Professional Documents
Culture Documents
Minimal access surgery in children – 5 years institutional experience
Minimal access surgery in children – 5 years institutional experience
Uploaded by
Gunduz AgaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Minimal access surgery in children – 5 years institutional experience
Minimal access surgery in children – 5 years institutional experience
Uploaded by
Gunduz AgaCopyright:
Available Formats
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.
181]
Original Article
Minimal access surgery in children – 5 years
institutional experience
S N Oak, S V Parelkar, T Akhtar, M Joshi, R Pathak, N Viswanath, K Satish Kumar V, K Ravikiran
L Manjunath, A Ahmed
Department of Paediatric Surgery, T.N.M. C and B.Y.L. Nair Hospital, Mumbai, India
Address for correspondence: SN Oak, Dean and Professor and Head,Department of Paediatric Surgery, T.N.M.C and B.Y.L. Nair Hospital,
Mumbai – 400 008, India, E-mail: drtanveer28@yahoo.co.in
Abstract The role of minimal access surgery (MAS) in surgery
of children is slowly emerging over the last decade.
Context: Minimal access surgery (MAS) in children
The scope of MAS is to minimize the traumatic insult
are common place and performed worldwide with
gratifying results as the learning curve of the to the patient without compromise of the safety and
surgeon attains plateau. We share our experience efficacy of the treatment. For over two decades,
of this technically evolving modality of surgery, paediatric MAS was restricted mainly to diagnostic
performed at our setup over a period of 5 years. We use. More recently, however, with increasing
also review and individually compare the data for
experience and advances in miniaturized
commonly performed procedures with other
available series. Author also briefly discuss instrumentation, the role of MAS in the modern
potential advantages of MAS in certain debatable paediatric surgical armamentarium has become
conditions performed quickly and with cosmesis accepted. The paediatric surgical community has
as open procedure. Materials and methods: We embraced minimal access techniques for some
performed 677 MAS in children aged between 7
operations; others remain controversial. With each
days and 12 years. Five hundred and sixty-eight of
these were Laparoscopic procedures and 109 were advancing year, the instruments and optics are being
Video assisted thoracoscopic surgeries (VATS). In refined and newer indications are getting added to
all laparoscopic procedures, the primary port the list of laparoscopically manageable maladies.
placement was by the Hasson’s open technique.
We have used 5, 3 and 2 mm instruments. Our MATERIALS AND METHODS
study include 259 inguinal hernia, 161
Appendectomies, 95 VATS for empyema, 51
orchiopexies, 49 diagnostic laparoscopy, 29 Six hundred and seventy-seven children aged between
cholecystectomies, 22 adhesionlysis and other 7 days and 12 years underwent MAS in Paediatric
uncommonly performed procedures. Results: The Surgery Department of a University teaching Hospital
ultimate outcome of all the performed procedures between June 2000 and March 2005. Five hundred
showed gratifying trend, the data of which are and sixty-eight of these were laparoscopic procedures
discussed in detail in the article. Conclusion: As
we gained experience the operating time showed a
and 109 were Video assisted thoracoscopic surgery
decreasing trend, the complication rates and (VATS) [Table 1].
conversion rate also reduced. The advantages we
came across were better postoperative In all laparoscopic procedures, the primary port
appearances, less pain and early return to placement was by the Hasson’s open technique. The
unrestricted activities.
abdomen was insufflated with prewarmed carbon
dioxide starting at a pressure of 6 mmHg and slowly
Key words: laparoscopy; minimal access surgery; video
assisted thoracoscopic surgery increased to 12 mmHg depending upon the age and
121 Journal of Minimal Access Surgery | September 2005 | Volume 1 | Issue 3
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
weight of the child. A 5 mm wide-angle 0° telescope cases we felt the repair was not secure and in one
was used. We have used 5, 3 and 2 mm instruments. case there was bleeding from inferior epigastric vessel.
Placement and number of secondary ports were We had nine recurrences mainly in the earlier phase
dependent on the area of interest taking utmost care of study while using the intracorporeal suturing with
in triangularization. A thorough diagnostic intracorporeal knotting with absorbable suture
laparoscopy was done once the scope was inserted technique during the learning curve giving a total
including the walking of the bowel to rule out any recurrence rate of 3.5%. After shifting to
bowel pathology. Then the procedure was completed extracorporeal knotting and avoidance of absorbable
depending on the pathology. sutures, there are no recurrences. Four patients had
postoperative hydroceles which resolved
Hundred and nine children underwent VATS. The spontaneously within 2 months. One patient with
scope was inserted through the tube thoracostomy persistent hydrocele after 3 months underwent open
site in cases where it was inserted preoperatively but herniotomy. Doppler at 3 months after surgery
in the other patients it was inserted in the mid- showed no testicular atrophy.
axillary line at the sixth or seventh intercostal space.
In empyema, most of the time for toileting and even
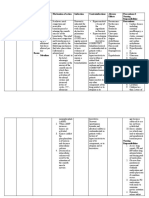
Table 1: Showing spectrum of cases
for decortication we have used only two ports.
