Professional Documents
Culture Documents
Role of Intraoperative Ultrasound in Resection of Pediatric Brain Tumors
Uploaded by
Ramo Willa Abraham-JacobOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Role of Intraoperative Ultrasound in Resection of Pediatric Brain Tumors
Uploaded by
Ramo Willa Abraham-JacobCopyright:
Available Formats
Childs Nerv Syst (2010) 26:11891193 DOI 10.
1007/s00381-010-1091-4
ORIGINAL PAPER
Role of intraoperative ultrasound in resection of pediatric brain tumors
Mohamed Ahmed El Beltagy & Mohamed Aggag & Mohamed Kamal
Received: 27 December 2009 / Accepted: 26 January 2010 / Published online: 24 February 2010 # Springer-Verlag 2010
Abstract Purpose In neurosurgery, ultrasound is useful in determination of the tumor location, differentiation between solid tumors and cystic components, as well as definition of the shortest and safest access to the mass. This study aims to evaluate the role of the intraoperative ultrasound in resection of pediatric brain tumors. Methods Intraoperative ultrasonography (conventional BMode) was performed in 25 pediatric patients with brain tumors pre-, during, and post-resection, in whom eight patients were supratentorial and 17 were infratentorial. Post-op Grayscale images of the brain tumors on conventional ultrasound were compared with the results of immediate postoperative magnetic resonance imaging. Results The border of the tumor and post-resection residual tumor were more distinguishable from healthy brain on ultrasound during the operation. Improved definition of the tumor tissue from normal brain with ultrasound was demonstrated in all cases aiding in tumor resection. Conclusion Intraoperative ultrasound is suggested to be a useful imaging technique in defining the border between the tumor and healthy brain tissue pre-resection, in detecting residual tumor tissues after the resection of the
mass, and in guiding to the shortest and safest access to the tumor during neurosurgery. Keywords Intraoperative ultrasound . Brain tumors . Resection
Introduction Brain tumors are the most common form of solid tumors in children. According to the data from the American Cancer Society, brain tumors account for 20.7% of pediatric malignancies [1]. Pediatric brain tumors are the leading cause of death from solid tumors in children [2]. Pediatric neurooncology has evolved into a multidisciplinary collaborative specialty that combines the expertise from radiation oncologists, neuroradiologists, neurologists, neuropathologists, and pediatric oncology. Each of these specialties provides important components of comprehensive care. Current management strategies can optimize outcomes by integrating the standard of care with novel and investigative therapies. The role of neurosurgery in pediatric brain tumors is to reduce the tumor burden, minimize symptoms, and preserve functional abilities. Recent improvements in the surgical management of brain tumors have reduced morbidity and increased the possibility for aggressive tumor resection [3]. For operable brain tumors, surgical resection remains the treatment of choice. However, maximal resection sometimes remains challenging due to lack of definite border between some malignant tumors and normal brain tissue. Therefore, defining the border of the tumor is a major concern in neurosurgery [4]. Modern imaging tools and recent advances in imaging techniques now serve as the basis of early diagnosis of brain tumors. This technology has moved into the operating room. Magnetic resonance imaging (MRI)
M. A. El Beltagy (*) Department of Neurosurgery, Childrens Cancer Hospital, Cairo, Egypt e-mail: Beltgy_mohamed@hotmail.com M. Aggag Department of Radiodiagnosis, Childrens Cancer Hospital, Cairo, Egypt M. Kamal Department of Research, Childrens Cancer Hospital, Cairo, Egypt
1190
Childs Nerv Syst (2010) 26:11891193
continues to be the most sensitive and preferred diagnostic study for identifying these lesions. All imaging sequences from preoperative MRIs should be carefully reviewed. Anatomical location of a tumor, tumor size, and edema are often delineated on T1, T2, and FLAIR sequences [3]. Ultrasound offers real-time imaging; however, showing a tumors definite margins is controversial. Echogenic tissues such as brain edema or gliosis can interfere with the differentiation of normal from abnormal tissues [5]. One study has suggested that intraoperative sonography overestimates tumor volume, especially when used within the context of recurrent tumors [6]. In contrast, another study has suggested that sonography helps differentiate brain edema, brain tumor, and normal brain [7]. This study evaluates the role of intraoperative ultrasound resection of pediatric brain tumors: defining the shortest access to the mass as well as delineation of the solid and cystic components.
