Professional Documents
Culture Documents
RESPIRATION
Uploaded by
Audhrey B0 ratings0% found this document useful (0 votes)
2 views19 pagesOriginal Title
RESPIRATION (2).ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views19 pagesRESPIRATION
Uploaded by
Audhrey BCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 19
RESPIRATION
• Respiratory system is charged both with
ensuring uptake of adequate oxygen to meet the
metabolic needs of the body’s cells and
disposing of the carbon dioxide produced during
metabolism by these cells.
Oxygen is the final electron acceptor for all the
metabolic processes taking place within the
mitochondria, including fatty acid oxidation, the
citric acid cycle, and the electron transport chain,
the last of which generates adenosine
triphosphate (ATP) for energy needs of the cell.
• In aggregate, these metabolic processes consume a
considerable amount of oxygen. To meet this ceaseless
demand for oxygen, three system must interact in a
seamless manner so that the individual can promptly
adjust to varying metabolic demands. These three
systems are:
1. The lungs and associated muscular pumping
mechanisms which take in oxygen from the air and
exhale carbon dioxude into the atmosphere.
2. The blood and circulatory system with hemoglobin
rich red blood cells that transport O2 and CO2.
3. The nervous system which controls the rhythmic
action of the respiratory system including the lungs,
airways, and muscular bellows in response to the body’s
needs.
• Surfactant and surface tension.
Even though surface tension is crucial to
maintaining the intimacy of two pleural suefaces,
this same physical force could obliterate the
alveolar spaces if there was not some substance
to mitigate alveolar surface tension. Fortunately, a
group of proteins and phospholipid, collectively
referred to as surfactant, decreases the surface
tension in the alveoli, thus maintaning their
patency, much as soap bubbles maintain
themselves.
To prevent alveolar collapse, the alveolar wall
contains a specialized, Type II, pneumocyte,
which is responsible for synthesis and secretion
of surfactant into the extracellular space
interposed between the alveolar air and the
epithelial cell surface.
• Surfactant functions to lower the surface tension
at the gas-liquid interface.
Approximately 90% of the composition of
surfactant is lipid in nature, of which virtually
90% is phospholipid
(dipamitoylphosphatidylcholine [DPPC] which
constitutes 70%-80% of the phospholipid).
By lowering the surface tension, surfactant
prevents alveolar collapse and reduces the effort
to expand the lungs after each expiration.
When, because of prematurity, surfactant is not
manufactured, respiratory distress syndrome
(RDS) of the neonate results. And when in any
age group, sepsis or other serious disease
damage the lung and consequently the
synthesis of surfactant, adult RDS results.
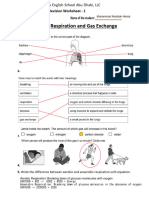
• Physical exchange of gases
The term of this kind of respiration is
applied to the interchange of the 2 gases,
oxygen and CO2, between the body and
its environment.
The atmospheric air which we inhale has
the following composition: oxygen, 20.96%
(PO2: 159 mm Hg) ; CO2, 0.04% (PCO2:
30.4 mm Hg); and nitrogen, 79% (PNO2:
570 mm Hg). Other gases present in trace
amount but are not of physiologic
importance.
• The expired air contains the same amount
of nitrogen as the inspired air; the total
pressure in the alveoli after correction for
the vapor pressure of water (47 mm Hg) is
713 mm Hg. In the alveoli, the oxygen has
been reduced to about 15% (PO2: 107
mm Hg), and the CO2 increased to about
5% (PCO2: 36 mm Hg). About one-fourth
of the oxygen of the inspired air has
passed into the blood and has been
replaced in the expired air by an equal
amount of CO2 which has left the blood
• When the gases of the inspired air come in
contact with the alveolar membrane of the
lung, it is assumed that the exchange of
gases takes place in accordance with the
usual physical laws of diffusion. Thus, the
gas passes through the membrane and
into the blood, or in the reverse direction,
in accordance with the difference in the
pressure of that particular gas on either
side of the membrane.
