Professional Documents
Culture Documents
NP Outreach Curriculum in Rheumatology St. Joseph's Health Care, London, ON Dr. Sherry Rohekar November 12, 2009
NP Outreach Curriculum in Rheumatology St. Joseph's Health Care, London, ON Dr. Sherry Rohekar November 12, 2009
Uploaded by
kinanthi asmara0 ratings0% found this document useful (0 votes)
6 views50 pagesOriginal Title
LBP.ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views50 pagesNP Outreach Curriculum in Rheumatology St. Joseph's Health Care, London, ON Dr. Sherry Rohekar November 12, 2009
NP Outreach Curriculum in Rheumatology St. Joseph's Health Care, London, ON Dr. Sherry Rohekar November 12, 2009
Uploaded by
kinanthi asmaraCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 50
NP Outreach Curriculum in Rheumatology
St. Joseph’s Health Care, London, ON
Dr. Sherry Rohekar
November 12, 2009
An Important Issue
One of the most common reasons for seeking medical
attention, second only to respiratory issues
84% of adults will have low back pain at some point
Wide variety of approaches for treatment
Suggests that optimal approach is unsure
Most episodes are self-limited
Some suffer from chronic or recurrent courses, with
substantial impact on quality of life
Epidemiology
Almost any structure in the back can cause pain,
including ligaments, joints, periosteum, musculature,
blood vessels, annulus fibrosus and nerves
Intervertebral discs and facet joints most commonly
affected
85% of those with isolated low back pain do not have a
clear localization
Usually called “strain” or “sprain” no histopathology, no
anatomical location
Men and women equally affected
Age of onset 30-50 years
Epidemiology
Leading cause of work disability in those < 45 years
Most expensive cause of work disability in terms of
worker’s compensation
Multiple known risk factors:
Heavy lifting, twisting, vibration, obesity, poor
conditioning
Common Pathoanatomical Conditions of the Lumbar Spine
Deyo R and Weinstein J. N Engl J Med 2001;344:363-370
Differential Diagnosis of Low Back Pain
Deyo R and Weinstein J. N Engl J Med 2001;344:363-370
History
Any evidence of systemic disease?
Age (especially >50), hx of cancer, unexplained weight
loss, IVDU, chronic infection
Duration
Presence of nocturnal pain
Response to therapy
Many patients with infection or malignancy will not
have relief when lying down
Note for arthritis patients – young age, nocturnal pain and
worsening with rest are common in AS
History
Any evidence of neurologic compromise?
Cauda equina syndrome is a medical emergency
Usually due to tumor or massive herniation compressing the
nerves of the cauda equina
Urinary retention with overflow, saddle anesthesia, bilateral
sciatica, leg weakness, fecal incontinence
Sciatica caused by nerve root irritation
Sharp/burning pain down posterior or lateral leg to foot or
ankle; can be associated with numbness/tingling
If due to disc herniation often worsens with cough, sneeze or
performing the Valsalva
History
Any evidence of neurologic compromise?