Localization of the tumor, its consistency, and borders with normal brain were studied, followed by a colored mode scanning to identify any close vascular structures, then returning back to B-mode scan to look for any relation of the tumor to nearby anatomical landmarks, like: the ventricles, the tent, and the cerebral aqueduct. After collecting all these data, we start tumor excision from the nearest safe part. As the tumor debulking proceeds, repeated scanning is performed to evaluate the tumor residue and its new relation to surrounding structures. After assuming total excision, another scan is performed after filling the tumor cavity with sterile saline to get an idea about the size of the created cavity and compare it to the original tumor size, and any tumor residue is looked for and excised.
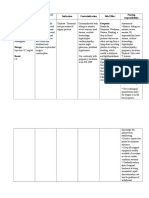
Results Patients and methods Retrospective study of intraoperative ultrasound on 25 inpatients (male/female=13:12, age range 217 years) with brain tumor enrolled between January 1, 2008, and July 30, 2009. All of patients (Table 1) had comprehensively physical and neurological examinations, including MRI before the operation. Ultrasound equipment Intraoperative ultrasound was performed with GE LOGIQ BOOK XP device (General Electric, USA) A 6.5-MHz intraoperative probe was applied. The transducer and cord were placed in a transparent plastic surgical sterile sheath secured at the scan head by a sterile rubber band. For proper transmission of the acoustic beam between the sheathed scan head and the dura mater, irrigation of the operative fieldas neededwith sterile saline was done. Intraoperative scanning After a craniotomy was performed, the radiologist was called to the operating room to help in interpreting the data. First, the sheathed scan head was placed on the surface of the dura mater for scanning before opening the dura where we identify the site and size of the lesion before any brain shift, which could result from CSF drainage after dural opening; the distance from the tumor to the dura mater and the location and size of the tumor were measured and compared with preoperative available MRI images. Dural opening then follows, and the scan head is placed directly to the surface of the brain tissue for further scanning, during which continuous irrigation with saline is performed. Many studies have demonstrated the reliability of intraoperative ultrasound since the 1980s explained by the high resolution and the real-time investigations [8]. In our series, we found reliable tumor localization in all 25 cases without any complications confirming the data of the literature. Tumor localization by intraoperative ultrasound reaches 100% independent of the histopathological diagnoses. Intraoperative conventional ultrasound was useful in the determination of tumor location, its most superficial portion, and in the differentiation between solid tumors and cystic components. The border of the tumor and remained tumor tissue were more distinguishable from healthy brain on ultrasound during the operation which helps in identifying residual tumors after assuming total resection under microscope. Intraoperative ultrasonography (IOUS) was very useful during resection of posterior fossa tumors extending to the lateral parts of the fourth ventricle or upwards to the aqueduct. Improving differentiation of the tumor tissue from normal brain with ultrasound was demonstrated in almost all cases. IOUS was very helpful in posterior fossa, intraventricular, and cortical tumors to ensure total and safe resection, while in craniopharyngiomas, it was helpful in the localization and excision of the cystic component in one case; in the second case, residual solid tumor was identified and excised. Comparing the results of immediate post-op MRI to those from the IOUS (Figs. 1 and 2), we were not surprised by any missed tumor residue that could have been resected.
