Professional Documents
Culture Documents
FIX BOOK Reading Treatment Fracture
Uploaded by
Selma Mutiara0 ratings0% found this document useful (0 votes)
32 views52 pagesOriginal Title
FIX BOOK reading treatment fracture.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
32 views52 pagesFIX BOOK Reading Treatment Fracture
Uploaded by
Selma MutiaraCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 52
BOOK READING
dr. Sholahuddin Rhatomy, Sp.OT
Selma Mutiara Hani
Nadia Dini Yulianti
Felicia Seruni Sekar Asri
Treatment For Fracture
the four basic goals of all fracture treatment :
1) to relieve pain
2) to obtain and maintain satisfactory position of the fracture
fragments
3) to allow, and if necessary encourage, bony union
4) to restore optimum function, not only in the fractured limb or spine
but also in the patient as a person
treatment for closed fracture
• Protection Alone (without Reduction or Immobilization)
Indication : Protection alone is indicated for undisplaced or
relatively undisplaced, stable fractures of the ribs,
phalanges, metacarpals-and in children, of the clavicle. A
second indication is that group of fractures, such as mild
compression fractures of the spine and impacted fractures
of the upper end of the humerus, in which the total result
will be better without either reduction or immobilization.
Protection alone is also indicated after clinical union has
been obtained by other means) but before complete
radiological consolidation has been established.
Risk : The protection provided may not be adequate for the
particular patient (especially a very young child or an
uncooperative adult), in which case the fracture may become
displaced; hence, the need for radiographic examinations of the
fracture site at re gular intervals during the healing process.
treatment for closed fracture
• Immobilization by External Splinting (without Reduction)
• Immobilization of a fracture by external splinting is only
relative immobilization, as opposed to rigid fixation, in as
much as some motion can still occur inside the limb or trunk
at the fracture site during the early phases of healing.
Relative immobilization is usually, achieved by the use of
plaster-of-Paris casts of varying design and occasionally by
metallic or plastic splints
• Indication : Immobilization by external splinting without
reduction is indicated for fractures that are relatively
undisplaced, yet unstable.
• Such fractures merely require maintenance of the existing position of
the fracture fragments during the healing process. A long bone
fracture in which there is only sideways shift of the fragments in
relation to one another but good contact and no significant angulation
or rotation does not re- quire reduction; it does, however, require
relative immobilization
• Risk : subsequent muscle pull and gravitational forces may cause
further displacement such as angulation, rotation) or overriding that is
unacceptable; hence the need for repeated radiographic
examinations during the early stages of healing. Improperly applied
casts or splints may cause local pressure sores over bone
prominences, or constriction of a limb with resultant impairment of
venous or arterial circulation, or both.
treatment for closed fracture
• Closed Reduction by Manipulation Followed by Immobilization
Closed reduction of a fracture, which is a form of surgical
manipulation, is by far the most common method of treatment for
the majority of displaced fractures in both children and adults.
Immobilization of the fracture by means of a plaster-of-Paris cast is
the most common method of maintaining the reduction.
in general it involves placing the fracture fragments where they
were at the time of maximal displacement and then reversing the
path of displacement.
Indication : Closed reduction by manipulation followed by
immobilization is indicated for displaced fractures that require
reduction and when it is predicted that sufficiently accurate
reduction can be both obtained. and maintained by closed means.
• Risk : Closed reduction that is ineptly and inaptly applied with more
force than skill may cause further damage to soft tissues
including blood vessels) nerves and even the periosteum.
Excessive traction in the longitudinal axis of the limb during
reduction may even produce arterial spasm particularly at the
elbow and knee, with resultant Volkmann's ischemia. Pressure
sores over bony prominences and pressure injuries to
peripheral nerves over bony prominences (especially the lateral
popliteal nerve where it crosses the neck of the fibula) may also
occur . Fractures in which the reduction is not sufficiently stable,
especially oblique, spiral, and comminuted fractures, may become
displaced subsequently within the cast and repeated radiographic
assessments of the positron of the fragments are essential during
the early stages of healing.
treatment for closed fracture
• Closed Reduction by Continous Traction followed by
Immobilization
• For fractures in young children, continuous traction can be
applied through the skin by means of extension tape (skin
traction) .For older children and adults in whom greater traction
force is required, it is best applied through bone by means of a
transverse rigid wire or pin (skeletal traction). Furthermore, the
traction device may be fixed to the end of the bed (fixed
traction), or it may be balanced by cords with pulleys and
weights (balanced traction)
• Indication : Closed reduction by continuous traction is
indicated for unstable oblique, spiral, or comminuted fractures
of major long bones, and unstable spinal fractures. Skeletal
traction is also applicable to the treatment of fractures
complicated by vascular injuries) excessive swelling, or skin
loss in which an encircling bandage or cast would be
dangerous.