Spinal stenosis is caused by narrowing of the spinal
canal, nerve root canals, or intervertebral foramina
Most commonly due to bony hypertrophic changes in facet
joints and thickening of the ligamentum flavum
Disc bulging or spondylolisthesis may also cause
Back pain, transient leg tingling, pain in calf and lower
extremity that is triggered by ambulation and improved with
rest
Can differentiate from vascular claudication through
detection of normal arterial pulses on exam
Physical Examination
Inspection of back and posture (ie. Scoliosis, kyphosis)
Range of motion
Palpation of the spine (vertebral tenderness sensitive
for infection)
If high suspicion of malignancy, do a
breast/prostate/lymph node exam
Peripheral pulses to distinguish from vascular
claudication
Physical Examination
Straight leg raise: for those with sciatica or spinal
stenosis symptoms
Patient supine, examiner holds patient’s leg straight
Elevation of less than 60 degrees abnormal and suggests
compression or irritation of nerve roots
Reproduces sciatica symptoms (NOT just hamstring)
Ipsilateral straight leg raise sensitive but not specific for
herniated disk
Crossed straight leg raise (symptoms of sciatica
reproduced when opposite leg is raised) insensitive byt
highly specific
Physical examination
Neurologic examination
L5: ankle and great toe
dorsiflexion
S1: plantar flexion, ankle
reflex
Dermatomal sensory loss
L5: numbness medial foot
and web space between 1st
and 2nd toes
S1: lateral foot/ankle
Imaging
AP and lateral L-spine if no clinical improvement after
4-6 weeks
Guidelines for American College of Physicians and
American Pain Society: “Clinicians should not
routinely obtain imaging or other diagnostic tests in
patients with nonspecific low back pain”
Do perform x-rays if: fever, unexplained weight loss, hx
of cancer, neurologic deficits, EtOH, IVDU, age <18 or
>50, trauma, immunosuppression, prolonged steroid
use, skin/urinary infection, indwelling catheter
Imaging
CT and MRI
More sensitive for detection of infection and cancer than
plain films
Also able to image herniated discs and spinal stenosis,
which cannot be appreciated on plain films
Beware: herniated/bulging discs often found in
asymptomatic volunteers may lead to
overdiagnosis/overtreatment
MRI better than CT for detection of infection,
metastases, rare neural tumours
Natural History
Most recover rapidly
90% of patients seen within 3 days of symptom onset
recovered within 2 weeks
Recurrences are common
Most have chronic disease with intermittent
exacerbations
Spinal stenosis is the exception usually gets
progressively worse with time
Therapy
Non-specific low back pain
Few RCTs; methodology of studies generally poor
quality
NSAIDs and muscle relaxants good for symptomatic
relief
Try giving regular rather than prn
Spinal manipulation (ie. chiropractic) of limited utility
in studies
Should recommend rapid return to normal activities
with neither bed rest nor exercise in the acute period
Bed rest found to not improve and may delay recovery
Exercises not useful in acute phase; use in chronic
Therapy
Nonspecific low back pain
Traction, facet joint injections, TENS ineffective or
minimally effective
Systematic reviews of acupunture have shown little
benefit
? Massage therapy some promising results
Surgery only effective for sciatica, spinal stenosis or
spondylolisthesis
Therapy
Herniated intervertebral discs
Nonsurgical treatment for at least a month
Exceptions: cauda equina syndrome, progressive neurologic
deficits
Early treatment same as for nonspecific low back pain,
but may need short courses of narcotics for pain control
Bed rest not useful
Some patients benefit from epidural corticosteroid
injections
If severe pain, neurologic defecits MRI and consider
surgery
Therapy
Spinal stenosis
Physiotherapy to reduce risk of falls
Analgesics, NSAIDs, epidural corticosteroids (no clinical
trials)
Decompressive laminecotomy
Spinal fusion + decompression if there is additional
spondylolisthesis
Symptoms often recur, even after successful surgery
Therapy
Chronic low back pain
Intensive exercise improves function and reduces pain,
but is difficult to adhere to
Anti-depressants: many with chronic low back pain are
also depressed
? Maybe for those without depression (tricyclics)
Opiates
Small RCT showed better effect on pain and mood than
NSAIDs
No improvement in actity
Significant side effects: drowsiness, constipation, nausea
Therapy
Chronic low back pain
Referral to multidisciplinary pain center
Cognitive-behavioural therapy, education, exercise, selective
nerve blocks
Surgical procedures rarely helpful
Introduction
Spondyloarthritis
Refers to inflammatory changes involving the spine and
the spinal joints.
Remember – can sometimes have peripheral arthritis without
spinal symptoms!
Seronegative Spondyloarthritis
Absence of Rheumatoid Factor
Psoriatic Arthritis
Ankylosing Spondylitis
Reactive Arthritis
Enteropathic Arthritis
Undifferentiated Spondyloarthropathy
How do you differentiate inflammatory from mechanical
back pain?