Surgery Number
Inguinal hernia repair (number of repairs) 259
RESULTS Appendectomy 161
VATS for empyema 95
Laparoscopic inguinal herniorrhaphy Orchiopexy 51
Diagnostic laparoscopy 49
This series includes 200 children with inguinal hernia Cholecystectomy 29
treated laparoscopically (158 males, 41 females and Adhesions 22
1 intersex). The age range was from 1 month to Pullthrough for hirschsprungs 13
Ovarian tumours and cysts 10
12 years. Total of 259 hernias were repaired [201 in Mesenteric lymph node biopsy 8
male, 56 in female, 2 in a child with intersex (CAIS)]. Nephrectomy 6
Pullthrough for ARM 6
Twenty-one of the patients who presented with left
Fundoplication 5
hernia and 32 of those who presented with right Splenectomy 5
hernia (totally 53) had a contralateral patent processus VATS lung biopsy 5
Congenital diaphragmatic hernia 4
vaginalis (PPV). In three patients, both the internal Liver abscess 4
rings were closed. In female, majority were repaired Lung hydatid 4
using an endoloop and the redundant sac excised. Meckel’s diverticulum 4
VATS aspiration of abscess 4
But in three female hernias suturing with Mediastinal mass 2
extracorporeal knotting was done. The type of repair Mesenteric cyst 2
Pancreatic pseudocyst 2
in males has progressed from just dissection to
Primary peritonitis 2
intracorporeal suturing (darning or purse-string) with Pyeloplasty 2
inracorporeal knotting to intracorporeal suturing with VP Shunt with pseudocyst 2
Adrenelectomy 1
extracorporeal knotting without dissection. Initially Cholangiogram 1
we used to use absorbable vicryl and in two of these Faecal fistula 1
cases we had recurrence. Now we use 3-0 Ethilon® Hydrometrocolpos 1
Intersex-gonadectomy 1
nonabsorbable sutures. We have repaired 62 hernias Intussusception 1
with extracorporeal knotting using 3-0 Ethilon in Ovarian torsion 1
Parovarian cyst 1
which we did not have any recurrence. The operating
PD Catheter 1
time showed a decreasing trend as the team gained Pyloromyotomy 1
experience. A unilateral repair required 25 min and Retroperitoneal tumour biopsy 1
Ureterocoele 1
a bilateral repair 35 min. There were four Varicocoele 1
conversions to open herniotomy in our study. In three VATS in Chest trauma (bronchial tear) 1
Journal of Minimal Access Surger y | September 2005 | Volume 1 | Issue 3 122
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
Laparoscopic appendicectomy
Two hundred and ten children presented with history Laparoscopic cholecystectomy [Figure 3]
of abdominal pain. Of these 161 children had features Since the introduction of ultrasonography,
of acute appendicitis for whom laparoscopic cholelithiasis in children is being increasingly
appendicectomy. The remaining 49 children who recognized and referred to us. In our series 29 patients
presented with Recurrent abdominal pain underwent under went laparoscopic cholecystectomy. The
diagnostic laparoscopy which revealed features of youngest patient in the study was a 2½-year-old boy.
Appendicitis in 11 cases, adhesions in 22 cases, Kochs Ninteen patients were males and ten were females.
abdomen in five cases, Twisted ovarian cyst in three Symptomatic gallstones were present in 26 patients.
cases, Meckels in two cases [Figure 1], pelvic Acalculous cholecystitis was the indication for
peritonitis in one case [Figure 2] and in five patients cholecystectomy in only three patients. Four patients
no abnormality could be detected. We had five had hereditary spherocytosis and one had sickle cell
conversions, two due to hidden retrocaecal appendix, anaemia.
two due to gangrenous base and in one we had
bleeding from appendicular artery. Most of these Operative time varied from 45 to 180 min with a
conversions are in our learning curve period. mean time of 75 min and as we gained experience
the operative time reduced. Of the 29 patients, 25
For laparoscopic appendicectomy mean time taken patients were discharged on second postoperative
was 44.1 min. The analgesic and antibiotic day. Twenty-six patients returned to their normal
requirement was significantly low in laparoscopic activity i.e., going to school and play with in 8 days.
appendectomy. The postoperative stay and return to We had three conversions, two due to bleeding and
normal activity was early. No patient of laparoscopic in one case we had bile duct injury, which was
group had port site infection. fortunately identified and repaired during same
sitting.
Laparoscopic orchiopexy
Forty-three children with 51 nonpalpable Video assisted thoracoscopic surgery
undescended testes underwent laparoscopy in our In our series 109 children underwent VATS. VATS for
center. Among this, four had absent testes. 32 of the empyema was done in 95 cases of which 15 cases
47 (68.1%) testes were intra-abdominal as against were converted to open procedure due to very thick
varying reports ranging from 38.1 to 81.8%. A high peel and badly damaged underlying lung. In cases
intra-abdominal testis is one, which is more than who had presented early by the end of 5–7 days of
2.5 cm from the internal ring. Twelve (37.5 %) of our beginning of thoracic suppurative disorder, toileting
32 intra-abdominal testes were high and all these of pleural cavity was done by first clearing the pleural
were treated by a staged Stephen–Fowler cavity of collection and then removing all adhesions
laparoscopic orchiopexy. All the patients who had between the lung and the parietal pleura. Suction
undergone orchiopexies showed good vascular flow irrigation cannula itself was used to remove the tough
on postoperative Doppler examination. Postoperative as well as the fibrinous adhesions. In case where the
atrophy was seen in two testes on follow up and patients had presented later than seven days, the
another testis was found to be retracted into the pleural peel appeared to be thick and densely
inguinal canal for which an inguinal exploration and adherent to the underlying lung as well as to the
orchiopexy was done at 6 months postlaparoscopic thoracic wall and diaphragm and these may require
orchiopexy. Both atrophic testes were seen after a decortication.
staged procedure while the retraction was seen after
a single stage laparascopic orchiopexy. The overall There were 59 male patients and 36 female patients.
success rate of laparoscopic orchiopexy is 93.61%. The average age of the patients was 6 years with a
123 Journal of Minimal Access Surgery | September 2005 | Volume 1 | Issue 3
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
range from 11 months to 12 years. CT scan was done good procedure with least morbidity. Histopathology
for all the patients preoperatively. CT scan revealed Tuberculosis in three cases, sarcoidosis in
documented the disease process in a better way and one case and interstitial lung disease in one case.
facilitated in placement of trocars.
