Professional Documents
Culture Documents
Clinical Pharmacokinetics of Theophylline
Uploaded by
DelisaPutriChaniago0 ratings0% found this document useful (0 votes)
29 views33 pagesOriginal Title
kelompok 12.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
29 views33 pagesClinical Pharmacokinetics of Theophylline
Uploaded by
DelisaPutriChaniagoCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 33
Clinical Pharmacokinetics
THEOPHYLLIN
KELAS A/KELOMPOK 12
AYU ANDARINI (1511014017)
ARINI INTAN MUTIA (1511014018)
BEBA SHIAMI (1511014019)
MARHANI DWITHANIA (1511014020)
SITI SARI K. (1511014021)
INTRODUCTION
Theophyllin is a drug of the metylxanthin group used
for the asma treatment, chronic obstructive
pulmonary, and apnea premature. The primary key
of the disease is broncospasm. Theophyllin use has
different profiles for everyone, although some
people exhibit mixed disease with reversible airway
component. Theophyllin is now regarded as
adjunctive therapy, since asthmais also considered
an inflammatory disease that can be treat with
corticosteroid.
Baur, 2008 : 745
THEURAPETIC AND TOXIC
CONCENTRATION
• Treatment asthma : 10-20 µg/ml
• Premature apnea : 6-13 µg/ml
• Pulmonary disease : 5- 15 µg/ml ( suggest of
guideline)
upper end of the theurapetic range (>15 µg/ml) some
patient will experience the side effect (nausea,
vommiting, dyspepsia, insomnia, nervousness and
headache)
Concentration 20-30 µg/ml : tachiarrythmia
Concentration >40 µg/ml : ventricular arrythmias
(Baur, 2008 : 746)
PARAMETER CLINICAL MONITORING
• Measurment pulmonary function test
• Forced expiratory volume 1 second
• Peak- flow meter
• Spirometric test
• Clinical signs and symptoms ( dyspneas,
coughing,wheezing, impairmant in normal
activity)
(Baur, 2008 : 746- 747)
BASIC CLINICAL PHARMACOKINETIC
PARAMETERS
• Primarily eliminated by hepatic metabolism
(>90%)
• Hepatic metabolism is mainly via the CYP1A2
enzyme system with a smaller amount
metabolized by CYP3A and CYP2E1
• About 10% of a theophylline dose is recovered
in the urine as unchanged drug
(Bauer, 2008 : 748-749)
• There’s 3 different forms of theophylline
• Aminophylline is the ethylenediamine salt of
theophylline, and anhydrous aminophylline
contains about 85% theophylline while
aminophylline dihydrate contains about 80%
theophylline (oral and IV injection use)
• Oxtriphylline is the choline salt of theophylline
and contains about 65% theophylline (only
oral use)
(Bauer, 2008 : 749)
• The oral bioavailability of all three
theophylline-based drugs is very good and
generally equals 100%
• Theophylline plasma protein binding is only
40%
• Theophylline serum concentrations increase in
a patient more than expected after a dosage
increase for an unidentifiable reason (Non
Linear Pharmacokinetics)
(Bauer, 2008 : 749)
EFFECTS OF DISEASE STATES AND CONDITIONS ON
THEOPHYLLINE PHARMACOKINETICS AND DOSING
• Most disease states and conditions that
change theophylline pharmacokinetics and
dosage requirements alter clearance but
volume of distribution remains stable at ~0.5
L/kg
• Tobacco and marijuana smoke causes
induction of hepatic CYP1A2 which accelerates
the clearance of theophylline (people who
smoke these has t 1/2 is 5 hr)
(Bauer, 2008 : 749)
• Patients with liver cirrhosis or acute hepatitis have
reduced theophylline clearance which results in a
prolonged average theophylline half-life of 24 hours
(Bauer, 2008 : 750)
(Bauer, 2008 : 750)
(Bauer, 2008 : 751)
(Bauer, 2008 : 751)
• Heart failure causes reduced theophylline clearance because
of decreased hepatic blood flow secondary to compromised
cardiac output
• Venous stasis of blood within the liver may also contribute to
the decrease in theophylline clearance found in heart failure
patients
• Patients with mild heart failure (New York Heart Association
or NYHA Class I or II) have an average theophylline half-life
equal to 12 hours (range: 5–24 hours) while those with
moderate to severe heart failure (NYHA class III or IV) or cor
pulmonale have an average theophylline half-life of 24 hours
(5–50 hours)
(Bauer, 2008 : 752)
(Bauer, 2008 : 752)
• Premature neonates have average theophylline half-
lives equal to 30 hours 3–15 days after birth and 20
hours 25–57 days after birth
• Newborns have decreased theophylline clearance
• Children (1–9 y.o) have accelerated theophylline
clearance rates resulting in an average half-life of 3.5
hours (range: 1.5–5 hours)
• The breast milk to serum ratio for theophylline is 0.7
(Bauer, 2008 : 753)
DRUG INTERACTIONS
• Serious inhibition drug interactions are those that decrease theophylline Cl more
than 30%.
