Professional Documents
Culture Documents
Gastrointestinal Bleeding Full
Uploaded by
Anna Sofia ReyesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gastrointestinal Bleeding Full
Uploaded by
Anna Sofia ReyesCopyright:
Available Formats
GASTROINTESTINAL BLEEDING • Small and large intestines have no nerve endings
• can come from any of the areas in the digestive for us to determine kung nagkakaroon na ng
tract. pagkabulok.
• from the mouth to the anus • Compression/alteration in surrounding
• signs of bleeding in the digestive tract depend structures/blood vessels will give a hint to the px.
where it is and how much bleeding there is. • Possibility of pagkabulok of bowel.
• malaking factor sa amount of bleeding is kung • Ischemic portion can slough off and can cause
anong blood vessel yung affected. bleeding.
• Artery - more massive bleeding
• Manifestations will depend here Intussusception
• GI bleeding is a symptom of a disease or a • Telescoping of the small intestine into another part
condition, rather than a disease or condition itself. of the small intestine.
• When pxs come into the hospital with GI bleeding • Literally like a telescope.
assessment is important. Determine the root cause • Area na nagtelescope will be compressed and in
why the px is bleeding internally. the long run can necrotise and can slough off to
• Overt cause bleeding; or it can also cause an obstruction.
Meckel diverticulum
• Diverticula - out pouching
• Meckel diverticulum - occurs in the large intestine.
• Diverticulosis - small intestine
Increase build up of intraluminal pressure.
• Congenital defect that is said na karugtong ng
umbilcal cord ng isang neonate.
• Diverticulum can rupture and can cause bleeding
lalo na kapag may increaseed build up of pressure.
• Food particles na Hindi na-absorb or fecal material
can accumulate sa out pouches > can cause
inflammation > can cause rupture > can cause
bleeding
Angiodysplasia
bleeding can be recognized immediately unlike • Angio - blood vessel
occult bleeding. • Dysplasia - alteration of normal characteristic and
• the amount of bleeding can be so small that only a appearance of blood vessel
laboratory test can find it. • Increased BP can cause rupture.
Esophageal Varices Colonic cancer and rectosigmoid carcinoma
• varicosities/dilation ng mga blood vessels in the • Can cause lower GI bleeding.
esophageal are. Associated with portal • Cancer cell - needs blood supply. They create their
hypertension secondary to liver cirrhosis. own blood vessel (angiogenesis) - they branch it off
• A result of backflow of blood from hepatic the original blood vessel of the host. These vessels
circulation backward to the GI system because of are thin and can easily rupture > can cause
obstruction or inflammation or cirrhosis. bleeding.
Malory-Wise tear Inflammatory bowel disease
• Minute tear in the esophagaus • Classified into 2 diseases.
• Commonly associated with strenuous coughing or • 1. Regional enteritis - affects the small intestine
vomiting episodes (induced vomiting) • 2. Ulcerative colitis - affects primarily the colon
• Condition that promotes excessive diarrhea - some
Gastritis pxs can manifest bloody diarrhea.
• Inflammation of the lining of the gastric mucosa • Exact cause is unknown.
• Continuous exposure to insult will lead to ulcer >
perforation > tendency for bleeding episodes > Hemorrhoids
hemorrhagic gastritis - namumula lang muna but • Most common factor for lower Gi bleeding.
later on can cause bleeding. • Like outpouching pero kasama blood vessels.
• Secondary to constipation
Ischemic bowel disease • Px can also suffer from anal fissures.
• Ischemia in the bowel.
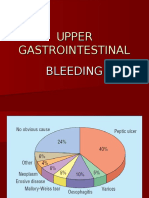
GI BLEEDING CLASSIFICATION
A. Visibility of bleeding:
• Occult bleeding: ulcerative colitis
Bleeding in quantities too small to be (UC) & Crohn
macroscopically observable (requires chemical disease (CD)
- Invasive or
tests or microscopic examination to be detected). inflammatory
Maaring capillaries lang diarrhea -
• Overt (visible) GI bleeding: bacterial
Macroscopically observable bleeding with gastroenteritis,
due to e.g.,
accompanying clinical symptoms. (e.g., anemia, shigella,
tachycardia) enterohemorrha
gic escherichia
B. Degree of bleeding: coli (EHEC)
• Acute GI bleeding: VASCULAR - esophageal varices - Hemorrhoids
Sudden and sever (sometimes) or gastric varices - Ischemia (e.g.,
Acute, massive bleeding - can lead to - Gastric antral ischemic colitis,
hypovolemic shock, and even death; vascular ectasia mesenteric
(“watermelon ischemia)
- Can occur at any age from birth. stomach”) - Arteriovenous
- Mas nakakatakot kapag very young or very - Dieulafoy lesion: malformation
old ang px. minor mucosal - Rectal varices
• Chronic GI bleeding: trauma to an
abnormal
Slight bleeding that can last a long time or may submucosal artery -
come and go aneurysm (usually
Minute GI bleeding; mahirap madetect located in the
Kapag may manifestations na like anemia tsaka proximal stomach)
leads to major
lang mas napapansin bleeding (acute
Prolonged microscopic bleeding - can lead to UGIB)
loss of iron, causing anemia.
- anglodysplasia: a
common
C. Site of bleeding is divided into: degenerative
• Upper GI bleeding - located between the mouth disorder of GI
and the upper part of the small intestine. vessels (mostly
venous) that can
~70% - 80% of GI hemorrhages
cause GI bleeding
The source of the bleeding is proximal to the in the stomach,
ligament of Treitz (suspensory muscle of the duodenum,
duodenum). jejunum, and colon.
• Associated with
It is characterized by hematemesis and melena.
age >60 years, von
Hematemesis - pagsuka ng dugo Willebrand disease,
Kapag hindi nasuka it can go down further sa GI aortic stenosis, and
tract and then lumabas as melena (or black tarry ESRD
• Manifests with
stools) because na-digest na yung blood along
episodic bleeding
the GI tract. (hemtochezia) that
About half of cases are due to PUD ceases
Esophagitis and erosive disease is the next most spontaneously
(>90% of cases)
common causes (also ulcers)
• Diagnosis usually
• Lower GI bleeding - located between the upper part requires
of the small intestine and the anus. anglography.
• ~20% - 30% of all GI hemorrhages • Lesions are usually
multiple tortuous
• The source of the bleeding is distal to the
dilated vessels
ligament of Treitz, usually in the colon. Most
• Hematochezia - passage of blood in the stool. commonly
• It may be indicated by passage of red blood located in the
discharge per rectum, especially in the absence right-sided colon
(~75%).
of hematemesis.
• The most common cause is hemorrhoids.
GI BLEEDING ETIOLOGIES • Crohn disease and inflammatory diarrhea - usually
ETIOLOGY UGIB LGIB
manifest bloody diarrhea.
• Ectasia - dilation of blood vessels
INFLAMMATO - PUD (`30% of - diverticulosis • Characteristic that signifies vascular ectasia is the
RY/ EROSIVE cases) (~30% of watermelon stomach (yung parang may stripes)
- Esophagitis cases)
- Erosive gastritis - Inflammatory Lining of the stomach is may parts na mapula tas
and/or duodenitis bowel disease may parts na pale.