VATS in pulmonary hydatid
We had 44 patients of empyema where we did We have treated three children with primary
Primary VATS (patients in whom tube thoracostomy pulmonary hydatid cysts (total of six cysts). For four
was not done preoperatively). Of these only four cysts we did VATS assisted minithoracotomy with
patients required a conversion to thoracotomy. Fifty- enucleation and capittonage and two with VATS
one patients had been initially treated with a tube assisted limited resection.
thoracostomy and out of these 11 were converted to
thoracotomy. These patients had collapsed lungs and VATS in trauma
extremely dense fibrous peel [Figure 4]. These findings We had a 6-year-old boy who presented with blunt
suggest that an initial tube thoracostomy increases injury to chest. Chest X-ray revealed Right
the chances of conversion. Chances of conversion are pneumothorax. Inspite of 3 days of intercostal
also more if the disease process is more than 7 days drainage there was no improvement. On VATS, we
and increases as the duration increases. Total found the tip of endotracheal suction tube introduced
conversion rate in our series was 15.7%. The mean by the anaesthetist in pleural cavity. Thoracotomy
operating time was 90 min (ranging between 150 revealed complete transection of right main bronchus,
and 45 min). In all patients intercostal drainage tubes which was repaired. The child had uneventful recovery
were kept postoperatively. The average time that the and is doing well.
intercostal tube was kept was for 3.5 days.
Neonatal ovarian cysts
Good lung expansion in the immediate postoperative We encountered three cases of neonatal ovarian cysts,
period was seen in 92% of cases. Two patients of VATS which were more than 5 cm in size. Two cases
had postoperative residual collection for which Re- underwent laparoscopic aspiration and deroofing and
do VATS was done after which there was complete in other case laparoscopic oophorectomy was done
expansion. Three patients developed pneumothorax because of torsion [Figure 6]. Histopathologically, all
6 weeks, 8 weeks and 4 months after VATS, which the three cysts turned out to be Follicular cyst. There
was treated with simple tube drainage. All patients is no recurrence of the cyst with a mean follow up of
have been clinically asymptomatic since their 15 months till now.
discharge and have been followed up on an average
of 12–36 months. The chest X-ray of all patients is Lap assisted pull through
normal. There was no mortality in our study. The Ninteen cases underwent Lap assisted pull through
average duration of hospital stay has been 8 days of which 13 cases were Hirschsprungs and six were
postoperatively in empyema. High anorectal malformations. Three cases were
converted to open procedure.
VATS in lung abscess
In our series we had four cases of lung abscess not Laparoscopy in solid organs
responding to parenteral antibiotics (>2 weeks) in In present series, six patients under went
which VATS aspiration was done. All the patients nephrectomy, five underwent splenectomy and one
responded very well to antibiotics after aspiration. case adrenalectomy.
VATS lung biopsy Laparoscopic mesenteric lymph node biopsy
We have done VATS lung biopsy [Figure 5] in five We have done laparoscopic mesenteric lymph node
cases. In two cases endoscopic stapler was used and biopsy in eight cases. In five cases we delivered the
in three vicryl loop was used. We find it to be very mesentery through the umbilical port and did
Journal of Minimal Access Surger y | September 2005 | Volume 1 | Issue 3 124
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
Figure 1: Meckel’s diverticulum Figure 4: Pleural peel in empyema
Figure 2: Frank pus in pelvis in a case of primary peritonitis Figure 5: Endoscopic stapler for lung biopsy
Figure 3: Extensive omental adhesions in cholecystitis Figure 6: Deroofing of neonatal ovarian cyst with 2 mm instruments
125 Journal of Minimal Access Surgery | September 2005 | Volume 1 | Issue 3
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
extracorporeal biopsy and in three cases we took Intestinal resection and anastomosis.
biopsy within the abdomen. We have found
laparoscopy to be a very good diagnostic tool, which Group IV: Unsuitable by laparoscopy like Major cancer
could yield adequate tissue for histopathological resections and Hepatic resections. These are the
confirmation with least morbidity. operations where access trauma forms only a small
percentage of total operative insult.
DISCUSSION
Inguinal hernia repair
The horizon of Paediatric laparoscopic surgery has Inguinal hernia repair is one of the most common
widened so much that most of the intra-abdominal operations per formed in children [Table 2].
pathologies in children can now be safely tackled Laparoscopic inguinal hernia repair in children is often
laparoscopically. The different indications for considered controversial but as the surgeon gains
paediatric laparoscopy can be divided into four experience it has been proved to be feasible, safe and
groups depending upon the benefit of laparoscopy reliable technique. A contralateral PPV is present in a
compared to open surgery. significant number of children and laparoscopy offers
safe alternative to treat both sides at the same
Group I: Operations where the laparoscopic approach sitting.[1,2] An internal opening of less than 2 mm can
provides an undoubted benefit and has replaced open be left alone as it is unlikely to cause a hernia.[4]
intervention like Cholecystectomy, Cryptorchidism
(diagnostic and therapeutic), Appendicectomy, Appendicectomy
Fundoplication, Adrenelectomy, Varicocele operations Since MacKernan and Saye did first laparoscopic
and Nephrectomy for benign conditions. appendicectomy in 1988, it has rapidly gained
acceptance and has shown to be safe and effective
Group II: Laparoscopy appears beneficial and safer technique. If only the size of the scar is compared,
but more information is warranted. These include laparoscopy seems to have very few advantages over
Hernia repair, Adhesiolysis, Treatment of V.P. Shunt classic Mc Burney’s incision. However, there is very
complications and Pyeloplasty. little doubt that a laparoscopic appendicectomy has
reduced postoperative morbidity and early return to
Group III: Operations, which are currently under school with virtually scarless abdomen and has a
evaluation and should not be attempted outside significantly low incidence of postoperative
clinical trials like TEF repairs, Ureteric implantations, adhesions. [5–7]
Table 2: Comparative study with similar series
Schier et al.[4] Montupet and Esposito[3] Current
No. of repairs 223 339 259
Age 3 weeks to 13 years 8 months to 14 years 1.5 months to 12 years
Median age 2.0 years 4.2 years 4.6 years
No. of girls 58 (26%) 5 (1%) 56 (21.6%)
No. of boys 185 (74%) 334 (99%) 201 (77.6%)
Contra-lateral patent Rt. side hernia – Overall 60 out of 339 Rt. side hernia –
vaginalis Lt CPPV = 147 B-137 G-10 Lt CPPV = 32
Lt. side hernia – Lt. side hernia –
Rt. CPPV = 152 B-131 G-21 Rt. CPPV =21
Direct hernia 9 (4%) 4 (1.2%) 3 (1.15%)
No hernia 1.9% 4 (1.54%)
Suture used 4-0 Nonabsorbable 4-0 Nonabsorbable 3-0 Nonabsorbable
Operating time
(unilateral/bilateral) 14/21 min 13/23 min 25/35 min
Recurrence 8 (3.5%) 12 (3.5%) 9 (3.5%)
Hydrocele 9 (4%) 4 (1.2%) 4 (1.54%)
Testicular atrophy 1 (0.5%) – –
Journal of Minimal Access Surger y | September 2005 | Volume 1 | Issue 3 126
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
Sometimes in the presence of acute or chronic Table 3: Showing comparison of parameters between
recurrent abdominal pain syndrome, laparoscopy present study and other studies
shows a normal appendix. If another disease, which Variable Kim et al. [12] Jawad et al.[13] Present
study
explains the pain syndrome is found and treated, the
1. Parenteral 1.8 ± 1.4 1
appendix can be left alone. On the other hand, if no analgesia (days) LC
anomaly is found it seems more judicious to remove OC 2.7 ± 0.9 3
2. Operating time
the appendix. The argument in favour of this approach (minutes)
is endoappendicitis, which reaches only the mucosa. (Mean) LC 129.8 ± 74.1 89.81 ± 21.89 75
Most of the ‘normal-looking appendix’, which were OC 86.4 ± 30.9 50
3. Duration of stay
removed showed either fecoliths or worms or (days)
histopathological evidence of chronic inflammation. (Mean) LC 2.0±1.8 1.68±0.46 3.35
OC 6.32.9 6.07±0.30 8.5
4. Resume activity
Orchiopexy at LC 8
Laparoscopy has been accepted as the surgical (Days) OC 21
5. Wound infection LC 0
procedure of choice in children with nonpalpable (Number) OC 1
undescended testis. This has proved to be a safe and Abbreviations: OC, Open Cholecystectomy; LC, Laparoscopic
Cholecystectomy.
reliable diagnostic test for nonpalpable undescended
Unpaired t -test applied for operating time and duration of stay.
testis with an accuracy of 100%, which no radiological For operating time: t-value is 2.131 and P-value is 0.0427 (significant).
method could achieve. Since 25–56% of nonpalpable For duration of stay: t -value is 4.286 and P-value is 0.0002 (significant).
testes are reported to be vanishing, laparoscopy
avoids extensive retroperitoneal dissection in these hospitalization. VATS has recently regained popularity
patients. The other important advantage is the as an attempt to decrease the morbidity associated
decision about the technique of orchiopexy in intra- with open decortication.[14–16]
abdominal testis where a single or double staged
laparoscopic procedure is done depending on VATS lung biopsy is more efficient as it saves operative
whether the testis is high or low lying within the time and provides good visualization of lung and
abdomen.[8–11] pleural surfaces in addition to reducing postoperative
pain and hospital stay. Fiona et al. concluded that
Cholecystectomy sufficient tissue could be provided for both
In our series nonhaemolytic cholelithiasis is the microbiological and histological study.[17]
commonest indication for cholecystectomy in
children. Even other studies show nonhaemolytic VATS assisted minithoracotomy is being described as
cholelithiasis as the commonest indication for an alternative in the management of pulmonary
cholecystectomy.[12] By comparison with conventional hydatid. The postoperative morbidity is much
open cholecystectomy, laparoscopic approach appears reduced compared to the classical thoracotomy in the
to be associated with minimal morbidity, shorter surgical treatment of pulmonary hydatid cysts in
hospital stay, earlier return to school and a better children.[18]
cosmetic result [Table 3].[13]
Neonatal ovarian cyst
VATS Small simple ovarian cysts fewer than 5 cm in
In empyema cases, it was initially thought that diameter can be obser ved carefully with serial
proper decortication and debridement can only be ultrasonography. But, all symptomatic and complex
accomplished by open thoracotomy and therefore ovarian cysts and simple cysts over 5 cm in diameter
earlier recommendations were for early thoracotomy in addition to smaller cysts less than 5 cm showing
and decortication in all cases of empyema in children. no decrease in size should be considered as a surgical
Unfortunately, these procedures are associated with indication to rescue the ovarian tissue. Laparoscopy
significant morbidity and mortality and prolonged is well tolerated by newborns. In addition to
127 Journal of Minimal Access Surgery | September 2005 | Volume 1 | Issue 3
[Downloaded free from http://www.journalofmas.com on Sunday, October 8, 2017, IP: 5.197.213.181]
Oak SN et al: Minimal access surger y in children
confirming the diagnosis, laparoscopy can be used in children: Report of 1379 cases. J Pediatr Surg 1994;29:786-9.