• Clinicians should consider an arbitrary decrease in theophylline dose of 30–50%
for patients receiving these agents until the actual degree of hepatic enzyme
inhibition can be assessed using theophylline serum concentration monitoring.
• Cimetidine given at higher doses (≥1000 mg/d) on a multiple daily dosage
schedule decreases theophylline Cl by 30–50%.
Other cimetidine doses (≤800 mg/d) given once or twice daily decrease
theophylline clearance by 20% or less.
• Ciprofloxacin and enoxacin, both quinolone antibiotics, and troleandomycin, a
macrolide antibiotic, also decrease theophylline Cl by 30–50%.
• Estrogen and estrogen-containing oral contraceptives, propranolol, metoprolol,
mexiletine, propafenone, pentoxifylline, ticlopidine, tacrine, thiabendazole,
disulfiram, nefazodone, interferon, zileuton, and fluvoxamine can also decrease
theophylline Cl by this extent.
(Bauer, 2008 : 753-754)
• many clinicians believe that a routine decrease in
theophylline dose is unnecessary for patients with Css
theophylline below 15 μg/mL, but should be considered
on a case-by-case basis for those with concentrations
above this level. Should a decrease be warranted in a
patient, theophylline doses can be cut by 20% to avoid
adverse effects.
• Patients should be actively monitored for the signs and
symptoms of theophylline toxicity.
• The CCB, verapamil, and diltiazem, have been reported to
cause decreases in theophylline Cl by 15–25%.
• Clarithromycin and erythromycin, both macrolide
antibiotics, and norfloxacin, a quinolone antibiotic, can
also decrease theophylline Cl by this magnitude. At doses
of 600 mg/d or above, allopurinol has been reported to
decrease theophylline clearance by 25%.
(Bauer, 2008 : 754)
INITIAL DOSAGE DETERMINATION
METHODS
• Pharmacokinetic Dosing Method
The goal of initial dosing of theophylline is to compute the best
dose possible for the patient given their set of disease states and
conditions that influence theophylline pharmacokinetics and the
pulmonary disorder being treated
• HALF-LIFE AND ELIMINATION RATE CONSTANT ESTIMATE
Theophylline is predominately metabolized by liver.
Unfortunately, there is no good way to estimate the elimination
characteristics of liver metabolized drugs using an endogenous marker of
liver function in the same manner that serum creatinine and estimated
creatinine clearance are used to estimate the elimination of agents that
are renally eliminated. Because of this, a patient is categorized according
to the disease states and conditions that are known to change
theophylline t1/2, and the t1/2 previously measured in these studies is
used as an estimate of the current patient’s t1/2
(Bauer, 2008 : 755)
• VOLUME OF DISTRIBUTION ESTIMATE
Theophylline Vd is relatively stable in patients regardless of the
disease states and conditions that are present. Vd is assumed to equal
0.5 L/kg for nonobese patients.
For obese patients (>30% above ideal body weight), ideal body weight
is used to compute theophylline volume of distribution
• SELECTION OF APPROPRIATE PHARMACOKINETIC MODEL AND
EQUATIONS
When given by continuous iv infusion or orally, theophylline
follows a onecompartment pharmacokinetic model (Figures 18-1, 18-3,
18-4). When oral therapy is required, most clinicians utilize a
sustained-release dosage form that has good bioavailability (F = 1),
supplies a continuous release of theophylline into the GI tract, and
provides a smooth theophylline serum concentration/time curve that
emulates an iv infusion after once or twice daily dosing.
