Professional Documents
Culture Documents
JR Inka
Uploaded by
Inka Nadya Triayesha0 ratings0% found this document useful (0 votes)
46 views10 pagesOriginal Title
JR inka.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
46 views10 pagesJR Inka
Uploaded by
Inka Nadya TriayeshaCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 10
Intravenous paracetamol vs dexketoprofen vs
morphine in acute mechanical low back pain
in the emergency department: a randomized
double-blind controlled trial
Cenker Eken, Mustafa Serinken, Hayri Elicabuk, Emrah Uyanik, Muhammed Erdal
Emergency Medical Journal. 2014;31:177–181
Inka Nadya Tri Ayesha
4151151402
INTRODUCTION
• Acute mechanical low back pain (LBP) is one of the most
common complaints at the emergency department,
accounting for more than six million cases in the USA
• Therapy for acute LBP aims to relieve pain and improve
function. NSAIDs and opioids can be used for acute LBP in
the ED
• Opioids are effective analgesics that act rapidly, but
have side effects such as hypotension, nausea, vomiting
and dizziness. NSAIDs are not less effective than opioids
with less rescue medication and side effects
• Intravenous paracetamol is a new and safe alternative to
NSAIDs and opioids
MATERIAL AND METHODS
Study design
Three treatment arms, intravenous paracetamol, intravenous
dexketoprofen and intravenous morphine were compared in
this single-center, prospective, randomised, double-blind,
controlled clinical trial. This study was planned as a
superiority trial
Participants
Adults (aged 18–55) with moderate or severe acute
mechanical LBP according to the 4-point VRS were
accepted as eligible for the study. Acute LBP was accepted
as having pain that started over the last week
Interventions
Study patients were randomised in a 1:1:1 ratio to receive
single IV dose of paracetamol (1g), dexketoprofen (5mg)
and morphine (0.1 mg/kg). Patients with inadequate pain
relief after 30 min received fentanyl as a rescue drug.
Methods of measurement
Measurement of pain intensity was performed by a 100
mm VAS and a 4-point VRS before the study drug
administration and at the 15th and 30th minutes. The need
for the rescue drug at the 30th minute was also recorded
Outcome measures
Primary: the change in VAS and VRS at the 15th and 30th
minutes. Secondary: the need for the rescue drug and
presence of adverse events
RESULTS
• A total of 874 patients were eligible for the study, and 737 of
them were excluded due to a variety of reasons. A total of 137
patients were randomised for the study.
• The median reduction in VAS score at the 30th minute for the
paracetamol group was 65 mm (95% CI 58 to 72), 67 mm (95%
CI 60 to 73) for the morphine group and 58 mm (95% CI 50 to 64)
for the dexketoprophen group. Although morphine was not superior
to paracetamol at 30 min (difference: 3.8±4.9 (95% CI −6 to 14),
the difference between morphine and dexketoprofen in reducing
pain was 11.2±4.7 (95% CI 2 to 21).
• A total of 17 patients required the rescue drug at the end of the
study. The rescue drug was required by 8 (17.4%) patients in
the paracetamol group, 2 patients (4.4%) in the morphine group
and 7 patients (15.2%) in the dexketoprofen group
• At least one adverse effect occurred in 8.7% (n=4) of the cases in
the paracetamol group, 15.5% (n=7) of the morphine group, and
8.7% (n=4) of the dexketoprophen group (p=0.482).
DISCUSSION
The presented study was the first to investigate the efficacy
of paracetamol and dexketoprofen in acute LBP in the ED.
Morphine decreased the pain intensity 15 mm more than
dexketoprofen with a lack of statistical significance, and 11
mm more than paracetamol at the 15th minute. Although
there was no difference between morphine and
paracetamol at the 30th minute, morphine decreased the
pain 11 mm more than dexketoprofen with a statistical
significance, but a lack of clinical significance. Patients in the
morphine group also required less rescue drug but
experienced more side effects, both of which occurred at a
lack of statistical significance.
Limitations
The measurements only the 15th and 30th minute VAS scores.
The delayed effects of these drugs should be the interest of
future studies. Instead of measuring the weight of patients,
we calculated the dose of morphine according to patient
statements.