• The exchange of gases between the alveoli and
the blood is illustrated by the following:
Oxygen tension in alveolar air: 107 mm Hg
Oxygen tension in venous blood: 40 mm Hg
A pressure difference of 67 mm Hg serves to
drive oxygen from the alveoli of the lung into the
blood.
CO2 tension in alveolar air: 36 mm Hg
CO2 tension in venous blood: 46 mm Hg
• A relatively small difference of 10 mm Hg is
sufficient to drive CO2 from the blood into the
lung. This small difference in pressure is
adequate because of the rapidity of the diffusion
of CO2 through the alveolar membrane (the
diffusion coefficient for CO2 is 20 times that of
O2 because CO2 is much more soluble than O2
is).
After this exchange of gases has occured, the
blood becomes arterial (in chemical sense).
Arterial blood has an oxygen tension of about
100 mm Hg and a CO2 tension of 40 mm Hg.
• The transport of oxygen by the blood.
The transport of oxygen by the blood from the
lung to the tissues is due mainly to the ability of
hemoglobin to combine reversibly with oxygen.
Hb + O2 = HbO2
The degree of combination of oxygen with
hemoglobin or its dissociation of oxyhemoglobin
is determined by the tension of the oxygen in the
medium surrounding the hemoglobin.
At a tension of 100 mm Hg or more, hemoglobin
is completely saturated. Under these condition,
approximately 1.34 ml of oxygen are combined
with each gram of hemoglobin.
• Effect of CO2 on blood pH
Although the CO2 evolved from the tissues will
form carbonic acid, very little CO2 can actually
be carried in this form because the effect of
carbonic acid on the pH of the blood. Is is
estimated that in 24 hours the lungs remove the
equivalent of 20-40 liters of 1N acid as carbonic
acid. This large acid load is successfully
transported by the blood with hardly any
variation in the blood pH, since most of the
carbonic acid formed is promptly converted to
bicarbonate.
H2CO3 = H + + HCO3 + B+ = BHCO3 + H+.
• The buffer system of the blood
Although venous blood carried considerably
more CO2 than does arterial blood, the buffers
of the blood are so efficient that the pH of
venous blood is more acid than that of arterial
blood by only 0.01-0.03 units, ie, pH 7.40 vs pH
7,43.
These blood buffers consist of plasma protein,
hemoglobin, and oxyhemoglobin and
bicarbonate and inorganic phosphates.
• The hemoglobin buffers
Hemoglobin acts as a buffer because it carries the basic
amino acid histidine in a number of exposed position.
These histidine residues can combine reversibly with
hydrogen ions, producing protonated and unprotonated
forms of hemoglobin.
Most important, is the unique buffering role of
hemoglobin and oxyhemoglobin, which account for 60%
of the CO2 carrying capacity of whole blood.
The remarkable buffering capacity of hemoglobin is due
to the fact that this protein in the oxy form is a stronger
acid than in the reduced form.
• Bicarbonate distribution between plasma and
erythrocytes.
CO2 reacts with water to form carbonic acid
which undergoes partial dissociation to produce
the conyugate base, bicarbonate. The reaction
CO2 with water to carbonic acid is reversible
and mainly made inside the red blood cell since
the catalyzing enzyme, carbonic anhydrase, is
found within the erythrocyte and other cell types.
Bicarbonate and chloride exchanged freely
across the erythrocyte membrane.
Electrical neutrality must be maintained across
the membrane. Maintenance of this neutrality
can be accomplished by exchange mechanism
between bicarbonate and chloride which is
called chloride shift
• Acid-base balance
The buffers in the blood act in conyunction with
mechanisms in the kidneys for excreting protons as well
as with mechanisms in the lungs for exhaling CO2 to
maintain the pH within the normal range (acid-base
balance).
Although a buffer solution is most effective at mitigating
pH shift when its initial pH (7.35-7.45 in blood) is the
same as its pKa, this limitation for the HCO3-/H2CO3
system, with a pKa of 6,1, is overridden by the body’s
ability to eliminate CO2 via the lungs.
HCO3- and H2CO3 can be conveniently expressed in a
useful form as the familiar Henderson-Hasselbalch
equation:
pH = pKa + log [HCO3-]/{H2CO3]
or
pH = pKa + log (kidney/lungs), where kidney = [HCO3-]
and lungs = [H2CO3]
• Disturbances in acid-base balance
A. Metabolic acidosis
Caused by a decrease in the bicarbonate fraction.
It occurs in uncontrolled diabetes with ketosis, in renal disease, in
diarrhea.
Compensation by lungs (hyperventilation).
B. Respiratory acidosis
Caused by an increase in carbonic acid fraction.
It occurs in any disease which impaired respiration, in morphine
poisoning (depression of the respiratory center).
Compensation by the kidney (increase reabsorption of bicarbonate)
C. Metabolic alkalosis
Caused by an increase in the bicarbonate fraction.
It occurs in prolonged vomiting, after ingestion of large quantities of
alkali, in Cushing syndrome.
Compensation by the lungs (hypoventilation).
D. Respiratory alkalosis
Caused by a decrease in the carbonic acid fraction.
It occurs in hysterical hyperventilation, in the early stages of
salicylate poisoning (stimulate the respiratory center).
You might also like
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument55 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsAudhrey BNo ratings yet
- Ehaa575 PDFDocument79 pagesEhaa575 PDFPatricia MarceloNo ratings yet
- GINA 2019 Main Pocket Guide Wms PDFDocument39 pagesGINA 2019 Main Pocket Guide Wms PDFmyikellaNo ratings yet
- Category Indeks Brinkman in Mild 1-199 in Patient With Lung Cancer PDFDocument8 pagesCategory Indeks Brinkman in Mild 1-199 in Patient With Lung Cancer PDFtheaNo ratings yet
- Overview of Gram - Negative Rods Enterobacteriaceae & Other Than EnterobacteriaceaeDocument51 pagesOverview of Gram - Negative Rods Enterobacteriaceae & Other Than EnterobacteriaceaeAudhrey BNo ratings yet
- J Neurosurg Article p1764Document8 pagesJ Neurosurg Article p1764Audhrey BNo ratings yet
- History Taking of Fever Torniquete Ba Rev 21032011Document24 pagesHistory Taking of Fever Torniquete Ba Rev 21032011Audhrey BNo ratings yet
- Glomerular Diseases: What Are The Kidneys and What Do They Do?Document12 pagesGlomerular Diseases: What Are The Kidneys and What Do They Do?Galo FarfanNo ratings yet
- VirusDocument28 pagesVirusAudhrey BNo ratings yet
- Anthelmintec & Antiprotozoa 2019Document31 pagesAnthelmintec & Antiprotozoa 2019Audhrey BNo ratings yet
- ImmunoDocument10 pagesImmunoAudhrey BNo ratings yet
- Lecture 11 - Circulation .UPH - BB 2019Document33 pagesLecture 11 - Circulation .UPH - BB 2019Audhrey BNo ratings yet
- Antimicrobial DrugsDocument11 pagesAntimicrobial DrugsAudhrey BNo ratings yet
- Dna VirusesDocument37 pagesDna VirusesAudhrey BNo ratings yet
- Congenital Heart Disease Table PDFDocument5 pagesCongenital Heart Disease Table PDFAudhrey BNo ratings yet
- Anthelmintec & Antiprotozoa 2019Document31 pagesAnthelmintec & Antiprotozoa 2019Audhrey BNo ratings yet
- Congenital Heart Disease Table PDFDocument5 pagesCongenital Heart Disease Table PDFAudhrey BNo ratings yet
- GINA 2019 Main Pocket Guide Wms PDFDocument39 pagesGINA 2019 Main Pocket Guide Wms PDFmyikellaNo ratings yet
- Anti Fungal: Dr. Dr. Nico L Lumbuun, SPFKDocument45 pagesAnti Fungal: Dr. Dr. Nico L Lumbuun, SPFKAudhrey BNo ratings yet
