Professional Documents
Culture Documents
Pneumonia 13
Uploaded by
Ez Ball0 ratings0% found this document useful (0 votes)
9 views23 pagesInternal medicine note. Pediatrics.
Original Title
Pneumonia_13.ppt
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentInternal medicine note. Pediatrics.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views23 pagesPneumonia 13
Uploaded by
Ez BallInternal medicine note. Pediatrics.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 23
Pneumonia
• Pneumonia is an inflammation of the
paranchyma of the lung
• the various clinical pneumonia are often
classified by their anatomic distribution
lobar
lobular
interstitial
bronchopneumonia
conti
• By the agent that cause
viral
bacterial
aspiration
• Certain lesion are commonly produced by
specific causative agent
Example
Pneumococcus produces an inflammatory
mucosal lesion and alveolar exudates usually
without destruction of mucosal cells or extensive
involvement of interstitial tissue.
• The gross lesion is a consolidation of all parts of
a lob or lobular variety, or of scattered lobules
the broncho-pneumonic variety
• Pneumocccal pneumonia characteristically
assumes a lobar pattern in alder children and
young adults, but lobar consolidation is less
typical in young children.
• In contrast, viral agents, H.influenza and certain
strains of viridance group of streptococcusi
invade or destroy the mucus membrane and may
produce principally bronchiolitis and
peribronchiolitis and interstitial lesion
• Both staphylococcus and klebsiella tend to
destroy tissue and to produce multiple small
abscesses
Etiology
• The age of the child and the presence or absence
of underlying disease, determine the etiology of
bacterial pneumonia.
• Bacterial pneumonia presenting in the first 2
days of life is generally acquired in utero or
intrapartum- group B streptococci, listeria
monocytogenes, H,influenza, gram negative
enteric bacilli
conti
• After neonatal period- strep, pneumonia,
H,influenza type b, staphylococcus aureus,
group A streptococci
• Children older than 4-5yr- streptococcal-
pneumonia, mycoplasma pneumonia
Pathogenesis
• The respiratory tract bellow the vocal cord is
sterile, micro organism, are excluded from the
tracheobronchial tree by nonspecific host
defenses, including the blanket of mucus
covering the mucosal epithelium, ciliary
transport activity, and the cough reflex
• Secretory IgA antibody
• Within lung parenchyma by the lymphatic
channels and macrophages that line the terminal
bronchioles and alveoli
conti
• By systemic humeral and cell mediated immune
mechanism, including passively acquired
maternal antibody
• The transmission is person to person via close
personal contact or via airborne spread
• Colonization of the URT with pathogenic
bacteria is relatively common
• The prevalence of carriage of pneumococci,
H,influenza, type b or meningococci in
approximately 40%, 10% and 2% respectively
conti
• Pneumonia results from aspiration of
pathogenic bacteria in the LRT
• The process may be aided by concurrent viral
infection, particularly with RSV, measles, and
influenza virus
• Acute viral infection serves to disrupt the normal
anatomic and physiological barriers of the
respiratory tract mucosa and may briefly
suppress the activity of phagocytic leukocytes in
the airway and lungs
conti
• Less common, bacterial spread in the lung
hematogenously from distant focus
Clinical feature
• Older children and adolescent present-
Fever, chilliness, headache, dyspnea,
productive cough, chest pain, abdominal
pain and nausea or vomiting, circumoral
cyanosis,
Retraction, nasal flaring, dullness,
diminished tactile and vocal fremitus, BBS,
and rales
• Young infants
present with non specific symptoms of
fever, lethargy, poor feeding, respiratory
distress (grunting, nasal flaring, IC, SC,
Supra clavicular)
Dullness, BBS and rales
Displacement of the diaphragm,
abdominal distention, nuchial rigidity with
out meningeal infection
Complication
1. Parapneumonic effusion
Transudate few WBC, low protein and
PH > 7.2
Exudate (empyma) WBC> 15,000/cm, protein
more than 3.o gm/l, PH <7.2
Staph-aureus, Hinfluenza and strep pneumonia
Continous fever, chestpain, dyspnea,
tachycardia, dullnes and diminished breath sound
X- ray lateral ducubitus
• RX antibiotic
drainage pleural fluid- needle aspiration for
empyema requires insertion of one or more
thoracotomy tube
2. Pneumatocel cx of 40% staphylococcus
pneumonia
Asymptomatic , except when rupture into
pleural space, causing a pneumothorax or pyo
pneumothorax
Most persist for 2-3 months and resolve
spontaneously
3. Lung abscess
Dependent segment of the lung- the
posterior segment of the right upper lobe
Anaerobic bacteria play a prominent role
Sx fever cough, tachypnea, and fetid breath
oder
X ray focal infiltrate surrounding a cavity
that contain an air fluid level, in 10% of pts have
more than one cavity
