Professional Documents
Culture Documents
Managing ..
Managing ..
Uploaded by
Janine Katherine BejaranoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Managing ..
Managing ..
Uploaded by
Janine Katherine BejaranoCopyright:
Available Formats
ReviewArticle
Managing chromoblastomycosis
Mahreen Ameen
MRCP MD
St Johns Institute of Dermatology, Guys and St. Thomas Trust, London SE1 7EH, UK Correspondence to: Mahreen Ameen, St Johns Institute of Dermatology, Guys and St. Thomas Trust, London SE1 7EH, UK Email: mahreenameen@hotmail.com TROPICAL DOCTOR 2010; 40: 65 67 DOI: 10.1258/td.2009.090264
consist of only a single papule or nodule. Over years they enlarge, forming plaques with a characteristic verrucous appearance (Figure 1). Disease is usually localized but satellite lesions can develop as a result of autoinoculation from scratching or from lymphatic dissemination. As lesions extend they leave areas of sclerotic or keloidal scarring. Complications include secondary bacterial infection, ulceration, secondary lymphoedema, and, rarely, the development of squamous cell carcinoma. Lymphoedema itself can predispose to attacks of cellulitis. Extension of infection to underlying muscle and bone is rare and usually only occurs in association with immunosuppression.2,4 The principal differential diagnosis of chromoblastomycosis in the Tropics is verrucous variants of tuberculosis, sporotrichosis and leishmaniasis.
SUMMARY Chromoblastomycosis is a subcutaneous fungal infection caused by the traumatic inoculation of the skin with pigmented saprophytic moulds. Although infection is rarely fatal, it is characteristically chronic and can be complicated by lymphatic damage and malignant transformation. Despite a variety of treatment modalities, which are often combined and include long courses of antifungals, surgical excision and destructive physical therapies, it remains one of the most difficult deep mycotic infections to eradicate.
Diagnosis
The clinician can conrm the diagnosis easily by direct microscopy of a scraping taken from the characteristic black dots visible on the surface of skin lesions (Figure 1). These black dots represent transepidermal elimination of fungae. A positive direct examination of scrapings in 10% potassium hydroxide will demonstrate thick-walled, multiseptate, brown sclerotic cells that are pathognomonic of chromoblastomycosis, irrespective of the causative species (Figure 2). These are known alternatively as copper pennies, Medlar bodies or muriform cells. The fungal agents are typically slow-growing and culture may be inconclusive due to poor morphological differentiation. Polymerase chain reaction (PCR) has been developed for the identication of Fonsecaea and Cladophialophora carrionii.5,6 Serological tests such as ELISA can be useful in evaluating therapy response, but like PCR it is not widely available in most endemic settings.7 A biopsy demonstrates the typical sclerotic bodies within a granulomatous inltrate (Table 2).