CONCLUSION
Intravenous paracetamol, dexketoprofen and morphine are
not superior to each other for the treatment of mechanical
LBP in the ED.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Essentials of Geriatric PsychiatryDocument87 pagesEssentials of Geriatric PsychiatryFeisalAlykhanNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- DR Siraj AhmadDocument20 pagesDR Siraj AhmadswethaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
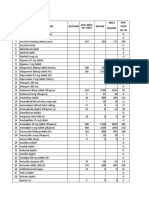
- Out of Stock Items List - Till Last Week.27 JunDocument65 pagesOut of Stock Items List - Till Last Week.27 Junmanuella ANo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Daftar ObatDocument1 pageDaftar ObatPramukadua DepokNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Websitecompanies NewDocument33 pagesWebsitecompanies NewRajiv JulakantiNo ratings yet
- NAPLEX Prep 2018 Ch01 CardioDocument56 pagesNAPLEX Prep 2018 Ch01 CardioFaith50% (2)
- Barang Bebas Buat PKPADocument152 pagesBarang Bebas Buat PKPABrian FoxNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- PharmacologyDocument84 pagesPharmacologyhenrydycoco100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Yovita - The Role of Clinical Pharmacist On Safe Administration AntibioticDocument48 pagesYovita - The Role of Clinical Pharmacist On Safe Administration AntibioticRois HasyimNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Stok Opname 2020Document63 pagesStok Opname 2020Hafizh JhunkoNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- MCQ PharmacologyDocument140 pagesMCQ PharmacologyVazeerNo ratings yet
- List of Basic Essential Medicines Ministry of Health Seychelles 2010Document14 pagesList of Basic Essential Medicines Ministry of Health Seychelles 2010portosinNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Food&Drug Interactions GuideDocument8 pagesFood&Drug Interactions GuideNiken SaraswatiNo ratings yet
- 460 Oxycodone in Pain ManagementDocument93 pages460 Oxycodone in Pain ManagementSinta Chaira Maulanisa100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Management of Asthma During Pregnancy: Symposium ContDocument6 pagesManagement of Asthma During Pregnancy: Symposium ContWulan CerankNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Aus Pi TargocidDocument5 pagesAus Pi TargocidAsto Ata InteristiNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Indrajit Barua Muthsuddy - 1620793049 - PHR 426 - Section-1Document13 pagesIndrajit Barua Muthsuddy - 1620793049 - PHR 426 - Section-1Indrajit BaruaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- 175 Anaesthesia and Psychiatric Drugs Part 2 Mood Stabilisers and Antipsychotics PDFDocument6 pages175 Anaesthesia and Psychiatric Drugs Part 2 Mood Stabilisers and Antipsychotics PDFWahyu Permata LisaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- WC ListDocument42 pagesWC ListyoganaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Cns Stimulants: (MOA and Uses)Document39 pagesCns Stimulants: (MOA and Uses)Mirza Shaharyar BaigNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Adults Parenteral Dilution Manual: Yousef AlomiDocument55 pagesAdults Parenteral Dilution Manual: Yousef AlomiAmeng GosimNo ratings yet
- Forbes - Ten Misleading Drug AdsDocument8 pagesForbes - Ten Misleading Drug AdsrdandapsNo ratings yet
- Giving Injections: Subcutaneous (SC), Intramuscular (Im) and Intravenous (Iv) 1. PurposeDocument9 pagesGiving Injections: Subcutaneous (SC), Intramuscular (Im) and Intravenous (Iv) 1. Purposemilliondreams009No ratings yet
- Danh Muc San Pham DHG 2016Document60 pagesDanh Muc San Pham DHG 2016Thư PhùngNo ratings yet
- Test Bank For Focus On Nursing Pharmacology 7th Edition by Karch All ChaptersDocument409 pagesTest Bank For Focus On Nursing Pharmacology 7th Edition by Karch All Chaptersabbie100% (1)
- Guideline On Good Pharmacovigilance Practices (GVP) Module VII - Periodic Safety Update Report (Rev 1)Document68 pagesGuideline On Good Pharmacovigilance Practices (GVP) Module VII - Periodic Safety Update Report (Rev 1)Salló TivadarNo ratings yet
- Role of Bempedoic Acid in Dyslipidemia ManagementDocument13 pagesRole of Bempedoic Acid in Dyslipidemia ManagementkkkljlkjNo ratings yet
- EE Tarek Exam Hints 2019-1Document83 pagesEE Tarek Exam Hints 2019-1Ibrahim Sayed AhmedNo ratings yet
- 6 Studii StatineDocument37 pages6 Studii Statinejust4uhopeNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- ALERGIDocument3 pagesALERGIdyahNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)