Because of this, a very simple pharmcokinetic equation that
computes the average theophylline (Css in μg/mL = mg/L) is widely
used and allows maintenance dosage calculation:
Css = [F ⋅ S (D/τ)]/Cl or
D = (Css ⋅ Cl ⋅ τ)/(F ⋅ S),
(Bauer, 2008 : 755)
• (F = 1 for most oral theophylline sustained-release products),
• S is the fraction of the theophylline salt form that is active
theophylline (S = 1 for theophylline, S = 0.85 for anhydrous
aminophylline, S = 0.80 for aminophylline dihydrate, S = 0.65
for oxtriphylline),
• D is the dose of theophylline salt in milligrams, and τ is the
dosage interval in hours.
• Cl is theophylline Cl in L/h and is computed using estimates of
theophylline elimination rate constant (k) and Vd : Cl = k.Vd
(Bauer, 2008 : 755-756)
• When intravenous therapy is required, a similar pharmacokinetic
equation that computes the theophylline Css (Css in μg/mL =
mg/L) is widely used and allows dosage calculation for a
continuous infusion: Css = [S ⋅ k0]/Cl or k0 = (Css ⋅ Cl)/S,
• (S = 1 for theophylline, S = 0.85 for anhydrous aminophylline, S =
0.80 for aminophylline dihydrate) and k0 is the dose of
theophylline salt in mg
• Cl is theophylline Cl/h and is computed using estimates of
theophylline elimination rate constant (k) and Vd : Cl = kV.
(Bauer, 2008 : 756)
• STEADY-STATE CONCENTRATION SELECTION
• The generally accepted therapeutic ranges for theophylline are 10–
20 μg/mL for the treatment of asthma or chronic obstructive
pulmonary disease, or 6–13 μg/mL for the treatment of premature
apnea.
• Recent guidelines suggest that for initial treatment of pulmonary
disease, clinical response to theophylline concentrations between
5–15 μg/mL should be assessed before higher concentrations are
used.
• Many patients requiring chronic theophylline therapy will derive
sufficient bronchodilatory response with a low likelihood of adverse
effects at concentrations of 8–12 μg/mL.
• However, theophylline therapy must be individualized for each
patient in order to achieve optimal responses and minimal side
effects.
(Bauer, 2008 : 757)
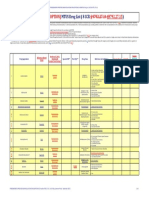
• Literature-Based Recommended Dosing
• Because of the large amount of variability in theophylline pharmacokinetics, In
general, the expected theophylline Css used to compute these doses was 10
μg/mL.
• For obese individuals (>30% over ideal body weight), ideal body weight should be
used to compute doses. Because the doses are given in terms of theophylline,
doses for other theophylline salt forms need to be adjusted accordingly (S = 0.85
for anhydrous aminophylline, S = 0.8 for aminophylline dihydrate, S = 0.65 for
oxtriphylline).
• If theophylline is to be given orally, the dose given in Table 18-4 (in mg/kg/h) must
be multiplied by the appropriate dosage interval for the dosage form being used: D
= (theophylline dose ⋅ Wt ⋅ τ)/S, where Wt is patient weight, τ is the dosage
interval, and S is the appropriate salt form correction factor for aminophylline or
oxtriphylline.
• If theophylline is to be given as a continuous iv infusion the following equation is
used to compute the infusion rate: k0 = (theophylline dose ⋅ Wt)/S, where Wt is
patient weight and S is the appropriate salt form correction factor for
aminophylline.
• When more than one disease state or condition is present in a patient, choosing
the lowest dose suggested by Table 18-4 will result in the safest, most conservative
dosage recommendation. If an iv loading dose is necessary, theophylline 5 mg/kg
or aminophylline 6 mg/kg is used; ideal body weight is used to compute loading
doses for obese patients (>30% over ideal body weight).
(Bauer, 2008 : 776-777)
(Bauer, 2008 : 776)
CHIOU METHOD
BAUER, 2008 : 770
BAYESIAN PHARMACOKINETIC
COMPUTER PROGRAMS
The most reliable computer programs use a nonlinear regression
algorithm that incorporates components of Bayes’ theorem.
Nonlinear regression is a statistical technique that uses an iterative
process to compute the best pharmacokinetic parameters for a
concentration/time data set.
Briefly, the patient’s drug dosage schedule and serum
concentrations are input into the computer. The computer program
has a pharmacokinetic equation preprogrammed for the drug and
administration method (oral, intravenous bolus, intravenous
infusion, etc.).