8. Esposito C, Garipoli V. The value of 2-step laparoscopic Fowler-
for aspiration, deroofing, cystectomy and Stephens orchiopexy for intra-abdominal testes. J Urol.
oopherectomy in cases of ovarian cyst.[19,20] 1997;158:1952-4.
9. Docimo SG, Moore RG, Adams J, Kavoussi LR. Laparoscopic
orchiopexy for for the high palpable undescended testis:
CONCLUSION preliminary experience. J Urol 1995;154:15-3.
10. Schleef J, von Bismarck S, Burmuric K, Gutmann A. Mayr Graz:
MAS is here to stay. This is as truer in Paediatric Groin exploration for nonpalpable testes: Laparoscopic approach.
J Pediatr Surg 2002;37:1552–5.
surgery as in adults. It is needless to mention the 11. Merry CC, Sweeney B, Puri P. The vanishing testis: anatomical and
advantages of MAS. With proper judgment and self- histological findings. Eur Urol 1997;65-7.
assessment, an exciting and stimulating time exists 12. Kim PC, Wesson D, Superina R, Filler R. Laparoscopic
Cholecystectomy versus open Cholecystectomy in Children:
in the future for surgeons incorporating MAS into Which is better’’ J Pediatr Surg. 1995;30:971-3.
their clinical practice. Nevertheless conversion to open 13. Jawad AJ, Kurban K, el-Bakry A, al-Rabeeah A, Seraj M, Ammar A.
Laparoscopic cholecystectomy for cholelithiasis during infancy
procedure in case of difficulty, anomalous anatomy
and childhood; Cost analysis and review of current indications.
or unsuspected pathology by killing the personal ego World J Surg 1998;22:69-73.
represents sound surgical judgement and is a 14. Mandal AK, Thadepalli H. Treatment of spontaneous bacterial
empyema thoracis. J Thorac Cardiovasc Surg 1987;94:414-8.
testimony to a surgeon’s conservative and more 15. Hoover EL, Hsu HK, Ross MJ. Reappraisal of empyema thoracis:
importantly ‘safe approach’. Surgical intervention when the duration of illness is unknown.
Chest 1986;90:511-5.
16. Oakes DD, Sherck JP, Brodsky JB, James BD. Mark. Therapeutic
REFERENCES thoracoscopy. J Thorac Cardiovasc Surg 1984;87:269-73.
17. Fiona MC, William SW, Evan WJ. Efficacy of video assisted
1. Miltenburg D, Nucbtern JG, Jaksic T, Kozinetiz C. Laparoscopic thoracoscopic lung biopsy: an historical comparison with open
evaluation of the pediatric inguinal hernia- a meta- analysis. J lung biopsy. Thorax 1994;49:361-3
Pediatr Surg 1998;33:874-9. 18. Oto O, Silistreli E, Erturk M, Maltepe F. Thoracoscopic guided
2. Sparkman RS. Bilateral exploration in inguinal hernia in juvenile minimally invasive surgery for giant hydatic cyst. Eur J
patients. Surgery 1987;51:393-406. Cardiothorac Surg 1999;116:494-5.
3. Montupet P, Esposito C. Laparoscopic treatment of congenital 19. Chiaramonte C, Piscopo A, Cataliotti F. Ovarian Cysts in Newborns
inguinal hernia in Children. J Pediatr surg 1999;34:420-3 PSI 2001;17:171-4.
4. Schier F, Montupet P, Esposito C. Laparoscopic inguinal 20. Widdowson DJ, Pilling DW, Cook RC. Neonatal ovarian cysts:
herniorrhaphy in children: a three-center experience with 933 therapeutic dilemma. Arch Dis Child 1988;63:737-42.
repairs. J Pediatr Surg 2002;37:395-7.
5. Atwood SE, Hill AD, Murphy PG. A prospective randomized trial
of laparoscopic Vs open appendicectomy. Surgery 1992;112:497- Cite this article as: Oak SN, Parelkar SV, Akhtar T, Joshi M, Pathak R,
501. Viswanath N, Satish Kumar KV, Ravikiran K, Manjunath L, Ahmed A.
6. Martin LC, Uente I, Sosa JI. Open Vs laparoscopic appendicectomy. Minimal access surgery in children – 5 years institutional experience. J Min
Access Surg 2005;121-128.
