Professional Documents
Culture Documents
Medical Records Completion Guidelines
Uploaded by
idno1008Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Records Completion Guidelines
Uploaded by
idno1008Copyright:
Available Formats
Medical Records Completion Guidelines I. Admit Checklist II. Allergies Listed A. H&P sheet 1. Timeliness 2.
History sheet should be completed. If patient has pain, please do the pain scoring. 3. Examination findings should be completed 4. Nutritional screen should be completed by doctors and adequate referrals be send as required 5. Functional screen should be completed by doctors and adequate referrals be send as required 6. Discharge plan should be completed. In cases where discharge plan is superfluous, kindly mention discharge criteria, fulfilling which patient may be discharged. 7. Treatment plan should be completed 8. Legibility kindly write in legible handwriting. 9. Accuracy Wherever you need not write details, use approved abbreviations like No Abnormality Detected (NAD), Not Applicable (N/A) etc. 10. Date written Date your documentation 11. Time written Time has to be documented, it is mandatory. 12. Consultant Sign in History & Physical Form is mandatory. B. Nursing Admission Assessment 1. Timeliness 2. Completeness 3. Legibility C. Consent 1. Completeness Treating physician should obtain consent. Each consent process must involve information about a) the patients condition; b) the proposed treatment(s); c) the name of the person providing the treatment; d) potential benefits and drawbacks; e) possible alternatives; f) the likelihood of success; g) possible problems related to recovery; and h) possible results of non treatment. 2. Legibility 3. Date 4. Sign Consultants signature in consent forms are highly desirable, (exception , General Consent, Blood Transfusion Consent) 5. Witness
D. Nutrition Form A (Dietician) 1. Completeness 2. Legibility 3. Accuracy E. Nutrition Form B (Dietician) 1. Completeness 2. Legibility 3. Accuracy F. In house Transfer Form 1. Medical Reconciliation 2. Completeness 3. Accuracy G. Consultant Referral Form 1. Completeness 2. Date & Time 3. Referral Notes should only be written in the Consultant Referral Form. 4. Consultant Referral Form should be placed alongside the progress note on the date referral was first made. H. Restraint Form 1. Completeness 2. Consent for restraint 3. Type of Restraint 4. Family Educated I. Anesthesia Assessment 1. Completeness 2. Anesthesia Consent Ideally all anesthesia consent shall be documented during the PAC. Consent shall be taken by person conducting PAC 3. Pre-Op Check Documented 4. Pre Operative Vitals Documented 5. Pre induction checklist 6. Operative Anesthesia Records Completion 7. Recovery Room (RR) records have to be completed before the patient is wheeled out of the RR. 8. Consultant Signature, Date & Time are mandatory. J. Operation Theater Record 1. Legibility 2. All sections have to be filled up properly. 3. Please note the Start Time and End Time (Tourniquet Time) wherever applicable. 4. Pre and Post (Peri) Operative Diagnosis (not Histopathology) have to be mentioned 5. Complications or no complications - mention 6. Completed before transfer out of recovery K. Progress Notes Must Do 1. Completeness
2. Legibility 3. Written daily In critical care areas, review patient and document the findings as per the laid down norms in Critical Care Manual 4. Effect of medication shall be documented 5. Pain Assessment Pain assessment shall be done during each assessment of the patient and pain score be documented (e.g. 0/10 for No pain) according to the VAS (Visual Analogue Scale). In any patient, if the pain scores are on or above 3/10; please provide a plan for pain management. 