Typically, a one-compartment model is used,
BAUER. 2008 : 772
Bayes’ theorem is used in the computer algorithm to
balance the results of the computations between values
based solely on the patient’s serum drug concentrations
and those based only on patient population parameters.
Some clinicians use Bayesian pharmacokinetic computer
programs exclusively to alter drug doses based on serum
concentrations.
An advantage of this approach is that consistent dosage
recommendations are made when several different
practitioners are involved in therapeutic drug monitoring
programs.
BAUER. 2008 : 772
DOSING STRATEGIES
BAUER. 2008 : 774
USE OF THEOPHYLLINE BOOSTER
DOSES TO IMMEDIATELY INCREASE
SERUM CONCENTRATIONS
A modified loading dose equation is used to
accomplish computation of the booster dose
(BD) which takes into account the current
theophylline concentration present in the
patient:
BAUER. 2008 : 775
Where :
C desired : the desired theophylline
concentration,
C actual : the actual current
theophylline concentration for the patient,
S : the fraction of the
theophylline salt form that is active
theophylline,
V : the volume of distribution
for theophylline.
BAUER. 2008 : 775
CONVERSION OF THEOPHYLLINE
DOSES FROM INTRAVENOUS TO ORAL
ROUTE OF ADMINISTRATION
Occasionally there is a need to convert a patient stabilized on theophylline
therapy from the oral route of administration to an equivalent continuous
infusion or vice versa. In general, oral theophylline dosage forms, including
most sustained-release tablets andcapsules, have a bioavailability equal to
one. Assuming that equal theophylline serum concentrations are desired, this
makes conversion between the intravenous
[k0 = (Css ⋅ Cl)/S] and oral [D = (Css ⋅ Cl ⋅ τ)/(F ⋅ S)]
routes of administration simple equivalent doses of drug (corrected for
theophylline salt form) are prescribed:
k0 = Dpo/(24 h/d ⋅ Siv) or Dpo = Siv ⋅ k0 ⋅ 24 h/d
where k0 is the equivalent intravenous infusion rate for the theophylline salt
in milligrams per hour, Dpo is equivalent dose of oral theophylline in
milligrams per day, and Siv is the fraction of the intravenously administered
theophylline salt form that is active theophylline.
REMOVAL OF THEOPHYLLINE BODY
STORES IN MANAGEMENT OF
THEOPHYLLINE OVERDOSE
Extracorporeal methods to remove theophylline in emergency
situations include hemodialysis and charcoal hemoperfusion.
Hemoperfusion is a technique similar to hemodialysis except
the blood is passed through a column of activated charcoal
instead of through an artificial kidney.
Theophylline can also be removed from the body using oral
doses of activated charcoal. Activated charcoal physically
adsorbss theophylline rendering it nonabsorbable from the
gastrointestinal tract.
BAUER. 2008 : 776
REFERENCES
• Bauer, Larry A. 2008. Applied Clinical
Pharmacokinetics. First Edition.USA : The
McGraw-Hill Companies.
You might also like
- RA5921 10918 ComparisonDocument50 pagesRA5921 10918 ComparisonAlfie1680% (40)
- Pediatric Hematology Oncology Ward Officer HandbookDocument40 pagesPediatric Hematology Oncology Ward Officer HandbookAnonymous FSUnLYr4yNo ratings yet
- Drug calculation practice problemsDocument2 pagesDrug calculation practice problemsTati KimNo ratings yet
- FDA Inspection Checklist for Sardam Drugstore RoutineDocument3 pagesFDA Inspection Checklist for Sardam Drugstore RoutineJohanna MonroyNo ratings yet
- Good Faith Dispensing GuidelinesDocument3 pagesGood Faith Dispensing GuidelinesKerriNo ratings yet