A randomized comparison. Ann Surg 1995;222:256-62
7. El Ghoneimi A, Valla JS, Limonne B. Laparoscopic appendicectomy Date of submission: 24/03/05, Date of acceptance: 28/10/05
Journal of Minimal Access Surger y | September 2005 | Volume 1 | Issue 3 128
You might also like
- Amboss NotesDocument12 pagesAmboss NotesVee Mend100% (2)
- TAPP HernioplastyDocument5 pagesTAPP HernioplastyMaryam Alam KhanNo ratings yet
- Use Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenDocument4 pagesUse Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenYelisa PatandiananNo ratings yet
- Rajapandian 2018Document5 pagesRajapandian 2018DH SiriruiNo ratings yet
- Appendicitis MattiotiDocument6 pagesAppendicitis MattiotiMedardo ApoloNo ratings yet
- Laparoscopic Appendicectomy in All Trimesters of PregnancyDocument7 pagesLaparoscopic Appendicectomy in All Trimesters of PregnancyJason CalvinNo ratings yet
- 4 Kuratani2008Document5 pages4 Kuratani2008M RidwanNo ratings yet
- Lawal 2016Document3 pagesLawal 2016firmankamalNo ratings yet
- Endoscopic Treatment of Choanal Atresia and Use of Balloon Dilation: Our ExperienceDocument6 pagesEndoscopic Treatment of Choanal Atresia and Use of Balloon Dilation: Our Experiencefarah maulida martaNo ratings yet
- Ciencia e Technica Omentum Overlay PDFDocument10 pagesCiencia e Technica Omentum Overlay PDFAlin MihetiuNo ratings yet
- DAnnibale2004 Article RoboticAndLaparoscopicSurgeryFDocument7 pagesDAnnibale2004 Article RoboticAndLaparoscopicSurgeryFWarren SeowNo ratings yet
- Fifteen Years Experience in Laparoscopic Inguinal Hernia Repair in Pediatric Patients. Results and Considerations On A Debated ProcedureDocument5 pagesFifteen Years Experience in Laparoscopic Inguinal Hernia Repair in Pediatric Patients. Results and Considerations On A Debated ProcedureRagabi RezaNo ratings yet
- Ijcem0007 1366Document4 pagesIjcem0007 1366Ratih Kusuma DewiNo ratings yet
- Omentum OverlayDocument10 pagesOmentum OverlayAlin MihetiuNo ratings yet
- Ismaeil 2018Document15 pagesIsmaeil 2018Javier ZaquinaulaNo ratings yet
- Total Laparoscopic HysterectomyDocument8 pagesTotal Laparoscopic HysterectomySamir CastilloNo ratings yet
- Alesina Et Al., 2021Document9 pagesAlesina Et Al., 2021NyomantrianaNo ratings yet
- Complicationsoflapmyomectomy ANZ 2010Document7 pagesComplicationsoflapmyomectomy ANZ 2010Nadila 01No ratings yet
- Al Sadek2014Document7 pagesAl Sadek2014AYŞE GÜLŞAH ATASEVERNo ratings yet
- Laparoscopic Ventral Hernia Repair With Tacker Only Mesh Fixation: Single Centre ExperienceDocument5 pagesLaparoscopic Ventral Hernia Repair With Tacker Only Mesh Fixation: Single Centre ExperienceMudassar SattarNo ratings yet
- TVP 2022 0708 - OvariohysterectomyDocument9 pagesTVP 2022 0708 - Ovariohysterectomysimon alfaro gonzálezNo ratings yet
- Vaginal Agenesis: Experience With Sigmoid Colon NeovaginoplastyDocument5 pagesVaginal Agenesis: Experience With Sigmoid Colon NeovaginoplastyismuNo ratings yet
- 8ring and Res. ClipDocument6 pages8ring and Res. ClipJorge CisnerosNo ratings yet
- Robotics and InfertilityDocument6 pagesRobotics and InfertilityConsultorio Ginecología y ObstetriciaNo ratings yet
- Laparoscopic Herniotomy For Congenital Inguinal Hernia Prospective Assessment of Feasibility and Outcome Analysis in Tertiary Center in NepalDocument5 pagesLaparoscopic Herniotomy For Congenital Inguinal Hernia Prospective Assessment of Feasibility and Outcome Analysis in Tertiary Center in NepalrhmathidayatNo ratings yet
- Endoscopic Excision of Antrochoanal PolypDocument3 pagesEndoscopic Excision of Antrochoanal PolypreginalisaNo ratings yet
- Is 2Document10 pagesIs 2intan juitaNo ratings yet
- Saravanan 10.41030971 9261.43800Document7 pagesSaravanan 10.41030971 9261.43800CherNo ratings yet
- 10 1 1 115Document151 pages10 1 1 115Angela TorrenteNo ratings yet
- Proximal Hypospadias Repair With Bladder Mucosal Graft: Our 10 Years ExperienceDocument6 pagesProximal Hypospadias Repair With Bladder Mucosal Graft: Our 10 Years ExperienceLastri HillaryNo ratings yet
- Transvaginal Myomectomy With Screw Traction by Colpotomy: OriginalarticleDocument5 pagesTransvaginal Myomectomy With Screw Traction by Colpotomy: OriginalarticleWillis WiNo ratings yet
- Laparoscopic Appendectomy As An AltDocument6 pagesLaparoscopic Appendectomy As An Altmarcela.orellanatNo ratings yet
- 1 PDFDocument6 pages1 PDFSamiaNazNo ratings yet