• Risk = excessive longitudinal traction cause arterial spasm with
resultant Volkmann's ischemia (compartment syndrome). Ineptly
applied skin traction) excessive traction, or both may result in
superficial skin loss, whereas skeletal traction may become
complicated by pin track infection that reaches the bone. if
inaccurate, applied and monitored, may fail to achieve and
maintain adequate reduction of the fracture. Excessive traction may
also distract the fracture fragments with resultant delayed union or
even nonunion; osteoblasts can creep but cannot leap.
treatment for closed fracture
• Closed Reduction Followed by Functional Fracture-Bracing
• The principle of functional fracture-bracing is based on the
following concepts: I ) that rigid immobilization of fracture
fragments is not only unnecessary but also undesirable for
fracture healing; 2) that function and the resultant controlled
motion at the fracture site actually stimulate healing through
abundant callus formation; 3) that such function prevents
iatrogenic joint stiffness; 4) that some what less than perfect
(anatomical) reduction of a fracture of the shaft of a long
bone does not create significant problems concerning either
function or appearance (cosmesis)
• Indication : Closed reduction followed by functional fracture-
bracing is indicated for fractures of the shaft of the tibia, the
distal third of the femur, the humerus, and the ulna in adults.
The method is contraindicated for fractures drat can be more
effectively treated by open reduction and internal skeletal
fixation, including intertrochanteric fractures of the femur,
subtrochanteric and mid-shaft frac- tures of the femur, and
shaft of the radius and intra- articular fractures.
• Risk : Although functional fracture-bracing is relatively risk
free, there is a possibility that the method will fail to maintain
an acceptable position of the fracture fragments, in which case
alternative methods such as open reduction and internal
fixation may still be applied.
treatment for closed fracture
• Closed Reduction by Manipulation Followed by External skeletal
Fixation
Indications: for severely comminuted (and unstable) fractures of the
shaft of the tibia or femur, especially type 3 open fractures with
extensive injuries to soft tissues including arteries and nerves, the
repair of which necessitates immobilization of the fracture site.
External skeletal fixation may also be indicated for unstable fractures
of the pelvis, humerus, radius, and metacarpals
Risks: The main risk of external skeletal fixation is pin track infection
with or without osteomyelitis. If the pins are inserted by means of a
high-speed pourer drill, the surrounding bone may be "burnt to death"
by the heat of friction, in which case superimposed infection will
produce a ring sequestrum.
treatment for closed fracture
• Closed Reduction by Manipulation Followed by Internal skeletal
Fixation
Indications: for certain fractures in which accurate reduction can be
obtained by closed means but cannot or should not be maintained by
external immobilization, for example unstable fracture of the neck of the
femur in both children and adults. After accurrate reduction, the internal
fixation device is driven across the fracture site through a small skin
incision using radiographic control. Certain fractures in the midshaft of
the long bones that can be reduced by closed means also lend
themselves to blind intramedullary nailing under radiographic control.
Risks: The closed manipulative reduction may fail to obtain a
satisfactory position of the fracture fragments and the skeletal fixation
may fail to achieve sufficiently rigid fixation of the fracture. Because with
internal skeletal fixation the skin is traversed, the risk of infection is ever
present.
treatment for closed fracture
• Open Reduction Followed by Internal Skeletal Fixation
The operative reduction of fractures should be performed (or at least
supervised) only by an experienced surgeon and only in a favorable setting
such as an operating theater that has a consistently low infection rate and is
properly equipped with adequate instruments. Once the fracture has been
reduced at open operation, the reduction must be maintained by internal
fixation, which is achieved by using some type of metallic device, a technique
that is sometimes referred to as osteosynthesis.
Indications: where there is a coexistent vascular injury that requires
exploration and repair, displaced avulsion fractures, intra-articular fractures in
which reduction of the joint surface must be perfect, displaced fractures in
children that cross the epiphyseal plate (physis), and fractures in which soft
tissues have become interposed and trapped between the fragments.
Risks: infection, also carries the risk of further damage to the blood. supply of
the fracture fragments which, in turn, may lead to delayed union and even
nonunion.
treatment for closed fracture
• Excision of a Fracture Fragment and Replacement by an
Endoprosthesis
Indications: Because of the high incidence of avascular necrosis of
the femoral head and nonunion of the fracture, displaced intracapsular
fractures of the neck of the femur in the elderly cannot always be
managed satisfactorily by internal fixation. Comminuted fractures of the
radial head in adults are not amenable to internal fixation. If the elbow
joint is grossly unstable as a result of coexistent ligamentous injury, the
radial head may be replaced by an endoprosthesis. For severely
comminuted and grossly, unstable supracondylar fractures of the
humerus in adults, an elbow prosthesis may be required
Risks: infection, there is also a risk, particularly in the elderly hip, that
the endoprosthesis will gradually migrate through osteoporotic bone of
the pelvis or femur.
Treatment for open fracture
• Prevention of infection and obtaining union of the fracture.
• The extent of the skin wound of an open fracture varies considerably. It may be a
small puncture wound caused by penetration of the skin from within by a sharp,
jagged spike of bone (Fig. 15.10), or by penetration of the skin from without by a
missile such as a bullet. The wound may be a sizeable tear in the skin through which
bare bone is still protruding.
• Classification of open fracture (Gustilo & Anderson):
1. Type 1 : clean wound less than I cm in length (usually from within with little soft tissue
injury)
2. Type 2 : a laceration more than I cm in length but without extensive soft tissue
damage, skin flaps, or avulsions and with a simple transverse or oblique fracture
3. Type 3A : extensive soft tissue damage but adequate bone coverage, segmental
fractures and gunshot wounds
4. Type 3B : extensive soft tissue damage with extensive periosteal stripping and
devascularized bone that requires skin flaps or free grafts. This type is usually
associated with gross contamination
Treatment for Open Fractures
• Because open (compound) fractures have communicated with
the external environment through the skin and have already
been complicated by bacterial contamination, they carry the
serious risk of becoming further complicated by infection.
• Emphasis on the prevention of infection and obtaining
union of the fracture.
• Because of the extensive soft tissue injury associated with
open fractures, they usually take much longer to unite than
closed fractures.
• An instant ("polaroid") photograph should be taken of every
open fracture in the emergency room before a sterile
dressing has been applied, or in the operating room, to
provide an important item for the hospital record and to avoid
the risk of additional contamination from repeated
preoperative inspections of the open wound by consulting
surgeons.
Classification of Open Fractures
Gustilo and Anderson were able to distinguish three distinct categories, based on the
severity of the soft tissue injury :
• Type 1 : a clean wound less than I cm in length (usually from within with little soft
tissue injury);
• Type 2 : a laceration more than I cm in length but without extensive soft tissue
damage, skin flaps, or avulsions and with a simple transverse or oblique fracture;
• Type 3 : extensive soft tissue damage such as skin flaps, avulsions, and muscle and
nerve injuries.
More recently, Gustilo has described three categories of type 3 open fractures:
• 3A : extensive soft tissue damage but adequate bone coverage, segmental
fractures, and gunshot wounds;
• 3B : extensive soft tissue damage with extensive periosteal stripping and
devascularized bone that requires skin flaps or free grafts. This type is usually
associated with gross contamination;
• 3C : associated vascular injury requiring repair.
• The authors recommended primary closure of the skin in
types I and 2 open fractures (this is controversial) but
delayad primary closure in type 3 open fractures.
• In many trauma centers, open fractures are left open initially,
that is, for the first 4 to 7 days.
• Using antibiotics (usually one of the cephalosporins) before,
during, and after operation, the overall infection rate was 2,4
% whereas the infection rate for type 3 injuries alone was
l0%.
Aspects of Treatment for Open Fractures
Cleansing the Wound :
• Gross dirt, bits of clothing, and other foreign material should
be literally washed away by extensive pulsating irrigation as
well as by mechanical cleansing with copious amounts of
sterile water or isotonic saline (rather than merely
camouflaged by strong antiseptics that cause further tissue
damage).
• The wound may even have to be opened further to allow
adequate assessment of the degree of contamination and to
deal with it.
Excision of Devitalized Tissue (Debridement).
• Because tissues that have lost their blood supply prevent
primary wound healing and enhance infection, the
meticulous surgical excision of all devitalized tissue, such as
skin, subcutaneous fat, fascia, muscle, and loose fragments of
bone, is essensial.
• It also is wise to obtain a culture of the wound at the time of
operation.
Treatment of the Fracture :
• When the open wound is small, such as a puncture wound from
within, the fracture can usually be treated by closed means, after
the wound has been cleansed, debrided, and left open.
• In general, internal fixation may be used unless it is thought that
its mere insertion would tend to traumatize and devitalize more
tissue and increase the risk of infection.
• Under certain circumstances, such as excessive instability of the
fracture or an associated vascular injury, internal fixation is
completely justified because the risks of its application are less
serious than the risks of alternative methods.
Closure of the Wound :
• Even when the open fracture is treated within "the golden period" of
the first 6 or 7 hours and contamination is not extensive,
immediate primary closure of the wound is usually
contraindicated, in keeping with the aphorism "leave open
fractures open." After the first 4 to 7 days, provided no infection
has developed, delayed primary closure of the wound is
indicated.
• Loss of skin may necessitate the delayed application of split
thickness skin grafts. Suction drainage should be used to prevent
accumulation of blood and serum in the depths of the wound.
• Delayed primary closure is particularly applicable in grossly
contaminated open fractures sustained on the battlefield or in
major disasters.
Antibacterial Drugs :
• To be effective in the prevention of infection, antibacterial
drugs must be administered in large doses before, during, and
after treatment of the wound. Even so, antibacterial treatment
is no guarantee against infection because many bacteria are
resistant to various drugs.
• Furthermore, antibacterial drugs cannot reach any wound
tissue that has lost its blood supply. The surgical care of
the wound is of even greater importance than the
antibacterial therapy.
Prevention of Tetanus :
• All patients with open fractures require preventive measures
against the uncommon but serious complication of tetanus.
• If the patient has been previously immunized by tetanus
toxoid, a booster dose of toxoid should be given.
• If there has been no previous immunization, or if inadequate
information is available, immediate passive immunity can be
achieved by the use of 250 units of tetanus immune
globulin (human). Active immunity with tetanus toxoid is
initiated at the same time.
Anesthesia for Patients with Fractures
• During the first hour after a fracture has occurred, the
patient's tissues are somewhat numb and under these
circumstances only, it may be possible to reduce certain
fractures without anesthesia.
• Even then, however, reduction without anesthesia should be
performed only if the physician or surgeon is confident that it
can be accomplished with one deft manipulation and the
patient is not unduly tense and nervous.
• Certain fractures, such as a Colles' fracture at the lower end of
the radius in adults, are amenable to reduction after
infiltration of a local anesthetic agent in and around the
fracture site.
• Other fractures in the limbs can be reduced under regional
anesthesia such as a brachial plexus block for the upper
limb and a spinal anesthetic for the lower limb.
• In general, the majority of fractures requiring reduction are
best treated under general anesthesia, which provides
complete comfort and the muscle relaxation necessary in
reducing a fracture.
• The risk of aspiration of stomach contents during the
induction of general anesthesia as well as during the
recovery period merits special mention in relation to patients
with fractures.
• After a significant injury, such as a fracture, gastric motility
virtually ceases for many hours and consequently, if the
patient has ingested food or drink shortly before or after the
injury, the stomach retains a mixture of undigested food and
gastric acid, either of which can cause death if aspirated into
the trachea or lungs.
• Under these circumstances, unless there is a serious
complication such as an open fracture or a vascular injury,
general anesthesia should be delayed until at least 6 hours
after the ingestion of food or drink; even after this period,
special precautions, such as removal of gastric contents
through a tube, are necessary to prevent the serious
complication of aspiration.
• The welfare of the patient must always take precedence over
the convenience of his or her physician or surgeon.
• Temporary splints should not be removed nor the fractured
part be moved during the preliminary stages of anesthesia, or
the painful stimulus could initiate either cardiac arrest or
laryngeal spasm.
After-Care and Rehabilitation for Patients with
Fractures
Four aims of all fracture treatment are :
1. to relieve pain;
2. to obtain and maintain satisfactory position of the fracture
fragments;
3. to allow and if necessary to encourage bony union;
4. to restore optimum function.
The most important is restoration of function.
• Excessive and persistent edema in soft tissues produces
glue-like adhesions with resultant joint stiffness.
• It should be prevented or minimized by appropriate elevation
of the fractured limb during the early phase of fracture healing,
as well as by improvement of venous return through active
exercises of all regional muscles.
• Muscles that are not used soon exhibit disuse atrophy, which
can be prevented by active static (isometric) exercises of
those muscles that control the immobilized joints, and active
dynamic (isotonic) exercises of all other muscles of the limb
or trunk.
• Supervised physiotherapy is particularly important in the after-
care of adults with fractures.
• All joints that are not immobilized by the fracture treatment
should be put through a full range of motion daily by the
patient.
• In addition to presentation of function in the muscles and joints
after a fracture, healthy function in the patient's mind must
also be preserved, because the patient's attitude toward his or
her injury determines to a considerable extent the rate at
which recovery will progress.
• Indeed, psychological consideration added to good care of
the patient's fracture can usually prevent unnecessary
despondency, depression, and undue concern about the
future.
• After the period of external immobilization of the fracture,
active exercises should be continued even more vigorously
until normal muscle power and joint motion have been
regained.
• If necessary, the patient should be retrained in the activities of
daily living and occupation, usually through supervised
occupational therapy.
• Rehabilitation of the whole person, is always important,
especially when the fracture has required a particularly long
period of treatment or has been associated with serious
complications.
Complications of Fracture Treatment
These complications are mostly preventable; they are related to three main
factors: excessive local pressure, excessive traction, and infection.
1. Skin Complications : Tattoo effect from abrasions, Pressure lesions
(pressure sores), Bed sores (decubitus ulcers), Cast sores (cast ulcers)
2. Vascular Complications : Traction and pressure lesions, Volkmann's
ischemia (compartment syndromes), Gangrene and gas gangrene,
Venous thrombosis and pulmonary embolism
3. Neurological Complications : Traction and pressure lesions
4. Joint Complications : Infection (septic arthritis) complicating open
operative treatment of a closed injury
5. Bony Complications : Infection (osteomyelitis) complicating open
operative treatment of a closed injury
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Cosmology: Beyond The Big BangDocument60 pagesCosmology: Beyond The Big BangHaris_IsaNo ratings yet
- Jharkhand Bijli Vitran Nigam LimitedDocument2 pagesJharkhand Bijli Vitran Nigam LimitednandksrkumarNo ratings yet
- APO SNP Training - GlanceDocument78 pagesAPO SNP Training - GlanceAshwani SharmaNo ratings yet
- Learning - Module.Facial Care Proj.Document24 pagesLearning - Module.Facial Care Proj.Ria Lopez100% (8)
- Hughes Consciousness and Society 1958Document468 pagesHughes Consciousness and Society 1958epchot100% (1)
- Jama 2017 11469Document10 pagesJama 2017 11469Selma MutiaraNo ratings yet
- Supp Mdu526 Mdu526suppDocument37 pagesSupp Mdu526 Mdu526suppSelma MutiaraNo ratings yet
- Clinical Relevance of Folinic Acid Over Rescue AFTER HFMTXDocument6 pagesClinical Relevance of Folinic Acid Over Rescue AFTER HFMTXSelma MutiaraNo ratings yet
- Sumup Toxi OsDocument21 pagesSumup Toxi OsSelma MutiaraNo ratings yet
- Laporan Jaga IGD 24 Juni 2019Document16 pagesLaporan Jaga IGD 24 Juni 2019Selma MutiaraNo ratings yet
- EBM-Internal Med Students-FinalDocument29 pagesEBM-Internal Med Students-FinalSelma MutiaraNo ratings yet
- Statement of Purpose For Studying MechatronicsDocument2 pagesStatement of Purpose For Studying MechatronicsBivash NiroulaNo ratings yet
- My Two Week Meal Plan: Day Date Breakfast Lunch Dinner SignatureDocument1 pageMy Two Week Meal Plan: Day Date Breakfast Lunch Dinner SignatureIan Nathaniel Versoza AmadorNo ratings yet
- My Kind Neighbour Simple Present Grammar Guides Reading Comprehension Exercises Tes - 74419Document1 pageMy Kind Neighbour Simple Present Grammar Guides Reading Comprehension Exercises Tes - 74419algarinejo100% (1)
- Power Transmission, Distribution and Utilization: Lecture# 13 &14: Underground CablesDocument29 pagesPower Transmission, Distribution and Utilization: Lecture# 13 &14: Underground CablesPhD EENo ratings yet
- Safety Data Sheet: 1. Identification of The Substance / Mixture and of The Company /undertakingDocument7 pagesSafety Data Sheet: 1. Identification of The Substance / Mixture and of The Company /undertakingOrshanetzNo ratings yet
- Linear RegressionDocument541 pagesLinear Regressionaarthi devNo ratings yet
- Digital Photography in OrthodonDocument48 pagesDigital Photography in OrthodonSrinivasan BoovaraghavanNo ratings yet
- Indore BrtsDocument22 pagesIndore BrtsRaj PatelNo ratings yet
- ESL Mid Test Semester 1 Grade 3Document3 pagesESL Mid Test Semester 1 Grade 3Elis ElisNo ratings yet
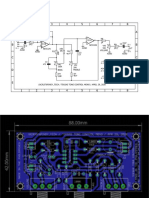
- Teksas Tone Control MonoDocument17 pagesTeksas Tone Control MonoRhenz TalhaNo ratings yet
- Engglis Isma E. N (18010107023) Tadris IpaDocument6 pagesEngglis Isma E. N (18010107023) Tadris IpaLita Dwi HasjayaNo ratings yet
- Martinal LEO - Product RangeDocument6 pagesMartinal LEO - Product RangeAdamMitchellNo ratings yet
- John 8 - 58 - Truly, Truly, I Tell You, - Jesus Declared, - Before Abraham Was Born, I Am!Document8 pagesJohn 8 - 58 - Truly, Truly, I Tell You, - Jesus Declared, - Before Abraham Was Born, I Am!Joshua PrakashNo ratings yet
- Food and DrinkDocument5 pagesFood and DrinkHec Al-HusnaNo ratings yet
- NCM 117 - Case Study 1 DarundayDocument18 pagesNCM 117 - Case Study 1 DarundayEzra Miguel DarundayNo ratings yet
- By: DR Evita Febriyanti Fast Track - Dual Degree 2016 Brawijaya UniversityDocument12 pagesBy: DR Evita Febriyanti Fast Track - Dual Degree 2016 Brawijaya UniversityEvitaFebriyantiPNo ratings yet
- Classified Coordinate Geometry Further Maths ExercisesDocument24 pagesClassified Coordinate Geometry Further Maths ExercisesAbrar RahmanNo ratings yet
- Industry X.0: Realizing Digital Value in Industrial SectorsDocument15 pagesIndustry X.0: Realizing Digital Value in Industrial SectorsJamey DAVIDSONNo ratings yet
- Green Gram CultivationDocument7 pagesGreen Gram CultivationSudhakar JayNo ratings yet
- CTR201Document2 pagesCTR201Vicente RezabalaNo ratings yet
- Tacticity, Geometric IsomerismDocument7 pagesTacticity, Geometric IsomerismbornxNo ratings yet
- 2.1 Energy Flow in An EcosystemDocument13 pages2.1 Energy Flow in An EcosystemJoanne OngNo ratings yet
- Investigation of Liquid-Liquid Phase Equilibria For Reactive Extraction of Lactic Acid With Organophosphorus SolventsDocument6 pagesInvestigation of Liquid-Liquid Phase Equilibria For Reactive Extraction of Lactic Acid With Organophosphorus Solventskudsiya firdousNo ratings yet
- Stories of Love and AdventureDocument24 pagesStories of Love and AdventureMargie HernandezNo ratings yet
- Harga Satuan Precast 2017Document2 pagesHarga Satuan Precast 2017GenTigaBrotherhood BantenNo ratings yet