- Asthma Broncial (Theophylline)Document41 pagesAsthma Broncial (Theophylline)Nadya Zahra Henni100% (1)
- Asha Nayshalya Jafri (1511011004) Winny Rhamadani (1511011005) Nadya Prafita (1511011007) Indriyani (1511011008) Hurul Aini (1511011011)Document40 pagesAsha Nayshalya Jafri (1511011004) Winny Rhamadani (1511011005) Nadya Prafita (1511011007) Indriyani (1511011008) Hurul Aini (1511011011)Nadya PrafitaNo ratings yet
- Asthma Bronchial Treatment TheophyllinDocument27 pagesAsthma Bronchial Treatment TheophyllinAci LusianaNo ratings yet
- TeofilinDocument18 pagesTeofilinMARIA DEWINo ratings yet
- Theophylline by DP 307 936,933,946,956Document10 pagesTheophylline by DP 307 936,933,946,956Muhammad AbdullahNo ratings yet
- Theophylline: Yeli Pandu Gustia 0811012071Document31 pagesTheophylline: Yeli Pandu Gustia 0811012071Yeli Pandu Gustia100% (1)
- AMINOPHYLLINE INJECTION DOSAGE AND ADMINISTRATIONDocument12 pagesAMINOPHYLLINE INJECTION DOSAGE AND ADMINISTRATIONWendra PrastowoNo ratings yet
- Farmakokinetik Klinik TeofilinDocument18 pagesFarmakokinetik Klinik TeofilinTessarinaNo ratings yet
- Studies Suggest That RedDocument17 pagesStudies Suggest That Redlia lykimNo ratings yet
- 5241 PDFDocument14 pages5241 PDFicaeeNo ratings yet
- Aminophylline: InjectionDocument14 pagesAminophylline: InjectionEko Dian SyafithraNo ratings yet
- Theophylline and Caffeine Toxicity: DR - Qayssar Joudah Fadheel Ph.D.Pharmacology and TherapeuticsDocument24 pagesTheophylline and Caffeine Toxicity: DR - Qayssar Joudah Fadheel Ph.D.Pharmacology and TherapeuticsMustafa Salah MahdiNo ratings yet
- Pediatric Hematology Oncology Ward Officer HandbookDocument40 pagesPediatric Hematology Oncology Ward Officer HandbookLetchumana KrishnanNo ratings yet
- Hypothyroidism and Myxedema ComaDocument53 pagesHypothyroidism and Myxedema ComaKuba ArebaNo ratings yet
- Terbutalin SulfatDocument2 pagesTerbutalin SulfatZainab WowoussNo ratings yet
- Summary of RetigabineDocument117 pagesSummary of RetigabineAsher2225No ratings yet
- Aminophylline For Treating Asthma and Chronic Obstructive Pulmonary DiseaseDocument0 pagesAminophylline For Treating Asthma and Chronic Obstructive Pulmonary DiseaseOkky Winang SaktyawanNo ratings yet
- Theophylline or CaffeineDocument4 pagesTheophylline or CaffeineDebora ChenNo ratings yet
- Topotecan powder for infusion SPC summaryDocument59 pagesTopotecan powder for infusion SPC summaryBRDNo ratings yet
- Duplimuab Efficacy in AsthmaDocument37 pagesDuplimuab Efficacy in Asthmasruthimeena6891No ratings yet
- Jurnal CimetidineDocument7 pagesJurnal CimetidineAidahNo ratings yet
- LithiumDocument21 pagesLithiumvikaseptideyaniNo ratings yet
- Tumor Lysis Syndrome Guidelines 2014Document13 pagesTumor Lysis Syndrome Guidelines 2014Dinesh KamalNo ratings yet
- Nusrat Jahan Mim ID - 1920495 PHA 207 Sec-01 Assignment (THEOPHYLLINE)Document13 pagesNusrat Jahan Mim ID - 1920495 PHA 207 Sec-01 Assignment (THEOPHYLLINE)Mahadi Hasan KhanNo ratings yet
- TDM of PhenytoinDocument5 pagesTDM of PhenytoinMounika16 PedamalluNo ratings yet
- Allopurinol tablets summary of product characteristicsDocument12 pagesAllopurinol tablets summary of product characteristicsasdwasdNo ratings yet
- TB 2 FollowupDocument1 pageTB 2 FollowupJohn OmandacNo ratings yet
- Lidocaine Dosing and Monitoring GuideDocument27 pagesLidocaine Dosing and Monitoring GuideNadya PrafitaNo ratings yet
- Albumin Guidelines UHS April 2010Document5 pagesAlbumin Guidelines UHS April 2010dradrianramdhanyNo ratings yet
- trelegy-ellipta-epar-product-information_enDocument44 pagestrelegy-ellipta-epar-product-information_enandricmilovan888No ratings yet
- Theophylline Dosing & Side EffectsDocument3 pagesTheophylline Dosing & Side EffectsWindy Gigiers SeptianiNo ratings yet
- Tylenol Overdose: Causes, Symptoms and TreatmentDocument9 pagesTylenol Overdose: Causes, Symptoms and TreatmentTyler HempelNo ratings yet
- 10-Disease State PharmacokineticsDocument44 pages10-Disease State PharmacokineticsKerolus Joseph AminNo ratings yet
- Name of The Medicinal Product: 4.1 Therapeutic IndicationsDocument4 pagesName of The Medicinal Product: 4.1 Therapeutic IndicationsIndah BryanKeyNo ratings yet
- Azathioprine: Class: IndicationsDocument3 pagesAzathioprine: Class: IndicationsAnna GozaliNo ratings yet
- Intro To Clinical PharmacokineticsDocument71 pagesIntro To Clinical PharmacokineticsMa. Blesilda Michaela SarbuesNo ratings yet
- Seretide Accuhaler Provides Effective Asthma ReliefDocument17 pagesSeretide Accuhaler Provides Effective Asthma ReliefSagacious Veracity0% (1)
- 0.1.clinical PharmacokineticsDocument60 pages0.1.clinical PharmacokineticsSolomon D FatormaNo ratings yet
- Intravenous Anaesthetic AgentsDocument6 pagesIntravenous Anaesthetic AgentsSuresh KumarNo ratings yet
- How To Interpret Thyroid Function TestDocument5 pagesHow To Interpret Thyroid Function TestSiveshKathirKamarajahNo ratings yet
- EtosuksimidDocument14 pagesEtosuksimidMaharani IndriatyNo ratings yet
- Bahan Translate Biofar Pak OpikDocument1 pageBahan Translate Biofar Pak OpikPuty Prianti Novira100% (1)
- Aminophylline (Theophylline Ethylenediamine) : TruphyllineDocument4 pagesAminophylline (Theophylline Ethylenediamine) : TruphyllineRosalie SepayaNo ratings yet
- Tpnlabmonitoring PDFDocument5 pagesTpnlabmonitoring PDFMohamad SamirNo ratings yet
- Aminophylline Loading and Maintenance Dose v3Document3 pagesAminophylline Loading and Maintenance Dose v3Tera SurbaktiNo ratings yet
- Adrenergic AntagonistDocument29 pagesAdrenergic AntagonistAreesha ArifNo ratings yet
- CP 3Document71 pagesCP 3Bandameedi Ramu100% (1)
- Total Parenteral NutritionDocument9 pagesTotal Parenteral NutritionUday Kumar100% (1)
- Hepari̇n İnfüzyon ŞemasiDocument4 pagesHepari̇n İnfüzyon ŞemasiAhmet MercanNo ratings yet
- Parmacon Ass EdtDocument5 pagesParmacon Ass EdtMalcolm SharfNo ratings yet
- TB Special SituationsDocument34 pagesTB Special SituationsAyu AriestaNo ratings yet
- Therapeutic Drug Monitoring:: TheophyllineDocument23 pagesTherapeutic Drug Monitoring:: Theophyllinekiki rawitriNo ratings yet
- Acetamenophen ToxicityDocument10 pagesAcetamenophen Toxicityknowlegebook6No ratings yet
- KetosterilDocument2 pagesKetosterilmonia agni wiyatamiNo ratings yet
- Excretion and Elimination KineticsDocument39 pagesExcretion and Elimination KineticsYashasv BhatnagarNo ratings yet
- The Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016Document10 pagesThe Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016ddandan_2No ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Ajg 2017154 ADocument26 pagesAjg 2017154 ADelisaPutriChaniagoNo ratings yet
- Ferment As IDocument17 pagesFerment As IDelisaPutriChaniagoNo ratings yet
- AbeDocument8 pagesAbeDelisaPutriChaniagoNo ratings yet
- Ketahanan (Jasni Sri)Document9 pagesKetahanan (Jasni Sri)DelisaPutriChaniagoNo ratings yet
- Sterilisation of Medical DevicesDocument49 pagesSterilisation of Medical DevicesYogesh BorkarNo ratings yet
