Professional Documents
Culture Documents
PSORIASIS
PSORIASIS
Uploaded by
Aditya Yoga WidyaswaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PSORIASIS
PSORIASIS
Uploaded by
Aditya Yoga WidyaswaraCopyright:
Available Formats
PSORIASIS
Psoriasis is a disease which
affects the skin and joints .
It commonly causes red
scaly patches to appear on
the skin.
The scaly patches caused by
psoriasis, called psoriatic
plaques, are areas of
inflammation and excessive
skin production.
Skin rapidly accumulates at
these sites and takes a
silvery-white appearance.
Plaques frequently occur on
the skin of the elbows and
knees, but can affect any
area including the scalp and
genitals.
Psoriasis is an inflammatory skin disease in which skin cells
replicate at an extremely rapid rate. New skin cells are
produced about eight times faster than normal--over several
days instead of a month--but the rate at which old cells slough
off is unchanged. This causes cells to build up on the skin's
surface, forming thick patches, or plaques, of red sores (lesions)
covered with flaky, silvery-white dead skin cells (scales).
The disorder is a chronic recurring
condition
which varies in severity from minor
localised patches to complete body
coverage.
Fingernails and toenails are frequently
affected (psoriatic nail dystrophy) - and
can be seen as an isolated finding.
Psoriasis can also cause inflammation
of the joints, which is known as
psoriatic arthritis .
The cause of psoriasis is not known, but it is
believed to have a genetic component.
Several factors are thought to aggravate
psoriasis. These include stress,
excessive alcohol consumption , and smoking.
Individuals with psoriasis may suffer from
depression and loss of self-esteem.
As such, quality of life is an important factor
in evaluating the severity of the disease.
Certain medicines, including lithium salt and
beta blockers, have been reported to trigger
or aggravate the disease.
There are two main hypotheses about the process that
occurs in the development of the disease.
The first considers psoriasis as primarily a disorder of
excessive growth and reproduction of skin cells. The
problem is simply seen as a fault of the epidermis and its
keratinocytes .
The second hypothesis sees the disease as being an
immune-mediated disorder in which the excessive
reproduction of skin cells is secondary to factors
produced by the immune system. T cells (which normally
help protect the body against infection) become active,
migrate to the dermis and trigger the release of
cytokines (tumor necrosis factor-alpha TNF, in
particular) which cause inflammation and the rapid
production of skin cells. It is not known what initiates
the activation of the T cells.
The immune-mediated model of psoriasis has been
supported by the observation that immunosuppressant
medications can clear psoriasis plaques.
Types of Psoriasis
Plaque psoriasis (psoriasis
vulgaris) is the most common form
of psoriasis. It affects 80 to 90% of
people with psoriasis. Plaque
psoriasis typically appears as raised
areas of inflamed skin covered with
silvery white scaly skin. These areas
are called plaques.
Flexural psoriasis (inverse
psoriasis) appears as smooth
inflamed patches of skin. It
occurs in skin folds,
particularly around the genitals
(between the thigh and groin),
the armpits, under an
overweight stomach (pannus),
and under the breasts
(inframammary fold). It is
aggravated by friction and
sweat, and is vulnerable to
fungal infections.
Guttate psoriasis is
characterized by numerous
small oval (teardrop-shaped)
spots. These numerous spots of
psoriasis appear over large
areas of the body, such as the
trunk, limbs, and scalp. Guttate
psoriasis is associated with
streptococcal throat infection
Pustular psoriasis appears as
raised bumps that are filled with
non-infectious pus (pustules). The
skin under and surrounding pustules
is red and tender. Pustular psoriasis
can be localised, commonly to the
hands and feet , or generalised with
widespread patches occurring
randomly on any part of the body.
Nail psoriasis produces a variety of
changes in the appearance of finger
and toe nails. These changes include
discolouring under the nail plate,
pitting of the nails, lines going
across the nails, thickening of the
skin under the nail, and the
loosening (onycholysis) and
crumbling of the nail.