Inflammatory vs. Mechanical Back
Pain
Inflammatory Mechanical
Age of onset < 40 Any age
Insidious onset Acute onset
> 3 months duration < 4 weeks duration
> 60 min am stiffness < 30 min am stiffness
Nocturnal pain
No nocturnal pain
Improves with activity
Worse with activity
Tenderness over SI joints
Loss of mobility in all planes No SI joint tenderness
Decreased chest expansion Abnormal flexion
Unlikely to have neurologic Normal chest expansion
deficits Possible neurologic deficits
Clinical Features
Sacroiliitis
Usually bilateral and symmetric
Initially involves the synovial-lined lower 2/3 of the SI
joint
Earliest change: erosion on the iliac side of SI joint
(cartilage is thinner)
Could cause “pseudowidening” of SI joint
Bony sclerosis, then complete bony ankylosis or fusion
Spinal Involvement
Spinal Involvement
Gradual ossification of the outer layers of the annulus
fibrosis (Sharpey’s fibers) form interverterbral bony
bridges
Called syndesmophytes
Fusion of the apophyseal joints and calcification of the
spinal ligaments along with bilateral syndesmophyte
formation can result in “bamboo spine”
Enthesitis
Enthesis: site of insertion of ligament, tendon or
articular capsule into bone
Enthesitis: inflammation of enthesis resulting in new
bone formation or fibrosis
Common sites: SI joints, intervertebral discs,
manubriosternal joints, symphysis pubis, iliac crests,
trochanters, patellae, clavicles, calcanei (Achille’s or
plantar fasciitis)
More Than Just Back Pain . . .
“ANK SPOND”
A Aortic insufficiency, ascending aortitis,
conduction abnormalities, pericarditis
N Neurologic: atlantoaxial subluxation and cauda
equina syndrome
K Kidney: amyloidosis, chronic prostatitis
S Spine: Cervical fracture, spinal stenosis, spinal
osteoporosis
More Than Just Back Pain . . .
P Pulmonary: upper lobe fibrosis, restrictive
changes
O Ocular: anterior uveitis (25-30% of patients)
N Nephropathy (IgA)
D Discitis or spondylodiscitis
Also: microscopic colitis in terminal ileum and colon (30-60%)
More Than Just Back Pain . . .
Remember that patients with AS can also have a
peripheral arthritis
Usually an oligoarthritis of the lower extremities
Occasionally, patients will present with peripheral
arthritis before they have back complaints
Physical Exam
Schober test
Detects limitation in forward flexion of the lumbar
spine
Place mark at dimples of Venus (or level of the posterio
superior iliac spine) and another 10 cm above, at the
midline
Ask patient to maximally forward flex with locked knees
Measure should increase from 10 cm to at least 15 cm
Modified Schober
Test
Making The Diagnosis
Treatment
Physiotherapy for all
Maintains good posture
Maintains chest expansion
Minimizes deformities
Treatment
NSAIDs
Good for mild symptoms
Potentially disease modifying
Indomethacin seems to work the best
Beware of side effects, especially gastrointestinal disease
Treatment
DMARDs
Sulfasalazine 1000-2000 mg bid
Seems to be the most effective for spinal symptoms
Methotrexate 15-25 mg weekly
For patients with prominent peripheral arthritis
Doesn’t work very well for spinal symptoms
Treatment
Steroids
Not very effective at all in AS
Local injections for enthesitis or peripheral arthritis
Anti-TNFα agents
Remicade (infliximab), Enbrel (etanercept) and Humira
(adalimumab)
Very useful for treating symptoms, improving ROM,
improving fatigue
Hopefully disease-modifying . . .
Any questions?