(IBD) - i.e.,
• Dieulafoy lesion > aneurysm > can lead to mahor up in the relates to
bleeding stomach sexual acts
• Aneurysm - permanent dilation of an artery; arteries that involves
become weak. objects
• There are different types of aneurysm: inserted in the
Dissecting aneurysm - the different tunica’s ay na- anus)
infiltrate na **Following open or endoscopic surgery (e.g.,
Remember na arteries have high pressure so anastomotic bleeding following a gastric bypass)
kapag bumaba sya in areas na may dilation it can Other Postal Anal fissures
cause rupture Causes Hypersensitive
gastropathy –
Ischemia - Kapag ang isang area ng bowel sa small gastric mucosa
or large intestine ay nabubulok, pwedeng mapull out is inflamed,
yung area na yon na pwedeng reason for bleeding becomes
Arteriovenous malformation (AVM) edematous and
o Normally: Artery connects to a capillary then dilated blood
tsaka sa vein vessels
o In AVM, there is no capillary. Artery connects Coagulopathies
directly to a vein,which causes the problem.
o Because the capillary functions as a gradient INCIDENCE
that decreases the pressure. UGIB 100/100,000
o Therefore, kapag direct ang artery and vein, LGIB 20/100,000
hinid kakayanin ng walls ng veins ang high o Both are more common in males and elderly.
pressure blood flow ng artery kaya there is Bleeding from the upper respiratory tract (e.g.,
possibility of rupture, which is common sa mga nocturnal nosebleeds) can be mistaken for GI
may AVM. bleeding because the blood can be swallowed and
AVM- a congenital defect na walang capillary ang vomited or appear in the stool as melena. Careful
isang patient. examination and history taking is the key to
Von Willebrand – abnormal blood coagulation. differentiating respiratory sources of bleeding from
Aortic stenosis – narrowed path/opening of aortic GI ones.
valve
Angiography – visualization of the blood vessels
with the help of a contrast medium.
Specifically located in the right-sided colon
PROBABLY, yun yung area ng colon natin na
nagrereceive ng flow ng digested and undigested
food from the ileum na highly fluid pa.
ETIOLOGY UGIB LGIB
Tumors Esophageal Colorectal
cancer and/or cancer and/or
gastric anal cancer
carcinoma Colonic polyps
(grape-like
structures,
predispose to
colon cancer)
Traumatic Hiatal Hernias Lower
or Mallory-Weiss abdominal
Iatrogenic Syndrome (tear trauma -
in the blood Hemorrhoids Ligament of Treitz – the line to determine if it is an
vessel in the leading to upper or lower GI bleeding.
Esophagus) bleeding COMMON CAUSES OF GI BLEEDING
Boerhaave Anorectal Drug-Induced Corticosteroid
Syndrome trauma (e.g.,
NSAIDS
(Spontaneous anorectal
avulsion, Salicylates
Esophageal
rupture) – this is impalement Esophagus Esophageal varices
secondary to injuries) Esophagitis
extreme Anorectal Mallory-Weiss tear
pressure build avulsion Stomach and Duodenum Stomach Cancer
Hemorrhagic gastritis
PUD RISK ASSESSMENT
Polyps PRE-ENDOSCOPY
Stress-related o All patients with GI bleeding should be risk-
mucosal disease stratified to guide the diagnostic and
Systemic Diseases Blood dyscrasias therapeutic approach, timing of endoscopy,
(e.g., leukemia, and patient disposition.
aplastic anemia) LOWER-RISK CLINICAL SCENARIOS
Renal failure o Occult GI bleeding
- Hard to perform when patient experiences
RISK ASSESSMENT active massive bleeding.
GI Bleeding is not merely the disease, this is the - Risky on the part of the client
manifestation of underlying conditions. - EGD is not a priority procedure to do.
It is important to perform risk assessment to - We need to address the bleeding by giving
determine if the patient is at risk for GI bleeding. fluids to replenish or blood transfusion for
This is usually done of physicians. low hemoglobin or hematocrit levels
ENDOSCOPY o Scant intermittent hematochezia due to
The best determination of risks is through benign anorectal disease (e.g., hemorrhoid,
endoscopy anal fissure)
o Could be done in the Esophagus, gastro or HIGHER-RISK CLINICAL SCENARIOS
duodenum. Or sigmoid, recto-sigmoid or o Overt GI bleeding with high-risk features
colonoscopy. - see table below
o Determine where is the source of bleeding, what o Esophageal variceal bleeding
type of bleeding, etc. - Esophageal varices: dilated blood vessels
Pre-endoscopy on the esophagus. When you perform the
o All patients with GI bleeding should be risk- EGD procedure, there is an increase
stratified to guide the diagnostic and therapeutic likelihood to hit an area of dilated
approach, timing of endoscopy, and patient esophageal varices causing rupture and
disposition. bleeding. Ideally, this procedure is not done
Lower-risk clinical scenarios when there is suspected esophageal
o Occult GI Bleeding varices.
First address the bleeding. High-risk features of GI bleeding
o Scant intermittent hematochezia due to benign https://next.amboss.com/us/article/ZS0Zy2#Za9Ba909
anorectal disease (e.g., Hemorrhoids, anal ec46171fc7d61894f4c263065
fissure)
Higher-risk clinical scenarios Patient Factors Age >60 years
o Overt GI bleeding with high-risk feature - wala Chronic comorbidities
kang makikita kapag may massive bleeding and History of diverticulosis
mas risky or angioectasia (for
o Esophageal variceal bleeding. LGIB)
HIGH-RISK FEATURES OF GI BLEEDING -Ectasia: dilated blood
vessels
Patient factors Age >60 y/o
- Especially in the GI
Chronic comorbidities tract, there is a higher
History of diverticulitis chance of bleeding
or angioectasia (for associated with
LGIB) colonoscopy procedure
History of an AAA and enema (prior to
graft colonoscopy)
Features Presentation Hemodynamic History of an AAA graft
instability - Some patient
Ongoing bleeding experience dilation of
Anemia, HVT ≤ 355, abdominal aorta. Pag
coagulopathy, or tumaas/lumaki yung
elevated BUN dilation of blood vessel
Need to transfuse ≥ 6 (above 5.5 or 6cm in
units of packed RBCs diameter), there is an
Interpretation: >1 feature is associated with a risk of increase likelihood of
severe or recurrent bleeding rupture that may cause
massive bleeding. g/dL
Repair is necessary ≤ 10 ≤ 10 5
and patient is g/dL g/dL
candidate for AAA Clinical Systemic ≥ 110 mmHg 0
graft) Features Blood 100-109 mmHg 1
Features at Hemodynamic Pressure 90-99 mmHg 2
presentation instability ≤ 90 mmHg 3
Ongoing bleeding Additional Heart rate ≤ 1
Anemia, HCT ≤ 35%, Criteria 200/min
coagulopathy, or Melena at 1
elevated BUN presentation
- in relation in BUN, Syncope at 2
elevation of it may be presentation
caused by active GI Liver disease 2
bleeding due to the - Liver:
blood present in the responsible for
stomach that is producing the
metabolized and clotting factors
digested into urea. - If patient is
Need to transfuse ≥ 6 bleeding, and her
units of packed RBCs liver function is
Interpretation > 1 feature is associated with a risk of incapable to
severe or recurrent bleeding produce
UGIB scoring systems: coagulating
e.g., the Glasgow-Blatchford score (GBS) factor, further
Used to guide patient disposition in bleeding episode
hemodynamically stable patients with UGIB. is possible.
Along with other scoring system it helps estimate: Heart Failure 2
o The likelihood of rebleeding - Heart finds it
- Purpose of creating this scoring system is difficult to
compensate to
for proper categorization.
the decreasing
- GI bleeding is not the disease perse of the
fluid volume or
patient, it is more often a manifestation of an cardiac output
underlying gastrointestinal disorder. that is being
o The need for urgent hemostatic control circulated into the
o Mortality body.
Scores are directly proportional with risk of Interpretation
rebleeding and need for urgent intervention. Score 0 low-likelihood of rebleeding or need for
o Score ≥ 7 – associated with a higher urgent intervention.
likelihood of urgent endoscopic intervention Score ≥ 1 higher likelihood of rebleeding and or
and mortality. need for urgent intervention.
- Urgent endoscopic intervention: kailangang
susunugin yung blood vessels to create a Critical assessment is needed – who is more likely is
tamponade for the bleeding to stop. at risk to develop GI bleeding.