Epidemiology and aetiology
The pigmented (dematiaceous) fungi responsible for chromoblastomycosis are prevalent worldwide but infection is more common in the Tropics, with particular foci in India, Madagascar, Brazil, Venezuela, Mexico and the Dominican Republic. The most common aetiological agents are of the genera Fonsecaea, Phialophora and Cladophialophora, which are found as saprophytes in soil and plants. Fonsecaea pedrosoi is the most common agent found in tropical forests, such as the Amazon, as well as temperate regions of Latin America. Cladophialophora carrionii is the most important agent in dry countries and desert regions such as Australia, South Africa and Cuba (Table 1).1,2
Treatment
Cure rates for chromoblastomycosis are low and range from 15% to 80%. Chronic and extensive disease is particularly
Table 1 Principal causative agents of chromoblastomycosis1
Clinical presentation
Chromoblastomycosis has a propensity to affect those who are barefoot, particularly agriculturists and labourers, and has a male and lower socioeconomic class predominance. The distal limbs are most commonly affected, although unusual body sites such as the genitalia and nose have also been described.3 Disease progression is extremely slow and usually asymptomatic. Therefore, patients often seek medical treatment many years, or even decades, after acquiring the infection and developing skin lesions. Early lesions
Fonsecaea pedrosoi
Cladophialophora carrionii Phialophora verrucosa Exophiala jeanselmei Exophiala spinifera Rhinocladiella aquaspersa
Most common species worldwide (70 90%) Tropical rainforests and temperate regions Second most important species worldwide Endemic in dry and desert regions Also causes phaeohyphomycosis Rare agents of chromoblastomycosis
Tropical Doctor
April 2010, 40
65
Review Article
Table 2 Investigations for chromoblastomycosis
Direct microscopy Culture (species identication) Histopathology PCR (species identication) ELISA Rapid Easy to perform Sample taken from black dots Slow May fail or be inconclusive Often not necessary with characteristic clinical presentation in endemic area and positive microscopy Rapid and sensitive Useful when culture fails Not available in many endemic regions For monitoring response to treatment Not commonly used
Figure 1 Verrucous plaque over elbow with characteristic black dots
resistant to treatment. In addition, F. pedrosoi, the most common aetiological agent of chromoblastomycosis, is less sensitive to antifungal chemotherapy than C. carrionii or P. verrucosa.8 The goal of treating small and early lesions should be cure. However, in the case of extensive infection a more realistic goal might be to reduce disease, control spread and prevent complications. Clinical cure is dened as complete resolution of lesions with scarring, and mycological cure is dened as negative microscopy and culture. Drug therapy consists of long courses of high dose antifungals. Unfortunately, there are no comparative trials of their use in chromoblastomycosis. First-line agents are itraconazole (200 400 mg daily) and terbinane (500 1000 mg daily), which have both demonstrated good in vitro activity against causative species of chromoblastomycosis.9,10 They are given for a minimum of 612 months, preferably at the higher dose if tolerated.11 13 Pulse itraconazole (200 mg twice daily for one week every month) has demonstrated comparable efcacy to daily itraconazole, and the consequent reduction in its cumulative dose has the dual advantage of reducing risks of long-term drug therapy and bringing
Figure 2 Direct examination in a potassium hydroxide mount of skin scrapings demonstrate characteristic copper pennies (400 magnication)
down its cost.14 Combination therapy with itraconazole and terbinane is recommended if it is affordable.15 It is welltolerated and its enhanced efcacy may be accounted for by its synergistic effects, which have been demonstrated in recent in vitro studies.16,17 Ketoconazole has low efcacy against chromoblastomycosis and cannot be given at high doses for long periods of time because of its hepatotoxic potential.8 Fluconazole and amphotericin B are also not recommended as in vitro studies have shown that it has poor activity against dematiaceous fungi.9 Flucytosine was an early treatment for chromoblastomycosis.18 However, it is highly toxic and is associated with high levels of resistance. It is rarely used now except for the treatment of cases resistant to rst-line agents. The new second generation broad-spectrum triazoles such as posaconazole and voriconazole are promising drugs for treating deep cutaneous mycoses, but experience to date is limited because of their prohibitive costs. A single study demonstrated cure with long-term posaconazole in ve out of six patients with chromoblastomycosis refractory to standard antifungal therapies, and long-term therapy (up to 34 months) was well tolerated.19 Drug therapy should be continued for several months after cure in order to prevent relapse, which is more common for extensive disease. Drug therapy can be combined with surgery or physical destructive treatments such as cryotherapy or thermotherapy. Excision of small, localized lesions with wide surgical margins can be very successful.8 Ideally, antifungal chemotherapy should be given before surgery in order to reduce the size of the lesion, and should be continued afterward to reduce any risk of recurrence. Physical treatment modalities have the advantage that they are inexpensive and easy to administer. They are also a useful option for patients unable to take systemic medication. Cryotherapy, involving the application of liquid nitrogen to lesions, produces low temperatures, which freezes and destroys diseased tissue. Multiple lesions may be treated as tolerated and treatment can be combined with antifungal chemotherapy. Cryotherapy of large lesions is usually done in stages. However, treatment of smaller lesions is usually more successful and sometimes requires only a single application.4,20,21 Thermotherapy involves the application of local heat to produce controlled temperatures ranging from 428C to 458C. Various devices, such as benzene pocket warmers and pocket handkerchief-type warmers, have been used. The few reports of its use originate from Japan and demonstrate high efcacy as monotherapy.22,23 Thermotherapy in combination with antifungals may reduce treatment duration and improve efcacy (Table 3).
