Professional Documents
Culture Documents
Gopi PG - Et.al
Uploaded by
kang.asep008Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gopi PG - Et.al
Uploaded by
kang.asep008Copyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/5491681
Impact of improved treatment success on the prevalence of TB in a rural
community based on active surveillance
Article in The Indian journal of tuberculosis · February 2008
Source: PubMed
CITATIONS READS
8 46
5 authors, including:
Gopi Pg Roshni Subramani
76 PUBLICATIONS 3,316 CITATIONS
Tata Institute of Social Sciences
58 PUBLICATIONS 2,434 CITATIONS
SEE PROFILE
SEE PROFILE
Vedachalam Chandrasekaran Thotttikkamath Santha
Indian Council of Medical Research National Institute for Research in Tuberculosis
74 PUBLICATIONS 3,333 CITATIONS 63 PUBLICATIONS 2,669 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Gopi Pg on 25 July 2017.
The user has requested enhancement of the downloaded file.
Original Article
IMPACT OF IMPROVED TREATMENT SUCCESS ON THE PREVALENCE OF TB IN
A RURAL COMMUNITY BASED ON ACTIVE SURVEILLANCE
P. G. Gopi, R. Subramani, V. Chandrasekaran, T. Santha and P. R. Narayanan
(Original article received on 16.1.2007. Revised on 29.6.2007. Accepted on 11.9.2007)
Summary
Objective: To study the impact of improved treatment outcome of a cohort of patients treated under DOTS strategy
on the prevalence of pulmonary tuberculosis (TB) in the community.
Design: The data from TB register of one Tuberculosis Unit (TU) in Tiruvallur district of Tamilnadu, and two TB
disease surveys conducted in the same area during 1999-2003 were analysed. The successful treatment outcome was
compared to the prevalence of TB in the subsequent cohort.
Results: The proportion of patients who completed treatment successfully was 75.3% in the first cohort period. This
higher proportion of treatment success among patients treated under DOTS in the first cohort period (1999-2001)
compared to the 51-55% reported during SCC, resulted in a lower prevalence of smear-positive cases, irrespective of
culture results observed in the survey conducted during 2001-2003 compared to that in the survey conducted during
1999-2001 (252 vs. 323 per 100,000; annual decline of 9%). Similarly, a decline in culture-positive cases, irrespective
of smear results, was also observed (443 vs. 605; annual decline 11%).
Conclusion: The higher proportion of successful completion of treatment after DOTS implementation was associated
with a substantial decline in the prevalence of TB. These findings showed that we are in the direction towards achieving
the Millennium Development Goals (MDGs). [Indian J Tuberc 2008; 55:22-27]
Key words: TB, DOTS, Cohort, Treatment outcome, Prevalence
INTRODUCTION The key components of DOTS strategy are
political commitment, sputum diagnosis by smear
Tuberculosis (TB) is highly prevalent in microscopy, short course chemotherapy under
India in terms of morbidity and mortality1. It is direct supervision, uninterrupted supply of drugs,
estimated that India accounts for one-fifth of monitoring, recording and evaluation of the
world’s new TB cases. World Health Organization programme. This is an effective and successive
(WHO) declared tuberculosis a global public health programme for the control of the disease.
emergency in 1993 because of the high mortality Tuberculosis Research Centre (TRC) in
rate among adults, its association with HIV collaboration with Government of Tamil Nadu
infection and emergence of Multi-Drug Resistance established a centre in one TU of Tiruvallur district,
(MDR) TB. After the failure of the National Tamil Nadu for DOTS implementation, tuberculosis
Tuberculosis Programme (NTP) as reviewed in control, training and research.
1992, Government of India revised the
tuberculosis control and launched the Directly Government of Tamil Nadu implemented the
Observed Treatment Short course (DOTS) under DOTS strategy in the year 1999 in Tiruvallur district.
the Revised National Tuberculosis Control There are 17 health facilities (HFs) in the study area.
Programme (RNTCP) with the aim of achieving Under the DOTS programme, patients are detected
85% cure among new patients diagnosed to have by symptom screening at this HFs through the
pulmonary tuberculosis and detect at least 70% examinations of three sputum smears for acid-fast
of the cases in the community2. bacilli. All patients diagnosed based on three sputum
Tuberculosis Research Centre, Chennai
Correspondence: Dr. P.R. Narayanan, Director, Tuberculosis Research Centre, Mayor V.R. Ramanathan Road, Chetput, Chennai-600 031;
E-mail: prnarayanan@trcchennai.in
Indian Journal of Tuberculosis
P. G. GOPI ET AL 23
examinations are put on anti-TB treatment. In this community surveys were conducted in Tiruvallur
strategy, smear microscopy is the most efficient district, Tamil Nadu during 1999-2001 and 2001-
means of case detection among those persisting with 2003 to estimate the prevalence of pulmonary TB.
