ratings yet
- Dr. Clay Forsberg, CV - Orange County Plastic SurgeryDocument5 pagesDr. Clay Forsberg, CV - Orange County Plastic SurgeryAnželika NezinamaNo ratings yet
- Beef Blackleg Clostridial DiseasesDocument4 pagesBeef Blackleg Clostridial DiseasesYan Lean DollisonNo ratings yet
- Edu 537 100 Item Rationale Questionnaire With KeyDocument26 pagesEdu 537 100 Item Rationale Questionnaire With KeyGresell Diaz100% (1)