0% found this document useful (0 votes)
70 views5 pagesMedical Exam Forms
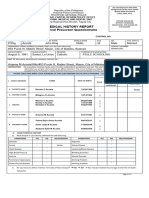
The document outlines the compulsory medical history and physical examination requirements for students enrolling at the University of the Philippines Mindanao. It includes sections for personal data, family history, vaccination status, and various health-related questions that must be completed and submitted as part of the enrollment process. Additionally, it provides a physical examination form to be filled out by a university physician, detailing the student's health status and any medical advice or prescriptions.
Uploaded by
Pia Noelle VelascoCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
70 views5 pagesMedical Exam Forms
The document outlines the compulsory medical history and physical examination requirements for students enrolling at the University of the Philippines Mindanao. It includes sections for personal data, family history, vaccination status, and various health-related questions that must be completed and submitted as part of the enrollment process. Additionally, it provides a physical examination form to be filled out by a university physician, detailing the student's health status and any medical advice or prescriptions.
Uploaded by
Pia Noelle VelascoCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd