Cardiac Monitoring Notes
Patient Care III
MI 211c
Cardiac Monitoring
Cardiac Conduction Cycle
- Provides electrical stimulus to cause the heart muscle to continually
Contract (systole)
Relax (diastole)
- SA node
- AV node
- Bundle of His
- Bundle Branches
- Purkinje Fibers
- Electrical impulses cause each myocardial cell to:
1) Change from a resting (polarized) state
2) To a state of contraction (depolarized)
3) Back to a resting state by recharging (repolarized)
1
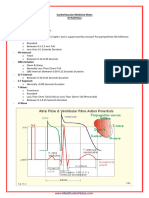
� Cardiac Conduction Cycle Electrophysiology
- Heart cells (myocytes) are capable of conductivity, excitability, contractility, and
automaticity
- Myocytes influenced by Na+, Ca2+, and K+
- At rest – cells polarized
Cell interior negatively charged
Charge builds up until threshold is reached
- Na+ ions flood into the cell, followed by Ca2+ ions – cells depolarized
Cell interior becomes more positive than outside
Followed by mechanical event = contraction
- K ions move out of the cell – cells repolarized
+
Interior cell charge transitions to be more negative
Cardiac Conduction Cycle
Electrocardiogram
- An electrical picture of the heart measured externally
Ability to do so discovered in mid-1880’s
- ECG vs. EKG
Dr. Willem Einthoven, 1901
- Labeled with letters
P, Q, R, S, T, U
Letters correspond to events in the cardiac cycle
2
� Electrocardiogram
Cardiac Cycle Waves
- P-wave
- QRS complex
- T-wave
- U-wave
Cardiac Cycle Waves Description Image
Atrial depolarization -
Contraction
Location - Precedes the QRS
complex
Amplitude - Not more than
0.25 mV (2-2.5 boxes)
Duration - 0.06-0.11 seconds
P-Wave
Appearance - Rounded and
upright
3
� Ventricular depolarization -
Contraction
Location - Follows the PR
interval
Amplitude - Variable with
ECG lead
QRS Complex Duration - <0.12 seconds
Appearance - 3 waves
Ventricular repolarization -
Return to resting state
Location - Follows the S wave
Amplitude - 0.5 mV or less
Duration - Not measured
Appearance - Rounded and
smooth
T-Wave
His-Purkinje repolarization -
Return to resting state
Location - Follows the T wave
Amplitude - Not measured
Duration - Not measured
U-Wave Appearance - Upright and
rounded
4
� Cardiac Cycle Waves
- PR Interval
Beginning of the P-wave to the beginning of the QRS complex.
• Beginning of atrial depolarization to the beginning of ventricular
depolarization
• 0.12 - 0.2 sec duration
- ST segment
End of the S-wave to the beginning of the T-wave
Represents the end of ventricular depolarization and the beginning of
ventricular repolarization
Duration
- Not Measured QT Interval
Beginning of the Q wave to the end of the T Wave
Time from ventricular depolarization to ventricular repolarization
Duration
• 0.36 - 0.44 seconds duration
- RR Interval
Distance from one R-wave to the next
Used to determine if rhythm is regular
Cardiac Cycle Waves
5
� Interpreting Rhythm Strips
a. Step 1:
Determine the rates
• Atrial rate = P waves per 6s x 10
• Ventricular rate = QRS complex (R waves) per 6s x 10
b. Step 2:
Assess regularity of rhythm (20 – 30 s)
• Atrial = P wave to P wave
• Ventricular = R wave to R wave
c. Step 3:
Assess atrial activity
• Compare appearance and configuration of P waves
o Present?
o Normal shaped?
o Position?
d. Step 4:
Determine the duration of the PR interval
• Is it WNL?
o 0.12 - 0.20 sec
• Is there one P wave for each QRS complex?
e. Step 5:
Determine the duration of the QRS complex
• Size and shape
• Duration (0.04 - 0.11 sec)
• Distance from T-wave
• Point in same direction
f. Step 6:
Evaluate the T-wave
• Present
• Size and Shape
• Point in same direction as QRS complex
g. Step 7:
ST segment flat on isoelectric line
6
�Part II
What is expected of you?
- Recognize normal sinus rhythms
- Be observant for signs and symptoms
- Respond appropriately
Calm, reassuring attitude
Assess vital signs
Elevate patient’s head
Be prepared to administer oxygen
Be prepared for IV drug administration
Be prepared to call a CODE
Recognize Common ECG Abnormalities
- Sinus Bradycardia -Ventricular Fibrillation
- Sinus Tachycardia - Atrial Fibrillation
- Ventricular Tachycardia - Atrial Flutter
- Premature Ventricular Contractions (PVCs) - Heart Block
Bradycardia vs. Tachycardia
- Bradycardia
Slow heart rate
<60 beats/min
- Tachycardia
Fast heart rate
>100 beats/min
Bradycardia
Tachycardia
7
� Ventricular Tachycardia
- Hear rate between 150-250 bpm
- Low Cardiac output
Pt. lose consciousness
Becomes hypotensive
- Solution:
Amiodarone via IV
May need to use defibrillator
Premature Ventricular Contractions
- PVCs
A ventricular contraction preceding the normal impulse initiated by the SA
node.
May occur singly, in pairs or in threes
- ECG Characteristics
Rhythm: irregular
P-wave: Absent
QRS complex
• Bizarre configuration
• Occurs early
- Causes:
Caffeine, tobacco, alcohol ingestion, exercise, scarring from MI’s, foreign
body ‘tickling’ the heart
- Signs/Symptoms:
Asymptomatic
Palpitations
Decreased cardiac output
Ventricular Fibrillation
- Chaotic, irregular contractions of the
ventricles
- Waves are jagged
- Life threatening
- Ventricles fail to pump blood
- Leads to asystole and death
- ECG Characteristics:
normal parameters not measurable
- Causes:
Acute MI
Electric Shock
Untreated Tachycardia
Electrolyte Imbalance
Hypothermia
8
� Ventricular Fibrillation CONT.
- Symptoms
Absent Pulse and BP
Loss of Consciousness
Cyanosis
- Treatment
CPR
Defibrillation
Epinephrine
Atrial Fibrillation
- Both atria and ventricles contracting
rapidly
- Atrial and ventricular rhythms
irregular
- May lead to PE or stroke
- Symptoms
Palpitations
Nausea
Weakness & Fatigue
- Treatment
Slow the ventricular response.
Increase cardiac output
Atrial Flutter
- Rapid, but regular contractions of the
atria
- Waves are rounded
- Atrial rate 250 – 400 beats/minute
- ECG Characteristics
P-wave: Absent
• Flutter waves are present
QRS complex: < 0.12 seconds
- Causes:
Valve Disorder
Infection
Alcoholism
Hyperthyroidism
- Symptoms
Chest pain
SOB
Hypotension
9
� Heart Block
- An interference of the
normal electrical
conduction of the heart
- Defined by the location of
the block
A-V Heart Block
- Symptoms
SOB
Chest pain
Hypotension & lightheadedness
10