66
Tropical Doctor
April 2010, 40
Review Article
Table 3 Treatments for chromoblastomycosis
Drug therapies Itraconazole 200 400 mg Terbinane 500 1000 mg daily Posaconazole 800 mg daily Physical therapies Surgical excision Cryotherapy Heat therapy Given daily or as monthly one week pulse therapy (Refs 11, 14) Can be combined with itraconazole (Refs 12, 13, 15) High efcacy and tolerability but very expensive (Ref. 18) Suitable for single and small lesions Combined with drug therapy Mean of seven treatments required (range 1 22) (Refs 4, 20) 2 6 months daily treatment (Refs 21, 22)
Conclusion
The diagnosis of chromoblastomycosis may be conrmed easily at the rst clinical visit by the direct microscopic examination of scrapings of a suitable skin lesion. Treatment choice must be tailored according to the aetiological agent, extent of disease and its location, and any co-morbidities which preclude long-term antifungal chemotherapy. Combination high-dose intraconazole and terbinane therapy is recommended in conjunction with surgery and cryotherapy of small lesions. References
1 Sanche Se, Sutton DA, Rinaldi MG. Dematiaceous fungi. In: Anaissie EJ, McGinnis MR, Pfaller MA, eds. Clinical Mycology. New York: Churchill-Livinstone, 2003;32551 2 Lupi O, Tyring SK, McGinnis MR. Tropical dermatology: fungal tropical diseases. J Am Acad Dermatol 2005;53:931 51 3 Sharma NL, Sharma RC, Grover PS, Gupta ML, Sharma AK, Mahajan VK. Chromoblastomycosis in India. Int J Dermatol 2002;41:162 4 Bonifaz A, Carrasco-Gerard E, Saul A. Chromoblastomycosis: clinical and mycologic experience of 51 cases. Mycoses 2001; 44:17 5 Abliz P, Fukushima K, Takizawa K, Nishimura K. Specic oligonucleotide primers for identication of Cladophialophora carrionii, a causative agent of chromoblastomycosis. J Clin Microbiol 2004;42:404 7 6 de Andrade TS, Cury AE, de Castro LG, Hirata MH, Hirata RD. Rapid identication of Fonsecaea by duplex polymerase chain reaction in isolates from patients with chromoblastomycosis. Diagn Microbiol Infect Dis 2007;57:267 72 7 Oberto-Perdigon L, Romero H, Perez-Blanco M, Apitz-Castro R. An ELISA test for the study of the therapeutic evolution of chromoblastomycosis by Cladophialophora carrionii in the endemic area of Falcon State, Venezuela. Rev Iberoam Micol 2005;22: 3943 [Spanish]
8 Bonifaz A, Paredes-Solis V, Saul A. Treating chromoblastomycosis with systemic antifungals. Expert Opin Pharmacother 2004;5:24754 9 Vitale RG, Perez-Blanco M, De Hoog GS. In vitro activity of antifungal drugs against Cladophialophora species associated with human chromoblastomycosis. Med Mycol 2009;47:3540 10 Caligiorne RB, Resende MA, Melillo PH, Peluso CP, Carmo FH, Azevedo V. In vitro susceptibility of chromoblastomycosis and phaeohyphomycosis agents to antifungal drugs. Med Mycol 1999;37:405 9 11 Queiroz-Telles F, McGinnis MR, Salkin I, Graybill JR. Subcutaneous mycoses. Infect Dis Clin North Am 2003;17:5985 12 Esterre P, Inzan CK, Ramarcel ER, et al. Treatment of chromomycosis with terbinane: preliminary results of an open pilot study. Br J Dermatol 1996;134(Suppl. 