symptoms suggestive of pulmonary tuberculosis Patients who were diagnosed based on smear and/
(cough of three weeks or more with or without other or culture were referred and treated under DOTS
clinical symptoms). All patients diagnosed with as per RNTCP guidelines. From the first survey,
tuberculosis are given directly observed treatment the prevalence of pulmonary TB was estimated to
in accordance with RNTCP policies2. All the smears be 323 per 100, 000 for smear-positive cases and
are stained and examined by Ziehl – Neelson 605 per 100, 000 for culture-positive cases4. These
microscopy for detection of tuberculosis. If the estimates served as the baseline information at the
patient is positive on smear microscopy on at least end of the SCC and start of the DOTS
two specimens and not treated previously for TB implementation.
for more than one month, he is termed as new
sputum smear-positive case and put on Category I This paper describes the treatment outcome
regimen 2(HRZE) 3 /4(HR) 3 (H-isoniazid; R- of a cohort of patients registered under DOTS and
rifampicin; Z=pyrazinamide; E=ethambutol; S- compares with the prevalence of TB as estimated
streptomycin). Numbers before the letters indicates from the disease surveys conducted after the
the duration in months and that in subscript indicates implementation of the DOTS strategy.
the number of times the drug given in each week).
If the patient is sputum smear-positive and treated MATERIAL AND METHODS
for more than a month, he is treated under Category
II regimen 2(HRZES)3 /1(HRZE)3 / 5(HRE)3. Such The study area is a rural population of
patients will be either a relapse case after declaring Tiruvallur district in Tamilnadu where TRC
cure when treated first or failure case or default monitored the DOTS programme for a period of
case. Other sputum smear-negative cases not about six years since its implementation in 1999.
seriously ill, extra pulmonary cases are put on Patients diagnosed at any one of the HFs were treated
Category III regimen 2(HRZ)3 /4(HRE)3. In case, for TB as per the RNTCP guidelines2. TRC has
the smear is positive only on one specimen out of undertaken a series of disease surveys at every two
three specimens examined, the patient is prescribed and-a-half years to measure the epidemiological
for one week antibiotic treatment and reviewed after impact of DOTS implemented from 1999 in
a week with a chest X-ray. If the symptom is still Tiruvallur district. These disease surveys were
persisting, the patient is put on Category III regimen. undertaken in a random sample of 82,000 adults
Intensive phase treatment of patients in categories I aged 15 years or more. The sample size estimated
and II is extended for one month if the smear is for community disease survey was based on an
positive at the end of the intensive phase. Every annual incidence of culture-positive TB of 260 per
dose of treatment is to be directly observed in the 100,000 population, a precision of 20% at 95%
initial intensive phase of treatment and at least the confidence level, with the coverage of examined
first of the three doses is to be directly observed population 9% and a design effect of two. The
during the continuation phase. methodology of survey is explained elsewhere4. In
each survey, all persons in the selected villages/units
Before the implementation of DOTS, the were registered by door-to-door census and all adults
Government of India introduced Short aged >15 years were questioned about chest
Chemotherapy (SCC) on a pilot basis in the District symptoms and underwent chest radiograph (70 mm
Tuberculosis Programme in 18 districts spread over photo-fluorogram posteroanterior view) at a nearby
India. A concurrent cohort analysis of the data centre. For those with an abnormal radiograph
collected from these districts during 1985-1991 suggestive of TB and/or chest symptoms, attempts
showed that the overall treatment completion for were made to collect two sputum specimens. Those
SCC was 51-55% with a case finding of 41%3. Two who were absent for examinations were revisited
Indian Journal of Tuberculosis
24 TREATMENT SUCCESS ON THE PREVALENCE OF TB
the same day or on subsequent days until at least 4. Expired/Died: Patient who died during
90% had the required investigations. The sputum treatment, regardless of cause.
specimens were examined by fluorescence 5. Failure: Smear-positive case who is smear-
microscopy and cultured on Lowenstein-Jensen positive at five months or more after starting
medium. Those yielding growth were subjected to treatment. Also, a patient who was initially
identification tests for Mycobacterium tuberculosis smear-negative but who became smear-
and drug susceptibility tests. A case of tuberculosis positive during treatment.
was defined as a person with a positive smear (>3 6. Transferred out: A patient who has been
acid-fast bacilli) irrespective of culture results. transferred to another TU/District and his/
her treatment results are not known.
