0% found this document useful (0 votes)
160 views52 pagesSelmar Maribojo JR, MD First Year Medical Resident
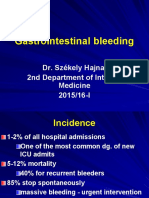
The document discusses gastrointestinal bleeding (GIB), which can present as overt or occult bleeding. It describes signs and symptoms of different types of GIB and evaluates patients based on heart rate, blood pressure, and hemoglobin levels. The most common causes of upper, small intestinal, and lower GIB are described. Management involves endoscopy for diagnosis and potential treatment. Medical therapies including proton pump inhibitors are discussed.
Uploaded by
Selmar Quimpo Maribojo Jr.Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
160 views52 pagesSelmar Maribojo JR, MD First Year Medical Resident
The document discusses gastrointestinal bleeding (GIB), which can present as overt or occult bleeding. It describes signs and symptoms of different types of GIB and evaluates patients based on heart rate, blood pressure, and hemoglobin levels. The most common causes of upper, small intestinal, and lower GIB are described. Management involves endoscopy for diagnosis and potential treatment. Medical therapies including proton pump inhibitors are discussed.
Uploaded by
Selmar Quimpo Maribojo Jr.Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd