100% found this document useful (1 vote)
397 views29 pagesNeuro 101: Nursing Neuro Assessment: Kristen Ankrom, RN, SCRN, CCCC Stroke Coordinator Coliseum Medical Centers
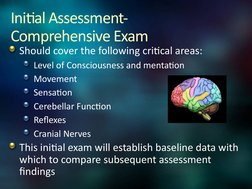
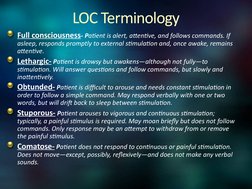
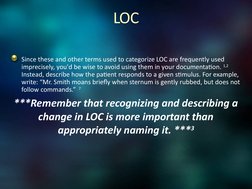
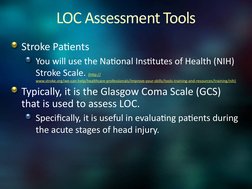
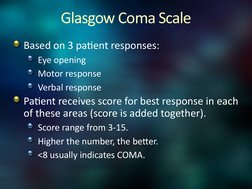
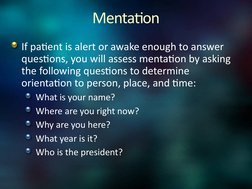
This document provides an overview of conducting a neuro assessment for nursing. It outlines the key areas to assess including level of consciousness, mentation, motor function, sensation, cerebellar function, reflexes, and cranial nerves. For each area, it describes the specific tests, responses to look for, and tools that may be used. The assessment establishes a baseline and monitors for changes that could indicate deterioration. Recognizing even subtle changes, like in level of consciousness, is emphasized as the most important part of neuro assessment for nurses.
Uploaded by
Darvin MathewCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
100% found this document useful (1 vote)
397 views29 pagesNeuro 101: Nursing Neuro Assessment: Kristen Ankrom, RN, SCRN, CCCC Stroke Coordinator Coliseum Medical Centers
This document provides an overview of conducting a neuro assessment for nursing. It outlines the key areas to assess including level of consciousness, mentation, motor function, sensation, cerebellar function, reflexes, and cranial nerves. For each area, it describes the specific tests, responses to look for, and tools that may be used. The assessment establishes a baseline and monitors for changes that could indicate deterioration. Recognizing even subtle changes, like in level of consciousness, is emphasized as the most important part of neuro assessment for nurses.
Uploaded by
Darvin MathewCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
- Introduction to Nursing Neuro Assessment: An overview of neuro assessment in nursing, introduced by the instructor's credentials and the training purpose.
- Initial Assessment: Details the areas covered in the initial comprehensive neuro assessment including consciousness and critical neurological functions.
- Assessing Neurological Signs: Covers methods and tools for assessing various neurological signs including mentation, pupil response, and motor function.
- Reflex Assessments: Explores deep tendon and superficial reflex tests, detailing the physiological responses expected during assessment.
- Cranial Nerve Evaluation: Comprehensive guide to evaluating each cranial nerve, including appropriate tests for sensory and motor functions.
- Vital Signs & Neuro Status: Discusses the integration of neuro assessments with vital signs, emphasizing the monitoring of changes in patients.
- Final Reminders and References: Provides key reminders for conducting neuro assessments effectively and consistently, followed by references for further reading.