The details of all patients started on
treatment in a TU are entered in a register called All new TB patients identified in the two
Tuberculosis Register (TB Register) and these prevalence surveys and treated under DOTS along
patients are monitored in accordance with the with other new smear-positive cases detected from
RNTCP guidelines. This register is maintained by other areas not included in the sample and registered
the Senior Treatment Supervisor (STS). The TB in the TU from May 1999 to June 2001 formed the
Register is the backbone of the DOTS strategy. study population.. The data collected from the study
Every patient put on treatment is registered under a was computerized, edited and corrected for any
specific TB number. A TB patient is known by this discrepancies. The proportion of patients who
number and the year in which he/she was registered. successfully completed the treatment was obtained.
The particulars like name, age, sex, category, type, The potential risk factors for a higher likelihood of
smear result at admission, 2nd /3rd month, 4th /5th default from treatment were identified. The
month and at the end of treatment are the details prevalence of the smear-positive and culture-positive
entered in the TB Register. The treatment outcome cases was estimated from the second survey and
of the patient is an important parameter of the compared to that in the first survey. Chi-square test
programme available in the TB Register. The of significance was used to test the difference in
international definitions were followed to classify proportions. A p value of < 0.05 was considered as
TB patients according to outcome as follows5: statistically significant.
1. Cured: Initially smear-positive patient who RESULTS
has completed treatment and had negative
sputum smears, on at least two occasions,
one of which was at completion of A total of 805 new smear- positive TB
treatment. patients were registered during the above period;
2. Treatment Completed: Sputum smear- successful treatment completion rate was 75.3%
positive case who has completed treatment, and 15.9% had defaulted. The prevalence of TB
with negative smears at the end of the initial (smear-positive cases irrespective of culture results
phase but none at the end of treatment (or) and culture-positive cases irrespective of smear
Sputum smear-negative TB patient who has results) estimated from the first survey and second
received a full course of treatment and has survey is in Table 14. The prevalence of smear-
not become smear-positive during or at the positive cases, irrespective of culture results, was
end of treatment (or) extra-pulmonary TB 252 in the second survey as compared to 323 per
patient who has received a full course of 100,000 in the first survey. The corresponding
treatment and has not become smear- figures for culture-positive cases were 443 and 605
positive during or at the end of treatment. per 100,000 respectively. The annual decline in the
3. Default: A patient who, at any time after prevalence of smear-positive cases from the first
registration, has not taken anti-TB drugs for survey and second survey was estimated to be 9%.
2 months or more consecutively The corresponding figure for culture- positive cases
Indian Journal of Tuberculosis
P. G. GOPI ET AL 25
Table 1: Prevalence of pulmonary tuberculosis (per 100000) in two disease surveys conducted
during 1999-2001 and 2001-2003 in a TU in Tiruvallur district, Tamil Nadu.
Survey (round) Population Smear Culture
positive* positive**
First survey 83390 323 605
(1999-2001)
Second survey 85472 252 443
(2001-2003)
Annual dec line (%) - 9 11
* Irrespective of culture ** irres pect ive of smea r
(P1 - P2) x 100 P1 and P2 are the prevalence at two time
Annual decline (%) = points at an interval of ‘N’ years.
P1 x N
Table 2: Risk factors for default of patients registered during 1999-2001under a DOTS programme
in Tiruvallur district, Tamil Nadu
Factors Number* Default (%) P value
Age <45 358 44 (12.3) P<0.001
>45 376 84 (22.3)
Sex Male 581 114 (19.6) P<0.01
Female 153 14 (9.2)
Education Illiterate 316 56 (17.7) P=0.1
Literate 348 47 (13.5)
Occupation Un-employed 173 32 (18.5) P=0.2
Employed 493 72 (14.6)
Patient’s < 4 weeks 508 78 (15.4) P=0.7
Delay > 4 weeks 136 19 (14.0)
DOTS No 97 19 (19.6) P=0.4
convenient Yes 447 72 (16.1)
Smoking No 350 32 (9.1) P<0.001
Yes 314 71 (22.6)
Alcoholism No 438 40 (9.1) P<0.001
Yes 227 63 (27.8)
DOTS Private 272 44 (16.2) P=0.5
provider Government 394 57 (14.5)
DOTS centre Private 333 60 (18.0) P<0.05
Government 333 41 (12.3)
Supervision- No 203 27 (13.3) P=0.4
during IP Yes 461 74 (16.0)
*Those successfully completed treatment including default
Note: For variables except for sex and age, the number of patients
is less than 734 due to non-availability of all patients at the time
of interview.