Discussion Intraoperative US has been used in neurosurgery for more than 20 years, and it still has many attributes that make it
Childs Nerv Syst (2010) 26:11891193 Table 1 Demographic and clinical characteristics of study patients Patients Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case Case 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Age (years) 12 1.4 2 2.5 2.8 2.8 3.3 3.6 5.1 5.9 6.5 6.6 6 8 9 9 7 9.3 9.4 11.1 6 13 14.9 15 17 Degree of resection STR GTR GTR STR GTR GTR GTR STR STR STR GTR STR GTR GTR STR GTR STR GTR GTR STR STR GTR GTR STR GTR Gender M M M F M F F F M F M F M M M M M F F F F M F M F Diagnosis Craniopharyngioma Pineoblastoma Meningioma GBM MB, classic Dermoid cyst MB, classic Pilocytic astrocytoma Immature teratoma GBM MB, large cell Pilocytic astrocytoma Craniopharyngioma Pilocytic astrocytoma MB, classic MB, classic Fibrillary astrocytoma Cellular ependymoma Fibrillary astrocytoma Pilomyxoid astrocytoma Anaplastic astrocytoma Choroided glioma GBM Pilocytic astrocytoma MB, large cell Location
1191
Suprasellar mass Posterior fossa Posterior fossa Right temporal lobe Posterior fossa Posterior fossa Posterior fossa Posterior fossa Posterior fossa Right temporal region Posterior fossa Posterior fossa Suprasellar mass Posterior fossa Posterior fossa Posterior fossa Right temporal lobe Posterior fossa Posterior fossa Posterior fossa Frontal lobe Intraventricular glioma Left parietal lobe Posterior fossa Posterior fossa
GTR gross total resection, STR subtotal resection, M male, F female, GBM glioblastoma multiforme, MB medulloblastoma
attractive for neurosurgical guidance [9]. Ultrasound is very useful in determination of the tumor location, its most superficial portion, and in differentiation between solid tumors and cystic components [10]. Ultrasound examination of the brain and spinal cord is hindered by the absence of an adequate acoustic window. Other important limitations of ultrasound are the necessity of a tradeoff between frequency range, spatial resolution, and tissue penetration of acoustic waves, not to mention that ultrasound is an operator-dependent technique. After removal of skeletal acoustic barriers, intraoperative ultrasound examination of the CNS has been suggested in the identification and characterization of brain and spinal cord lesions [11]. The precise localization provided by ultrasound imaging shortens the time of surgery and increases the safety for the patient [12]. Like intraoperative magnetic resonance imaging, intraoperative US can be used to detect any intraoperative or post-craniotomy brain shifts. IOUS can simply track a biopsy needle in real time and define cysts, ventricles, cisterns, and other fluid-filled spaces. The borders of the
tumors are generally simple to define, and, although the borders of low-grade gliomas may be hard to identify, they are also frequently difficult to define by the magnetic resonance imaging. In addition, US during neurosurgery have some definite advantages over MR imaging: above all, the imaging investigations are in real time. By practice, it becomes very easy for neurosurgeons to scan the brain and look for lesions [13]. The most critical drawback in ultrasound detection of tumor borders is peritumoral edema, which appears echogenic relative to the surrounding brain [14, 15]. Surgical trauma may lead to minor hemorrhages along the cavity borders, thus making the defining of edema even more complicated. In this case, we depend on the microscopic differentiation between the brain and tumor tissue, together with comparing the size of the created cavity after resection to that before resection. In case of solid tumors, the cavity created after resection was filled with saline to compare the size of the saline-filled cavity to the pre-resection tumor size which can give us a clue about the extent of resection, and if the normal
1192 Fig. 1 Intraoperative ultrasound and pre- and postoperative magnetic resonance imaging on a 9-year-old male patient with classic medulloblastoma (case 16)
Childs Nerv Syst (2010) 26:11891193
a. Magnetic resonance imaging (T1 with contrast) pre-operative
b. Magnetic resonance imaging (T1 with contrast) post-operative
c. Ultrasound imaging pre-resection
brain borders were violated during tumor resection, this was very useful especially in benign or wellcircumscribed tumors or in tumors inside a ventricle as lateral and 4th ventricular tumors, but in case of
d. Ultrasound imaging post-resection
malignant gliomas, it is usually difficult to differentiate between hyperechogenicity due to surrounding edema or tumor infiltration or residue which is also the case in MRI.
Fig. 2 A 13-year-old male patient with intraventricular chordoid glioma (case 22). Magnetic resonance image T1 with contrast preoperative (left) and postoperative (right)
Childs Nerv Syst (2010) 26:11891193
1193
Furthermore, the use of Surgicel in the tumor cavity may interfere with interpretation of the IOUS. Surgicel is a gauzelike surgical hemostat composed of oxidized regenerated cellulose [16]. The air trapped between the interwoven fibers of cellulose leads to ring-down artifact, with deleterious effects on the sonographic image. This was avoided by performing the sonography before inserting the surgicel. In all 17 cases of infratentorial tumors and three cases of supratentorial tumors, the IOUS was a very useful tool to guide us for total tumor excision and identify any tumor residue intraoperative which was confirmed by the MRI performed immediately postoperative within the following 48 h, showing that IOUS in such cases can substitute the intraoperative MRI, thus decreasing the length of the operation and making it more simple with less cost effect. In the other five cases of supratentorial gliomas, it was not easy to differentiate between hyperechogenicity due to tumor residue or that from brain edema and surgical trauma; when comparing this to the immediate postoperative MRI, it was similar difficulty that we face indicating that intraoperative MRI is not far more superior than IOUS in such cases. IOUS was introduced in our operating room since January 2008, and we were using it since that time in certain random cases without selection to identify its value and get an idea about which cases could benefit from using IOUS; since then, it is routinely used in all our cases, as it always adds to our preoperative knowledge about the tumor without any further cost or time.
ultrasound presents as a practical and cost affordable alternative in most of pediatric brain tumors.