- Overview of Gram - Negative Rods Enterobacteriaceae & Other Than EnterobacteriaceaeDocument51 pagesOverview of Gram - Negative Rods Enterobacteriaceae & Other Than EnterobacteriaceaeAudhrey BNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Cbse LP RevisionDocument18 pagesCbse LP RevisionKanak ChhajerNo ratings yet
- Organisma L BiologyDocument35 pagesOrganisma L BiologyJvc CawiliNo ratings yet
- Grade 9 Chapter 1 Revision Worksheet - 1Document3 pagesGrade 9 Chapter 1 Revision Worksheet - 1Abdullah AkmalNo ratings yet
- Oxygen InsuffiencyDocument21 pagesOxygen InsuffiencyAntony Raj Culandai Swamy100% (1)
- Biology Paper 1Document24 pagesBiology Paper 1Nyakweba DenisNo ratings yet
- GCE Biology-Human Biology-Teachers' Guide Revised 18-02-14Document93 pagesGCE Biology-Human Biology-Teachers' Guide Revised 18-02-14mariumrana40No ratings yet
- Chapter 06Document47 pagesChapter 06gayathmipereraNo ratings yet
- Chap8F4 Respiratory Systems in Humans and AnimalsDocument77 pagesChap8F4 Respiratory Systems in Humans and AnimalsSyahir NajmiNo ratings yet
- Session 6 The Living Organisms-Characteristics and HabitatsDocument8 pagesSession 6 The Living Organisms-Characteristics and HabitatsAakritiNo ratings yet
- Cambridge IGCSE: BIOLOGY 0610/43Document20 pagesCambridge IGCSE: BIOLOGY 0610/43Sraboni ChowdhuryNo ratings yet
- Science Final X 1mcqDocument51 pagesScience Final X 1mcqbhagyapatel9723No ratings yet
- Tilapia DissectionDocument3 pagesTilapia DissectionQuentin LopezNo ratings yet
- Nursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationDocument10 pagesNursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationmalindaNo ratings yet
- ARDS With PathophysiologyDocument79 pagesARDS With Pathophysiologymabec pagaduan95% (19)
- CHN 215 - PTB CasepresDocument57 pagesCHN 215 - PTB CasepresJeanneva Osorio EscoteNo ratings yet
- SPM 4 - RespirationDocument1 pageSPM 4 - RespirationKumar AyavooNo ratings yet
- 0610 w07 QP 1Document19 pages0610 w07 QP 1Hubbak Khan100% (3)
- Respiratory and Circulatory SystemsDocument58 pagesRespiratory and Circulatory SystemsmiomodgNo ratings yet
- Pulmonary Physiology Ninth Edition 9thDocument57 pagesPulmonary Physiology Ninth Edition 9thmarlene.harder135100% (40)
- Worksheet - I: Biology XDocument7 pagesWorksheet - I: Biology XDharmendra SinghNo ratings yet
- 7.2 Lungs - Gas Exchange Exam QuestionsDocument3 pages7.2 Lungs - Gas Exchange Exam QuestionsManan Patel100% (1)
- Lesson Plan Biology Form 4 2011Document8 pagesLesson Plan Biology Form 4 2011rafidah1966No ratings yet
- Grade 9 Question Review ScienceDocument40 pagesGrade 9 Question Review ScienceValentino TommyNo ratings yet
- Grade 8 RespirationDocument6 pagesGrade 8 RespirationShanel WisdomNo ratings yet
- MYP Biology Booklet # 3 Grade9 - MS1Document27 pagesMYP Biology Booklet # 3 Grade9 - MS1Aref Dahabrah100% (1)
- Grade 7 Biology Revision Worksheet II 2022Document5 pagesGrade 7 Biology Revision Worksheet II 2022Ishanee BoseNo ratings yet
- Bgcse Coursework BiologyDocument5 pagesBgcse Coursework Biologyjlnggfajd100% (3)
- Class 10th Biology - Maha Marathon (Prashant Kirad)Document183 pagesClass 10th Biology - Maha Marathon (Prashant Kirad)yashuummachgiNo ratings yet
- Bio4 5Document11 pagesBio4 5HarmonyChuiNo ratings yet
- Characteristics of Living ThingsDocument18 pagesCharacteristics of Living ThingsNinad ChoudhuryNo ratings yet