Professional Documents
Culture Documents
017 Burns
Uploaded by
api-2366499880 ratings0% found this document useful (0 votes)
574 views12 pagesOriginal Title
017 burns
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
574 views12 pages017 Burns
Uploaded by
api-236649988Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 12
BURNS
Incidence and Causes
8,000-10,00 burns per year in the U.S.A.
75-80% occur in homes
Major causes: flames, scalds, heat, chemicals and electricity
Under age 6, major cause is scalding
75% of burns could be avoided
Body surface affected (BSA)
The Rule of Nines
Entire head = 9%
Each arm = 9% (18%)
Chest = 9%
Abdomen = 9%
Upper back = 9%
Lower back = 9%
Front of each leg = 9% (18%)
Back of each leg = 9% (18%)
Groin = 1%
Total 100%
This along with the cause of
the burn helps determine the
severity of the burn
Lund-Browder
Accurate assessment of TBSA
Complications of Major Burns
Pulmonary injury; Stridor (whistling) with breathing
Hypovolaemia; loss of plasma and decreased BP
Hypothermia; with skin gone there is no thermoregulation
Cardiac Arrhythmia; irregular heart beat.
Kidney Failure
Death
When burns are critical
Any burn greater than 25% BSA
Full or deep-partial-thickness burns greater than 10% BSA
Burns complicated by a respiratory or airway injury
Most burns involving the face, hands, feet or genitals
Burns complicated by a fracture or major soft-tissue injury
Electrical or deep-chemical burns
Burns occurring in patients with serious pre-existing medical conditions
Classification of Burns
First degree or superficial burns
involve only the epidermis;
burned area is red; no blisters.
Second degree or partial thickness burns
involve all of epidermis & varying depths of the dermis.
Appearance -blisters, pink, moist, Extremely painful.
Third degree or full thickness burns
involve epidermis & entire dermis, possible deeper tissue such
as muscle and bone.
Appearance- white and dry. May be free of pain. Requires
skin grafting.
Burn types
Thermal - most common (Other than sunburn)
direct flame, scalds and direct contact.
Chemical - contact strong acids or alkalis.
burning process continues as long as the chemical, or agent, is on the body.
need to know the specific chemical because the treatment must be specific
Electrical - type I, II and III.
Type I - contact burn - most common - true electricity injury. burn is most severe at the
entry and exit points.
Type II - flash burn - victim becomes part of an electrical arc.
Type III - flame burn - electricity ignites the victim's clothing.
Sunburn. Radiation burns are by far the most common burns because of being exposed to
an enormous nuclear reactor, the sun.
sunburns are almost always superficial.
Don't underestimate the potential severity of sunburn. Using the Rule of Nines, it is not
uncommon for sunburn to reach the critical stage (burns greater than 25 percent BSA),
Some patients require skin grafting after prolonged sun exposure.
Burn treatment
1.stop the burning
2. evaluate the injury
3. relieve pain
4. prevent shock
5. infection.
Even though the fire is out, the burning can continue.
Remove all burned clothing
flush the skin with cool water.
Flushing is crucial to a chemical burn, particularly alkalis which must be flushed for 1 to 2 hours
Burned skin loses heat more rapidly than intact skin and cool water can cause hypothermia if a
large BSA has been burned.
Pay particular attention to the airway. An airway problem may not be immediately apparent.
If the patient has airway involvement or any respiratory difficulty, advanced rapid treatment is
required.
Superficial burns are easily managed with cool compresses and acetaminophen for the pain.
An extensive superficial burn will demand a slightly stronger analgesic and should be accompanied by an
increase in fluid intake by the patient.
basic systemic pain control along with fluid intake is the best approach.
treatment of partial-thickness burns follows the same approach of cooling the area and covering the burn
with a sterile dressing.
Do not break the blisters; they are actually the best burn dressing available. If the blisters rupture later,
apply Silvadene as an antibiotic ointment and cover with dry, sterile dressing.
Fluid loss can be an early complication and is most common with partial-thickness and deeper burns.