Glasgow-Blatchford score Detailed History must also be done.
Parameters Findings But if patient is suffering from massive bleeding,
Laboratory BUN ≤ 18.2 mg/dL 1 withhold the history taking, focus to the assessment
Features 18.2 mg/dL – 2 and address the current problem/physiological
22.3 g/dL status of the patient. Avoid the occurrence of
22.4 mg/dL – 3 hypovolemic shock.
27.9 mg/dL LGIB scoring systems:
28 mg/dL – 69.9 4 e.g., the Oakland score.
mg/dL This externally validated risk score based on
5 o Age
Hemoglobin Male Female o Sex
≥ 13 ≥ 12 0 o Prior admissions for LGIB
g/dL g/dL
o Vital signs
12-13 10-12 1
o DRE findings
g/dL g/dL
10-12 N/A 3 o Hemoglobin at admission
It can help identify patients at low risk of poor Age
outcomes who can be safely managed as ≤ 40 0
outpatients. 40-69 1
Variables comprising the Oakland score ≥ 70 2
Predictor Score component value Gender
Age Female 0
≤ 40 0 Male 1
40-69 1 Previous LGIB
≥ 70 2 admission
Gender No 0
Female 0 Yes 1
Male 1 DRE findings
Previous LGIB No blood 0
admission Blood 1
No 0 Heart Rate
Yes 1 ≤ 70 0
DRE findings 70-89 1
No blood 0 90-109 2
Blood 1 ≥ 110 3
Heart Rate Systolic blood
≤ 70 0 pressure
70-89 1 < 90 5
90-109 2 90-119 4
≥ 110 3 120-129 3
Systolic blood 130-159 2
pressure ≥ 160 0
< 90 5 Hemoglobin
90-119 4 < 70 22
120-129 3 70-89 17
130-159 2 90-109 13
≥ 160 0 110-129 8
Hemoglobin 130-159 4
< 70 22 ≥ 170 0
70-89 17 Patients scoring ≤ 8, with no other indications for
90-109 13 hospital admission are suitable for immediate
110-129 8 discharge from Accident and Emergency and
130-159 4 outpatient investigation. DRE, digital rectal
≥ 170 0 examination: LGIB, lower gastrointestinal bleeding.
Patients scoring ≤ 8, with no other indications for
hospital admission are suitable for immediate DRE – Digital Rectal Exam
discharge from Accident and Emergency and Kapag lower ang risk ng patient, the Dr may perform
outpatient investigation. DRE, digital rectal further assessment like colonoscopy
examination: LGIB, lower gastrointestinal bleeding.
FORREST CLASSIFICATION OF BLEEDING PEPTIC
LGIB scoring systems: ULCERS
e.g., the Oakland score.
This externally validated risk score based on
o Age
o Sex
o Prior admissions for LGIB
o Vital signs
o DRE findings
o Hemoglobin at admission
It can help identify patients at low risk of poor
outcomes who can be safely managed as
outpatients.
Variables comprising the Oakland score
Predictor Score component value
Ia – spurting arterial haemorrhage, damaged bleeding: of blood from
integrity of mucosal lining maroon, the upper GI
Ib – mas malakas ang bleeding episode jelly-like tract may also
IIa – may visible vessel na if exposed to higher traces of result in
blood in hematochezia
insult, pwedeng matuklap ang outermost layer ng
stools
blood vessel that may cause spurting arterial or
- Rectal
active oozing haemorrhage bleeding:
IIb – Ulcer with an adherent clot, shows that streaks of
nagkaroon ng recent PUD fresh blood
IIc – Flat ulcer with a dark base (covered with on stools
hematin) (hematin – greenish yellow covering on Both melena and hematochezia can be caused by
top of ulcer) either UGIB or LGIB.
III – flat ulcer base (no active haemorrhage) Unexplained iron deficiency anemia (in men or
postmenopausal women) should raise suspicion for
COLONOSCOPY GI bleeding.
Inpatient treatment is recommended if there are
UPPER GI BLEEDING
features requiring intervention or associated with
rebleeding Bright red or coffee ground vomitus (hematesis)
Melena
UPPER ENDOSCOPY Decreased BP
The Forrest classification is commonly used to Increased HR
determine the need for hemostatic interventions Weak peripheral pulses
during the procedure and can help guide disposition Acute confusion (in older adults)
by predicting the risk of rebleeding Vertigo
Dizziness or light-headedness
GASTROINTESTINAL BLEEDING MANIFESTATIONS Syncope (loss of consciousness)
Anemia due to chronic blood loss Decreased haemoglobin and hematocrit
o Acute haemorrhage with significant blood loss
Signs of circulatory insufficiency or hypovolemic GI BLEEDING MANIFESTATION
shock Cannot be generalized kasi pwedeng ,magresult
o Tachycardia, hypotension (dizziness, collapse, from different area yung bleeding sa lower GI.
shock) LOWER GI BLEEDING
o Altered mental status IBD
Features of overt GI bleeding
Young patients may not present with abdominal
Description Cause pain, rectal bleeding, diarrhea, and mucus
Hematemesis Vomiting blood, Most commonly discharge.
may be red or due to bleeding ANGIODYSPLASTIC LESIONS
coffee-ground in in the upper GI Elderly patients with atherosclerotic heart
appearance tract disease may not present with intermittent LGIB
(esophagus, and syncope.
stomach)
Blood vessels in the colon become tortuous.
Melena Black tarry Most commonly
ISCHEMIC COLITIS
stool, with due to bleeding
strong offensive in the upper GI Elderly patients presenting with abdominal pain,
odor tract rectal bleeding and diarrhea.
PERIANAL PATHOLOGY (such as anal fissure or
Can also occur hemorrhoidal bleeding)
in bleeding from Stools are streaked with blood.
the small bowel Patients has perinatal pain and
or the right (+) blood drops on the toilet paper or in the toilet
colon
bowl.
Hematochezia The passage of Most commonly
MASSIVE LGBI
bright red due to bleeding
(fresh) blood in the lower GI A life-threatening condition in which patient
through the tract (distal present with:
anus (with or colon) A SBP below 90 mm Hg and
without stool) A Hgb level of 6 g/dl or less
- Colonic Rapid passage Patient manifest signs of hypovolemic shock
Affected patients are usually: palpitation ischemia
o 65 years and older Rectal exam Bloody or Check the anal
o w/ multiple medical problems &, melanotic stool fissure,
o are at risk of death from acute hemorrhoids,
masses and
hemorrhage or its complications.
gross blood on
The passage of maroon stool or bright red blood stool exam
from the rectum is usually indicative of massive
lower GI hemorrhage. CHARACTERISTIC OF BLOOD
BRIGTH RED
PRESENTATION OF LGIB DEPENDING ON
Vomited from high in esophagus (hematemesis):
ETIOLOGY
from rectum or distal colon (coating stool).
INFECTIOUS OR NONINFECTIOUS (IDIOPATHIC)
COLITIS Hematochezia
o Left -sided bleeding of the colon
A young patient may present with fever,
dehydration, abdominal cramps, and o If the bleeding is brisk and massive – it
hematochezia. maybe evident also in patients with
Common sa mga infectious conditions leading to UGIB and those with right-sided colonic
colitis ay mga inflammatory bowel diseases. bleeding.
MIXED WITH DARK RED
Noninfectious have unknown cause.
Signs and symptoms are secondary to Higher up in colon and small intestine: mixed
excessive blood or stool excreted. with stool.
DIVERTICULAR BLEEDING OR ANGIODYSPLASIA o Right-sided bleeding of the colon
SHADES OF BLACK (COFFEE GROUND)
Older patient may have minimal symptoms and
present with painless bleeding and Esophagus, stomach, & duodenum; vomitus
o Mild and intermittent LGIB (if due to from these areas
angiodysplasia) It represents that there is digestion of blood from
o Moderate or severe LGBI (if due to GI tract.