Indian Journal of Tuberculosis
26 TREATMENT SUCCESS ON THE PREVALENCE OF TB
was 11%. After the implementation of DOTS during of 9% and 11% for smear-positive and culture-
this cohort period, case detection was about 80% positive cases respectively. The ARTI estimates from
with a cure rate of 75%. This has resulted in a lower the three tuberculin surveys conducted in the same
prevalence of smear-positive as well as culture- area among children aged <10 years during 1999-
positive cases in the subsequent survey (323 to 252 2005 were 1.6%, 1.4% and 1.2% respectively9.
and 605 to 443 per 100,000 respectively). There was a significant decline in the trend of TB
infection (annual decline of 6%). An increase in the
Risk factors for default: The distribution success rate due to the implementation of the
of patients according to those successfully effective DOTS strategy was in association with a
completed the treatment and defaulted is given in substantial reduction in the prevalence of TB and
the Table 2. A uni-variate analysis showed that a infection as demonstrated from the disease and
higher default was significantly associated with tuberculin surveys carried out in the area.
patient’s sex (male), aged < 45 years, smoking,
alcoholism and the DOTS centre (private) where The successful treatment outcome obtained
patients took treatment. A multivariate analysis in our study was less than the national expected
showed that age and alcoholism were the average of 85%. The cure rate was 91% among the
independent risk factors associated with a higher category I patients treated under DOTS in one of
likelihood of default. the chest diseases clinics run by the Municipal
Corporation of Delhi10. The study concluded that
DISCUSSION the cure rate could have been more if tracing of
defaulter had been intensified. Our study had a higher
The Tiruvallur area provides a unique default rate and we identified old age and alcoholism
opportunity to evaluate the TB situation before as the independent risk factors necessitating targeted
and after implementation of DOTS. The health education programme through Information,
epidemiological data generated during the 15 year Education and Communication (IEC) for this group
follow-up of BCG vaccine Trial in this area showed of patients. An earlier report from the same area
that there was no decline in the prevalence of also recommended retrieval action of defaulters in
smear-positive cases over the period 1968-1986 order to increase the successful treatment
(pre-SCC period) 6. Using available information outcome11.
indicated in NTP, the efficiencies were about 30%
for case finding, 35% for case holding, 80% for We have correlated the activities of the
chemotherapy and 50% for relative efficiency (ie. HFs in this area and the programme indicators
the proportion of patients with successful like conversion and cure12. Both were found to be
outcome even without completing their prescribed well correlated indicating that success of the
course of treatment relative to the proportion with DOTS depends on the health function. This
a favourable response at the end of the prescribed emphasizes the need for periodic evaluation of the
course). From these estimates, the success rate functioning of each HF for better management of
was estimated to be only 16% 7 . The three treatment.
tuberculin surveys conducted among children aged
1- 9 years in 1969, 1979 and 1984 in this area CONCLUSION
showed that there was no change in the prevalence
of infection namely, 9.0%, 10.2% and 9.1% and The study showed that an increase in the
the computed ARTI of 1.7%, 1.9% and 1.7% successful treatment outcome of the patients treated
respectively8. under DOTS was associated with substantial decline
in the prevalence of TB in the community. This would
A repeat survey conducted during 2001- be a milestone towards achieving the MDGs of
2003 after the baseline survey (1999-2001) in the reverting and reducing the prevalence of TB by 50%
same population showed that the annual decline was in 2015 related to 1990 levels.
Indian Journal of Tuberculosis
P. G. GOPI ET AL 27
ACKNOWLEDGEMENTS P.R. A baseline survey of the prevalence of
tuberculosis in a community in south India at the
commencement of a DOTS programme. Int J Tuberc
The authors are grateful for the assistance Lung Dis 2003; 7(12): 1154-1162.
and cooperation of the Joint Deputy Director Health 5. World Health Organisation. Revised international
Services of Tiruvallur district, Tamil Nadu and all definitions in tuberculosis control. Int J Tuberc Lung
the medical and paramedical staff, including Dis 2001; 5: 213-215.
6. Tuberculosis Research Centre, Chennai, India.
treatment observers, who participated in this work. Trends in prevalence and incidence of tuberculosis
The authors thank all field workers involved in the in south India. Int J Tuberc Lung Dis 2001; 5:
epidemiological survey, Mr. S. Radhakrishnan (STS) 142-157.
and Mr. E. Prabhakaran (Senior Treatment 7. Radhakrishna S. Direct impact of treatment
programme on totality of tuberculosis patients in
Laboratory Supervisor) for maintaining patient the community. Indian J Tuberc 1988; 35 :
Tuberculosis register. The staff of Epidemiology 110-113.
Unit Statistics and EDP divisions is gratefully 8. Mayuranath S, Vallishayee R S, Radhamani M P,
acknowledged for scrutiny of the data, data entry Prabhakar R. Prevalence study of tuberculosis
infection over fifteen years, in a rural population in
and data management. Lastly, the authors are grateful
Chingleput district (south India). Ind J Med Res 1991;
to all the patients for their cooperation. 93: 74-80.