You might also like
- Hip Disorders, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentFrom EverandHip Disorders, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentNo ratings yet
- A Simple Guide to The Posture, Spine Diseases and Use in Disease DiagnosisFrom EverandA Simple Guide to The Posture, Spine Diseases and Use in Disease DiagnosisNo ratings yet
- Cervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Back Disorders, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentFrom EverandBack Disorders, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentNo ratings yet
- Carpal Tunnel Syndrome, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandCarpal Tunnel Syndrome, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Achilles Tendinitis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandAchilles Tendinitis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- Low Back PainDocument8 pagesLow Back PainLev KalikaNo ratings yet
- Trochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandTrochanteric Bursitis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Adhesive Capsulitis, (Frozen Shoulder) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAdhesive Capsulitis, (Frozen Shoulder) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Acromioclavicular Joint Injury, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAcromioclavicular Joint Injury, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- DeQuervain Disease, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDeQuervain Disease, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Shoulder Disorders, A Simple Guide To The condition, Diagnosis, Treatment And Improvised TreatmentFrom EverandShoulder Disorders, A Simple Guide To The condition, Diagnosis, Treatment And Improvised TreatmentRating: 5 out of 5 stars5/5 (1)
- A Simple Guide to Extensor Tendonitis, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Extensor Tendonitis, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Medial Meniscus Tears, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMedial Meniscus Tears, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Trigger Finger, A Simple Guide to The Condition, Treatment And Related DisordersFrom EverandTrigger Finger, A Simple Guide to The Condition, Treatment And Related DisordersNo ratings yet
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementFrom EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementNo ratings yet
- Herniated Disk, (Slipped Disk) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHerniated Disk, (Slipped Disk) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Sprain and Strains, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandSprain and Strains, A Simple Guide to the Condition, Treatment and Related DiseasesNo ratings yet
- Flat Foot (Pes Planus), A Simple Guide to The Condition, Treatment And Related ConditionsFrom EverandFlat Foot (Pes Planus), A Simple Guide to The Condition, Treatment And Related ConditionsRating: 1 out of 5 stars1/5 (1)
- PROLOG: Obstetrics, Ninth Edition (Assessment & Critique)From EverandPROLOG: Obstetrics, Ninth Edition (Assessment & Critique)No ratings yet
- Exercise your way to health: Arthritis: Exercise plans to improve your lifeFrom EverandExercise your way to health: Arthritis: Exercise plans to improve your lifeNo ratings yet
- Scaphoid Fracture, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandScaphoid Fracture, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Exploring Cupping Today: A Beginners Course On Cupping Therapy & It's BenefitsFrom EverandExploring Cupping Today: A Beginners Course On Cupping Therapy & It's BenefitsNo ratings yet
- Mobilization and Stimulation of Neuromuscular Tissue (MaSoNT)From EverandMobilization and Stimulation of Neuromuscular Tissue (MaSoNT)No ratings yet