TARRY STOOL (MELENA)
diverticula-related bleeding)
IMPORTANT EXAM FINDING Occurs in patients who accumulates excessive
blood in the stomach.
Physical exam Exam Finding Significance o Maybe present with cecal bleeding
component NO distinct method exists for determining the anatomic
Resting HR >90/min Loss of <15% source of bleeding based solely on stool color.
tachycardia total blood Stool color is not a confirmatory test that there is GI
volume bleeding. Therefore, still assess the patient because
Orthostatic Decrease in Loss of >15% signs and symptoms vary.
hypotension SBP ≥20 mm total blood
Hg or DPB ≥10 volume
mm Hg from
supine to
standing
position
Supine Supine BP ≤ Loss of ≥40%
hypotension 80/60 mm Hg total blood
volume
Abdominal Rebound Peritoneal signs
exam involuntary may indicate
guarding, perforated
extreme pain to viscus or bowel
ESOPHAGUS hemorrhoids, infectious diarrhea, inflammatory
Bright red blood via vomitus and hematochezia in bowel disease, polyps, tumors, ulcers, Mallory-
stool if there is heavy bleeding. Weiss tears.
Coffee ground vomitus and the stool is melena These conditions are the possible etiology or risk
and positive fecal occult blood if light bleeding. factor for the development or manifestation that
STOMACH leads to GI bleeding.
Blood clots and mixture of bright and dark red
blood vomitus, hematochezia may occur in stool GI BLEEDING DIAGNOSTIC/LABORATORY TEST
for heavy bleeding.
The same with esophagus for light bleeding. BLOOD TEST – to detect whether you have anemia or
DUODENUM bleeding disorders
More blood clots in the vomitus bright to dark red, COMPLETE BLOOD COUNT – low Hgb
stool is a mixture of dark red and black blood for indicates anemia; Thrombocytopenia can cause
heavy bleeding. GI bleeding
The same with esophagus for light bleeding. o To check if mababa na ang
COLON hemoglobin and platelet count.
No vomitus, stool fluctuate from bright red to dark Normal response of our body kapag
red for heavy bleeding. may bleeding, may platelet
No vomitus, on stool exam there are blood clots, aggregation so there is an increased
positive fecal occult blood for light bleeding. likelihood na bumaba ang platelet
SIGMOID count.
No vomitus, bright red blood in the stool for heavy COAGULATION STUDIES – a series of serum
bleeding. tests that evaluate for abnormal blood clotting
No vomitus, on stool exam there are blood clots, o Specifically for patients having GI
positive fecal occult blood for light bleeding. bleeding caused by coagulopathy
RECTUM BLOOD TYPE AND CROSSMATCHING –
No vomitus, bright red blood in the stool for heavy should be obtained promptly in patients with
bleeding. ongoing GI bleeding and/or hemodynamic
No vomitus, on stool exam there are streaks on instability at presentation
stool, positive fecal occult blood for light o In preparation for having blood
bleeding. transfusion, lalo na kapag may
Gastrointestinal bleeding Clinical features of massive bleeding
gastrointestinal (GI) bleeding, including hematemesis, BUN LEVEL – extensive bleeding into the
melena, and hematochezia, vary depending on source gastrointestinal (GI) tract will also cause an
and volume bleeding. elevated BUN because digested blood is a
GI BLEEDING DIAGNOSTIC/LABORATORY TESTS source of urea.
It is not difficult to diagnose bleeding, but it may o Tumataas ang BUN kasi nada-digest
be difficult to locate the source of bleeding. ng stomach yung blood accumulating
It is easier to address the situation if the bleeding in the GI tract.
location or root cause is known, and this is a LIVER FUNCTION TESTS (LIVER
challenge to the health practitioner to identify CHEMISTRIES) – a group of laboratory test that
where the bleeding is. serve as parameters of hepatocellular damage,
HISTORY cholestasis, and hepatic synthesis.
Change in bowel pattern, presence of pain or o Liver is also functioning in
tenderness, recent intake of food and what kind, manufacturing the clotting factors
alcohol consumption, such as aspirin or steroids. o Impairment of the liver leads to
Focus assessment ang ginagawa for emergency further bleeding episodes.
na dinudugo ang patient kapag dumating sa
- Anemia, low hematocrit, coagulopathy, and
hospital to prevent the patient from suffering sa
elevated BUN at presentation are signs of GI
hypovolemic shock
bleeding
STOOL EXAM
- An elevated BUN to creatinine ratio in a
To detect occult bleeding patient with hematochezia suggests a brisk
Occult blood: diverticular disease, esophagitis, UGIB
gastritis, esophageal varices, anal fissure,
o Normally if there is an elevation of - Consider intubation prior to endoscopy if
metabolic waste, creatinine is being there is a high risk of aspiration
observed in relation with renal o It is important to subject the patient in an
functioning. endotracheal intubation to create
o But in this condition, ang tinitingnan ay GI tamponade and prevent regurgitation and
bleeding na cause ng digestion ng RBC aspiration since ET tube balloon will be
and na ang by product ay urea, hindi inflated.
creatinine, kaya BUN ang tataas.
Colonoscopy (assess the lower GI tract)
o Source of GI bleeding identified:
NASOGASTRIC ASPIRATES (NG ASPIRATE) – this test Attempt endoscopic hemostasis.
is not routinely recommended other than as adjunct in Through an endoscope mag-create ng
patients with hematochezia with only moderate probability stasis para mahinto yung bleeding.
of UGIB as the source o Negative (nondiagnostic) colonoscopy
It is not routinely recommended because it will further Hemodynamically stable patients:
create trauma in the lining of the mucus membrane Evaluate for small bowel bleeding
further bleeding episode. Mas preferred ang EGD Hemodynamically unstable patients
Procedure: Instill 200-300 mL of warm with ongoing bleeding: Consult
isotonic saline via NG tube, then aspirate surgery or angioembolization
gastric contents for inspection - Lower endoscopy without bowel preparation
Findings: (including sigmoidoscopy) is not
o Positive: Bright red blood or coffee- recommended in the workup of acute LGIB.
grounds output; active UGIB confirmed
o Inconclusive: Non-bloody and non- VIDEO CAPSULE ENDOSCOPY (VCE)
bilious
o Negative: Non-bloody and bilious; active A diagnostic procedure using a tiny wireless
UGIB less likely camera fitted inside a capsule that is swallowed
- In patients with suspected UGIB, nasogastric by the patient to take pictures of the mucosa in
aspiration is poorly sensitive as ~15% of the GI tract
patients with active UGIB can have a false Pictures are analyzed after the capsule is
negative excreted 24-48 hours later.
- VCE is preferred in hemodynamically stable
ENDOSCOPY – to detect and see if and where you have patients with negative EGD and colonoscopy.
GI bleeding and the cause of the bleeding Hemodynamically unstable patients with
Cannot be performed kapag may massive bleeding ang suspected small bowel bleeding should
patient, it should be addressed first by giving undergo angiography.
vasoconstrictors, fluid resuscitation or blood transfusion to
stabilize the hemodynamic status before performing any IMAGING TESTS – may detect etiology of bleeding
diagnostic procedure. Angiogram – to help visualize abnormalities blood
EGD (assess the upper GI tract) vessels supplying the GI tract
o Source of GI bleeding identified (positive Computed Tomography Angiography (CTA)
EGD): Attempt endoscopic hemostasis. o A diagnostic imaging technique that uses
o Source of GI bleeding not identified computerized tomography, intravenous
(negative or nondiagnostic EGD) administration of a radiocontrast agent
Hemodynamically stable patients and specific timing to visualize blood
with hematochezia or melena: vessels of interest
Perform colonoscopy (if not performed o Also used to localize the source of GI
as the first-line intervention); consider bleed
evaluation for small bowel bleeding o Can detect bleeds as slow as 0.3-
Hemodynamically unstable patients 0.5mL/minute
with ongoing bleeding: Consider After ma-inject and contrast
angioembolization medium, magkakaroon ng series
Angioembolization – nagiinject ng pang- of images para makita ang status
block or emboli to stop the bleeding sa ng blood vessels.
vessels.