9. Gopi P.G, Subramani R, Narayanan P.R. Trend in
This work was funded, in part, by a grant the prevalence of TB infection and ARTI after
from the United States Agency for International implementation of a DOTS programme in south
India. Indian J Tuberc 2006; 10: 346-348.
Development provided through the World Health 10. Chadha SL and Bhagi RP. Treatment outcome in
Organization, SEARO, New Delhi. tuberculosis patients placed under directly observed
treatment short course (DOTS)-a cohort study.
REFERENCES Indian J Tuberc 2000; 47: 155.
11. Santha T, Garg R, Frieden TR, Chandrasekaran V,
Subramani R, Gopi PG, Selvakumar N, Ganapathy
1. Dye C, Scheele S, Dolin P, Pathania V, Raviglione M S, Charles N, Rajamma J and Narayanan PR. Risk
C. Global burden of tuberculosis: estimated incidence, factors associated with default, failure and death
prevalence and mortality by country. JAMA 1999; among tuberculosis patients treated in a DOTS
282: 677-686. programme in Tiruvallur District, south India,
2. Khatri G R, Frieden T.R. The status and prospectus 2000. Int J Tuberc Lung Dis 2002; 6(9):
of tuberculosis control in India. Int J Tuberc Lung 780-788.
Dis 2000; 4: 193-200. 12. Gopi PG, Subramani R, Santha T, Radhakrishnan
3. Tuberculosis Research Centre. Seven-year findings S, Chandrasekaran V, Rajeswari R, Balasubramanian
of Short Course Chemotheraphy in 18 districts in R, Thomas A, Miniyandi M and Narayanan PR.
India under district tuberculosis programme. Indian Performance of a DOTS programme:
J Tuberc 1996; 43: 131-142. administrative and technical challenges- a field
4. Gopi P.G, Subramani R, Radhakrishna S, Kolappan report from a district in south India. Indian J
C, Sadacharam C, Devi T.S, Frieden T.R, Narayanan Tuberc 2006; 53: 123-134.
Indian Journal of Tuberculosis
View publication stats
You might also like
- National Health ProgrammesDocument8 pagesNational Health ProgrammesRohit SharmaNo ratings yet
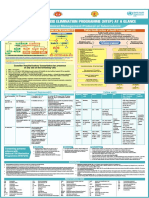
- NTEP at A Glance - Comprehensive Clinical Management Protocol For TBDocument1 pageNTEP at A Glance - Comprehensive Clinical Management Protocol For TBNael NajeebNo ratings yet
- CHC - 2Document15 pagesCHC - 2Babita Dhruw75% (4)
- Primary Health Centre Organization and FunctionsDocument9 pagesPrimary Health Centre Organization and FunctionsKailash NagarNo ratings yet
- Recent TB Treatment GuidelinesDocument28 pagesRecent TB Treatment GuidelinesDr venkatesh jalluNo ratings yet
- Purification Water Large ScaleDocument2 pagesPurification Water Large ScaleSushma RaniNo ratings yet
- Health Related Quality of Life Among TB Patients Q PDFDocument8 pagesHealth Related Quality of Life Among TB Patients Q PDFAmna SaifullahNo ratings yet
- Gopi Et AlDocument8 pagesGopi Et Alkang.asep008No ratings yet
- 2017 Article 4627Document10 pages2017 Article 4627ristaseptiawatiningsihNo ratings yet
- Bta TranslateDocument7 pagesBta TranslateCrysta SoniaNo ratings yet
- Artikel TBDocument8 pagesArtikel TBArryo P SudharyanaNo ratings yet
- A Study of Nutritional Assessment of Newly Diagnos PDFDocument7 pagesA Study of Nutritional Assessment of Newly Diagnos PDFKaushik SahaNo ratings yet
- TB Patient Case StudyDocument8 pagesTB Patient Case StudyprincyNo ratings yet
- 1 s2.0 S0422763815301023 MainDocument4 pages1 s2.0 S0422763815301023 MainEghar EverydayishellNo ratings yet
- National Tuberculosis Control Program: Dr. Kanupriya ChaturvediDocument37 pagesNational Tuberculosis Control Program: Dr. Kanupriya ChaturvediBen JosephNo ratings yet
- Rujukan Peneltian Yag Menggunakan FisherDocument8 pagesRujukan Peneltian Yag Menggunakan FisherDwi YulNo ratings yet
- RNTCP - Wikipedia, The Free EncyclopediaDocument5 pagesRNTCP - Wikipedia, The Free EncyclopediaakurilNo ratings yet
- Arsad Et AlDocument10 pagesArsad Et Alkang.asep008No ratings yet