46):33 6 13 Bonifaz A, Saul A, Paredes-Solis V, Araiza J, Fierro-Arias L. Treatment of chromoblastomycosis with terbinane: experience with four cases. J Dermatolog Treat 2005;16:47 51 14 Ungpakorn R, Reangchainam S. Pulse itraconazole 400 mg daily in the treatment of chromoblastomycosis. Clin Exp Dermatol 2006;31:245 7 15 Gupta AK, Taborda PR, Sanzovo AD. Alternate week and combination itraconazole and terbinane therapy for chromoblastomycosis caused by Fonsecaea pedrosoi in Brazil. Med Mycol 2002;40:529 34 16 Yu J, Li R, Zhang M, Liu L, Wan Z. In vitro interaction of terbinane with itraconazole and amphotericin B against fungi causing chromoblastomycosis in China. Med Mycol 2008;46: 745 7 17 Zhang JM, Xi LY, Zhang H, et al. Synergistic effects of terbinane and itraconazole on clinical isolates of Fonsecaea monophora. Eur J Dermatol 2009;19:4515 18 Lopez CF, Alvarenga RJ, Cisalpino EO, Resende MA, Oliveira LG. Six years experience in treatment of chromomycosis with 5-uorocytosine. Int J Dermatol 1978;17:4148 19 Negroni R, Tobon A, Bustamante B, Shikanai-Yasuda MA, Patino H, Restrepo A. Posaconazole treatment of refractory eumycetoma and chromoblastomycosis. Rev Inst Med Trop Sao Paulo 2005;47:339 46 20 Bonifaz A, Martinez-Soto E, Carrasco-Gerard E, Peniche J. Treatment of chromoblastomycosis with itraconazole, cryosurgery, and a combination of both. Int J Dermatol 1997;36:542 7 21 Castro LG, Pimentel ER, Lacaz CS. Treatment of chromomycosis by cryosurgery with liquid nitrogen: 15 years experience. Int J Dermatol 2003;42:40812 22 Tagami H, Ginoza M, Imaizumi S, Urano-Suehisa S. Successful treatment of chromoblastomycosis with topical heat therapy. J Am Acad Dermatol 1984;10:615 9 23 Hiruma M, Kawada A, Yoshida M, Kouya M. Hyperthermic treatment of chromomycosis with disposable chemical pocket warmers. Report of a successfully treated case, with a review of the literature. Mycopathologia 1993;122:107 14
Tropical Doctor
April 2010, 40
67
You might also like
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Carbide, Nitride and Boride Material Synthesis and ProcessingDocument674 pagesCarbide, Nitride and Boride Material Synthesis and ProcessingMarcia Gaby Cruz67% (3)
- Introduction To Non Destructive TestingDocument41 pagesIntroduction To Non Destructive Testingkmas161289% (9)
- Preview Chemistry IGCSEDocument76 pagesPreview Chemistry IGCSEAbdulrahman Mosfata0% (1)
- Complexometric TitrationDocument12 pagesComplexometric TitrationBwhzad HameedNo ratings yet
- MTPCL - WTP O&m ManualDocument62 pagesMTPCL - WTP O&m Manualm_ganesh1983100% (4)
- Tugas PPM Deny Saputro Arifin 113170039Document9 pagesTugas PPM Deny Saputro Arifin 113170039Vira IrnandaNo ratings yet
- Food Fish Processing NotesDocument14 pagesFood Fish Processing NotesRoselyn MyerNo ratings yet
- 10 Main Personal Protective EquipmentDocument7 pages10 Main Personal Protective EquipmentDaniel CastilloNo ratings yet