Psoriatic arthritis
involves joint and
connective tissue
inflammation.
Psoriatic arthritis can
affect any joint but is
most common in the
joints of the fingers and
toes. This can result in a
sausage-shaped swelling
of the fingers and toes
known as dactylitis.
Psoriatic arthritis can
also affect the hips, knees
and spine (spondylitis).
About 10-15% of people
who have psoriasis also
have psoriatic arthritis.
Erythrodermic
psoriasis involves the
widespread inflammation
and exfoliation of the skin
over most of the body
surface. It may be
accompanied by severe
itching, swelling and pain.
It is often the result of an
exacerbation of unstable
plaque psoriasis,
particularly following the
abrupt withdrawal of
systemic treatment. This
form of psoriasis can be
fatal, as the extreme
inflammation and
exfoliation disrupt the
body's ability to regulate
temperature and for the
skin to perform barrier
functions.
A diagnosis of psoriasis is usually based
on the appearance of the skin. There are
no special blood tests or diagnostic
procedures for psoriasis. Sometimes a
skin biopsy, or scraping, may be needed
to rule out other disorders and to confirm
the diagnosis. Skin from a biopsy will
show clubbed pegs if positive for
psoriasis.
Another sign of psoriasis is that when the
plaques are scraped, one can see pinpoint
bleeding from the skin below (Auspitz's
sign).
Treatment options
There can be substantial variation between
individuals in the effectiveness of specific
psoriasis treatments. Because of this,
dermatologists often use a trial-and-error
approach to finding the most appropriate
treatment for their patient.
The decision to employ a particular treatment is
based on the type of psoriasis, its location, extent
and severity. The patients age, gender, quality of
life, comorbidities, and attitude toward risks
associated with the treatment are also taken into
consideration.
Medications with the least potential for adverse
reactions are preferentially employed.
As a first step, medicated ointments or creams
are applied to the skin. If topical treatment fails
to achieve the desired goal then the next step
would be to expose the skin to ultraviolet (UV)
radiation. This type of treatment is called
phototherapy.
The third step involves the use of medications
which are taken internally by pill or injection :
systemic treatment.
Over time, psoriasis can become resistant to a
specific therapy. Treatments may be
periodically changed to prevent resistance
developing (tachyphylaxis) and to reduce the
chance of adverse reactions occurring:
treatment rotation.
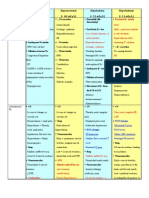
Topical treatment
Salicylic acid
Keratolytic agents, weak antifungals,
antibacterial agents
Remove accumulated scale, allow
topical agents to pass through
AE: irritation, salicylism (N&V,
tinnitus)
Coal Tar
Prefered for limited or scalp psoriasis
Can be effective in widespread
psoriasis
Antimitotic, anti-pruritic
No quick onset but longer remission
Often combined with SA, UV light
therapy
2 types: Crude coal tar and Liquor
picis carbonis
Dithranol
May restore normal epidermal
proliferation and keratinization
Useful in thick plaque psoriasis
Commonly used with SA
2 treatment approach: long contact
and short contact
Stains clothes, irritating to normal
skin
Topical CS
Anti-inflammatory, immunosuppressive
Quick onset than coal tar and dithranol
Tachyphylaxis can occur
High potent agents used in severe
cases, thick plaques
AE local and systemic
Should not be stopped abruptly
rebound psoriasis
Phototherapy
UVA, UVB, PUVA
UVB prefered
Administered by lamp, sunlight
exposure alone or in combo with
another topical agent
PUVA (methoxsalen) given PO 2 hours
before UVA or lotion applied 30mins
before exposure
AE: itch, edema
Systemic Therapy
Immunomodulators
Cyclosporin, methotrexate
commonly used
Antibiotics in case of secondary
bacterial infections
Systemic agents are generally
recommended for patients with
moderate-to-severe disease.
Moderate disease is defined as
greater than 5% body-surface area
involvement; severe disease is
defined by greater than 10%
Summary
Psoriasis is a lifelong condition.