Abdominal CT Scan – help detect gastric or o Oliguria suggests that there is a
duodenal ulcers or lesions that may cause or decreased perfusion
predisposes the client to develop GI bleeding Central Venous Pressure (CVP) may need to be
inserted
o Also called Right Atrial Pressure usually
measures 0-8mmHg
o Blood is received by the IVC/SVC and it
will be drained at the right atrium. The
MEDICAL-SURGICAL MANAGEMENT FOR PATIENTS CVP catheter ay iniisert sa may arms and
WITH GI BLEEDING ithe-thread sa veins. Ang tip ng catheter
Management of GI Bleeding is based on etiology: ay nasa junction ng SVC ang RA para
If aspirin or NSAIDs are the cause ma-measure ang fluid.
discontinue medication and treat bleeding o Kung ang patient ay magma-manifest ng
If ulcer is the cause medication, dietary and 8mmHg and above, it represents that
lifestyle modifications he/she is experiencing overhydration or
Therapeutic endoscopic procedure (cautery, fluid overload.
injection) o CVP/RAP represents the hydration status
o Yung blood vessel na nagkakaroon ng of the patient. If 0 or negative ang CVP
oozing of blood, that is the one being measurement, it is an indication na
cauterized or injected ng schelorsal agent hypovolemic or decreased venous return.
Surgery may be indicated for cancers, Conduct a focused history and examination
inflammatory diseases and vascular disorder (including DRE)
Risk stratify to guide further management
The following recommendations are consistent with the Prior to endoscopic hemostatic procedures: (see
2019 International Consensus Group (ICG) Nonvariceal “Empiric Pharmacotherapeutic Interventions for GI
UGIB guidelines, the 2016 American College of bleeding” for details) (PPI, Antibiotic,
Gastroenterology (ACG) LGIB guidelines, the 2014 Vasopressin, Analogs)
American Society for Gastrointestinal Endoscopy (AGSE)
Administer pre-treatment (e.g., IV PPI) as needed
LGIB guidelines
ALL PATIENTS Administer anticoagulant reversal if INR > 2.5
Ensure patient is NPO o Antidote for Heparin: Protamine Sulfate
Early identification of signs and symptoms of o Antidote for Warfarin: Vitamin K
Hypovolemic Shock and monitor vital signs every o Sa mga patient na may bleeding and
15 to 30 minutes nagtake previously ng warfarin and
o We need to assess the history but heparin, kailangan ng antidote para
address first the physiological needs of bumalik sa normal functioning ang blood
patient for us to know if may signs clotting mechanism since na-alter noong
indicating hypovolemic shock may anticoagulant therapy.
Insert two large-bore (a 16- or 18-gauge needle) o Kailangan i-reverse kasi patients are high
peripheral IV lines for: risk of massive bleeding.
o Fluid resuscitation (Isotonic) – e.g., Consider withholding antithrombotic agents
Lactated Ringers, and
Isotonic to lessen the chances of NURSING MANAGEMENT
fluid shifting
Plain LR – para mayroong fluid & NURSING ASSESSMENT
electrolytes
o Assessment for a description of pain
o Blood Transfusion (fresh whole blood,
o Assessment of relief measures to relieve the pain.
packed RBC, and fresh frozen plasma)
o Assessment of the characteristics of the vomitus.
Obtain blood samples for laboratory studies (e.g., o Assessment of the patient’s usual food intake and
CBC, ABO typing and screening)
food habits
Administer supplemental 02 delivered by
facemask or nasal cannula NURSING DIAGNOSIS
Insert an indwelling catheter – monitor UO hourly o Acute pain related to the effect of gastric acid
o Urine output is an important indicator of secretion on damaged tissue.
fluid volume status of patient o Anxiety related to an acute illness.
o Imbalanced nutrition related to changes in the diet. stool for occult or gross blood; monitor
o Deficient knowledge about prevention of symptoms vital signs frequently (tachycardia,
and management of condition hypotension, and tachypnea).
Insert an indwelling urinary catheter and
monitor intake and output; insert and
NURSING CARE PLANNING & GOALS maintain an IV line for infusing fluid and
o The goals for the patient may include: blood.
o Relief of pain Replenish fluid losses, urine will signify
o Reduced anxiety the concentration and fluid status.
o Maintenance of nutritional requirements Monitor laboratory values (hemoglobin
o Knowledge about the management and and hematocrit).
Insert and maintain a nasogastric tube
prevention of ulcer recurrence
and monitor drainage; provide lavage as
o Absence of complications
ordered.
Kailangan right pathway kung saan
NURSING INTERVENTIONS lalabas ang drainage since post-op.
o Nursing interventions for the patient may include: Lavage = washing; intake=output,
o Relieving Pain and Improving Nutrition aspirate by gravity.
The only way to stop lavage if ordered
Administer prescribed medications.
by a doctor, kapag yung output is clear,
Medications to relieve the pain as well as
no blood tinge or coffee ground.
to manage the cause of ulcer formation
Monitor oxygen saturation and
Avoid aspirin, which is an anticoagulant,
administering oxygen therapy.
and foods and beverages that contain
Place the patient in the recumbent
acid-enhancing caffeine (colas, tea,
position with the legs elevated to prevent
coffee, chocolate), along with
hypotension or place the patient on the
decaffeinated coffee.
left side to prevent aspiration from
Encourage patient to eat regularly
vomiting.
spaced meals in a relaxed atmosphere.
Treat hypovolemic shock as indicated.
Obtain regular weights and
encourage dietary modifications.
o Monitoring and Managing Complications: If
Encourage relaxation techniques.
penetration are concerns.
o Reducing Anxiety Note and report symptoms of penetration
(back and epigastric pain not relieved by
Assess what patient wants to know about
medications that were effective in the
the disease and evaluate level of anxiety;
past).
encourage patient to express fears
Penetration= nag through and through to
openly without criticism.
another organ and system. Ex: pancreas
Explain diagnostic tests and
Note and report symptoms of perforation
administering medications on schedule.
(sudden abdominal pain, referred pain to
If PPI, or trying to eradicate the H. Pylori
shoulders, vomiting and collapse,
or antacids which should be take at least
extremely tender and rigid abdomen,
30 mins before meals
hypotension and tachycardia, or other
To reduce anxiety and explain in a level
signs of shock).
that they understand.
Perforation is napunit. Example may
Interact in a relaxing manner, help in
gastric cancer so napunit tumagos yung
identifying stressors, and explain
laman sa peritonium and surrounding
effective coping techniques and
areas
relaxation methods.
Encourage family to participate in care
and give emotional support. MANAGEMENT FOR PATEINTS WITH GI BLEEDING
Nasogastric lavage
o Monitoring and Managing Complications: If o Its use before endoscopy in the ER remains
hemorrhage is a concern: controversial.
Assess for faintness or dizziness and o Lavage is stomach wash
nausea, before or with bleeding; test Benefits:
o To confirm an UGI source of bleeding (can Lower Gi tract, nireremove
still miss up to 15%) yung polyps na possible
o Prognostic index for identifying high-risk nagcacause ng bleeding,
lesions as presence of fresh red blood in the
NGT aspirate. Interventional Radiology (Angiography)
o Presence of blood will confirm na Acute bleeding tapos di possible yung
may bleeding. endoscopic procedure kasi unstable yung
o May exclude false hematemesis. patient.
o Respiratory tract sputum -> linunok o Indications:
yung dugo Preferred therapy in patients with
o To facilitate lavage of the upper GI tract to ongoing GI bleeding and
improve mucosal views at subsequent hemodynamic instability refractory to
endoscopy. resuscitation.
o If cause of bleeding is esophageal An alternative to colonoscopy in
varices, insertion of NGT may patients with acute LGIB who cannot
traumatizes and increase bleeding tolerate bowel preparation.
tendencies. Consider in patients with rebleeding or
o Reason to stop: if the return flow is ongoing bleeding despite endoscopic
clear. hemostasis.
o Techniques:
Approach to Overt GI bleeding
o Emergency resuscitation Angioembolization
A minimally invasive
o Choice of source control modality depends
procedure used to selectively
on multiple factors (e.g., suspected
occlude the arterial supply of
hemorrhage source, hemodynamic status,
target tissue.
available resources)
Primarily used to achieve
Endoscopy is indicated, feasible, and
hemostasis non-operatively
able to identify the source of
but can also be used as an
bleeding: Attempt endoscopic
adjunct to surgical
hemostasis.
hemostasis.
Endoscopy not recommended or
Pinasok na pang
unable to identify the source of
emboli is a coil or gel
bleeding: angioembolization of
foam para mag stop
surgery.
yung bleeding.
o Identify and treat the underlying cause.
Intraarterial vasopressin
Approach to Occult GI bleeding Vasopressin (Arginine
o Identify and treat underlying cause; correct vasopressin) (medication): a
anemia. synthetic ADH analog
Used to treat vasodilatory
Endoscopic Hemostasis shock, esophageal variceal
o Indications: any high-risk endoscopic findings hemorrhage, and control
Signs of active bleeding diabetes insipidus.
Nonbleeding visible vessel Directly inject ng
Adherent clot embolization particles
o Modalities May cause emboli to
Injection therapy (e.g., with diluted other area na
epinephrine, normal saline) madedeliver.
Cauterization (e.g., heater probes, Suspected LGIB
electrocauterization) o Stable patients: Refer for colonoscopy
Sinusunog yung blood vessels o Perform EGD: done first for unstable patients
na nag open-up/ oozing blood with hematochezia and to any of the following:
Mechanical therapy (e.g., band High probability of UGIB
ligation, clips) Moderate probability of UGIB with
Polypectomy in the case of bleeding positive or inconclusive NG aspirate
polyp (e.g., in the colon)
o Consider colonoscopy: first for unstable o Platelet count
patients with hematochezia and to all of the o Coagulation studies
following: o Test for occult blood if indicated
Moderate probability of UGIB and
negative NG aspirate NURSING DIAGNOSES
Able to tolerate rapid bowel prep. o Deficient Fluid Volume related to blood loss
o Consider angiography: for patients with o Imbalanced Nutrition: Less Than Body Requirements
refractory hemodynamic instability. related to nausea, vomiting and diarrhea
o Consider surgery: if other options have failed
NURSING INTERVENTIONS (ACTIVE BLEEDING)
o Monitor VS closely
o During the active bleeding, every 15-30 minutes
o Assess for signs of:
o Dehydration
LOWER GI BLEED TREATMENT Fluid losses
Management of Lower GIB is focused on colonoscopy o Hypovolemic shock
and mechanically treating bleeds with little Blood loss
pharmacological intervention o Sepsis
o Look for the source & location of bleeding o Respiratory insufficiency
o Wala masyadong tulong ang pharmacological Once hypovolemic shock occurs, the fluid
interventions when it comes to lower GI bleeding volume is decreased; the lungs would try to
After the initial assessment and risk stratification, and compensate which results to rapid breathing
once the patient is hemodynamically stable: o Maintain NPO status and administer IV fluid
o Colonoscopy preceded by colon cleansing is the replacements as prescribed
initial diagnostic procedure for most patient o Lactated ringers, Plain LR (isotonic solution)
presenting with a LGIB o To minimize chances of fluid shifting
Management of LGIB mostly includes non- o Insert another line for possible blood transfusion
pharmacologic interventions o Monitor intake & output
PPI Application in LGIB o Foley catheter needs to be inserted
o Evidence suggests that patients with LGIB do not o Urine output reflects the fluid volume status of
benefit from PPI therapy the patient
o Monitor the urine output per hour
o Monitor hemoglobin and hematocrit
NURSING ASSESSMENT o Continuous bleeding = hemoglobin and
o Change in bowel patterns or hemorrhoids hematocrit will decrease in value
o Change in color of stools o Administer blood transfusions as prescribed
o Dark black o Determine if the patient needs fresh raw blood,
o Red RBC, platelet concentrate, or fresh frozen
o Streaked with blood plasma
o Alcohol consumption o Prepare to assist with administering medications as
o Medications such as: prescribed to induce vasoconstriction and reduce
o NSAIDs bleeding
o Antibiotics o Examples: Epinephrine, Vasopressin
o Anti-coagulants
o Attaining Normal Fluid Volume
o Corticosteroids
o Maintain NG tube and NPO status
o Hematemesis
NGT will be inserted and connected to a
o Other medical conditions
drainage bottle, to allow for gastric
o Examples: Liver cirrhosis, Cancer, etc.
decompression; to drain secretion
o Evaluate for presence of abdominal pain or
To allow the GI tract to rest
tenderness
To evaluate bleeding
o Monitor VS
o Monitor intake & output as ordered
o Monitor laboratory tests that indicated bleeding:
To evaluate fluid status
o Hemoglobin
Determining the patient’s output allows you
o Hematocrit
to know how much to replenish in terms of
fluids & electrolytes since the patient is at
risk for dehydration and electrolyte
imbalances
Volume per volume replacement; Lactated
Ringer solution
o Monitor VS as ordered
Every 15 to 30 minutes
o Observe for changes indicating shock, such as:
Tachycardia
Hypotension
Increased respirations
Decreased urine output
Change in mental status
o Administer IV fluids and blood products as
ordered to maintain volume
o Attaining Balanced Nutritional Status
o Weigh daily to monitor caloric status
o Administer IV fluids, TPN if ordered
Promotes hydration and nutrition while on
oral restrictions
Examples for TPN: Ready for use glucose,
amino acids, fatty acids, etc. that our body
needs to replace enteral feeding
Usually makes use of the central line
because if you utilize the peripheral line,
there’s a possibility of phlebitis because the
TPN solutions used are highly osmolar &
hypertonic.