6. Care Plan shall be written at least once in 24 hours 7. Patient education shall be written in the progress note , including education about diagnosis, treatment and outcomes. Must Avoid 1. Avoid writing instructions in the Progress note ( Doctors Instruction Sheet) 2. Avoid writing the Cath Lab, OT & Endoscopy notes in the Progress notes ( separate forms are available for this purposes) 3. Avoid taking consent of patient & patients family member in their handwriting in progress notes. (Is not a necessity in Court of Law) 4. Avoid writing notes in progress notes as a referral physician or consultant. L. Nursing Notes 1. Completeness 2. Legibility 3. Effect of medication 4. Pain Assessment 5. Care plan written M. Blood Transfusion Notes 1. Consent shall be completed 2. Assessment during transfusion done 3. Duration of transfusion mentioned N. Physiotherapy Assessment 1. Completeness 2. Timeliness 3. Accuracy O. Doctors Instruction Sheet 1. ALL non drug orders written here 2. Legibility 3. Orders Dated by doctors 4. Orders Timed by doctors 5. Write verbal reports of the Lab, and Critical Test Results in Critical Test Result reporting form. P. Medication Chart 1. Write Weight, Allergies etc. 2. Legible / Capital Only for the Drug 3. Mention Injection or Oral 4. Mention Dose
5. Mention Route 6. Mention Frequency 7. When a medication has any change in Dose, Route & Frequency, Write STOP , and write a fresh order 8. For STAT and SOS orders, please write when and why it is given. 9. Doctors signature & time is must 10. Nurses signature & time is must on administration 11. Pharmacist should sign following verification of medicines 12. On 4th page, write name and signature Q. IDTR & Patient education sheet 1. Assessment 2. Completeness 3. Timeliness 4. Educate patient and document R. Discharge Checklist Completeness S. Discharge Summary Contents Reason for admission, Significant findings, Any diagnosis, Any procedures performed, Any medication and treatment, Condition upon discharge, Discharge Medication Follow up instructions If applicable, Stop Smoking Counseling 1. Condition of patient documented 2. Intra-hospital medication documented 3. Physical activity advice documented 4. Diet advice documented 5. Other non-drug advice documented 6. Completeness 7. Accuracy
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Severe and Multiple DisabilitiesDocument18 pagesSevere and Multiple DisabilitiesKavi Rehabian100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Spirit Releasement Protocol ListDocument4 pagesSpirit Releasement Protocol ListKristen Hammer100% (5)
- Diabetes EvaluationDocument3 pagesDiabetes Evaluatione-MedTools100% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Important Question For Dialysis TechnicianDocument7 pagesImportant Question For Dialysis Technicianhunbaitmiki hinge100% (1)
- The Fitness Project 2018Document34 pagesThe Fitness Project 2018San joe50% (2)
- Peter Pan Syndrome Is A DeepDocument3 pagesPeter Pan Syndrome Is A DeeptucklertNo ratings yet
- Compilation of Nutri Ed ProgramsDocument5 pagesCompilation of Nutri Ed ProgramsDarwell Chann RosalesNo ratings yet
- Practice HPIDocument3 pagesPractice HPImedicalmatins100% (1)
- Therapeutic Modalities: Prepared By: John Patrick B. de JesusDocument22 pagesTherapeutic Modalities: Prepared By: John Patrick B. de JesusChiee A. CentinoNo ratings yet
- Test Bank For Counseling and Psychotherapy Theories in Context and Practice Skills Strategies and Techniques 3rd Edition John Sommers Flanagan Rita Sommers FlanaganDocument17 pagesTest Bank For Counseling and Psychotherapy Theories in Context and Practice Skills Strategies and Techniques 3rd Edition John Sommers Flanagan Rita Sommers Flanagancuthbertfinncx2nNo ratings yet
- Recurrent MeningitisDocument14 pagesRecurrent Meningitisidno1008No ratings yet
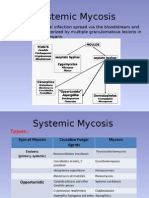
- MycosisDocument5 pagesMycosisMaiWahidGaberNo ratings yet
- Pathogenesis, Diagnosis and Treatment of Rasmussen EncephalitisDocument20 pagesPathogenesis, Diagnosis and Treatment of Rasmussen Encephalitisidno1008No ratings yet