- Neck Pain, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandNeck Pain, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Qi of Taking a Medical History and Performing a Physical ExaminationFrom EverandThe Qi of Taking a Medical History and Performing a Physical ExaminationNo ratings yet
- A Simple Guide to Pick Disease, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Pick Disease, Diagnosis, Treatment and Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Recent Advances in PhysiotherapyFrom EverandRecent Advances in PhysiotherapyCecily PartridgeNo ratings yet
- Presentation Lower Back PainDocument86 pagesPresentation Lower Back PainSten SchaperNo ratings yet
- Low Back Pain Presentation IMPDocument114 pagesLow Back Pain Presentation IMPrapannika100% (3)
- Low Back Pain PDFDocument54 pagesLow Back Pain PDFwiwiNo ratings yet
- Neck Pain PhysiotherapyDocument34 pagesNeck Pain Physiotherapysaini_shyam99100% (1)
- Mechanical or Inflammatory Low Back Pain PDFDocument7 pagesMechanical or Inflammatory Low Back Pain PDFHugo FalquetoNo ratings yet
- Effect of Physiotherapy Treatment On Frozen ShoulderDocument6 pagesEffect of Physiotherapy Treatment On Frozen Shoulderalfi putri bahriNo ratings yet
- 9 Pregnancy Stretches For The Whole Body 4 Pager Apr17 v3Document4 pages9 Pregnancy Stretches For The Whole Body 4 Pager Apr17 v3LeiltonNo ratings yet
- Shoulder Special TestsDocument36 pagesShoulder Special TestsNidal HusseinNo ratings yet
- Introduction PhysiotherapistDocument12 pagesIntroduction Physiotherapistapi-371068989No ratings yet
- Sciatica Pain - SI Joint Pain Prolotherapy TreatmentDocument3 pagesSciatica Pain - SI Joint Pain Prolotherapy Treatmentsherya12No ratings yet
- Forward Head Posture Correction Versus Shoulder Stabilization Exercises Effect On Scapular Dyskinesia and Shoulder Proprioception in Athletes An Experimental StudyDocument7 pagesForward Head Posture Correction Versus Shoulder Stabilization Exercises Effect On Scapular Dyskinesia and Shoulder Proprioception in Athletes An Experimental StudyInternational Journal of PhysiotherapyNo ratings yet
- Irogue Seminar Presentation October 2010Document186 pagesIrogue Seminar Presentation October 2010Kennedy Eghosa Irogue100% (2)
- Physiotherapy For Tennis ElbowDocument2 pagesPhysiotherapy For Tennis ElbowenadNo ratings yet
- Physiotherapy Rehabilitation Guidelines - Lumbar DisectomyDocument6 pagesPhysiotherapy Rehabilitation Guidelines - Lumbar Disectomyalina4891No ratings yet
- Physical Therapy For Low Back Pain (Jurnal Saraf)Document6 pagesPhysical Therapy For Low Back Pain (Jurnal Saraf)Aramanda DianNo ratings yet
- Multifidus ExercicesDocument2 pagesMultifidus Exercicesjo21cu100% (1)
- Brunstorm'sDocument19 pagesBrunstorm'sHARSH 23 (Jalu)No ratings yet
- Tennis Elbow ExerciseDocument2 pagesTennis Elbow Exercisedhirajkumar_1No ratings yet
- Physical Examination of The Shoulder FinalDocument28 pagesPhysical Examination of The Shoulder FinalAndinNo ratings yet
- Scapula DyskinesiaDocument5 pagesScapula Dyskinesiamiguelax1No ratings yet
- Soap Note 5.0Document4 pagesSoap Note 5.0Paulus IskandarNo ratings yet
- Therapeutic Exercise (I) : Theory and PracticeDocument155 pagesTherapeutic Exercise (I) : Theory and PracticeAbdulrhman MohamedNo ratings yet
- ASIA Impairment ScaleDocument10 pagesASIA Impairment Scaleazimahzainal211No ratings yet
- I. Etiology Primary Adhesive Capsulitis Secondary Adhesive CapsulitisDocument8 pagesI. Etiology Primary Adhesive Capsulitis Secondary Adhesive CapsulitisVanessa Yvonne Gurtiza100% (1)
- Anterior Cruciate Ligament Injuries-Orthoinfo - AaosDocument5 pagesAnterior Cruciate Ligament Injuries-Orthoinfo - Aaosapi-228773845No ratings yet
- Cervical RadiculopathyDocument36 pagesCervical RadiculopathyAri SudarsonoNo ratings yet
- Anterior Shin Splint ProjectDocument59 pagesAnterior Shin Splint ProjectK sai sufhaNo ratings yet
- Network ResultsDocument56 pagesNetwork Resultslynkx864No ratings yet