IV fluids – crystalloids only
TPN – can really provide nutrition, but are
pricey for the patient
o Begin liquids when patient is no long NPO
o Advance diet as tolerated
Should be high-calorie, high-protein
Frequent, small feedings may be indicated
Offer snacks, high-protein supplements
o Patient Education and Health Maintenance
Discuss the cause and treatment of GI
bleeding with patient
Instruct patient regarding signs and
symptoms of GI bleeding
Melena
Emesis – bright red, or coffee grounds
in color
Rectal bleeding
Weakness
Fatigue
Shortness of breath
Instruct patient on how to test stool or
emesis for occult blood, if applicable
You might also like
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- GI Bleeding - NursesDocument71 pagesGI Bleeding - Nursesapi-3760283100% (6)
- Presentation Liver CirrhosisDocument26 pagesPresentation Liver CirrhosisFaye Dominique Roxas PalmaresNo ratings yet
- GI Assessment Diagnosis and Case StudiesDocument66 pagesGI Assessment Diagnosis and Case StudiesCarla CalsadoNo ratings yet
- Complete Intestinal ObstructionDocument8 pagesComplete Intestinal ObstructionThuganamix100% (2)
- Intestinal ObstructionDocument35 pagesIntestinal Obstructionwht89100% (1)
- Intestinal ObstructionDocument27 pagesIntestinal ObstructionAna AvilaNo ratings yet
- Renal FailureDocument56 pagesRenal FailureKoRnflakes100% (2)
- Urinary Tract InfectionDocument4 pagesUrinary Tract InfectionGerardLum100% (2)
- Congestive Heart Failure ReportDocument6 pagesCongestive Heart Failure ReportSunshine_Bacla_4275100% (1)
- Shock, HypovolemicDocument2 pagesShock, HypovolemicNadya Syafitri100% (2)
- CKD PresentationDocument51 pagesCKD PresentationBasneyatPragyanNo ratings yet
- HyponatremiaDocument26 pagesHyponatremiaflorenciaii100% (1)
- Myocardial Infarction Case Analysis: Symptoms, Causes, Diagnosis (MIDocument76 pagesMyocardial Infarction Case Analysis: Symptoms, Causes, Diagnosis (MIIpeNo ratings yet
- Gastrointestinal DisordersDocument27 pagesGastrointestinal DisordersRI NA100% (5)
- Urolithiasis - Modified LectureDocument35 pagesUrolithiasis - Modified Lecturemarina_shawkyNo ratings yet
- Upper Gi BleedingDocument35 pagesUpper Gi Bleedingnawriirwan100% (1)
- PEDIA 4.1 NephrologyDocument7 pagesPEDIA 4.1 NephrologyAngela CaguitlaNo ratings yet
- AnginaDocument12 pagesAnginaHermiie Joii Galang Maglaquii0% (1)
- Cor Pulmonale: Dr. Gerrard UyDocument13 pagesCor Pulmonale: Dr. Gerrard Uyfaridah azzah sariNo ratings yet
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- PeritonitisDocument11 pagesPeritonitisMihir PatelNo ratings yet
- Approach To HyponatremiaDocument47 pagesApproach To HyponatremiaRajiv MedankiNo ratings yet
- Fluid and Electrolyte ImbalancesDocument35 pagesFluid and Electrolyte Imbalancesmardsz95% (22)
- Pulmonary EmbolismDocument14 pagesPulmonary EmbolismMutaz Dredei100% (5)
- Anemia IntroductionDocument15 pagesAnemia IntroductionNitesh Kotian100% (1)
- Case Study: Congestive Heart FailureDocument7 pagesCase Study: Congestive Heart FailureXI-E / 21 / MARY TRIANANo ratings yet
- CardiomyopathyDocument1 pageCardiomyopathyTrisha VergaraNo ratings yet
- Fluid, Electrolyte, and Acid-BaseDocument6 pagesFluid, Electrolyte, and Acid-BaseRaquel MonsalveNo ratings yet
- Gastrointestinal DisordersDocument9 pagesGastrointestinal DisordersKieran Levi100% (2)
- IV Fluid Replacement TherapyDocument12 pagesIV Fluid Replacement TherapyKamran Sheraz100% (1)
- CellulitisDocument12 pagesCellulitisAlma Bertos-Agub100% (1)
- Pathophysiology Infective EarditisDocument3 pagesPathophysiology Infective EarditisDanielJosephLim50% (2)
- Acute Abdominal Pain Case: AppendicitisDocument70 pagesAcute Abdominal Pain Case: AppendicitisVenny VeronicaNo ratings yet
- Pancreatitis: Pancreatitis Is Inflammation in The Pancreas. TheDocument27 pagesPancreatitis: Pancreatitis Is Inflammation in The Pancreas. ThenikkimaxinevaldezNo ratings yet
- Bowel ObstructionDocument25 pagesBowel Obstructionc0dy143100% (2)
- Hiatal HerniaDocument10 pagesHiatal HerniaZennon Blaze ArceusNo ratings yet
- Left Sided & Right Sided Heart FailureDocument29 pagesLeft Sided & Right Sided Heart FailureRachelle Ayn100% (3)
- Schistosomiasis Case StudyDocument5 pagesSchistosomiasis Case Studyapi-318749549No ratings yet
- Gastrointestinal Disorders GuideDocument14 pagesGastrointestinal Disorders GuideAnna Sofia Reyes100% (1)
- Ascites PresentationDocument19 pagesAscites PresentationDanielle FosterNo ratings yet
- Non-Variceal Upper GI Bleeding GuideDocument34 pagesNon-Variceal Upper GI Bleeding GuideChe Ainil ZainodinNo ratings yet
- DiarrheaDocument13 pagesDiarrheamarla danaoNo ratings yet
- Endocrine Disorders (Study Notes)Document11 pagesEndocrine Disorders (Study Notes)Danelle Harrison, RN90% (10)
- Thyroid CaseDocument53 pagesThyroid CaseKenisha HutsonNo ratings yet
- Intestinal Obstruction 4Document25 pagesIntestinal Obstruction 4Muvenn KannanNo ratings yet
- Chronic Renal FailureDocument46 pagesChronic Renal Failurestepharry08100% (1)
- Upper Gastrointestinal Bleeding.Document13 pagesUpper Gastrointestinal Bleeding.Gieselle Scott100% (1)
- Upper Gastrointestinal BleedingDocument3 pagesUpper Gastrointestinal Bleedingplayaz_dan2100% (1)
- Upper Gastrointestinal Bleeding (Ugib) : First Shift: August 13, 2018Document10 pagesUpper Gastrointestinal Bleeding (Ugib) : First Shift: August 13, 2018Angelo Dela Cruz VillaromanNo ratings yet
- Acute Renal Failure: Dr. Bobi Ahmad S, S.KPDocument62 pagesAcute Renal Failure: Dr. Bobi Ahmad S, S.KPdr.Bobi Ahmad Sahid, S.KepNo ratings yet
- Acute Gastrointestinal Bleeding GuideDocument47 pagesAcute Gastrointestinal Bleeding GuideJohn Clements Galiza100% (1)
- CKD Symptoms and TreatmentsDocument3 pagesCKD Symptoms and TreatmentsrhizzyNo ratings yet
- N196 GI Exam Study GuideDocument7 pagesN196 GI Exam Study Guideaznknight3230% (1)
- Acute GlumerulonephritisDocument77 pagesAcute GlumerulonephritisNicoleNo ratings yet
- Perdarahan Saluran Cerna CDocument18 pagesPerdarahan Saluran Cerna CCory PrimaturiaNo ratings yet
- MANAGING ACUTE GI BLEEDINGDocument35 pagesMANAGING ACUTE GI BLEEDINGharsani auroraNo ratings yet
- Acute Gi Bleeding: Rohman AzzamDocument34 pagesAcute Gi Bleeding: Rohman AzzamgebyarayuNo ratings yet
- Acute GI BleedingDocument35 pagesAcute GI BleedingGalih GimastiarNo ratings yet
- What Are The Signs of Bleeding in The Digestive Tract?Document6 pagesWhat Are The Signs of Bleeding in The Digestive Tract?draganNo ratings yet