- Systematic Review Pelaksanaan Programmatic Management of Drug-Resistant Tuberculosis Pada Pasien Tuberkulosis Resistan ObatDocument8 pagesSystematic Review Pelaksanaan Programmatic Management of Drug-Resistant Tuberculosis Pada Pasien Tuberkulosis Resistan ObatAdinda Pramesthi RiadyaniNo ratings yet
- Medi 99 E23649Document6 pagesMedi 99 E23649kornelis aribowoNo ratings yet
- 1030 2752 1 SMDocument7 pages1030 2752 1 SMOlimpius Gunawan HamidNo ratings yet
- ENTDocument9 pagesENTsurendra Prasad GuptaNo ratings yet
- 3373 12999 1 PBDocument8 pages3373 12999 1 PBdzulfiNo ratings yet
- National Tuberculosis ProgramDocument37 pagesNational Tuberculosis ProgramDon Oliveros ÜNo ratings yet
- Abassi Et AlDocument6 pagesAbassi Et Alkang.asep008No ratings yet
- Kruk Et Al-2008-Tropical Medicine & International HealthDocument10 pagesKruk Et Al-2008-Tropical Medicine & International Healthsuci K SariNo ratings yet
- National TB ControlDocument25 pagesNational TB Controlnirmal2444No ratings yet
- Treatment Seeking Behavior and Factors Associated With Its Delay Among Newly Diagnosed Pulmonary Tuberculosis Patients in Bhopal, Madhya PradeshDocument6 pagesTreatment Seeking Behavior and Factors Associated With Its Delay Among Newly Diagnosed Pulmonary Tuberculosis Patients in Bhopal, Madhya PradeshAdvanced Research PublicationsNo ratings yet
- Wabah TBC Di IndiaDocument7 pagesWabah TBC Di IndiaSatya WangsaNo ratings yet
- Life Experiences of Pulmonary Tuberculosis Patients Affected by Delays in Treatment, in ThailandDocument15 pagesLife Experiences of Pulmonary Tuberculosis Patients Affected by Delays in Treatment, in ThailandGlobal Research and Development ServicesNo ratings yet
- Ofx 137Document7 pagesOfx 137Sheila Alcalde RNo ratings yet
- Pengaruh Dinamika Kelompok Sosial Terhadap Angka Kejadian Dan Penyembuhan Penyakit Tuberkulosis Paru Di Wilayah Puskesmas MojorotoDocument8 pagesPengaruh Dinamika Kelompok Sosial Terhadap Angka Kejadian Dan Penyembuhan Penyakit Tuberkulosis Paru Di Wilayah Puskesmas MojorotohompalahompalaNo ratings yet
- Y. NagammanavarDocument22 pagesY. NagammanavarMamta KumariNo ratings yet
- Pone 0198080Document15 pagesPone 0198080kornelis aribowoNo ratings yet
- NTEP or RNTCP (Community Health Nursing)Document37 pagesNTEP or RNTCP (Community Health Nursing)Ankita ShaluNo ratings yet
- ARTIKEL NUR NAILY NISYA Terakhir EditDocument14 pagesARTIKEL NUR NAILY NISYA Terakhir EditNaily NisyaNo ratings yet
- Effect of Standard Tuberculosis Treatment On Plasma Cytokine Levels in Patients With Active Pulmonary TuberculosisDocument13 pagesEffect of Standard Tuberculosis Treatment On Plasma Cytokine Levels in Patients With Active Pulmonary TuberculosisDicky WahyudiNo ratings yet
- MH0040 - Health AdministrationDocument12 pagesMH0040 - Health AdministrationRahul GuptaNo ratings yet
- Peran Pengawas Minum Obat (Pmo) Dalam Keberhasilan Pengobatan Tuberculosis Paru Di Masyarakat (The Role of Direct Observed Treatment in Tuberculosis Treatment Successful at Comm...Document7 pagesPeran Pengawas Minum Obat (Pmo) Dalam Keberhasilan Pengobatan Tuberculosis Paru Di Masyarakat (The Role of Direct Observed Treatment in Tuberculosis Treatment Successful at Comm...petrayohanaNo ratings yet
- Pone 0194087 PDFDocument15 pagesPone 0194087 PDFInekeNo ratings yet
- Fluorescence Microscopy VS Truenat - Which Method Is Better For Diagnosis of Tuberculosis?Document4 pagesFluorescence Microscopy VS Truenat - Which Method Is Better For Diagnosis of Tuberculosis?IJAR JOURNALNo ratings yet
- 1728 3760 1 PB PDFDocument6 pages1728 3760 1 PB PDFTerminal ComputerNo ratings yet
- Evaluation of Tuberculosis Control Programs in Indonesian Community Health Centers Using Systemic ApproachDocument7 pagesEvaluation of Tuberculosis Control Programs in Indonesian Community Health Centers Using Systemic ApproachYoseph 'schatzi' DmcNo ratings yet