References
1. American Cancer Society (2009) American Cancer Society Cancer Facts & Figures. American Cancer Society, Atlanta 2. Orkin SH, Fisher DE, Thomas Look A, Lux S, Ginsburg D, Nathan DG (2009) Oncology of infancy and childhood. Elsevier, Amsterdam. ISBN 978-1-4160-3431-5 3. Baltuch GH, Bushnell C, Caplan LR, Stacy MA, Tuszynski MH (2007) Brain tumors: practical guide to diagnosis and treatment. Informa Healthcare, New York. ISBN 10-0-8493-3616-3 (Hardcover) 4. He W, Jiang XQ, Wang S, Zhang MZ, Zhao JZ, Liu HZ, Ma J, Xiang DY, Wang LS (2008) Intraoperative contrast-enhanced ultrasound for brain tumors. Clin Imaging 32:419424 5. Shinoura N, Takahashi M, Yamada R (2006) Delineation of brain tumor margins using intraoperative sononavigation: implications for tumor resection. J Clin Ultrasound 34:177183 6. LeRoux PD, Berger MS, Ojemann GA et al (1989) Correlation of intraoperative ultrasound tumor volumes and margins with preoperative computerized tomography scans: an intraoperative method to enhance tumor resection. J Neurosurg 71:691 7. LeRoux PD, Winter TC, Berger MS et al (1994) Comparison between preoperative magnetic resonance and intraoperative ultrasound tumor volumes and margins. J Clin Ultrasound 22:2936 8. Regelsberger J, Lohmann F, Helmke K, Westphal M (2000) Ultrasound-guided surgery of deep seated brain lesions. Eur J Ultrasound 12:115121 9. Rubin JM, Mirfakhraee M, Duda EE, Dohrmann GJ, Brown F (1980) Intraoperative ultrasound examination of the brain. Radiology 137:831832 10. Di Rocco C (2009) Cerebellar astrocytomas. Childrens Cancer Hospital Egypt, Cairo. Accessed at www.57357.com, 1st CCHE International Pediatric Oncology Conference 11. Cellerini M, Innocenti P, Milazzotto M, Bartolucci M, Guizzardi G, Mennonna P (2001) Intra-operative ultrasound of brain and spinal cord lesions. Radiography 7:5560 12. Chandler WF, Rubin JM (1987) The application of ultrasound during brain surgery. World J Surg 11(5):558569 13. Rubin JM, Quint DJ (2000) Intraoperative US versus intraoperative MR imaging for guidance during intracranial neurosurgery. Radiology 215:3 14. Johnson P, Hart S, Drayer B (1989) Human cerebral gliomas: correlation of postmortem MR imaging and neuropathologic findings. Radiology 170:211217 15. Rubin JM, Chandler WF (1998) Intraoperative sonography of the brain. In: Rumack CM, Wilson SR, Charboneau JW (eds) Diagnostic Ultrasound. Mosby, St. Louis, pp 631652 16. Melamed JW, Paulson EK, Kliewer MA (1995) Sonographic appearance of oxidized cellulose (Surgicel): pitfall in the diagnosis of postoperative abscess. J Ultrasound Med 14:2730
Conclusion In contrast to intraoperative MRI, intraoperative IOUS is less time-consuming, simpler, and less expensive. It allows monitoring the progress of neurosurgical procedure and even of the brain tumor resection during surgery. Thus, intraoperative intracranial ultrasound is suggested to be a useful imaging technique in defining the border between the tumor and healthy brain tissue pre-resection and in detecting residual tumor tissues after the resection of the mass. In comparison to intraoperative MR imaging which is not affordable for most hospitals considering the primary costs including nonferromagnetic tools and the time-consuming investigations,
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- What Is Caffeine? How Does Caffeine Work?Document16 pagesWhat Is Caffeine? How Does Caffeine Work?Agustinus SiswantoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Defining-Critically Ill-Icu SummaryDocument33 pagesDefining-Critically Ill-Icu SummaryNetNo ratings yet