- NCP FinalDocument19 pagesNCP FinalAnna Sofia ReyesNo ratings yet
- Somatoform DisorderDocument18 pagesSomatoform DisorderAnna Sofia ReyesNo ratings yet
- Maladaptive Patterns of Behavior A. AnxietyDocument19 pagesMaladaptive Patterns of Behavior A. AnxietyTeal OtterNo ratings yet
- 1 Colostomy and IleostomyDocument4 pages1 Colostomy and IleostomyAnna Sofia ReyesNo ratings yet
- Gastrointestinal Disorders GuideDocument14 pagesGastrointestinal Disorders GuideAnna Sofia Reyes100% (1)
- Hypothesis: Prepared By: Ma. Teresa A. Monderin, Rn-ManDocument29 pagesHypothesis: Prepared By: Ma. Teresa A. Monderin, Rn-ManAnna Sofia ReyesNo ratings yet
- Msnlec 0425 5thpart Obs&HemorrhoidsDocument2 pagesMsnlec 0425 5thpart Obs&HemorrhoidsAnna Sofia ReyesNo ratings yet
- 1 Colostomy and IleostomyDocument4 pages1 Colostomy and IleostomyAnna Sofia ReyesNo ratings yet
- Ethics in Research 2021Document52 pagesEthics in Research 2021Anna Sofia ReyesNo ratings yet
- MSN 0419 4thpart AppendicitisPeritonitisDocument3 pagesMSN 0419 4thpart AppendicitisPeritonitisAnna Sofia ReyesNo ratings yet
- Discovering Research (2021)Document52 pagesDiscovering Research (2021)Anna Sofia ReyesNo ratings yet
- Carbohydrates IntroDocument2 pagesCarbohydrates IntroCamille Ann Faigao FamisanNo ratings yet
- Variable: Prepared By: Ma. Teresa A. Monderin, Rn-ManDocument20 pagesVariable: Prepared By: Ma. Teresa A. Monderin, Rn-ManAnna Sofia ReyesNo ratings yet
- Variable: Prepared By: Ma. Teresa A. Monderin, Rn-ManDocument20 pagesVariable: Prepared By: Ma. Teresa A. Monderin, Rn-ManAnna Sofia ReyesNo ratings yet
- Research Problems 2021Document42 pagesResearch Problems 2021Anna Sofia ReyesNo ratings yet
- Hypothesis: Prepared By: Ma. Teresa A. Monderin, Rn-ManDocument29 pagesHypothesis: Prepared By: Ma. Teresa A. Monderin, Rn-ManAnna Sofia ReyesNo ratings yet
- Research Problems 2021Document42 pagesResearch Problems 2021Anna Sofia ReyesNo ratings yet
- Reporter#1: Karla Mae Monacillo (20) BiomoleculesDocument5 pagesReporter#1: Karla Mae Monacillo (20) BiomoleculesAnna Sofia ReyesNo ratings yet
- Oxaloacetate (4C) SynthaseDocument104 pagesOxaloacetate (4C) SynthaseAnna Sofia ReyesNo ratings yet
- Discovering Research (2021)Document52 pagesDiscovering Research (2021)Anna Sofia ReyesNo ratings yet
- Biomolecules and Carbohydrates IntroDocument5 pagesBiomolecules and Carbohydrates IntroCamille Ann Faigao FamisanNo ratings yet
- Formation of HemiacetalsDocument6 pagesFormation of HemiacetalsAnna Sofia ReyesNo ratings yet
- Introduction to Anabolic Metabolism and Lipid SynthesisDocument21 pagesIntroduction to Anabolic Metabolism and Lipid SynthesisAnna Sofia ReyesNo ratings yet
- Ethics in Research 2021Document52 pagesEthics in Research 2021Anna Sofia ReyesNo ratings yet
- Carbohydrates - DisaccharidesDocument3 pagesCarbohydrates - DisaccharidesCamille Ann Faigao FamisanNo ratings yet
- Carbohydrates IntroDocument2 pagesCarbohydrates IntroCamille Ann Faigao FamisanNo ratings yet
- CarbsDocument3 pagesCarbsAnna Sofia ReyesNo ratings yet
- Maladaptive Patterns of Behavior A. AnxietyDocument19 pagesMaladaptive Patterns of Behavior A. AnxietyTeal OtterNo ratings yet
- Carbohydrates - DisaccharidesDocument3 pagesCarbohydrates - DisaccharidesCamille Ann Faigao FamisanNo ratings yet
- TR019999012181 enDocument37 pagesTR019999012181 enAliTronic1972No ratings yet
- L1 Finding Nemo Teacher Notes American EnglishDocument9 pagesL1 Finding Nemo Teacher Notes American Englishcris_simescuNo ratings yet
- Cancer EssayDocument4 pagesCancer EssayCamille Joy BaliliNo ratings yet
- IR Spectroscopy Identification GuideDocument28 pagesIR Spectroscopy Identification GuideAby JatNo ratings yet
- 1,16Document138 pages1,16niztgirlNo ratings yet
- JAOP Progress ReportDocument36 pagesJAOP Progress ReportnidhisasidharanNo ratings yet
- CHUYÊN ĐỀ 8 - VIẾT LẠI CÂU BẰNG TỪ NỐIDocument27 pagesCHUYÊN ĐỀ 8 - VIẾT LẠI CÂU BẰNG TỪ NỐICà ChuaNo ratings yet
- UL Anatomy 2022Document4 pagesUL Anatomy 2022jhom smithNo ratings yet
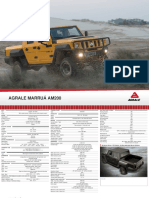
- Off Road and Military Vehicles Off Road Vehicles Agrale Marruaam200 1Document2 pagesOff Road and Military Vehicles Off Road Vehicles Agrale Marruaam200 1Victor SilvaNo ratings yet
- Viscous Fluid Flow Ch1-Preliminary Concepts: Kfupm ME 532-172Document40 pagesViscous Fluid Flow Ch1-Preliminary Concepts: Kfupm ME 532-172Majid KhanNo ratings yet
- Audi SSP 822703 4 2 L v8 Fsi Engine VolkswagenDocument4 pagesAudi SSP 822703 4 2 L v8 Fsi Engine Volkswagenmiriam100% (34)
- NIA045462022 KL 13 AR 1130 Royal Enfield Motors LTD Classic X 350 ESDocument10 pagesNIA045462022 KL 13 AR 1130 Royal Enfield Motors LTD Classic X 350 ESAkhil DasNo ratings yet
- Cast Steel y Strainer Ansi Class 150Document2 pagesCast Steel y Strainer Ansi Class 150aurinkokelloNo ratings yet
- Computer Education ModuleDocument22 pagesComputer Education ModuleJulia Melissa CzapNo ratings yet
- MAGA Training ReportDocument56 pagesMAGA Training ReportChaturanga WagaArachchige67% (3)
- PHYS205 Matlab Lab TasksDocument4 pagesPHYS205 Matlab Lab TasksjacobNo ratings yet
- Ipra IrrDocument58 pagesIpra IrrMac Manuel100% (1)
- 2.seismic Coefficient CalculationDocument14 pages2.seismic Coefficient CalculationVenkat PalliNo ratings yet
- Frequency-Domain Analysis of Discrete-Time Signals and SystemsDocument31 pagesFrequency-Domain Analysis of Discrete-Time Signals and SystemsSwatiSharmaNo ratings yet
- Ymfc Al SetupDocument18 pagesYmfc Al SetupredaNo ratings yet
- MarlinDocument28 pagesMarlincumpio425428No ratings yet
- Syngo - Via: HW Data SheetDocument4 pagesSyngo - Via: HW Data SheetCeoĐứcTrườngNo ratings yet
- Math Story FlowersDocument3 pagesMath Story Flowerstoxic_angel_love958No ratings yet
- Presidential Decree No. 1616 establishes Intramuros AdministrationDocument22 pagesPresidential Decree No. 1616 establishes Intramuros AdministrationRemiel Joseph Garniel BataoNo ratings yet
- YZF-R15: Parts & AccessoriesDocument55 pagesYZF-R15: Parts & AccessoriesSiam HussainNo ratings yet
- 016 Muscoril COPPDocument3 pages016 Muscoril COPPTheRoom23No ratings yet
- B757-200 MPDDocument393 pagesB757-200 MPDSebastian Rendon100% (3)
- Pacemaker 180508042454Document86 pagesPacemaker 180508042454padmaNo ratings yet
- DIESEL PARTS OF AMERICA DPA-240 USER'S MANUALDocument54 pagesDIESEL PARTS OF AMERICA DPA-240 USER'S MANUALEdinson Ariel Chavarro QuinteroNo ratings yet
- Pol Science ProjectDocument18 pagesPol Science ProjectAnshu SharmaNo ratings yet