- Implementation Fidelity of Tuberculosis Infection Prevention and Control Practices in Three Hospitals With The Highest Notified Tuberculosis Cases in Bhutan A Mixed Method StudyDocument13 pagesImplementation Fidelity of Tuberculosis Infection Prevention and Control Practices in Three Hospitals With The Highest Notified Tuberculosis Cases in Bhutan A Mixed Method Studykinley09No ratings yet
- Newer Diagnostic Tests For Tuberculosis Their UtilDocument5 pagesNewer Diagnostic Tests For Tuberculosis Their UtilAbrar TaraNo ratings yet
- Spatial Distribution of Dengue Incidence: A Case Study in PutrajayaDocument10 pagesSpatial Distribution of Dengue Incidence: A Case Study in PutrajayaBela NovitaNo ratings yet
- Bao Et AlDocument7 pagesBao Et Alkang.asep008No ratings yet
- Factors Contributing To Poor Compliance With Anti-Tb Treatment Among Tuberculosis PatientsDocument14 pagesFactors Contributing To Poor Compliance With Anti-Tb Treatment Among Tuberculosis PatientsAnonymous QPXAgjBwNo ratings yet
- Faktor-Faktor Yang Mempengaruhi Tingkat Kepatuhan Pasien Terhadap Pengobatan Tuberkulosis Paru Di Lima Puskesmas Se-Kota PekanbaruDocument20 pagesFaktor-Faktor Yang Mempengaruhi Tingkat Kepatuhan Pasien Terhadap Pengobatan Tuberkulosis Paru Di Lima Puskesmas Se-Kota Pekanbarueis kusmitaNo ratings yet
- Research Article Knowledge, Attitude, and Practices On Drug-Resistant Tuberculosis Infection Control in Nepal: A Cross-Sectional StudyDocument8 pagesResearch Article Knowledge, Attitude, and Practices On Drug-Resistant Tuberculosis Infection Control in Nepal: A Cross-Sectional StudySohrab RohaneNo ratings yet
- JURNALDocument9 pagesJURNALRia seprizaNo ratings yet
- TB 2Document12 pagesTB 2ikNo ratings yet
- An Opd Based Prospective Exploratory Study of DermDocument4 pagesAn Opd Based Prospective Exploratory Study of DermSankita SandalNo ratings yet
- What Is New in Management of Pediatric TuberculosisDocument9 pagesWhat Is New in Management of Pediatric Tuberculosisviani ayalNo ratings yet
- Prasetyo DKKDocument11 pagesPrasetyo DKKS Yogaa MuliaaNo ratings yet
- Unit 7Document136 pagesUnit 7Today ViralNo ratings yet
- Predictors of Medication Adherence PPT ProposalDocument19 pagesPredictors of Medication Adherence PPT ProposalKeana DacayanaNo ratings yet
- Jurnal Diagnosis-1Document6 pagesJurnal Diagnosis-1Dian ZiziNo ratings yet
- Contemporary Clinical Trials: Contents Lists Available atDocument11 pagesContemporary Clinical Trials: Contents Lists Available atEdgar MejíaNo ratings yet
- Servikal TBDocument15 pagesServikal TBnur wahidaNo ratings yet
- Case Study #3Document26 pagesCase Study #3Reshma MohabeirNo ratings yet
- Jamainternal Gopalan 2018 Oi 180003Document9 pagesJamainternal Gopalan 2018 Oi 180003pentaxNo ratings yet
- Efektivitas Health Promotion Terhadap Upaya Pencegahan Kekambuhan Dan Kontrol AsmaDocument4 pagesEfektivitas Health Promotion Terhadap Upaya Pencegahan Kekambuhan Dan Kontrol AsmaAkbar ZhagtrisNo ratings yet
- Artikel 4Document8 pagesArtikel 4drlazyboyNo ratings yet
- Telemedicine and Asthma: An innovative approach to improve morbidity and mortality rates for active adults.: Effects of Telemedicine in Asthma care for remote and inner-city underserved populations.From EverandTelemedicine and Asthma: An innovative approach to improve morbidity and mortality rates for active adults.: Effects of Telemedicine in Asthma care for remote and inner-city underserved populations.No ratings yet
- Atif Et Al - 2011Document3 pagesAtif Et Al - 2011kang.asep008No ratings yet
- Bloss Et AlDocument7 pagesBloss Et Alkang.asep008No ratings yet
- Ade Et AlDocument7 pagesAde Et Alkang.asep008No ratings yet
- Abernathy Et AlDocument9 pagesAbernathy Et Alkang.asep008No ratings yet