Depending on the extent of BSA involved, a fluid loss can rapidly lead to shock.
If the BSA is greater than 15 percent, fluid replacement is required. This is best managed with I-V fluids
Emergent Care
Burning process stopped with removal of clothing,
jewellery and covering affected area with cool
water
Increase blood volume with IV inserted in intact
skin area
Urinary catheter to monitor fluid output, indicates
dehydration
Intubation to secure an airway
Vitals; BP, HR, BPM, Temp
Determining extent of damage; Rule of Nines or
Lund -Browder
1 week after
3 weeks later
16 weeks later
You might also like
- Burns: ABC of Wound HealingDocument4 pagesBurns: ABC of Wound HealingRicardoGamalielNo ratings yet
- Burns Practice TeachingDocument58 pagesBurns Practice TeachingSakthi Devi100% (1)
- Burn Victims Care Manual 4 FirefightersDocument11 pagesBurn Victims Care Manual 4 Firefightershttps://scribd.vpdfs.com/No ratings yet
- Patel - Physiotherapy in BurnsDocument96 pagesPatel - Physiotherapy in BurnsFaridah saidNo ratings yet
- Burn Classification & Management Algorithm"TITLE"Airway, Breathing, Circulation Approach to Severe BurnsDocument3 pagesBurn Classification & Management Algorithm"TITLE"Airway, Breathing, Circulation Approach to Severe BurnsEl LenNo ratings yet
- Primary Care of BurnsDocument20 pagesPrimary Care of BurnsNatalie AlcântaraNo ratings yet
- Approach To Patient With Burn (S) : No Blisters Swollen and Blistered Whitish or Charred (Black)Document6 pagesApproach To Patient With Burn (S) : No Blisters Swollen and Blistered Whitish or Charred (Black)Suthar Keval CNo ratings yet
- Pamantasan NG Lungsod NG Maynila: (University of The City of Manila)Document23 pagesPamantasan NG Lungsod NG Maynila: (University of The City of Manila)Em Hernandez AranaNo ratings yet
- BurnsDocument58 pagesBurnsMarie MayNo ratings yet
- BurnsDocument37 pagesBurnskint100% (2)
- Burns & Burn Management, Asphyxiation, and Head InjuriesDocument77 pagesBurns & Burn Management, Asphyxiation, and Head InjuriesGabz GabbyNo ratings yet
- Introduction To Burns: Bacteria VirusesDocument6 pagesIntroduction To Burns: Bacteria Virusesanon-50728No ratings yet
- Acute Burn ManagementDocument23 pagesAcute Burn ManagementUsman AR VainceNo ratings yet
- First Aid for Burns GuideDocument21 pagesFirst Aid for Burns Guidegashbin MahdyNo ratings yet
- Basic First Aid - ToPIC 4 (Burns)Document33 pagesBasic First Aid - ToPIC 4 (Burns)Karl James RetaNo ratings yet
- Burns InjuriesDocument24 pagesBurns InjuriesRama SultanNo ratings yet
- Burns Assessment - TeachMeSurgeryDocument5 pagesBurns Assessment - TeachMeSurgeryLaroui HoNo ratings yet
- Interventions For ClientsDocument68 pagesInterventions For ClientsRinkish DalliahNo ratings yet
- Burn ManagementDocument7 pagesBurn ManagementnrhmhealthNo ratings yet
- BurnsDocument13 pagesBurnsmsah820No ratings yet
- Classification: by DepthDocument7 pagesClassification: by Depthstephanie_neri_2No ratings yet
- Trauma and Emergecny Nursing: Course TittleDocument64 pagesTrauma and Emergecny Nursing: Course TittleAbdisamed AllaaleNo ratings yet
- Care of The Burn Patient JafDocument99 pagesCare of The Burn Patient JafPaige Fox100% (1)