- New Drugs For Epilepsy Mangement 1Document48 pagesNew Drugs For Epilepsy Mangement 1idno1008No ratings yet
- To Whom It May ConcernDocument1 pageTo Whom It May Concernidno1008No ratings yet
- Dr. ShahriarDocument1 pageDr. Shahriaridno1008No ratings yet
- EEG1Document13 pagesEEG1idno1008No ratings yet
- Musa IbrahimDocument3 pagesMusa Ibrahimidno1008No ratings yet
- Farzana ApuDocument1 pageFarzana Apuidno1008No ratings yet
- Admin Protocol AhdDocument1 pageAdmin Protocol Ahdidno1008No ratings yet
- Department of NeuromedicineDocument4 pagesDepartment of Neuromedicineidno1008No ratings yet
- Aseptic MeningitisDocument24 pagesAseptic Meningitisidno1008100% (1)
- Activities of Neuromedicine DepartmentDocument2 pagesActivities of Neuromedicine Departmentidno1008No ratings yet
- CIDPDocument21 pagesCIDPidno1008No ratings yet
- Daily StarDocument3 pagesDaily Staridno1008No ratings yet
- What To Do, When Gbs PT Fails To Respond To TreatmentDocument4 pagesWhat To Do, When Gbs PT Fails To Respond To Treatmentidno1008No ratings yet
- ParkinsonsDocument2 pagesParkinsonsidno1008No ratings yet
- Vestibular Rehabilitation ExercisesDocument1 pageVestibular Rehabilitation Exercisesidno1008No ratings yet
- StrokesDocument1 pageStrokesidno1008No ratings yet
- MigraneDocument1 pageMigraneidno1008No ratings yet
- Neck Exercises1Document3 pagesNeck Exercises1idno1008No ratings yet
- DementiaDocument1 pageDementiaidno1008No ratings yet
- Tugas Bahasa InggrisDocument14 pagesTugas Bahasa InggrisAlfin MT16No ratings yet
- CVC - B Braun - CertofixDocument14 pagesCVC - B Braun - CertofixMargaretta LimawanNo ratings yet
- Coagulation Profile in Diabetes MellitusDocument5 pagesCoagulation Profile in Diabetes MellitusAsfandyar RoghaniNo ratings yet
- Wastewater Disposal.Document266 pagesWastewater Disposal.FarazNo ratings yet
- By Sweta Kumari Summer Project-II Submitted ToDocument22 pagesBy Sweta Kumari Summer Project-II Submitted ToSudarshanKumar0% (1)
- The Tylenol Crisis: How Effective Public Relations Saved Johnson & JohnsonDocument11 pagesThe Tylenol Crisis: How Effective Public Relations Saved Johnson & JohnsonMuhamad LutfilahNo ratings yet
- Olympian Benchmark - 400mDocument15 pagesOlympian Benchmark - 400merwandumontNo ratings yet
- Case No 1:-Bio DataDocument8 pagesCase No 1:-Bio DataSarah Saqib Ahmad100% (1)
- Stroke Pathophysiology 1Document5 pagesStroke Pathophysiology 1Jeco ValdezNo ratings yet
- Congenital DiseaseDocument39 pagesCongenital DiseaseRavi SharmaNo ratings yet
- Status AsthmaticusDocument5 pagesStatus AsthmaticusHimmzNo ratings yet
- CTTDocument47 pagesCTTleizelgalvezNo ratings yet
- B PharmacyDocument26 pagesB PharmacyAkankshaNo ratings yet
- Reiki, Medicine & Self-Care With Pamela Miles: "Try Reiki" - Dr. Mehmet OzDocument10 pagesReiki, Medicine & Self-Care With Pamela Miles: "Try Reiki" - Dr. Mehmet OzSuresh NarenNo ratings yet
- Dream Abstracts PDFDocument61 pagesDream Abstracts PDFAlice Gina100% (1)
- LFS 233:module 5 Fats: College of Health Sciences Integrated Sciences DepartmentDocument65 pagesLFS 233:module 5 Fats: College of Health Sciences Integrated Sciences DepartmentHussain Ali100% (1)
- Lactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonDocument15 pagesLactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonArrianne AcopNo ratings yet
- A Comparative Study of Nutritional Status of Children Aged 11-14 Years of Low and High Economical Background, SuratDocument4 pagesA Comparative Study of Nutritional Status of Children Aged 11-14 Years of Low and High Economical Background, SuratEditor IJTSRDNo ratings yet
- Evaluation of The Health Beneficial Properties of The Aromatic Ether Myristicin, A Volatile Oil Derived From Various Plants SourcesDocument17 pagesEvaluation of The Health Beneficial Properties of The Aromatic Ether Myristicin, A Volatile Oil Derived From Various Plants SourcesIndra syahputraNo ratings yet