Professional Documents
Culture Documents
Aki
Aki
Uploaded by
tutorial D10 ratings0% found this document useful (0 votes)
0 views15 pagesOriginal Title
127691_AKI.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
0 views15 pagesAki
Aki
Uploaded by
tutorial D1Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 15
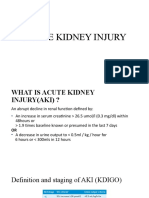
KDIGO Definition of AKI ( 2012 )
Defined by any of the following:
Increase in SCr by ≥0.3 mg/dL within 48 hours
Increase in Scr by ≥1.5 times baseline, which is known or
presumed to have occurred within the prior seven days
Urine volume <0.5 mL/kg/h for six hours
KDIGO Classification of AKI ( 2012 )
Stage Serum creatinine Urine output
1 1.5-1.9× baseline <0.5 ml/kg/hr for 6-12 hrs
OR
>0.3 mg/dL
<0.5 ml/kg/hr > 12 hrs
2 2-2.9× baseline
3 3 times baseline <0.3 ml/kg/hr > 24 hrs
OR OR
increase in Cr to ≥4.0 mg/dL Anuria > 12 hrs
OR
Initiation of RRT
KDIGO Clinical Practice Guideline for AKI. Kidney Int 2012
Prerenal AKI
Intravascular volume depletion:
-bleeding, GI loss, Renal loss, Skin loss (burn), Third space loss, poor
oral intake (NPO, AMS, anorexia)
Decreased effective circulating volume:
-congestive heart failure, cirrhosis, nephrotic syndrome, sepsis
Decreased flow through renal artery:
-RAS or occlusion (compartment syndrome), hepatorenal syndrome,
hypercalcemia
-pharmacologic impairment (RAAS blocker, NSAIDs, CNI)
Prerenal Azotemia Tx
In early stages can be rapidly corrected by aggressive
normalization of effective arterial volume.
Correction of volume deficits
Optimization of cardiac function
Discontinuation of antagonizing medications
NSAIDs/COX-2 inhibitors
Diuretics
RAAS blockers
Renal / Intrinsic AKI
Tubule: ATN (sepsis, ischemic, toxins)
Interstitium: AIN (Drug, infection, neoplasm)
Glomerulus: AGN (primary, post-infectious,
rheumatologic, vasculitis, HUS/TTP)
Vasculature:
Atheroembolic dz, renal artery thromboembolism, renal artery
dissection, renal vein thrombosis
Intratubular Obstruction
myoglobin, hemoglobin, myeloma light chains,
uric acid, tumor lysis, drugs (bactrim, indinavir,
acyclovir, foscarnet, oxalate in ethylene glycol toxicity)
Acute Tubular Necrosis (ATN)
Direct toxic Injury (20%)
Sepsis (48%)
Exogenous
Ischemia (32%) Radiocontrast
prolonged prerenal azotemia Aminoglycosides
Vancomycin
Hypotension Amphotericin B
hypovolemic shock Cisplatin
cardiopulmonary arrest Acyclovir
Calcineurin inhibitors
cardiopulmonary bypass HIV meds (tenofovir)
Endogenous (pigment
nephropathy)
Rhabdomyolysis
Hemolysis
Postrenal AKI: Classification
Level of obstruction
Upper tract (ureters)
Lower tract (bladder outlet or urethra)
Degree of obstruction
Partial vs. Complete
Type
Anatomic lesion (unilateral vs. bilateral)
Functional
Duration (Acute vs Chronic)
Cause (Congenital vs Acquired)
Etiologies: Upper tract
obstruction
Intrinsic: Extrinsic:
Nephrolithiasis Retroperitoneal or pelvic
Blood clot malignancy
Papillary necrosis Endometriosis/Prolapsed
Cancer uterus
Abdominal aortic
aneurysm or Iliac artery
aneurysm
Retroperitoneal fibrosis
Etiologies: Lower tract
obstruction
BPH or prostate cancer
Bladder cancer
Urethral strictures
Bladder stones
Blood clots
Functional obstruction as a result of
neurogenic bladder
Postrenal AKI tx
Prompt recognition and relief of obstruction can prevent the
development of permanent structural damage.
Lower tract obstruction (bladder catheter)
Upper tract obstruction
ureteral stents
percutaneous nephrostomies
Monitor for post-obstructive diuresis
Recovery of renal function dependent upon duration of
obstruction.
U/A, Urine protein/Cr, Urine Eosinophilla
FeNa, FeUrea
CPK, uric acid
Urine microscopy:
Muddy brown casts in ATN
WBC casts in AIN
RBC casts in AGN
Post-void residual (>100-150 ml c/w voiding dysfunction)
bladder catheterization
renal ultrasound
Management of AKI: general principle
No therapy to date have shown efficacy in treating
AKI.