- IsoketDocument2 pagesIsoketJaessa FelicianoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- High Volume HDF - Scientific Brochure - EN - 01oct2018 - Approved - Original - 112Document2 pagesHigh Volume HDF - Scientific Brochure - EN - 01oct2018 - Approved - Original - 112HARUMUKIZA Jean DomitienNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- General AnaestheticsDocument71 pagesGeneral AnaestheticsTamilarasanNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- ANEXA Nr. 9 Certificat Medical Medical Fitness CertificateDocument1 pageANEXA Nr. 9 Certificat Medical Medical Fitness CertificatePrisacaru MarianNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Cyanosis Definition of Cyanosis in The MedicalDocument4 pagesCyanosis Definition of Cyanosis in The MedicalTavish B PrasadNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- For Health & Wellness: Magnetic Therapy 101Document3 pagesFor Health & Wellness: Magnetic Therapy 101rodonetNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Medical Image Analysis - Overview - NewDocument11 pagesMedical Image Analysis - Overview - Newedi pNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- MCQs in para (With Answers)Document20 pagesMCQs in para (With Answers)janiceli020785% (26)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Bird Mark 7A Respirator BrochureDocument2 pagesBird Mark 7A Respirator BrochureLos Infantes Ska Jazz100% (4)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- RS5573 FONA 1000S User Manual 6476381 Ver2 201604 EN CN Reg SADocument36 pagesRS5573 FONA 1000S User Manual 6476381 Ver2 201604 EN CN Reg SAJuan carlos Isaza gNo ratings yet
- Maternal and Child HealthDocument60 pagesMaternal and Child HealthStar AcademyNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Fre Orto 3Document4 pagesFre Orto 3PutriNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Thyroid Eye Disease Diagnosis and TreatmentDocument486 pagesThyroid Eye Disease Diagnosis and TreatmentUnsmil UnguNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- MAPEH 9 PE and Halth 2nd Quarter Examination FinalDocument2 pagesMAPEH 9 PE and Halth 2nd Quarter Examination Finalcecile80% (10)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Legal Aspects of MedicationDocument17 pagesLegal Aspects of MedicationRitaNo ratings yet
- Etiology of Diabetes Mellitus PDFDocument2 pagesEtiology of Diabetes Mellitus PDFAdamNo ratings yet
- Schedule of Charges - April 2015Document69 pagesSchedule of Charges - April 2015Chocolete HeartNo ratings yet
- Test Bank For Pharmacology and The Nursing Process 9th by LilleyDocument6 pagesTest Bank For Pharmacology and The Nursing Process 9th by LilleyJames Philhower100% (30)
- Sodium Bicarbonate: PresentationDocument3 pagesSodium Bicarbonate: Presentationmadimadi11No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CLICO Group Health and Life Coverage 1Document12 pagesCLICO Group Health and Life Coverage 1buckianNo ratings yet
- A Simple Approach To Shared Decision Making in Cancer ScreeningDocument6 pagesA Simple Approach To Shared Decision Making in Cancer ScreeningariskaNo ratings yet
- NCP - Gestational DiabetesDocument2 pagesNCP - Gestational DiabetesKailah Rose CabantoyNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Women S Health MidtermDocument30 pagesWomen S Health MidtermKatarzyna CiesielskaNo ratings yet
- Concept PaperDocument12 pagesConcept Paperjlventigan100% (1)
- Purposive Communication - Writer: John Melvin Ibarra Type of Essay: Persuasive Instructor: Ms. Fhe de CastroDocument2 pagesPurposive Communication - Writer: John Melvin Ibarra Type of Essay: Persuasive Instructor: Ms. Fhe de CastroVincent Maralit Material100% (1)
- Somatic RecombinationDocument5 pagesSomatic RecombinationNoor Ul NaeemNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- 2926 Getinge Da Vinci Brochure 190301 en NonusDocument5 pages2926 Getinge Da Vinci Brochure 190301 en NonusHELIONo ratings yet
- Schizophrenia and Other Psychotic DisordersDocument85 pagesSchizophrenia and Other Psychotic DisordersEsraRamosNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)