- 10.1089lap.2016.0031Document5 pages10.1089lap.2016.0031dw21541No ratings yet
- Dis Colon Rectum - Endoscopic Mucosal Resection of Large Sessile Colorectal PolypsDocument10 pagesDis Colon Rectum - Endoscopic Mucosal Resection of Large Sessile Colorectal PolypsChargerNo ratings yet
- Thoracic Endoscopic Spine Surgery A ComprehensiveDocument11 pagesThoracic Endoscopic Spine Surgery A Comprehensivesanjay chhawraNo ratings yet
- The Learning Curve For Hernia PDFDocument5 pagesThe Learning Curve For Hernia PDFIgor CemortanNo ratings yet
- Anoplastia Percutanea 2022Document11 pagesAnoplastia Percutanea 2022Sandra Cárdenas HilasacaNo ratings yet
- Anterior Abdominal Wall HerniaDocument8 pagesAnterior Abdominal Wall HerniaOttofianus Hewick KalangiNo ratings yet
- Management of AUB in A Bicornuate Uterus - Endometrial Ablation in A CompDocument1 pageManagement of AUB in A Bicornuate Uterus - Endometrial Ablation in A Comptipu42No ratings yet
- 3 PBDocument6 pages3 PBAulia Rizqi MulyaniNo ratings yet
- Cme 200704Document16 pagesCme 200704tomyhardiantoNo ratings yet
- Elkhoury 2015Document5 pagesElkhoury 2015mod_naiveNo ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- Open Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective StudyDocument3 pagesOpen Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective Study'Adil MuhammadNo ratings yet
- Comparison of Two Different Method of Surgery in Ileus MeconiumDocument4 pagesComparison of Two Different Method of Surgery in Ileus MeconiumCirugía Pediátrica León Gto.No ratings yet
- Treatment of Anal Stenosis A 5year Revie PDFDocument3 pagesTreatment of Anal Stenosis A 5year Revie PDFJimi Kalvin SarareniNo ratings yet
- Russell 2017Document6 pagesRussell 2017pancholin_9No ratings yet
- Could Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProceduresDocument9 pagesCould Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProcedurespingusNo ratings yet
- Laparoscopic Entry TechniquesDocument9 pagesLaparoscopic Entry TechniquesDougNo ratings yet
- Jandrol 112 016444Document7 pagesJandrol 112 016444Павел ГичакNo ratings yet
- 2019 Simplified Minimally Invasive Surgical Approach For Prophylactic Laparoscopic Gastropexy in 21 CasesDocument8 pages2019 Simplified Minimally Invasive Surgical Approach For Prophylactic Laparoscopic Gastropexy in 21 CasesrizalakbarsyaNo ratings yet
- THT Jaga IiDocument2 pagesTHT Jaga IiZakkyMaulanaRahmatNo ratings yet
- Parastomal Hernias - Laparoscopic ManagementDocument6 pagesParastomal Hernias - Laparoscopic ManagementGrahamOliverAceroVieraNo ratings yet
- Artikel Tatalaksana APPDocument18 pagesArtikel Tatalaksana APPaulia agustinaNo ratings yet
- Umesh Singh. TLTK-47Document5 pagesUmesh Singh. TLTK-47HẢI HOÀNG THANHNo ratings yet
- Tecnica de Clips Nefrectomia ParcialDocument8 pagesTecnica de Clips Nefrectomia ParcialAlfredo BalcázarNo ratings yet
- Bun V34N3p223Document6 pagesBun V34N3p223pingusNo ratings yet
- Delatorre 2020Document5 pagesDelatorre 2020Rizky AmaliahNo ratings yet
- Hysterectomy For Gynecological Indication in Six Medical Facilities in LubumbashiDRC Frequency, Indications, Early Operative ComplicationsDocument11 pagesHysterectomy For Gynecological Indication in Six Medical Facilities in LubumbashiDRC Frequency, Indications, Early Operative ComplicationsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Modern_management_of_bladder_exstrophy_rDocument7 pagesModern_management_of_bladder_exstrophy_rGunduz AgaNo ratings yet
- Pediatric Sepsis Definition-A Systematic Review Protocol by The Pediatric Sepsis Definition TaskforceDocument7 pagesPediatric Sepsis Definition-A Systematic Review Protocol by The Pediatric Sepsis Definition TaskforceGunduz AgaNo ratings yet
- Surgical Advances in the Fetus and Neonate 2012Document13 pagesSurgical Advances in the Fetus and Neonate 2012Gunduz AgaNo ratings yet
- Daigle-Boerema Gastropexy PEHDocument7 pagesDaigle-Boerema Gastropexy PEHGunduz AgaNo ratings yet
- Congenital TEF - A Modified Technique of Anastomosis Using Pleural FlapDocument4 pagesCongenital TEF - A Modified Technique of Anastomosis Using Pleural FlapGunduz AgaNo ratings yet
- Anesthetic Considerations in A PretermDocument5 pagesAnesthetic Considerations in A PretermGunduz AgaNo ratings yet
- Pediatric Penile Pain Secondary To Idiopath - 2013 - Journal of Pediatric SurgerDocument2 pagesPediatric Penile Pain Secondary To Idiopath - 2013 - Journal of Pediatric SurgerGunduz AgaNo ratings yet