- TBC COMBINED W ACCESS 3.40 - 4 PDFDocument194 pagesTBC COMBINED W ACCESS 3.40 - 4 PDFlynkx864No ratings yet
- TBC Network Adjustment Settings AustraliaDocument19 pagesTBC Network Adjustment Settings Australialynkx864No ratings yet
- Sum Total of Regression Analysis06 - 12Document80 pagesSum Total of Regression Analysis06 - 12lynkx864No ratings yet
- Total Sum Regression Analysis 99 - 05Document119 pagesTotal Sum Regression Analysis 99 - 05lynkx864No ratings yet
- Regression Analysis 99 - 05Document119 pagesRegression Analysis 99 - 05lynkx864No ratings yet
- Analysis 99 05Document3 pagesAnalysis 99 05lynkx864No ratings yet
- DecompressionDocument6 pagesDecompressionPásztai ZoltánNo ratings yet
- MED BACK of LBPDocument23 pagesMED BACK of LBPleeyan2wenty6No ratings yet
- SciaticaDocument35 pagesSciaticaRahmadanii RahmadaniiNo ratings yet
- DownloadDocument11 pagesDownloadChristopher Chew Dian MingNo ratings yet
- Assessment of Back PainDocument59 pagesAssessment of Back PainDmitry VoxNo ratings yet
- UNIT 16 Spa Treatments Syllabus V2Document7 pagesUNIT 16 Spa Treatments Syllabus V2Jowie SooNo ratings yet
- 6 - Lumbar Disc HerniationDocument24 pages6 - Lumbar Disc HerniationHADI BADWANNo ratings yet
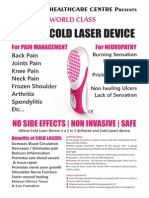
- Ultima Cold Laser DeviceDocument2 pagesUltima Cold Laser DeviceullasaaithalNo ratings yet
- Sapta Abhyas - Project For Commerce Degree PassoutDocument6 pagesSapta Abhyas - Project For Commerce Degree PassoutRavi GodaseNo ratings yet
- Diseases in The Nervous SystemDocument19 pagesDiseases in The Nervous SystemZachary me meNo ratings yet
- 1.medial Hamstring ReflexDocument5 pages1.medial Hamstring ReflexIgnatius EseneNo ratings yet
- Master Tong Information Document PDFDocument105 pagesMaster Tong Information Document PDFKimberly100% (2)
- Epidural Steroid InjectionsDocument48 pagesEpidural Steroid InjectionsMediatrix OhoiwirinNo ratings yet
- Intervertebral Disc Prolapse: AnnulusDocument2 pagesIntervertebral Disc Prolapse: AnnulusIndra KurniawanNo ratings yet
- In Re Briggs A WLS Employee 12-22560Document107 pagesIn Re Briggs A WLS Employee 12-22560NevadaGadflyNo ratings yet
- Sciatica Exercises - 6 StretchesDocument14 pagesSciatica Exercises - 6 StretchestonyNo ratings yet
- Canal Stenosis Vs HNPDocument12 pagesCanal Stenosis Vs HNPBayu Antara HadiNo ratings yet
- A Case Study of Cauda Equina SyndromeDocument5 pagesA Case Study of Cauda Equina SyndromeProfessor Stephen D. Waner100% (5)
- CLASS XII Physical Education NOTESDocument37 pagesCLASS XII Physical Education NOTESAbdullah JahufarNo ratings yet
- Caudal Epidural InjectionDocument6 pagesCaudal Epidural InjectionRS BaptisNo ratings yet
- KaufmanDocument2 pagesKaufmanrbtakemotoNo ratings yet
- Oet Online ListeningDocument270 pagesOet Online ListeningRoney88% (17)
- Jurnal 7 PDFDocument10 pagesJurnal 7 PDFAmorrita Puspita RatuNo ratings yet
- RAMNATH Sciatica Presentation 0812Document57 pagesRAMNATH Sciatica Presentation 0812Nisa SulistiaNo ratings yet
- Vegetable Kingdom Continued: SciaticDocument14 pagesVegetable Kingdom Continued: SciaticSatyendra RawatNo ratings yet
- Physiotherapy Management of SciaticaDocument6 pagesPhysiotherapy Management of SciaticaMuly Arafah ZakariaNo ratings yet
- Low Back Pain Guidelines-Reduced2Document26 pagesLow Back Pain Guidelines-Reduced2ranggadr100% (1)
- Mulligan Mobilization Versus Stretching On The Management of Piriformis Syndrome A Comparative StudyDocument6 pagesMulligan Mobilization Versus Stretching On The Management of Piriformis Syndrome A Comparative StudyInternational Journal of PhysiotherapyNo ratings yet
- Classification and Low Back Pain: Review Literature and Critical Analysis Selected SystemsDocument30 pagesClassification and Low Back Pain: Review Literature and Critical Analysis Selected SystemsKhilyatud DiniyahNo ratings yet
- Hildebrandt 2000 PDFDocument12 pagesHildebrandt 2000 PDFAlexandre FerreiraNo ratings yet