- Zyto Ardim, Dadang Sugiana, Uud Wahyudin Departemen Ilmu Manajemen Komunikasi Fakultas Ilmu Komunikasi Universitas PadjadjaranDocument15 pagesZyto Ardim, Dadang Sugiana, Uud Wahyudin Departemen Ilmu Manajemen Komunikasi Fakultas Ilmu Komunikasi Universitas PadjadjaranDelisaPutriChaniagoNo ratings yet
- NCD Report Annex1Document2 pagesNCD Report Annex1DelisaPutriChaniagoNo ratings yet
- Isotonic SolutionsDocument4 pagesIsotonic SolutionsMohamed BolbolNo ratings yet
- S6156e PDFDocument10 pagesS6156e PDFDelisaPutriChaniagoNo ratings yet
- 09 t2-4 - Shao JunDocument35 pages09 t2-4 - Shao JunDelisaPutriChaniagoNo ratings yet
- Daftar Obat LasaDocument8 pagesDaftar Obat LasaAmbar SulistyawanNo ratings yet
- Interaksi Obat Pada Tahap MetabolismeDocument10 pagesInteraksi Obat Pada Tahap MetabolismeNurul AsmiiyahNo ratings yet
- PRODUCT LIST MARKETING ETHICSDocument4 pagesPRODUCT LIST MARKETING ETHICSPaten PisanNo ratings yet
- MTUS Drug ListDocument1 pageMTUS Drug List9300187476No ratings yet
- Contoh Gol. Obat KIEDocument3 pagesContoh Gol. Obat KIEAndre D. Cahya100% (1)
- FDA FOIA Log - May 2022Document132 pagesFDA FOIA Log - May 2022Mayra MayaNo ratings yet
- Rekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFDocument11 pagesRekapitulasi Laporan Narkotika: NO Nama Satuan Stok Awal Pemasukan PBFBang23 ManikNo ratings yet
- Development and In-Vitro Evaluation of Catechin Loaded Ethosomal Gel For Topical DeliveryDocument6 pagesDevelopment and In-Vitro Evaluation of Catechin Loaded Ethosomal Gel For Topical DeliveryRAPPORTS DE PHARMACIENo ratings yet
- CDER Fast Track Products ApprovedDocument5 pagesCDER Fast Track Products ApproveddianNo ratings yet
- DAFTAR OBAT ApotekDocument3 pagesDAFTAR OBAT ApotekRiskiah NurfathinNo ratings yet
- A Current Review of Cytochrome P450 Interactions of Psychotropic DrugsDocument19 pagesA Current Review of Cytochrome P450 Interactions of Psychotropic Drugsdrguillermomedina100% (1)
- Immacule Product List - Injectables UpdatedDocument1 pageImmacule Product List - Injectables Updatedsanjay_gawaliNo ratings yet
- Common Drugs in SA MedicineDocument8 pagesCommon Drugs in SA MedicineJordan PetersNo ratings yet
- Daftar Pustaka FarmasiDocument3 pagesDaftar Pustaka Farmasipermata putriNo ratings yet
- Parenteral Medication Labels and Dosage CalculationDocument22 pagesParenteral Medication Labels and Dosage CalculationlisaNo ratings yet
- Presentasi Faisal Maulana Ibrahim TICADocument27 pagesPresentasi Faisal Maulana Ibrahim TICAFAISAL IBRAHIMNo ratings yet
- All Questions of D.FDocument18 pagesAll Questions of D.FYamaan Yamaan100% (1)
- Para SubirDocument1,125 pagesPara SubiralfredolavinNo ratings yet
- 0700 - 3110 StockDocument37 pages0700 - 3110 Stockparhananshori23No ratings yet
- PHAR 7633 Chapter 1 Online Resources: IndexDocument7 pagesPHAR 7633 Chapter 1 Online Resources: IndexkbnarkhedeNo ratings yet
- 14860Document3 pages14860Sahil DhamijaNo ratings yet
- 5. nhũ dịch, hỗn dịchDocument6 pages5. nhũ dịch, hỗn dịchTrần Thị NhungNo ratings yet
- Table of Contents CTD FormatDocument5 pagesTable of Contents CTD Formatgsharma20203158No ratings yet
- Keywords: Enzymology, Drug, Michaelis-Menten Equation, Pharmacokinetics, ToxicityDocument25 pagesKeywords: Enzymology, Drug, Michaelis-Menten Equation, Pharmacokinetics, Toxicityירדן לויןNo ratings yet
- Scholar 2007Document6 pagesScholar 2007Evelyn LimNo ratings yet
- Drug StudyDocument2 pagesDrug Studymegreen GamingNo ratings yet