- Loss of The Penile Glans andDocument6 pagesLoss of The Penile Glans andGunduz AgaNo ratings yet
- Fluid Management in Association With Neonatal SurgeryDocument3 pagesFluid Management in Association With Neonatal SurgeryGunduz AgaNo ratings yet
- Pediatric ShockDocument11 pagesPediatric ShockGunduz AgaNo ratings yet
- The Use of Alloderm For A Giant Omphalocele With - 2013 - Journal of PediatricDocument3 pagesThe Use of Alloderm For A Giant Omphalocele With - 2013 - Journal of PediatricGunduz AgaNo ratings yet
- The Peculiar Appearance of A Developing Pyog - 2013 - Journal of Pediatric SurgeDocument2 pagesThe Peculiar Appearance of A Developing Pyog - 2013 - Journal of Pediatric SurgeGunduz AgaNo ratings yet
- Патофизиология 1 (П.Ф. Литвицкий)Document739 pagesПатофизиология 1 (П.Ф. Литвицкий)Gunduz AgaNo ratings yet
- Research Article - Pulmonary Artery Measurements As Postnatal Prognostic Tool in Right Congenital Diaphragmatic HerniaDocument2 pagesResearch Article - Pulmonary Artery Measurements As Postnatal Prognostic Tool in Right Congenital Diaphragmatic HerniaGunduz AgaNo ratings yet
- Pediatric SurgeryDocument393 pagesPediatric SurgeryGunduz AgaNo ratings yet
- ScabiesDocument38 pagesScabiesSiti Sabrina AtamiaNo ratings yet
- Hematology MCQDocument19 pagesHematology MCQshamseerNo ratings yet
- Miasm ConsolidatedDocument72 pagesMiasm ConsolidatedSatyendra RawatNo ratings yet
- Low Vision: Care of The Patient WithDocument39 pagesLow Vision: Care of The Patient WithDattatri ReddyNo ratings yet
- Candidate'S Biodata: Project Code: Project Title: A. Personal DataDocument7 pagesCandidate'S Biodata: Project Code: Project Title: A. Personal DataAmazing and FunnyNo ratings yet
- Medical Terminology ١Document34 pagesMedical Terminology ١Spotify IraqNo ratings yet
- BGSD Health IssuesDocument3 pagesBGSD Health IssuesSemi FatimaNo ratings yet
- Aspiration PneumoniaDocument1 pageAspiration Pneumoniadamsel in distressNo ratings yet
- Medical CertificateDocument2 pagesMedical CertificateVartika VashistaNo ratings yet
- NUR 145 - SAS 16-18 Activity For THF GroupDocument10 pagesNUR 145 - SAS 16-18 Activity For THF Groupella retizaNo ratings yet
- Daniel Santiago Rincón PinzónDocument2 pagesDaniel Santiago Rincón PinzónYANDRA YINNETH RINCON PINZONNo ratings yet
- Dizziness HXDocument4 pagesDizziness HXbadmanNo ratings yet
- Art of Reporting: Prof .Sherein A.ShalabyDocument51 pagesArt of Reporting: Prof .Sherein A.ShalabySherein ShalabyNo ratings yet
- Root Canal Cover-Up by MEINIG G - DesconhecidoDocument216 pagesRoot Canal Cover-Up by MEINIG G - DesconhecidoOswaldorfNo ratings yet
- Clinical Notes On The Illness and Death of President Franklin D 1970Document13 pagesClinical Notes On The Illness and Death of President Franklin D 1970Đang Kết NốiNo ratings yet
- Trastorno de AdaptacionDocument11 pagesTrastorno de AdaptacionEduardo AguilarNo ratings yet
- Gentle Therapy With Biofrequency - AE BaklayanDocument92 pagesGentle Therapy With Biofrequency - AE BaklayanNeil Beechwood100% (1)
- Task 5 Sicknesses and Deseases, CWDocument6 pagesTask 5 Sicknesses and Deseases, CW2212070147 INEZ HILERY ARITONANGNo ratings yet
- 2018 Ultrasound A Core Review PDFDocument617 pages2018 Ultrasound A Core Review PDFsun sealNo ratings yet
- DS ICS DuaventDecilone ForteDocument6 pagesDS ICS DuaventDecilone ForteThrinNo ratings yet
- Smile TrioriginDocument161 pagesSmile TrioriginCristi Caras100% (5)
- Section 3 - WorksheetDocument4 pagesSection 3 - WorksheetEsraa AhmedNo ratings yet
- NBME Shelf Exam Sample Questions - OB GYNDocument6 pagesNBME Shelf Exam Sample Questions - OB GYNNehal LakdawalaNo ratings yet
- History of Nursing: Nursing in The PhilippinesDocument3 pagesHistory of Nursing: Nursing in The PhilippinesKeeshia CassandraNo ratings yet
- CHOLECYSTITIS With CHOLECYSTOLITHIASISDocument2 pagesCHOLECYSTITIS With CHOLECYSTOLITHIASISkennice_nereaNo ratings yet
- Treatment of Maxillary SinusitisDocument15 pagesTreatment of Maxillary SinusitisRabina PantaNo ratings yet
- Fluorouracil Drug StudyDocument8 pagesFluorouracil Drug StudyAlexandrea MayNo ratings yet
- GIT Examination PSC2021Document3 pagesGIT Examination PSC2021علي 707No ratings yet
- OLGMS Covid 19 GuidelinesDocument23 pagesOLGMS Covid 19 Guidelinesιωαναθαν ρααγασNo ratings yet