- Pediatric BurnsDocument9 pagesPediatric BurnsManoj KumarNo ratings yet
- Burns An Introduction To Burns and Basic Wound - 2023 - Physician Assistant CliDocument11 pagesBurns An Introduction To Burns and Basic Wound - 2023 - Physician Assistant CliJose AnaconaNo ratings yet
- BurnDocument7 pagesBurnpatlekhilesh8No ratings yet
- Management of Burns: CPT Allen Proulx, MPAS, PA-CDocument68 pagesManagement of Burns: CPT Allen Proulx, MPAS, PA-Cjimy006No ratings yet
- Initial Care of BurnsDocument53 pagesInitial Care of BurnsFrancr ToledanoNo ratings yet
- Burn in PediatricDocument5 pagesBurn in PediatricAbdulkadir HasanNo ratings yet
- Burns and ScaldsDocument14 pagesBurns and ScaldsMuhamad IqbalNo ratings yet
- PPP-BURNS 118slDocument30 pagesPPP-BURNS 118slCath BrilNo ratings yet
- Burns: What Are The Categories of Burns?Document8 pagesBurns: What Are The Categories of Burns?Marco1998No ratings yet
- Burns: Hadi Munib Oral and Maxillofacial SurgeryDocument79 pagesBurns: Hadi Munib Oral and Maxillofacial SurgeryAli ahmedNo ratings yet
- Management of Burn PDFDocument5 pagesManagement of Burn PDFaditiNo ratings yet
- Burns 2Document4 pagesBurns 2Charmae NaveaNo ratings yet
- BurnsDocument14 pagesBurnsKyla Baldonado BrunoNo ratings yet
- Plastic Surgery SummaryDocument30 pagesPlastic Surgery SummaryLailaAliNo ratings yet
- Acute Management of Burns in ChildrenDocument52 pagesAcute Management of Burns in ChildrenJonie Vince SañosaNo ratings yet
- Burn Treatment and Recovery GuideDocument5 pagesBurn Treatment and Recovery GuideMarcel Quario OrinaNo ratings yet
- Burns: BY Idris Abdulrashid, Department of Nursing Sciences Bayero University KanoDocument44 pagesBurns: BY Idris Abdulrashid, Department of Nursing Sciences Bayero University KanoNaija Nurses TV100% (3)
- Nursing Care of The Client With Burn Injury: BurnsDocument40 pagesNursing Care of The Client With Burn Injury: BurnsAhmad Rayan100% (2)
- Thermal BurnsDocument50 pagesThermal BurnsPooya WindyNo ratings yet
- Burns & PoisoningDocument19 pagesBurns & PoisoningFrancis Caster MatutesNo ratings yet
- King Saud University College of NursingDocument49 pagesKing Saud University College of Nursinghatem alsrour100% (2)
- BurnsDocument9 pagesBurnsVincentus BinNo ratings yet
- 8 - Reconsructive Surgery Pt&Ot 2023-2024Document41 pages8 - Reconsructive Surgery Pt&Ot 2023-2024MUGISHA GratienNo ratings yet
- Paediatric Burns FinalizedDocument28 pagesPaediatric Burns FinalizedKarthick UnleashNo ratings yet
- Thermal Injury: By: Supriadi, BSN, Mhs (Acute and Chronic Wound Specialist)Document34 pagesThermal Injury: By: Supriadi, BSN, Mhs (Acute and Chronic Wound Specialist)ari andiNo ratings yet
- Burns Assessment and ManagementDocument33 pagesBurns Assessment and ManagementErina Erichan Oto100% (1)
- Nursing Care of Children With BurnsDocument52 pagesNursing Care of Children With Burnskarpagamanbu100% (5)
- What Is A Burn?: Injury Pada Kulit Caused by Heat, Electricity, Chemicals, Friction, or RadiationDocument42 pagesWhat Is A Burn?: Injury Pada Kulit Caused by Heat, Electricity, Chemicals, Friction, or RadiationFirdaus Martha FriansahNo ratings yet
- Print ERDocument3 pagesPrint ERBJ DUQUESANo ratings yet
- Burns DebridementDocument27 pagesBurns DebridementNisha FatmaNo ratings yet
- Burn PPT VCMC 1Document70 pagesBurn PPT VCMC 1feva55100% (2)
- Sign up to receive weekly burns emailDocument9 pagesSign up to receive weekly burns emailParvathy R NairNo ratings yet
- BURNSDocument16 pagesBURNSRegina KadenyiNo ratings yet
- Introduction To BurnsDocument47 pagesIntroduction To BurnsanushavergheseNo ratings yet
- Managing Burns SafelyDocument30 pagesManaging Burns SafelyMamata BeheraNo ratings yet
- 017 Muscle PhysiologyDocument62 pages017 Muscle Physiologyapi-23664998867% (3)
- Ms Reviewsummary 327-331Document5 pagesMs Reviewsummary 327-331api-236649988No ratings yet
- Ms Performance 320-323Document5 pagesMs Performance 320-323api-236649988No ratings yet
- 017 Review Ms ChaptmartinDocument13 pages017 Review Ms Chaptmartinapi-236649988No ratings yet
- Ms Cardiac and Smooth 325-327Document5 pagesMs Cardiac and Smooth 325-327api-236649988No ratings yet
- Heart Review Question1Document6 pagesHeart Review Question1api-236649988No ratings yet
- 017 7 Heart Attack Coronary Artery Disease CadDocument7 pages017 7 Heart Attack Coronary Artery Disease Cadapi-236649988No ratings yet
- 708-715 CardiodynamicsDocument8 pages708-715 Cardiodynamicsapi-236649988No ratings yet
- Ms Contraction 300-307Document8 pagesMs Contraction 300-307api-236649988No ratings yet
- 017 3 Conduction EkgDocument18 pages017 3 Conduction Ekgapi-236649988No ratings yet
- 697 702conductionDocument6 pages697 702conductionapi-236649988No ratings yet
- Chapter Review HeartDocument5 pagesChapter Review Heartapi-236649988No ratings yet
- 017 Nails 017Document7 pages017 Nails 017api-236649988No ratings yet
- 017 6 Hearrt ConditionsDocument11 pages017 6 Hearrt Conditionsapi-236649988No ratings yet
- 017 4 Heart SoundsDocument8 pages017 4 Heart Soundsapi-236649988No ratings yet
- 017 2 Coronary ArteriesDocument12 pages017 2 Coronary Arteriesapi-236649988No ratings yet
- 017 5 Blood PressureDocument5 pages017 5 Blood Pressureapi-236649988No ratings yet
- Skin ColorDocument16 pagesSkin Colorapi-236649988No ratings yet
- 017 Infections and Allergies SkinDocument14 pages017 Infections and Allergies Skinapi-236649988No ratings yet
- Martin 017 HeartDocument58 pagesMartin 017 Heartapi-236649988No ratings yet
- 017 1 Intro Heart AnatDocument33 pages017 1 Intro Heart Anatapi-236649988No ratings yet
- 017 Skin Intro FNDocument8 pages017 Skin Intro FNapi-236649988No ratings yet
- Hair 017Document9 pagesHair 017api-236649988No ratings yet
- Dermis HypodermisDocument9 pagesDermis Hypodermisapi-236649988No ratings yet
- Integumentary System DisordersDocument15 pagesIntegumentary System Disordersapi-236649988No ratings yet
- 017 Epidermis LayersDocument17 pages017 Epidermis Layersapi-236649988No ratings yet
- Glands 017Document11 pagesGlands 017api-236649988No ratings yet
- 3817 Respiratory PreworkDocument3 pages3817 Respiratory PreworkAhmad BustamiNo ratings yet
- NEW CBT 2021 Summary Q 1Document34 pagesNEW CBT 2021 Summary Q 1himali ranasingheNo ratings yet
- BED Formula PDFDocument15 pagesBED Formula PDFMichelle Mora MariñoNo ratings yet
- McGrath Video Laryngoscope Rev 0.1Document6 pagesMcGrath Video Laryngoscope Rev 0.1adevasenNo ratings yet
