0% found this document useful (0 votes)
55 views7 pagesReviewer
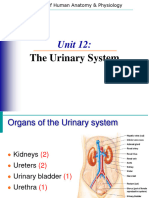
The urinary system is responsible for removing metabolic wastes, maintaining homeostasis, and regulating fluid balance in the body. Key organs include the kidneys, ureters, urinary bladder, and urethra, with nephrons serving as the functional units for urine formation through filtration, reabsorption, and secretion processes. The system also plays a crucial role in regulating water, electrolyte balance, and blood pH through hormonal control.
Uploaded by
aguilard953Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
55 views7 pagesReviewer
The urinary system is responsible for removing metabolic wastes, maintaining homeostasis, and regulating fluid balance in the body. Key organs include the kidneys, ureters, urinary bladder, and urethra, with nephrons serving as the functional units for urine formation through filtration, reabsorption, and secretion processes. The system also plays a crucial role in regulating water, electrolyte balance, and blood pH through hormonal control.
Uploaded by
aguilard953Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd