0% found this document useful (0 votes)
1K views82 pagesABO Grading System
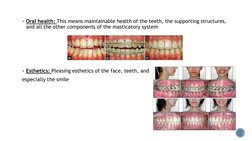
1. The document discusses the importance of defining clear treatment goals including oral health, esthetics, occlusion, function, and stability at the beginning of orthodontic treatment planning.
2. It outlines gnathological principles for achieving optimal occlusion during finishing, including achieving centric occlusion, mutually protective occlusion, and cusp embrasure occlusion.
3. Key factors for orthodontic finishing and detailing are discussed, such as tooth structure, position, torque, tip, overbite, overjet, and curve of Spee. Maintaining stability of the final occlusion is the ultimate goal.
Uploaded by
sanjeed sanjuCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
1K views82 pagesABO Grading System
1. The document discusses the importance of defining clear treatment goals including oral health, esthetics, occlusion, function, and stability at the beginning of orthodontic treatment planning.
2. It outlines gnathological principles for achieving optimal occlusion during finishing, including achieving centric occlusion, mutually protective occlusion, and cusp embrasure occlusion.
3. Key factors for orthodontic finishing and detailing are discussed, such as tooth structure, position, torque, tip, overbite, overjet, and curve of Spee. Maintaining stability of the final occlusion is the ultimate goal.
Uploaded by
sanjeed sanjuCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
- Introduction: An introduction to the finishing procedures considered in orthodontic treatments highlighting the objectives of treatment sequences.
- Historical perspective: Discusses the evolution of concepts in orthodontic finishing by examining historical perspectives from key figures like Angle and Tweed.
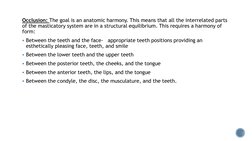
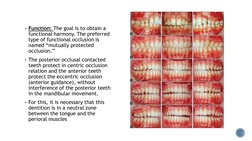
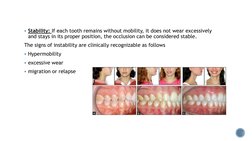
- Gnatological Principles in Finishing: Details the fundamental gnatological principles applied in orthodontic case finishing, including occlusion types and tooth positioning.
- Andrews Six Keys of Occlusion: Introduces Andrews' six keys theory which is pivotal in assessing orthodontic treatment results.
- Dougherty's Factors in Finishing: Lists Dougherty's 17 key factors for achieving precise finishing and detailing in orthodontics.
- MBT Guidelines: Offers guidelines on various aspects to consider during closing stages of orthodontic treatment under the MBT system.
- PAR Index: Describes the development and application of the PAR index in assessing orthodontic treatment outcomes.
- ABO: Details the scoring systems and grading protocols established by the American Board of Orthodontics.