• Rx
3-4 wks course of penicillin G
Metronidazole or clindomcin
Diagnosis
• Chest x ray
• Presence of lobar consolidation, pleural effusion,
suggestive of bacterial infection
• Pneumatocel and abscess cavities are diagnostic
• Culture from blood or pleural fliud
treatment
• Depends on the severity of the illness and
presence or absence of underlying chronic
disease
• Antibiotics and maintenance of oxygenation is
the main stay of treatment of bacterial
pneumonia
• Pneumococcal pneumonia penicillin G
100,000units/kg, cefotaxim 150 mg/kg/24hr,
Ceftriaxon 75mg/kg/24hr
Vancomycin 40mg/kg/24hr in case of penicillin
resistance
• Group A streptococcal pneumonia
Penicillin G 100,000 unit/kg/24hr
Stapylococcal pneumonia
semisyntetic ,penicilinase-resistant penicillin
naficillin 200mg/kg/24hr
• Haemophilus influenza pneumonia
Ceftriaxon 75mg/kg/24hr, cefotaxim
150mg/kg/24hr
Strain is sensitive ampicillin 100mg/kg/24hr
References
1. Nelson text book of pediatrics 20th dition
2. Principles and practice of pediatrics
by Frank A. Oski
3. International child health care, a practical
manual for hospitals worldwide
Child advocacy international
by David Southall, Brian Coulter, Christian
Ronald, Sue Nicholson, Simon Park
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- MF PDFDocument1 pageMF PDFEz BallNo ratings yet
- 6b026df416bab4acd92fe51e4 PDFDocument2 pages6b026df416bab4acd92fe51e4 PDFEz Ball100% (1)
- a2lobnZicWRyMTU5M PDFDocument2 pagesa2lobnZicWRyMTU5M PDFEz Ball0% (1)
- Classification of Newborn, - 130319150346Document45 pagesClassification of Newborn, - 130319150346Ez Ball100% (1)
- Classification of Newborn, - 130319150346Document45 pagesClassification of Newborn, - 130319150346Ez Ball100% (1)
- BronchiolitisDocument12 pagesBronchiolitisEz BallNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Factors Aff ToursmDocument15 pagesFactors Aff ToursmDheleepan GvNo ratings yet
- Intrapartum AssessmentDocument9 pagesIntrapartum AssessmentSarah RiceNo ratings yet
- Field Veterinarian Notes by DR CsDocument98 pagesField Veterinarian Notes by DR CsSanjay Kumar67% (3)
- FILARIASISDocument57 pagesFILARIASISadekayo100% (6)
- Child - Health - in - Developing - Countries 2015-2016 PDFDocument155 pagesChild - Health - in - Developing - Countries 2015-2016 PDFNovi AryandaNo ratings yet
- Insidious ScreenplayDocument104 pagesInsidious ScreenplayFaisal Hashmi100% (4)
- Culture MediaDocument3 pagesCulture MediaMicNo ratings yet
- 211221Document2 pages211221ZenitraNo ratings yet
- Contact Lens & Anterior EyeDocument6 pagesContact Lens & Anterior EyehansenpanjaitanNo ratings yet
- Atopic Disease Bronchial AsthmaDocument33 pagesAtopic Disease Bronchial AsthmaEmeraldyModyNo ratings yet
- Rules & Regulations For Medical Examination of Expatriates Coming To GCC States For ResidenceDocument25 pagesRules & Regulations For Medical Examination of Expatriates Coming To GCC States For Residencevj bharathNo ratings yet
- Case Study CopdDocument7 pagesCase Study CopdIrveen Joy RamirezNo ratings yet
- Rochester Treatment of Asthma 3 1906Document4 pagesRochester Treatment of Asthma 3 1906IGNo ratings yet
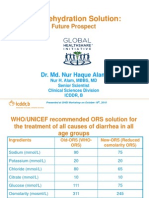
- Oral Rehydration Solution:: Future ProspectDocument48 pagesOral Rehydration Solution:: Future ProspectmustikaarumNo ratings yet
- Atypical MeaslesDocument2 pagesAtypical MeaslesBagusPranataNo ratings yet
- Exercicio Prefixo Sufixo 1Document5 pagesExercicio Prefixo Sufixo 1Jayla MouraNo ratings yet
- Dentures Types Benefits and Potential ComplicationsDocument294 pagesDentures Types Benefits and Potential ComplicationsSorabh JainNo ratings yet
- Management of Scabies PDFDocument5 pagesManagement of Scabies PDFAfnindyas AtikaNo ratings yet
- Standards Guidelines UVGIDocument5 pagesStandards Guidelines UVGIVipul JainNo ratings yet
- The Problem and Its Background The Feasibility of Garlic (Allium Sativum) As An Alternative Head Lice RemoverDocument20 pagesThe Problem and Its Background The Feasibility of Garlic (Allium Sativum) As An Alternative Head Lice RemoverKiller KnightNo ratings yet
- Antibiotics ClassificationDocument7 pagesAntibiotics ClassificationTabarcea Dorin100% (1)
- Teaching Plan SampleDocument3 pagesTeaching Plan SampleSoleil MaxwellNo ratings yet
- Course Objectives 3313Document11 pagesCourse Objectives 3313Hugh JacobsNo ratings yet
- Healthsystem IndiaDocument151 pagesHealthsystem IndiasanjnuNo ratings yet
- Helminth Revision 2Document1 pageHelminth Revision 2FarlogyNo ratings yet
- CD ExamsDocument3 pagesCD ExamsGilbert SalacupNo ratings yet
- SelulitisDocument37 pagesSelulitiswindhymonicaNo ratings yet
- 3rd Mid CaseDocument32 pages3rd Mid CaseHarshini MakkenaNo ratings yet
- Nazi Human Experimentation OutputDocument2 pagesNazi Human Experimentation OutputYana PotNo ratings yet
- Community Acquired PneumoniaDocument52 pagesCommunity Acquired Pneumoniatummalapalli venkateswara rao100% (6)