- For The Determination of Precious Metals in Autocatalyst SamplesDocument6 pagesFor The Determination of Precious Metals in Autocatalyst SamplesScumpika ElenaNo ratings yet
- Infrared Optical Materials and Their Antireflection CoatingsDocument5 pagesInfrared Optical Materials and Their Antireflection CoatingsnguyenthanhhopNo ratings yet
- Kuala Lumpur Kepong Berhad - WikipediaDocument17 pagesKuala Lumpur Kepong Berhad - Wikipedianoel.manroeNo ratings yet
- Vocabular PDFDocument5 pagesVocabular PDFAndra Ch123No ratings yet
- PNS 113 Rebars PDFDocument12 pagesPNS 113 Rebars PDFKenneth PenianoNo ratings yet
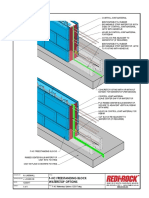
- F-HC Waterstop Options 122017Document1 pageF-HC Waterstop Options 122017ED WARMONDNo ratings yet
- Pozzolith 80 PDFDocument2 pagesPozzolith 80 PDFDoby YuniardiNo ratings yet
- Mixing A Balanced Nutrient SolutionDocument16 pagesMixing A Balanced Nutrient SolutionRómulo Del ValleNo ratings yet
- Biodegradable Polymers For Sustainable Packaging Applications - A ReviewDocument12 pagesBiodegradable Polymers For Sustainable Packaging Applications - A ReviewAngelito AraxielNo ratings yet
- Talaat A.Kader: Country ManagerDocument6 pagesTalaat A.Kader: Country ManagermohammedNo ratings yet
- AOAC Official Method - 962 - 16 - Sulfurous Acid (Total) in Food - Modifie...Document2 pagesAOAC Official Method - 962 - 16 - Sulfurous Acid (Total) in Food - Modifie...mustafa kaya100% (1)
- ادوية التخدير 2Document2 pagesادوية التخدير 2b2ddfnvfp6No ratings yet
- ACG Associated Capsules PVT LTD: A Member of ACG WorldwideDocument4 pagesACG Associated Capsules PVT LTD: A Member of ACG Worldwidepeter mackey mamani mamanchura100% (1)
- Project On Powder Dispensing System of Sand 3d PrintingDocument101 pagesProject On Powder Dispensing System of Sand 3d PrintingSameer MandaogadeNo ratings yet
- Preparation and Evaluation of Controlled Release Tablets Containing Mefenamic Acid 2161 1459.1000107Document3 pagesPreparation and Evaluation of Controlled Release Tablets Containing Mefenamic Acid 2161 1459.1000107Rike YulianingtyasNo ratings yet
- Pharmacology AlgesiologyDocument4 pagesPharmacology AlgesiologyCpopNo ratings yet
- Kinetics of The Selective Hydrogenation of Phenol To Cyclohexanone Over A Pd-Alumina CatalystDocument8 pagesKinetics of The Selective Hydrogenation of Phenol To Cyclohexanone Over A Pd-Alumina CatalystTaylor PennaNo ratings yet
- Class 12 Chemistry Biomolecules PyqDocument11 pagesClass 12 Chemistry Biomolecules PyqRakesh AgarwalNo ratings yet
- C898C898M 09.pdf (EngPedia - Ir)Document14 pagesC898C898M 09.pdf (EngPedia - Ir)Hossein DoudiNo ratings yet
- Astm A479Document7 pagesAstm A479Martin RomeroNo ratings yet
- Effects of Fly Ash and Silica Fume On The Resistance of Mortar To Sulfuric Acid and Sulfate AttackDocument10 pagesEffects of Fly Ash and Silica Fume On The Resistance of Mortar To Sulfuric Acid and Sulfate AttackMaziar Mehravar100% (1)
- Retrofitting of BuildingDocument5 pagesRetrofitting of BuildingEmily UyNo ratings yet