There is currently no cure but various
treatments can help to control the symptoms.
Many of the most effective agents used to treat
severe psoriasis carry an increased risk of
significant morbidity including skin cancers,
lymphoma and liver disease.
Psoriasis does get worse over time but it is not
possible to predict who will go on to develop
extensive psoriasis or those in whom the
disease may appear to vanish.
Individuals will often experience flares and
remissions throughout their lives. Controlling
the signs and symptoms typically requires
lifelong therapy.
You might also like
- Wound Dressing Guide PDFDocument2 pagesWound Dressing Guide PDFrufftuffcookieNo ratings yet
- Teaching Plan For Patient With CopdDocument2 pagesTeaching Plan For Patient With Copdapi-3530442990% (1)
- NandaDocument28 pagesNandaAmit MartinNo ratings yet
- Gout Diet Patient HandoutDocument3 pagesGout Diet Patient HandoutJenniferNo ratings yet
- Guideline, Management of HypoglycemiaDocument5 pagesGuideline, Management of HypoglycemianellieauthorNo ratings yet
- Lecture #7, Points On The Continuum - Ambulatory Care, Home Care, Hospice and Palliative CareDocument17 pagesLecture #7, Points On The Continuum - Ambulatory Care, Home Care, Hospice and Palliative CareKathleen LaNo ratings yet
- Homeostasis Temperature RegulationDocument22 pagesHomeostasis Temperature RegulationChris AllamNo ratings yet
- Burns 2Document34 pagesBurns 2Vaibhavi JainNo ratings yet
- Diabetic KetoacidosisDocument10 pagesDiabetic KetoacidosisdhanasundariNo ratings yet
- Graves DseDocument5 pagesGraves DseHester Marie SimpiaNo ratings yet
- Documentation System Focus ChartingDocument26 pagesDocumentation System Focus ChartingneehoshiNo ratings yet
- Monkeypox FAQDocument2 pagesMonkeypox FAQMaritza NunezNo ratings yet
- Constipation: Stools ExplainedDocument4 pagesConstipation: Stools ExplainedArun MuralidharanNo ratings yet
- Acute and Chronic DM ComplicationsDocument29 pagesAcute and Chronic DM ComplicationsJennicaNo ratings yet
- HHNK and DkaDocument4 pagesHHNK and Dkagoya100% (1)
- Acute Complications of Diabetes MellitusDocument13 pagesAcute Complications of Diabetes MellitusMark Christian M. GonzagaNo ratings yet
- Diabetes MellitusDocument9 pagesDiabetes MellitusBrylle CapiliNo ratings yet
- What Is Pressure Ulcer?: Signs and SymptomsDocument6 pagesWhat Is Pressure Ulcer?: Signs and Symptomsshenecajean carajayNo ratings yet
- Nursing Care Plan For ElderlyDocument4 pagesNursing Care Plan For ElderlyTony Chandra Bastian100% (1)
- Management of Bed SoreDocument19 pagesManagement of Bed Soreugandanursingschool bwindi100% (1)
- Treatment of Diabetes MellitusDocument31 pagesTreatment of Diabetes MellitusIrfan IdealistNo ratings yet
- Antidotes in Opioid Toxicity and Substance Dependence: MIMS Summary TableDocument1 pageAntidotes in Opioid Toxicity and Substance Dependence: MIMS Summary TableJake CaballoNo ratings yet
- Diabetes: Causes, Symptoms and TreatmentsDocument4 pagesDiabetes: Causes, Symptoms and TreatmentsAbdullah BazryNo ratings yet
- Presentation SWINE FLUDocument40 pagesPresentation SWINE FLUdr_hammadNo ratings yet
- Medication ErrorsDocument11 pagesMedication ErrorsJayson V Caranto RN100% (1)
- Emergency Management of Patients With Drug OverdoseDocument6 pagesEmergency Management of Patients With Drug Overdosetheglobalnursing0% (1)