Identify the etiology and treat the underlying cause
Optimization of hemodynamics to increase renal
perfusion
Lack of benefit – low dose dopamine, loop diuretics
only if markedly fluid overload
Identify and aggressively treat infection (early
removal of foley catheters, and minimize indwelling
lines)
Management of AKI:
treat complications
Correct fluid imbalances: strict I/O’s, daily wts. determine
fluid balance goals daily, fluid selection or diuresis, readjust for
UOP recovery, post diuresis or dialysis
Electrolyte imbalances (low K/phos diet, binder)
Metabolic acidosis (Bicarb deficit, mode and rate of
replacement)
Nutrition: adjust TPN/protein intake
Medication dosing: adjustment for eGFR to avoid under or over
dosing, timing for dialytic therapy, reassess dosing for renal
recovery or dialysis modality)
Procedural considerations (prefer non-contrast CT,
appropriate to delay contrast exposure, prophylaxis)
You might also like
- Acute Renal FailureDocument34 pagesAcute Renal Failureaibaloca67% (9)
- Acute Kidney InjuryDocument60 pagesAcute Kidney InjuryAbegail Fermanejo-GeneraoNo ratings yet
- Noel A. Villanueva, MD, FPCP, FPSNDocument62 pagesNoel A. Villanueva, MD, FPCP, FPSNagilNo ratings yet
- Acute Pancreatitis: Sudden Severe Abdominal Pain Systemic UpsetDocument40 pagesAcute Pancreatitis: Sudden Severe Abdominal Pain Systemic UpsetcoolcaesarNo ratings yet
- Integrated Therapeutics IiDocument165 pagesIntegrated Therapeutics IiSalahadinNo ratings yet
- Acute Pancreatitis CPCDocument38 pagesAcute Pancreatitis CPCSariu Ali DidiNo ratings yet
- Acute Kidney Injury (AKI)Document50 pagesAcute Kidney Injury (AKI)Omar AbdillahiNo ratings yet
- Acute Kidney InjuryDocument62 pagesAcute Kidney InjuryApidha KartinasariNo ratings yet
- Obat-Obat NefrotoksikDocument43 pagesObat-Obat Nefrotoksiknursidiq10100% (1)
- Prof. Syakib Acute Kidney Injury - Internal Medicine Emergency Course - Agustus 2019-DikonversiDocument35 pagesProf. Syakib Acute Kidney Injury - Internal Medicine Emergency Course - Agustus 2019-DikonversidrroytambunanNo ratings yet
- Aki - CKDDocument51 pagesAki - CKDAyu Luh Ratri WeningNo ratings yet
- Approach To Acute Kidney InjuryDocument44 pagesApproach To Acute Kidney InjuryKue GosongNo ratings yet
- Final AKI For IM 2014Document45 pagesFinal AKI For IM 2014Andika Yusuf RamadhanNo ratings yet
- Approach To Acute Renal FailureDocument40 pagesApproach To Acute Renal FailureMochammad Fariz AmsalNo ratings yet
- Acute Renal Failure or Acute Kidney InjuryDocument8 pagesAcute Renal Failure or Acute Kidney InjuryHemanth PrakashNo ratings yet
- Acute Kidney Injury-Handout: Definition (NICE 2014)Document2 pagesAcute Kidney Injury-Handout: Definition (NICE 2014)Diane-Richie PezLoNo ratings yet
- AkiDocument38 pagesAkiPhillip MartinezNo ratings yet
- 22.AKI ProtocolDocument2 pages22.AKI ProtocolRed DevilNo ratings yet
- Acute Kidney Injury: Syakib BakriDocument46 pagesAcute Kidney Injury: Syakib BakriBhisma D. SyaputraNo ratings yet
- 1 Acute Renal FailureDocument65 pages1 Acute Renal FailureDammaqsaa W BiyyanaaNo ratings yet
- ACUTE KIDNEY INJURY. 2016m UNISMUHDocument26 pagesACUTE KIDNEY INJURY. 2016m UNISMUHWhulandary DyaswaraNo ratings yet
- Acute Kidney InjuryDocument42 pagesAcute Kidney InjurysushmaNo ratings yet
- Renal Acute Kidney InjuryDocument41 pagesRenal Acute Kidney InjuryTim SilvaNo ratings yet
- 12a. Kuliah Aki 2017Document36 pages12a. Kuliah Aki 2017yussikafernandaNo ratings yet
- Dr. Tjatur Winarsanto SPPDDocument37 pagesDr. Tjatur Winarsanto SPPDEndah Risky GustiyantiNo ratings yet
- Acute Kidney InjuryDocument26 pagesAcute Kidney InjuryUmmuhani AbubakarNo ratings yet
- Materi 7 - Gagal Ginjal AkutDocument30 pagesMateri 7 - Gagal Ginjal AkutTegar Muhamad RifkiNo ratings yet