- Fillable Anesthesia SheetDocument2 pagesFillable Anesthesia Sheetetchemendyvet70790% (1)
- Clinical Pathway Neonatal PneumoniaDocument4 pagesClinical Pathway Neonatal PneumoniaSHAINA ALIH. JUMAANINo ratings yet
- 5.occlusal Risk Factors Associated With Temporomandibular Disorders in Young Adults With Normal OcclusionsDocument5 pages5.occlusal Risk Factors Associated With Temporomandibular Disorders in Young Adults With Normal Occlusionsthiên lữNo ratings yet
- Assessing Body TemperatureDocument6 pagesAssessing Body TemperatureemailNo ratings yet
- IPAC Checklist for Clinical Office PracticeDocument24 pagesIPAC Checklist for Clinical Office PracticeBABBY ZBOURGNo ratings yet
- A Clinicians Guide To Systemic Sex Therapy 2nd Edition Ebook PDFDocument57 pagesA Clinicians Guide To Systemic Sex Therapy 2nd Edition Ebook PDFpaul.marshall936100% (45)
- Formula and TablesDocument6 pagesFormula and TablesMaria RahimNo ratings yet
- Pflipsen Anaphylaxis Recognition and ManagementDocument10 pagesPflipsen Anaphylaxis Recognition and ManagementOlivia McCuskerNo ratings yet
- Loratadine Drug StudyDocument1 pageLoratadine Drug StudyShene Claire VigillaNo ratings yet
- DiabetesDocument170 pagesDiabetesKoRnflakesNo ratings yet
- 01 Drug File MHNDocument29 pages01 Drug File MHNamit85% (13)
- Screening TestDocument4 pagesScreening TestTed Martinez Desiderio Jr.No ratings yet
- Introduction to Public Health NursingDocument37 pagesIntroduction to Public Health NursingKailash NagarNo ratings yet
- The Heart, Part 1 - Under Pressure: Crash Course A&P # 25Document5 pagesThe Heart, Part 1 - Under Pressure: Crash Course A&P # 25Jordan TorresNo ratings yet
- Evaluating The Airway for Difficult Intubation (LEMON MethodDocument7 pagesEvaluating The Airway for Difficult Intubation (LEMON Methodtri-edge 8No ratings yet
- Stool Exam Guide - Key Tests, Colors, Consistencies in 40 CharactersDocument8 pagesStool Exam Guide - Key Tests, Colors, Consistencies in 40 CharactersLester John HilarioNo ratings yet
- Ultrasound Guided Nerve Block Part IDocument29 pagesUltrasound Guided Nerve Block Part ImartccNo ratings yet
- Jurnal Implementasi NCP Pada DMDocument5 pagesJurnal Implementasi NCP Pada DMwidhy okayantiNo ratings yet
- Antenatal CareDocument12 pagesAntenatal CarefiramnNo ratings yet
- Manual Removal of The Placenta After Vaginal DeliveryDocument5 pagesManual Removal of The Placenta After Vaginal DeliveryDara Mayang SariNo ratings yet
- About The Measure Domain MeasureDocument3 pagesAbout The Measure Domain MeasureMaríaA.SerranoNo ratings yet
- Acute Prescribing - Challenges and Solutions - Ajit KulkarniDocument51 pagesAcute Prescribing - Challenges and Solutions - Ajit KulkarniAgha QaimiNo ratings yet
- Anemia - AMBOSSDocument2 pagesAnemia - AMBOSStgayuNo ratings yet
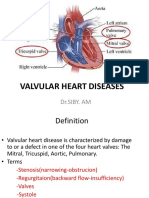
- VHD: Types, Causes, Symptoms & ManagementDocument42 pagesVHD: Types, Causes, Symptoms & ManagementareeparambilNo ratings yet
- Drinking Water and Losing WeightDocument3 pagesDrinking Water and Losing WeightMathana SuriaNo ratings yet
- 10.7 The Lymphatic System Extra NotesDocument5 pages10.7 The Lymphatic System Extra NotesVinieysha LoganathanNo ratings yet