- Delirium: Acute Confusion in The Elderly: Donald R. Noll DO FACOIDocument53 pagesDelirium: Acute Confusion in The Elderly: Donald R. Noll DO FACOIHema Laughsalot100% (2)
- Epidural Hematoma: A Slip and Fall Is All It Takes To Puncture An Artery and Cause An..Document19 pagesEpidural Hematoma: A Slip and Fall Is All It Takes To Puncture An Artery and Cause An..koringring100% (1)
- HemiplegiaDocument17 pagesHemiplegiaStefany CelineNo ratings yet
- 11 Diabetic FootDocument37 pages11 Diabetic Footkim suhoNo ratings yet
- Fall in ElderlyDocument39 pagesFall in ElderlyKHAIRUL NADIAHNo ratings yet
- Transferring People Safely - WebDocument36 pagesTransferring People Safely - Webkimbakicks100% (1)
- HEENT Focused Exam Soap NoteDocument5 pagesHEENT Focused Exam Soap Noteariel sparkmanNo ratings yet
- Pathophysiology DKADocument2 pagesPathophysiology DKALovely CacapitNo ratings yet
- Flip Chart: Integrated Management of Childhood IllnessDocument24 pagesFlip Chart: Integrated Management of Childhood IllnessCAREZAMBIANo ratings yet
- CardiovascularDocument34 pagesCardiovascularRianna LarezaNo ratings yet
- Disseminated Intravascular CoagulationDocument19 pagesDisseminated Intravascular CoagulationAnna MilliziaNo ratings yet
- Identification and Diagnosis: Compulsive Alcoholic BeveragesDocument3 pagesIdentification and Diagnosis: Compulsive Alcoholic BeveragesKaren JulaoNo ratings yet
- Common Skin DisordersDocument10 pagesCommon Skin DisordersPaul Vincent Alfonso100% (1)
- Type 2 Diabetes Mellitus - A Review of Current TrendsDocument5 pagesType 2 Diabetes Mellitus - A Review of Current TrendsRevivo RindaNo ratings yet
- HypertensionDocument12 pagesHypertensionDr. PARMINDER NAINNo ratings yet
- Ambulatory Care NursingDocument5 pagesAmbulatory Care NursingKim TanNo ratings yet
- PancreatitisDocument28 pagesPancreatitisFrench Pastolero-ManaloNo ratings yet
- UrinalysisDocument9 pagesUrinalysisyuppierajNo ratings yet
- Nursing Care in AIDSDocument18 pagesNursing Care in AIDSInsaniNo ratings yet
- Electrolyte ImbalancesDocument4 pagesElectrolyte Imbalancessccctutor100% (2)
- HNN215 Drug DiaryDocument10 pagesHNN215 Drug DiaryMaddison MitchellNo ratings yet
- Intra - Abdominal HypertensionDocument40 pagesIntra - Abdominal HypertensionBayu Surya Dana100% (1)
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Nurse Practitioner Wound Management Clinical ProtocolsDocument29 pagesNurse Practitioner Wound Management Clinical ProtocolsBrian HarrisNo ratings yet
- The Dangers of SmokingDocument2 pagesThe Dangers of SmokingEvi Febri RahmawatiNo ratings yet
- Writing Learning Objectives Nursing - Oct 2017Document3 pagesWriting Learning Objectives Nursing - Oct 2017Rawan RonaNo ratings yet
- Case Presentation Guideline All MedicalDocument1 pageCase Presentation Guideline All MedicalAnonymous 0WHX7nNo ratings yet
- Congenital Heart DefectsDocument20 pagesCongenital Heart DefectsJanina Loren NeyraNo ratings yet
- Types of Insulin For Diabetes TreatmentDocument8 pagesTypes of Insulin For Diabetes TreatmentChander KantaNo ratings yet
- Wound AssessmentDocument19 pagesWound Assessmentdrsonuchawla100% (1)
- Sexually Transmitted InfectionsDocument34 pagesSexually Transmitted InfectionsMariana Creciun100% (1)