- Acute Kidney InjuryDocument40 pagesAcute Kidney InjuryNabin SimkhadaNo ratings yet
- Acute Kidney Injury AKIDocument6 pagesAcute Kidney Injury AKIfazeel shah vlogsNo ratings yet
- Acute Renal FailureDocument75 pagesAcute Renal FailureAshwin Raghav SankarNo ratings yet
- RENAL Short CutsDocument3 pagesRENAL Short Cutssam ngNo ratings yet
- Acute Kidney Injury: Mohammad RudiansyahDocument80 pagesAcute Kidney Injury: Mohammad Rudiansyahshrt gtNo ratings yet
- Dr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalDocument81 pagesDr.P.Sankaranarayanan MD: Emeritus Professor of Medicine Acs Medical College & HospitalvaishnaviNo ratings yet
- Pancreatitis AcuteDocument42 pagesPancreatitis AcutearistadevyaNo ratings yet
- Acute Kidney Injury and Chronic Kidney DiseaseDocument44 pagesAcute Kidney Injury and Chronic Kidney DiseaseIda Bagus Putu Swabawa100% (1)
- Acute Kidney Injuri: Professor Ibrahim UmmateDocument46 pagesAcute Kidney Injuri: Professor Ibrahim UmmateElvis obajeNo ratings yet
- Acrf CDocument70 pagesAcrf CHussain AzharNo ratings yet
- Gangguan Ginjal Akut ("Acute Kidney Injury") : Prof. Dr. Dr. Adrian Umboh, Sp.A (K)Document22 pagesGangguan Ginjal Akut ("Acute Kidney Injury") : Prof. Dr. Dr. Adrian Umboh, Sp.A (K)Hans NatanaelNo ratings yet
- Renal DisordersDocument164 pagesRenal Disorderspblinder1319No ratings yet
- 11.0 Acute Kidney InjuryDocument26 pages11.0 Acute Kidney InjuryHeny KsNo ratings yet
- L11 Renal Failure General Approach 230213 002819Document16 pagesL11 Renal Failure General Approach 230213 002819S sNo ratings yet
- Lecture - Acute Renal FailureDocument57 pagesLecture - Acute Renal FailureJames StiltonNo ratings yet
- Acute Kidney Injury (AKI) : Haerani Rasyid FK Unhas 2016Document46 pagesAcute Kidney Injury (AKI) : Haerani Rasyid FK Unhas 2016Ana Yusriana AzzahraNo ratings yet
- Acute Kidney Injury: Dana BabaDocument31 pagesAcute Kidney Injury: Dana Babanaheel98shNo ratings yet
- Pathophysiology of Acute Kidney Injury (Aki) Caused by ShockDocument26 pagesPathophysiology of Acute Kidney Injury (Aki) Caused by ShockbokobokobokanNo ratings yet
- Acute and Chronic Renal Failure MyDocument45 pagesAcute and Chronic Renal Failure MyJoseph Krafft100% (3)
- Cirrhosis AndrewDocument33 pagesCirrhosis Andrewlionel andreaNo ratings yet
- Inter'Medic AKIDocument48 pagesInter'Medic AKIMAHEJS HDNo ratings yet
- Acute Kidney Injury: in The ClinicDocument29 pagesAcute Kidney Injury: in The ClinicAnitha SNo ratings yet
- CHOLECYSTITISDocument6 pagesCHOLECYSTITISAnar ChuluunNo ratings yet
- Tubulopathies. Interstitial NephritisDocument34 pagesTubulopathies. Interstitial NephritisIaros OlgaNo ratings yet
- Acute Renal Failure Acute Kidney Injury: (ARF and AKI)Document38 pagesAcute Renal Failure Acute Kidney Injury: (ARF and AKI)Vinod VijjeswarapuNo ratings yet
- Renal Faliure 1Document50 pagesRenal Faliure 1180045No ratings yet
- Nephrology NewDocument93 pagesNephrology Newsaeedassaf97No ratings yet
- AkiDocument42 pagesAkimarauder_popNo ratings yet
- Acute Renal FailureDocument30 pagesAcute Renal FailureCarmina SalvañaNo ratings yet
- Acute Kidney Injury: Ahmad Fariz Malvi Zamzam ZeinDocument30 pagesAcute Kidney Injury: Ahmad Fariz Malvi Zamzam ZeinFatwa Dea Ramdani OctaviyasminNo ratings yet
- Nephro Meets OncoDocument90 pagesNephro Meets OncoRenal Association MauritiusNo ratings yet
- Dna IsolationDocument58 pagesDna IsolationTitisPudyatikaDestyaAndiraNo ratings yet
- Cmped 10 2016 067 PDFDocument17 pagesCmped 10 2016 067 PDFTitisPudyatikaDestyaAndiraNo ratings yet
- Multifetal Pregnancy: Herman Sumawan FK Unsoed/Rs Margono SoekarjoDocument70 pagesMultifetal Pregnancy: Herman Sumawan FK Unsoed/Rs Margono SoekarjoTitisPudyatikaDestyaAndiraNo ratings yet
- Psikologi BencanaDocument19 pagesPsikologi BencanaTitisPudyatikaDestyaAndiraNo ratings yet