- Abubakar Et AlDocument5 pagesAbubakar Et Alkang.asep008No ratings yet
- Abassi Et AlDocument6 pagesAbassi Et Alkang.asep008No ratings yet
- Uttarkhand & JK Adv Online (Agra)Document8 pagesUttarkhand & JK Adv Online (Agra)sipuns827No ratings yet
- Rntcp-Revised National Tuberculosis Control ProgrammeDocument29 pagesRntcp-Revised National Tuberculosis Control ProgrammedranshulitrivediNo ratings yet
- Guidelines For PMDT in India-Low PDFDocument334 pagesGuidelines For PMDT in India-Low PDFjai kishanNo ratings yet
- Revised National Tuberculosis Control Programme (RNTCP) : Dr. NavpreetDocument30 pagesRevised National Tuberculosis Control Programme (RNTCP) : Dr. NavpreetYagnik SanjayNo ratings yet
- Social & Preventive PharmacyDocument62 pagesSocial & Preventive PharmacyShabd aksharNo ratings yet
- Telangana Health Medical and Family Welfare Annual Report 2018 19Document47 pagesTelangana Health Medical and Family Welfare Annual Report 2018 19vani reddyNo ratings yet
- Revised National TB Control Programme (RNTCP)Document12 pagesRevised National TB Control Programme (RNTCP)Viswa GiriNo ratings yet
- Himachal Pradesh Current Affairs 2020 by AffairsCloudDocument37 pagesHimachal Pradesh Current Affairs 2020 by AffairsCloudMohit ChoudharyNo ratings yet
- Medicine Update 2021 Section 14Document56 pagesMedicine Update 2021 Section 14Huda AminNo ratings yet
- Draft - Roles Responsibilities and Management - UPHC Under NUHMDocument7 pagesDraft - Roles Responsibilities and Management - UPHC Under NUHMSelina Christian 57No ratings yet
- Health Programs in India - RNTCPDocument28 pagesHealth Programs in India - RNTCPAkash Mittal100% (1)
- Pediatric TB Guidelines 2022Document132 pagesPediatric TB Guidelines 2022DYMSNo ratings yet
- 1324288818compendium of Best Practices CE 29 Sep 2022Document86 pages1324288818compendium of Best Practices CE 29 Sep 2022K SNo ratings yet
- 2492169650guidelines For Condemnation and Replacement TB Lab EquipmentDocument9 pages2492169650guidelines For Condemnation and Replacement TB Lab EquipmentSabuj AhmedNo ratings yet
- Senior Treatment Supervisors (STS) : Part 1: Ensuring Proper TreatmentDocument35 pagesSenior Treatment Supervisors (STS) : Part 1: Ensuring Proper TreatmentVikas BhatiNo ratings yet
- Social and Preventive Pharmacy Revision Questions CBS PublicationDocument20 pagesSocial and Preventive Pharmacy Revision Questions CBS PublicationAntar GayenNo ratings yet
- National Health PolicyDocument34 pagesNational Health PolicydranshulitrivediNo ratings yet
- Research Paper On Tuberculosis in IndiaDocument8 pagesResearch Paper On Tuberculosis in Indiakcjzgcsif100% (1)
- Tuberculosis (Part 2) : DR Ruchi Dua Associate Professor (MD, DNB) Department of Pulmonary Medicine Aiims RishikeshDocument36 pagesTuberculosis (Part 2) : DR Ruchi Dua Associate Professor (MD, DNB) Department of Pulmonary Medicine Aiims RishikeshMohammed HammedNo ratings yet
- National Tuberculosis Elimination ProgrammeDocument11 pagesNational Tuberculosis Elimination ProgrammeRekha ChaudharyNo ratings yet
- Chapter 5 - National Health Programme PDFDocument26 pagesChapter 5 - National Health Programme PDFPratik LengureNo ratings yet
- India Is Now Working On The Target of Ending TB by The Year 2025Document4 pagesIndia Is Now Working On The Target of Ending TB by The Year 2025TZ VersionNo ratings yet
- Tuberculosis Isolates From Delhi Using Genotype Mtbdrplus AssayDocument7 pagesTuberculosis Isolates From Delhi Using Genotype Mtbdrplus AssayrehanaNo ratings yet
- ASHA Incentive Master Claim Form Draft ENGLISH PDFDocument8 pagesASHA Incentive Master Claim Form Draft ENGLISH PDFPushpa GopiNo ratings yet
- Annexure III.h: Total Male Female TS/TG Male Female TS/TGDocument9 pagesAnnexure III.h: Total Male Female TS/TG Male Female TS/TGTanishk MahereNo ratings yet